Abstract
Objectives To describe the technique and results of the arthroscopic surgical treatment of volar ganglion cyst of the wrist.
Materials and Methods The present study comprised 21 patients submitted to the arthroscopic treatment of volar ganglion cysts of the wrist from January 2015 to May 2017, with a full evaluation for at least 6 months. The technique was indicated for patients presenting pain and functional impairment for more than four months, with no improvement with the conservative treatment, or for those with cosmetic complaints and cyst present for more than three months.
Results The mean age of the patients was 43.6 years; 16 (76%) patients were female, and 5 (24%) were male. The mean follow-up time from surgery to the final assessment was of 10.9 months. A total of 2 (9.6%) patients complained of mild pain after the procedure, and another patient presented slight motion restrictions. The 18 (90.4%) remaining patients reported cosmetic improvement, complete functional recovery, and pain improvement. There were no recurrences or infections. No patient required further surgery.
Conclusions The arthroscopic resection of volar ganglion cysts is a useful and safe technique. It is a minimally-invasive procedure, with low morbidity and very few complications, representing a good alternative to the open technique.
Keywords: musculoskeletal diseases/surgery, wrist joint, ganglion cyst, arthroscopy/use
Introduction
The synovial cyst, also known as ganglionic cyst, is the most common tumor lesion of the wrist. Although the volar location is not the most common, it is the location in up to 20% of the patients. 1 Most lesions originate from the radiocarpal joint, but they may arise from the midcarpal joint, especially the scaphotrapeziotrapezoid joint (STT, also called triscaphe joint). 1 2
The volar synovial cyst lies under the skin, between the flexor carpi radialis (FCR) and flexor pollicis longus (FPL) muscle tendons, and is caused by mucinous degeneration of the joint capsule. It is composed of an extracapsular portion, comprising a subcutaneous palpable mass, and an intracapsular portion, formed by the base and valve (or pedicle), which can be at the radiocarpal or midcarpal joints. 1
The treatment is predominantly conservative, but patients with symptomatic lesions following conservative procedures or those with esthetic complaints are candidates for surgical therapy. 3 4 5 The principle of the surgical treatment is decompression and drainage, resecting a portion of the joint capsule and cyst wall; complete tumor resection, however, is not required. 4
Today, arthroscopy has become a consolidated technique in the treatment of orthopedic conditions. Thanks to technological advancements, arthroscopic procedures in small joints through direct visualization enable the diagnosis and immediate treatment of intra-articular lesions. 6 Arthroscopic resection, initially described by Osterman and Raphael 7 for dorsal cysts, is a minimally invasive alternative to the open technique. 1 3 7 It has advantages such as lower postoperative pain, scarring and stiffness, in addition to a faster return to work without a higher incidence of complications. 7 In 2003, Ho et al 8 described the arthroscopic resection technique for volar cysts; however, since then, few series evaluating this treatment were published. 1 2 3 9 10 11 12 13
The present study aims to describe the arthroscopic technique for wrist volar synovial cyst treatment by retrospectively analyzing a case series.
Methods
After approval by the institutional Ethics Committee, patients who underwent wrist arthroscopy for volar synovial cyst treatment from January 2015 to May 2017 were included in the study. The synovial cyst was diagnosed by physical examination and imaging scans (ultrasound and/or magnetic resonance imaging).
From a total of 24 patients who underwent arthroscopic volar cyst resection, 3 were excluded due to lack of adequate follow-up; therefore, the sample consisted of 21 patients.
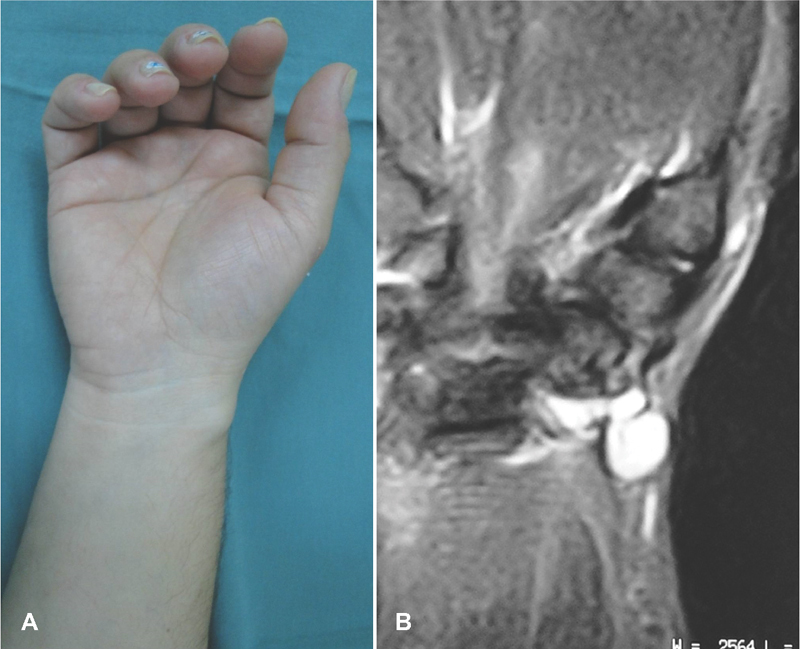
Only anterior wrist synovial cysts located proximal to the wrist flexion fold and between the radial edge of the FCR tendon and volar to the first extensor compartment were included in the study ( Figure 1 ). The surgical indication criteria were pain and functional disability – defined as difficulty or inability to use the hands in everyday activities – for more than four months, with no improvement after the conservative treatment (expectant therapy, analgesia and/or aspiration), and asymptomatic patients with esthetic complaints or lesions for more than three months.
Fig. 1.
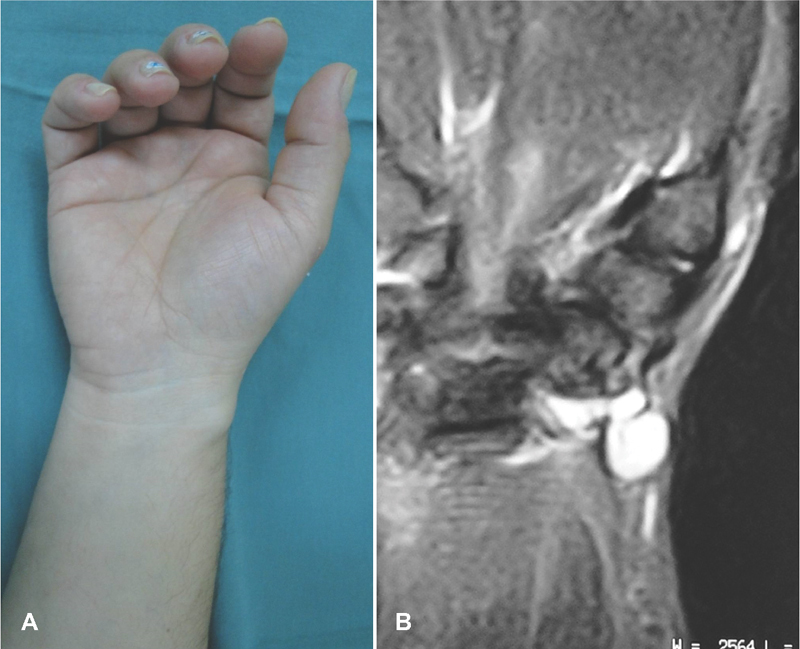
Clinical aspect of the volar synovial cyst observed under the skin, proximal to the wrist flexion fold, between the flexor carpi radialis (FCR) and flexor pollicis longus (FPL) muscle tendons ( A ). Magnetic resonance imaging scan of the lesion ( B ).
Patients with degenerative joint disease and those with postoperative follow-up period shorter than six months were not included in the study. After the procedure, the patients were reviewed weekly in the first month and then every 60 days until 6 months of follow-up, when the final assessment occurred. Relapse after puncture or previous surgical treatment were not considered exclusion criteria.
In the retrospective review, we analyzed the clinical outcomes and possible complications resulting from surgery. The outcomes were synthesized by filling out a questionnaire including data from the physical examination, which was directly performed by one of the authors and duly logged in the medical records.
Patient data such as age, gender, and dominance were included, as well as the characteristics of the lesion, such as location, size, previous treatments, complaints and time between its onset and surgery. The results were measured at least six months after surgery. The degree of patient satisfaction was also considered. Pain was assessed, both preoperatively and at the final evaluation, using the visual analog scale (which ranges from 0 to 10, in which 0 means no pain and 10 means the worst pain possible). Procedural features, including surgical time, used portals, pedicle location and associated injuries, as well as postoperative immobilization time, were investigated. Wrist mobility was assessed, and possible complications, such as recurrence, infection, hypertrophic scar, stiffness, tendon injury, or vascular-nervous injury, were evaluated. In addition, time until return to work (or normal activities in case of retired/unemployed patients) was questioned.
The results were classified as good, moderate and poor following the criteria described by Rocchi et al, 1 which are explained in Table 1 .
Table 1. Classification of postoperative results according to the criteria used by Rocchi et al 1 .
| Result | Criteria |
|---|---|
| Good | No recurrence; active movement and grip strength equal to those observed before surgery; no pain; painless and esthetically appropriate scar; no severe arterial lesions; no neurological lesions. |
| Moderate | No recurrence; active movement and grip strength equal to those observed before surgery; no severe arterial injury; local pain or broad or hypertrophic scar; painful scar; mild neurological injury. |
| Bad | Presence of one of the following criteria: recurrence; partial movement or grip strength loss; and arterial or neurological lesion. |
During the final evaluation, each patient reported his/her subjective satisfaction by choosing one the following options: very satisfied, satisfied, slightly dissatisfied and dissatisfied with the treatment.
Surgical technique
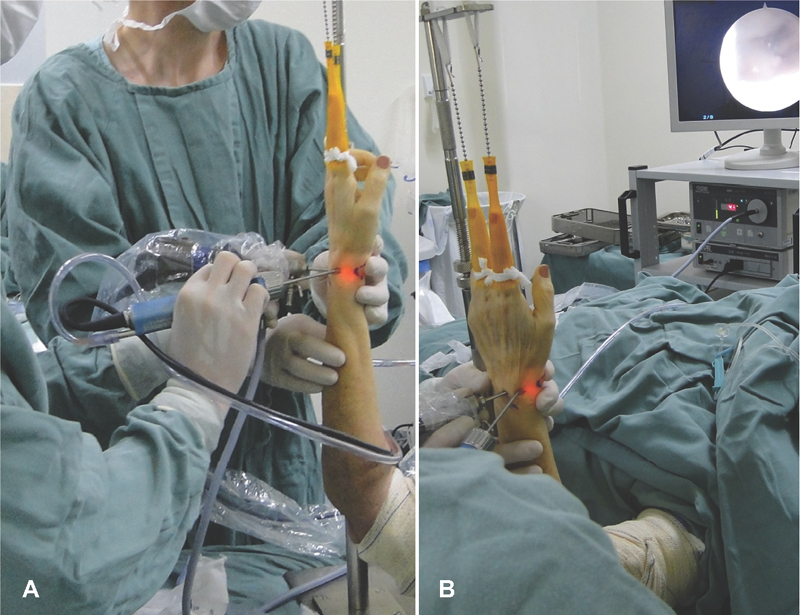
The procedure is performed with regional brachial plexus block and pneumatic tourniquet. In supine position, the patient's arm is fixed on the auxiliary table using a traction support with the elbow at 90° of flexion. The long fingers are encased in surgical finger traps, making it easy to position and place continuous 5-kg traction to the zenith ( Figure 2 ). Initially, the cyst is marked with a dermographic pen to demonstrate its size and location, which makes its resection easier and serves as a parameter to assess the emptying of its content after the procedure. Dorsal portals for wrist arthroscopy are palpated and marked. The procedure is performed with an endoscope with an angle of 30° and a diameter of 2.7 mm. At first, the 3/4 portal is made, with a 12° angle from from distal to proximal following the normal anatomy of the radiocarpal joint. This portal makes the entry of the endoscope easier, avoiding iatrogenic damage to the cartilaginous tissue. Next, a second portal, usually the 6R portal, is opened for instrumentation. Careful inspection of the entire joint is then performed, with visualization of chondral tissue, the capsule and ligaments, searching for other conditions that may cause symptoms ( Figure 3 ).
Fig. 2.

Positioning for wrist arthroscopy. The long fingers are encased in surgical finger traps, making it easy to position and place continuous 5-kg traction to the zenith ( A ). Volar cyst marked with a dermographic pen to show its size and location ( B ).
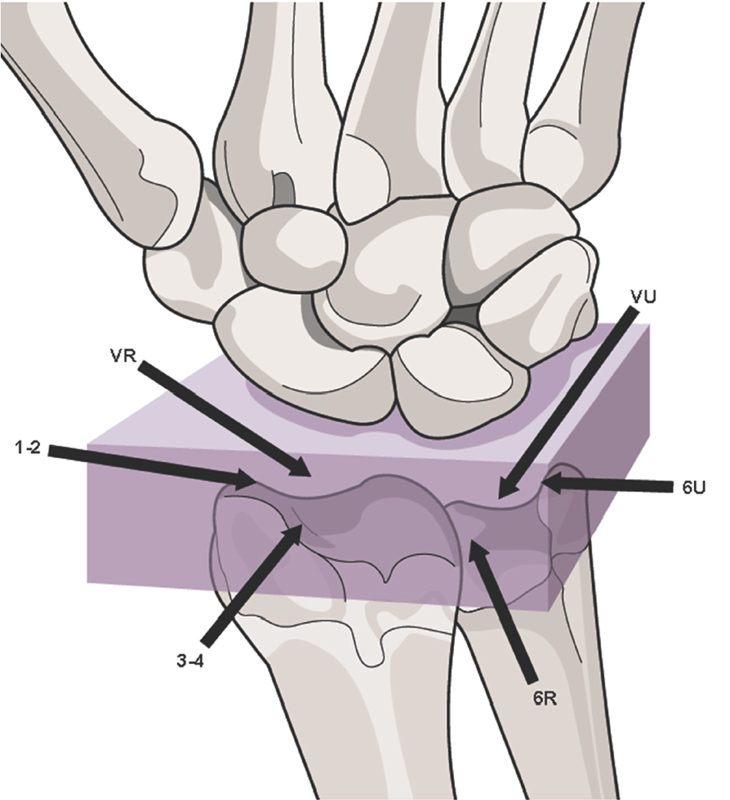
Fig. 3.
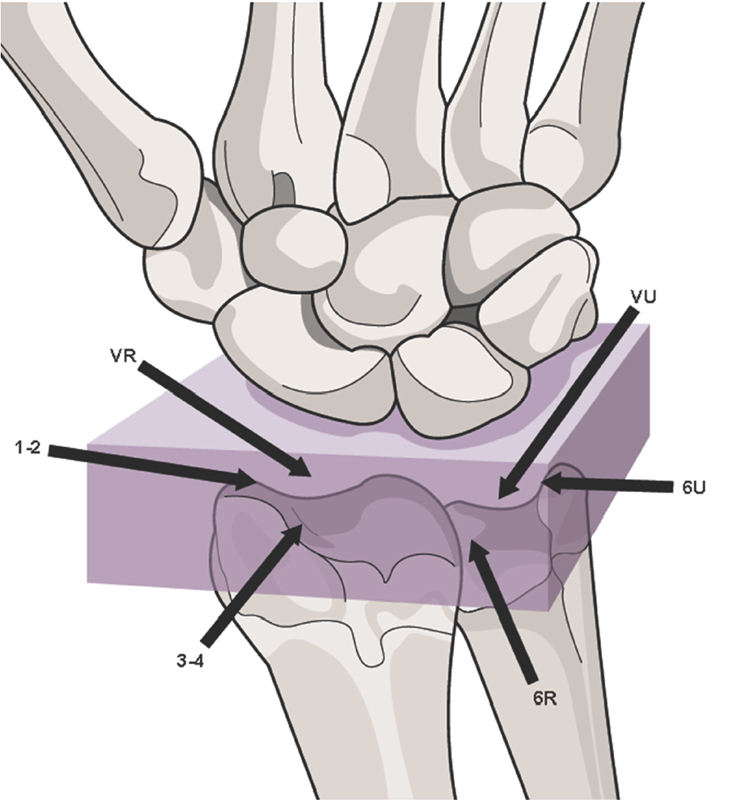
Portals most commonly used for wrist (radiocarpal) arthroscopy.
Next, the cyst pedicle is located; in most patients, it lies within the range of the volar radiocarpal ligaments, usually between the radioscaphocapitate ligament (RSCL) and the long radiolunate ligament (LRLL) ( Figure 4 ). For resection and drainage of the volar synovial cyst, the endoscope is positioned at the 3/4 portal in front of the interval between the RSCL and the LRLL. Under intra-articular vision, a new portal is made, the 1/2 portal, for 2.0- or 2.9-mm soft-tissue shaver instrumentation. External manual pressure is applied over the cyst to facilitate pedicle location. This maneuver results in the appearance of a hypertrophic synovial tissue prominence between these two ligaments ( Figure 5 ). This is the location of the cyst pedicle; once the capsule is punctured, the cyst's mucous content spills into the joint, proving that its wall has been ruptured ( Figure 6 ). Capsule opening and continuous suction of the cyst content lead to the complete disappearance of the mass. Then, great care is required with deeper, noble structures, such as the radial artery, flexor tendons and radial sensory nerve. The abnormal synovial tissue must be resected along with a 4- to 6-mm portion of the volar capsule, forming a window-shaped defect. Again, external pressure on the cyst may assist in pedicle resection and complete content drainage. If there is any doubt that the cyst has been completely resected or if drainage is difficult, the portals can be changed, that is, the endoscope can be placed at the 6R portal, and the shaver, at the 3/4 portal. This will provide a more direct angle of attack to the shaver regarding the pedicle of the cyst. Another option is to place the endoscope at the 1/2 or 3/4 portal for instrumentation. These variations in the position of the endoscope and shaver in the portals are also performed according to the operated wrist side and the dominant side of the surgeon.
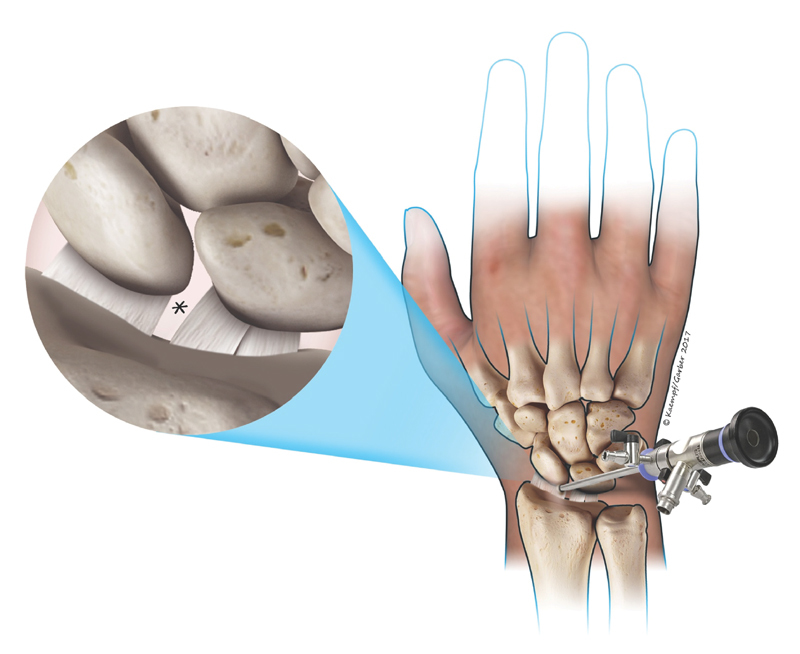
Fig. 4.
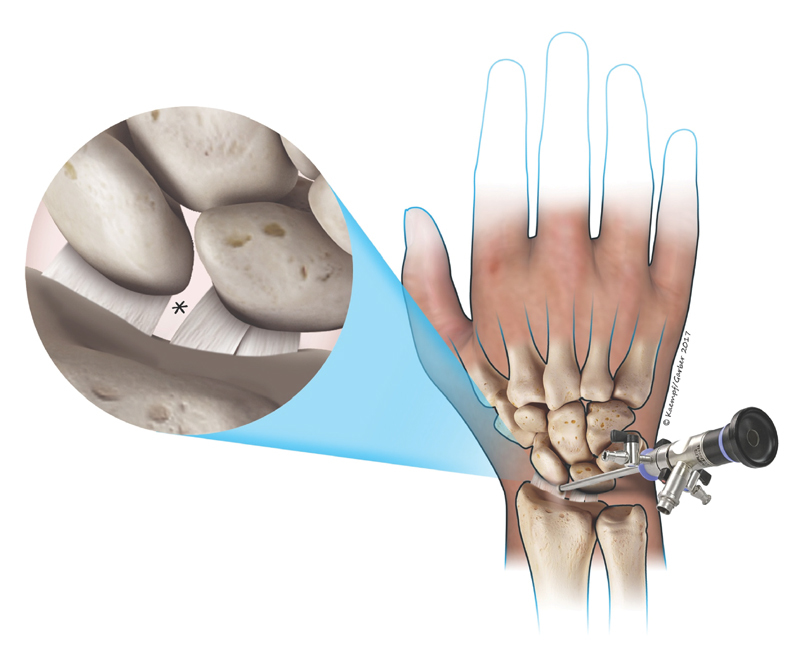
Schematic drawing of the endoscope positioned at the 3/4 portal, facing the gap between the radioscaphocapitate ligament (RSCL) and the long radiolunate ligament (LRLL).
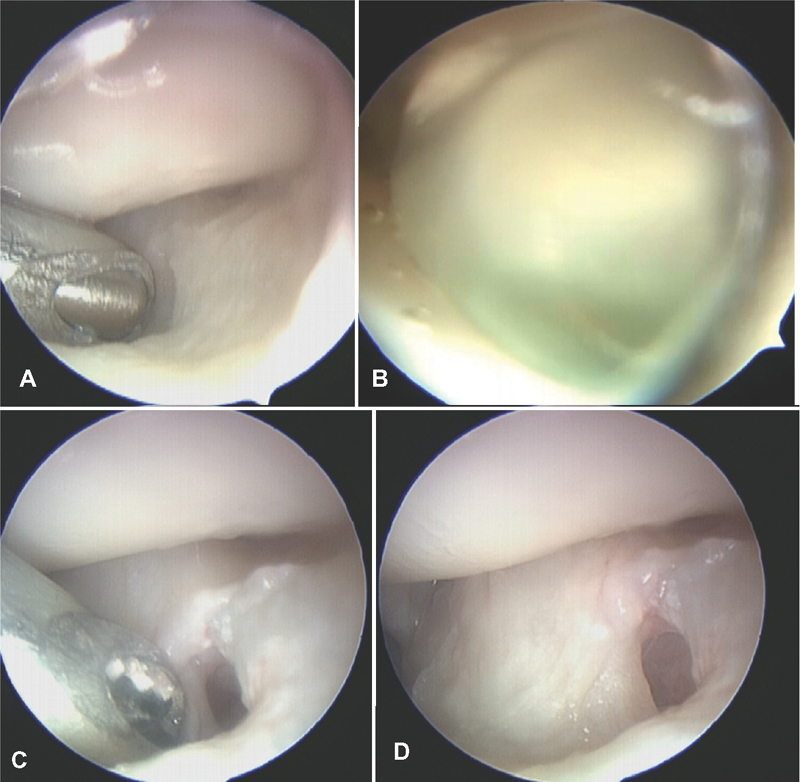
Fig. 5.
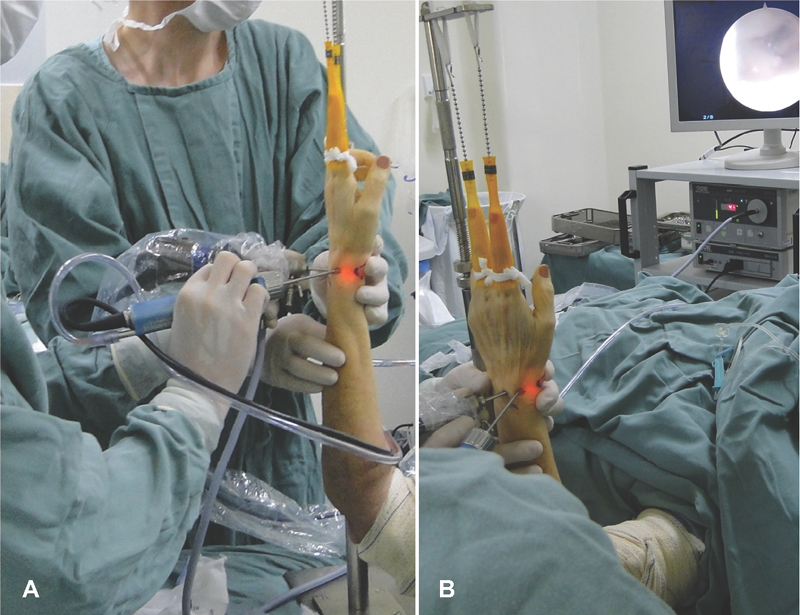
Endoscope positioned at the 3/4 portal, facing the gap between the RSCL and the LRLL), and instrumentation with the soft-tissue shaver positioned at the 1/2 portal ( A ). The location of the pedicle is facilitated by the external manual pressure applied on the cyst ( B ).
Fig. 6.
Soft-tissue shaver between the RSCL and the (LRLL) ( A ). The capsule was perforated, and the cyst mucous content leaks to the joint ( B ). New external pressure on the cyst helps complete the drainage of the contents ( C ). Resection of a 4- to 6-mm portion of the volar capsule, forming a window-shaped defect ( D ).
If radiocarpal arthroscopy reveals no changes, a midcarpal arthroscopy is performed to find the pedicle, which is usually located between the STT ligaments. This procedure is safer and simpler when using a 2.0-mm endoscope and applying traction on the thumb.
One of the authors of the present study uses the technique proposed by Yao and Trindade 13 to facilitate the location of the cyst pedicle. 14 Prior to arthroscopy, the cyst is infiltrated with 2 mL or 3 mL of methylene blue. As such, the whole cyst is tinted by the dye, and intra-articular visualization is made easier. This technique is used occasionally according to the surgeon's preference, and is not routinely adopted by all study authors.
Before the closure of the portals, the tourniquet is released to check the integrity of the vascular bundles. Incision closure is performed with a 5-0 monofilament nylon suture. Dressings with gauze and sterile bandages and a forearm-palmar plaster are used, immobilizing the wrist for a short period until the dressing is changed, which occurs 3 to 7 days after surgery. After this immobilization period, the operated wrist is free to move, and patients are instructed to perform digital pressure and massage over the cyst area to avoid fluid collection, according to the technique described by Ho et al. 8
Patients are followed up weekly at an outpatient facility for one month. In general, they are not submitted to a specific rehabilitation protocol with a hand therapist, being instructed by the medical team to perform stretching, mobility and strength gain exercises at home.
Results
Out of the 21 patients studied, 16 (76%) were female; in 16 (76%), the right side was affected. The average age was 43.6 years, ranging from 18 to 74 years. The average cyst size was 15.4 mm x 16.7 mm, ranging from 9 mm to 30 mm. Other patient data (age, gender, affected side, dominance) are shown in Tables 2 and 3 .
Table 2. Characteristics of the patients and the pathology.
| Identification | Cyst characteristics | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Gender | Age (years) | Dominance | Side | Size (mm) | Preoperative pain | Main complaint | Previous treatment | Lesion time (months) | |
| 1 | F | 42 | R | R | 10 × 9 | 6 | Esthetic + pain | Co | 12 |
| 2 | F | 54 | R | R | 12 × 10 | 7 | Esthetic + pain | Co | 12 |
| 3 | F | 35 | R | R | 15 × 15 | 4 | Esthetic + pain | Co | 12 |
| 4 | M | 20 | R | L | 20 × 20 | 6 | Pain | Co | 12 |
| 5 | F | 37 | R | R | 23 × 20 | 6 | Pain | Co | 10 |
| 6 | M | 64 | R | R | 20 × 30 | 6 | Esthetic + pain | Co | 36 |
| 7 | F | 36 | L | L | 15 × 20 | 4 | Esthetic + pain | Co | 18 |
| 8 | F | 56 | R | R | 10 × 20 | 7 | Esthetic + pain | Co | 12 |
| 9 | F | 36 | L | R | 30 × 30 | 7 | Esthetic + pain | Co | 6 |
| 10 | M | 49 | R | R | 20 × 20 | 6 | Pain | Co | 24 |
| 11 | F | 57 | L | L | 18 × 20 | 6 | Esthetic + pain | Co | 12 |
| 12 | F | 38 | L | L | 20 × 20 | 7 | Esthetic + pain | Co | 18 |
| 13 | M | 23 | R | R | 10 × 10 | 7 | Pain | Co | 12 |
| 14 | F | 74 | R | L | 15 × 15 | 6 | Esthetic + pain | Co | 12 |
| 15 | F | 40 | R | R | 12 × 12 | 8 | Esthetic + pain | Co | 18 |
| 16 | F | 68 | R | L | 16 × 15 | 5 | Esthetic + pain | Co | 12 |
| 17 | F | 63 | R | L | 9 × 10 | 7 | Esthetic + pain | Co | 24 |
| 18 | F | 41 | L | R | 10 × 10 | 4 | Esthetic + pain | Co | 18 |
| 19 | M | 37 | R | R | 15 × 12 | 3 | Esthetic + pain | Co | 18 |
| 20 | F | 18 | R | L | 12 × 18 | 3 | Esthetic + pain | Co | 12 |
| 21 | F | 29 | R | R | 12 × 15 | 3 | Esthetic + pain | Co | 24 |
Abbreviations: Co, conservative; F, female; L, left; M, male; R, right.
Table 3. Arthroscopic procedure and patient follow-up characteristics.
| Arthroscopic procedure | Early assessment | Late assessment | Observations | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Portals | Pedicle location | Procedural time (minutes) | Immobilization time (days) | Complications | Time until final evaluation | Postoperative pain | Outcome evaluation | ||
| 1 | 3/4,1/2, 6R | Between LRLL and RSCL | 60 | 5 | No | 6 | 0 | Good | No |
| 2 | 3/4,1/2 | Between LRLL and RSCL | 60 | 5 | No | 6 | 0 | Good | No |
| 3 | 3/4,1/2, 6R | Between LRLL and RSCL | 40 | 5 | No | 8 | 0 | Good | No |
| 4 | 3,4, 6R | Radial to RSCL | 50 | 12 | No | 7 | 3 | Moderate | Delayed range of motion recovery |
| 5 | 3,4, 6R, MC | Between LRLL and RSCL | 40 | 7 | No | 8 | 0 | Good | No |
| 6 | 3/4, 4/5 | Between LRLL and RSCL | 45 | 5 | No | 8 | 0 | Good | No |
| 7 | 3/4, 4/5, 6R | Between LRLL and RSCL | 40 | 5 | No | 6 | 0 | Good | No |
| 8 | 3/4, 4/5 | Between LRLL and RSCL | 35 | 7 | No | 10 | 0 | Good | No |
| 9 | 3/4, 4/5 | MC | 50 | 7 | No | 18 | 0 | Good | No |
| 10 | 3/4, 4/5 | Between LRLL and RSCL | 30 | 7 | No | 6 | 0 | Good | No |
| 11 | 3/4, 4/5 | Between LRLL and SRLL | 50 | 7 | No | 6 | 0 | Good | Still progressively gaining range of motion |
| 12 | 3/4, 6R | Between LRLL and SRLL | 30 | 7 | No | 14 | 0 | Good | No |
| 13 | 3/4, 4/5, 6R | Between LRLL and SRLL | 45 | 7 | No | 36 | 0 | Good | No |
| 14 | 3/4,1/2, 6R | Between LRLL and RSCL | 20 | 7 | No | 8 | 0 | Good | No |
| 15 | 3/4,1/2, 6R | Between LRLL and RSCL | 30 | 10 | No | 12 | 0 | Good | No |
| 16 | 3/4,1/2, 6R | Between LRLL and RSCL | 35 | 6 | No | 12 | 0 | Good | No |
| 17 | 3/4,1/2, 6R | Between LRLL and RSCL | 20 | 7 | No | 12 | 2 | Good | No |
| 18 | 3/4, 6R | Between LRLL and RSCL | 30 | 7 | No | 14 | 0 | Good | No |
| 19 | 3/4, 6R | Between LRLL and RSCL | 35 | 10 | No | 12 | 0 | Good | No |
| 20 | 3/4,1/2, 6R | Between LRLL and RSCL | 45 | 12 | No | 8 | 0 | Good | No |
| 21 | 3/4, 6R | Between LRLL and RSCL | 50 | 8 | No | 12 | 0 | Good | No |
Abbreviations: RSCL, radioscaphocapitate ligament; LRLL, long radiolunate ligament; SRLL, short radiolunate ligament; MC, midcarpal.
The mean interval between symptom onset and surgery was of 15.9 months, ranging from 12 to 36 months. And the average follow-up time between surgery and the final assessment was of 10.9 months, ranging from 6 to 36 months. Among the 21 patients, 2 (9.6%) still presented mild pain (2 to 3) after cyst removal, which was controlled with medication and physical therapy. Another patient (4.8%) developed paresthesia of the radial nerve sensory branch, which improved spontaneously after 6 weeks. There were no cases of infection, hypertrophic scarring or complex regional pain syndrome.
In total, 20 (95.2%) patients showed complete mobility recovery, with no losses related to the surgical procedure, and 1 (4.8%) patient, whose final evaluation occurred 6 months after surgery, is in rehabilitation with progressive joint movement gain. All measurements were performed according to the standard technique, with the elbow at 90° of flexion and no support of the upper limb on the table. Pain was assessed using an analog scale on a ruler. Preoperatively, the average pain was 5.6, ranging from 3 to 8. Postoperatively, the average pain was 0.2, ranging from 0 to 3.
The results were classified following the criteria presented by Rocchi et al; 1 19 (90.4%) were deemed good, 1 (4.8%) was moderate, and 1 (4.8%) was considered bad.
Only 1 (4.8%) patient ( Tables 2 and 3 , patient #2) presented increased cyst site volume during the immediate postoperative period, with complete resolution after manual pressure and daily massage.
In total, 19 (90.4%) patients were very satisfied, and 2 (9.6%) were satisfied with the procedure, according to the simple choice of method previously explained.
Discussion
Synovial cyst is a common benign tumor of the wrist. Even though the treatment is predominantly conservative, 15 some patients require surgery. Different surgical procedures are proposed, and there is no consensus regarding which technique is best. Most procedures are based on the concept that it is not necessary to remove the entire cyst, but rather drain its contents through an opening at the pedicle. This decreases the risk of injury recurrence. 2 4 8 Volar and dorsal cysts can be treated through open surgery. However, palmar incisions present a higher risk of complications due to the proximity to the palmar superficial branch of the radial artery, flexor tendons, superficial terminal branches of the median nerve and cutaneous palmar branch of the median nerve. 1 9 In a review, Yao and Trindade 13 reported a 20% overall recurrence rate of dorsal cysts subjected to open procedures, in addition to preliminary indications of lower incidence for arthroscopic procedures. Osterman and Raphael, 7 in their series about dorsal cysts, did not observe any recurrence. Ho et al, 2 in their series of 21 cases of arthroscopically-treated volar cysts, observed two cases of recurrence.
There is no study comparing the results of open and video-assisted surgeries in the treatment of volar cysts. Studies in dorsal cysts show similar recurrence rates and risk of complications; however, complications from open surgeries are more severe. 1 9 Arthroscopic resection was developed for intra-articular cyst removal, reducing the risk of neurovascular complications and the incidence of stiffness and hypertrophic scarring. 1 Our results with the arthroscopic treatment of volar synovial cysts show that this is a safe technique with a low complication rate, with no cases of recurrence or tendon injury in our sample. Since the main indication for surgery was for esthetic reasons (in 17 [80.9%] out of 21 patients), a minimally-invasive technique is warranted, leading to the formation of a smaller scar. In addition, this technique has the advantage of resulting in lower levels of postoperative pain, rapid return to work, and lower incidence of complications. It is also assumed that the minor surgical trauma inherent to the arthroscopic technique results in lower levels of postoperative pain and a quick return to work.
Although the arthroscopic treatment of dorsal cysts is well-defined and widespread, there are few series on volar cysts. Ho et al 8 first described the technique and initially analyzed six patients, achieving good results in five of them. In their study, arthroscopy was converted to open resection in a patient with a midcarpal cyst. Subsequently, with a larger series of 21 patients, the symptoms improved in all cases. 2
Ho et al 2 8 also pointed out that some cases formerly considered early cyst recurrences were actually due to hematoma and synovial fluid remnants within the cyst. This initial swelling must be treated with manual pressure and external massage directly over the original cyst site, draining the remaining contents into the joint. Therefore, these authors emphasize the importance of a short postoperative immobilization time in patients undergoing arthroscopic resections.
Rocchi et al, 9 in a series with 20 patients, had good results in 18 individuals, in addition to 1 case of relapse and 1 case of neuropraxia. Their results were worse when the pedicle was located at the midcarpal joint, since the joint space and pedicle are smaller. Furthermore, unlike radiocarpal volar cysts, midcarpal cysts are more superficial and present no risk of vascular or nervous injury during their open resection, thus diminishing the advantage of the video-assisted procedure. These authors claim that midcarpal volar cysts must be treated openly. As such, our sample consisted only of cysts of radiocarpal origin, as determined by a previous nuclear magnetic resonance imaging scan or by its location proximal to the wrist flexion fold.
Mathoulin et al 4 treated arthroscopically 32 patients with volar cysts, obtaining 100% of good results, with no recurrences in an average follow-up period of 26 months. These authors did not report midcarpal cysts in their series. More recently, Mathoulin and Gras 16 published a review article on the arthroscopic treatment of wrist dorsal and volar cysts, showing favorable results over conventional open surgery regarding recurrence risk, cosmesis, and risk of neurovascular and ligamentous injury.
Yao and Trindade 13 described the use of direct methylene blue infiltration for cases in which finding the cyst pedicle is difficult. This procedure was successfully used by one of the authors (GM) of the present study, and the blue tint provided by the dye is a guide to find the cyst pedicle during arthroscopy, facilitating its resection.
It is important to emphasize the cost of the procedure, since specific arthroscopy materials for small joints are required. Pang et al 5 compared the cost of the open and arthroscopic procedure for the resection of wrist synovial cysts, whether dorsal or volar, and found an average cost of US$ 1,821 for the open approach, and of US$ 3,668 for the arthroscopic approach. Therefore, the cost of the material used for arthroscopy should be considered at the moment of surgery indication. Because this is a mostly economically active population, this initial outlay can be offset by a faster return to work.
We have already emphasized in earlier studies 17 that arthroscopy in small joints must be performed by experienced, properly-trained physicians. 17 Before using this technique, the study of it in cadavers is recommended to avoid the risks of complications and iatrogenic articular injuries. This procedure is technically challenging, and the learning curve must be respected. The limitations of the present study lie on its retrospective nature, with a small series and a moderate follow-up period. A new prospective study is underway to compare patients undergoing open and arthroscopic techniques with a larger sample and longer follow-up period.
The use of arthroscopic techniques for the treatment of dorsal cysts is widespread. 1 4 5 6 13 18 19 20 21 22 The present work shows good results; in addition, compared to the classic open technique, this is also a good option for volar cysts. It is a reproducible and safe technique that leads to satisfactory results. Provided the technique is performed correctly, intracapsular resection offers few risks to the tendons and neurovascular bundles, as shown in our study, in which there were no complications of such nature. It is a minimally-invasive procedure with low morbidity and few complications and relapses – in fact, there were none in our sample. The arthroscopic cyst treatment was successful, resulting in a short immobilization time, early return to work, rapid functional recovery and high satisfaction rates, as demonstrated by the present study. Considering the cost and the learning curve, this technique proved to be a good alternative to the open technique. The analysis of the study results summarized in Tables 2 and 3 shows several benefits, especially the efficacy and safety of this treatment for wrist volar cysts.
Conclusion
The arthroscopic resection of volar synovial cysts was a useful and safe technique in this series of cases, becoming a good alternative to the open technique because it is a minimally-invasive procedure with few complications.
Agradecimentos
Os autores gostariam de agaradecer à artista Renata Ribak pela autoria da Figura 6 .
Fig. 6.
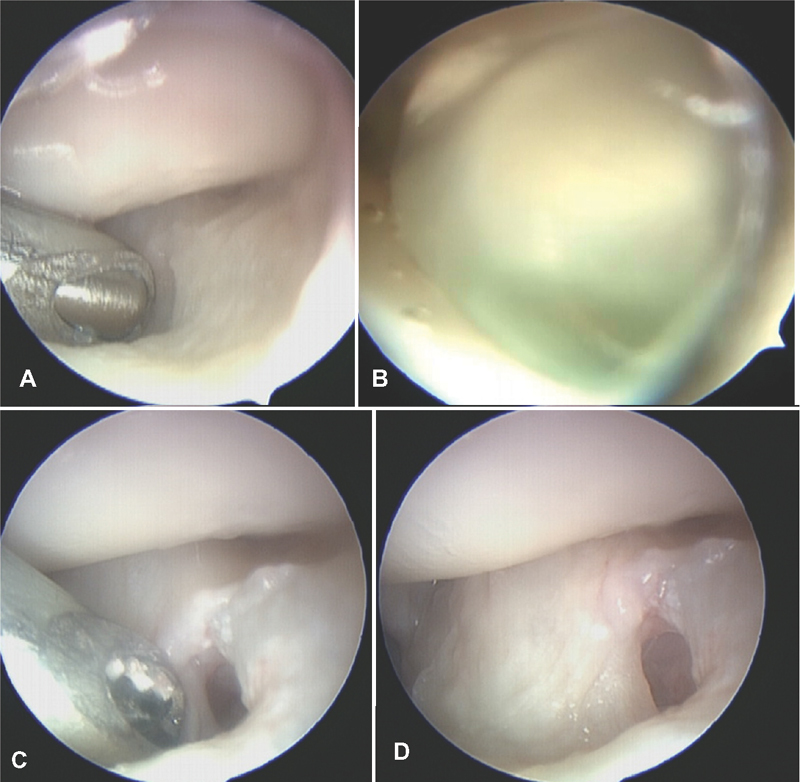
Shaver de partes moles no intervalo entre o LREC e o LRSL ( A ). Cápsula perfurada extravasando o conteúdo mucoso do cisto dentro da articulação ( B ). Nova pressão externa sobre o cisto ajuda na drenagem completa do seu conteúdo ( C ). Ressecção de uma porção de 4 a 6 mm da cápsula volar, formando um defeito em forma de janela ( D ).
Acknowledgment
The authors would like to thank visual artist Renata Ribak for drawing Figure 6 .
Conflito de Interesses Os autores declaram não haver conflito de interesses .
Trabalho feito na Santa Casa de Misericórdia de Porto Alegre e no Hospital Mãe de Deus, Porto Alegre, RS, Brasil.
Work performed at Santa Casa de Misericórdia de Porto Alegre and Hospital Mãe de Deus, Porto Alegre, RS, Brazil.
Referências
- 1.Rocchi L, Canal A, Fanfani F, Catalano F. Articular ganglia of the volar aspect of the wrist: arthroscopic resection compared with open excision. A prospective randomised study. Scand J Plast Reconstr Surg Hand Surg. 2008;42(05):253–259. doi: 10.1080/02844310802210897. [DOI] [PubMed] [Google Scholar]
- 2.Ho P C, Law B K, Hung L K. Arthroscopic Volar Wrist Ganglionectomy. Chir Main. 2006;25S1:S221–S230. doi: 10.1016/j.main.2006.07.028. [DOI] [PubMed] [Google Scholar]
- 3.Zaidenberg C R, Clembosky G A, Perrotto C J, Muratore A J. Resección artroscópica de los gangliones palmares del borde radial de la muñeca. Rev Argent Artosc. 2003;10(01):13–17. [Google Scholar]
- 4.Mathoulin C, Hoyos A, Pelaez J. Arthroscopic resection of wrist ganglia. Hand Surg. 2004;9(02):159–164. doi: 10.1142/s0218810404002169. [DOI] [PubMed] [Google Scholar]
- 5.Pang E Q, Zhang S, Harris A HS, Kamal R N. Cost Minimization Analysis of Ganglion Cyst Excision. J Hand Surg Am. 2017;42(09):7500–7.5E6. doi: 10.1016/j.jhsa.2017.05.012. [DOI] [PubMed] [Google Scholar]
- 6.Monaghan B A. Uses and abuses of wrist arthroscopy. Tech Hand Up Extrem Surg. 2006;10(01):37–42. doi: 10.1097/00130911-200603000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Osterman A L, Raphael J. Arthroscopic resection of dorsal ganglion of the wrist. Hand Clin. 1995;11(01):7–12. [PubMed] [Google Scholar]
- 8.Ho P C, Lo W N, Hung L K. Arthroscopic resection of volar ganglion of the wrist: A new technique. Arthroscopy. 2003;19(02):218–221. doi: 10.1053/jars.2003.50035. [DOI] [PubMed] [Google Scholar]
- 9.Rocchi L, Canal A, Pelaez J, Fanfani F, Catalano F.Results and complications in dorsal and volar wrist Ganglia arthroscopic resection Hand Surg 200611(1-2):21–26. [DOI] [PubMed] [Google Scholar]
- 10.Yamamoto M, Kurimoto S, Okui N, Tatebe M, Shinohara T, Hirata H. Sonography-assisted arthroscopic resection of volar wrist Ganglia: a new technique. Arthrosc Tech. 2012;1(01):e31–e35. doi: 10.1016/j.eats.2011.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fernandes C H, Miranda C D, Dos Santos J B, Faloppa F. A systematic review of complications and recurrence rate of arthroscopic resection of volar wrist ganglion. Hand Surg. 2014;19(03):475–480. doi: 10.1142/S0218810414300046. [DOI] [PubMed] [Google Scholar]
- 12.Sawyer G A, DaSilva M F, Akelman E. Volar wrist ganglion excision through the flexor carpi radialis sheath. Tech Hand Up Extrem Surg. 2012;16(03):145–147. doi: 10.1097/BTH.0b013e31825ae1ba. [DOI] [PubMed] [Google Scholar]
- 13.Yao J, Trindade M C. Color-aided visualization of dorsal wrist ganglion stalks aids in complete arthroscopic excision. Arthroscopy. 2011;27(03):425–429. doi: 10.1016/j.arthro.2010.10.017. [DOI] [PubMed] [Google Scholar]
- 14.Ahsan Z S, Yao J. Arthroscopic dorsal wrist ganglion excision with color-aided visualization of the stalk: minimum 1-year follow-up. Hand (N Y) 2014;9(02):205–208. doi: 10.1007/s11552-013-9570-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pardini A G, Junior, Freitas A D, Gusmão Filho N S. História natural do quisto sinovial do dorso do punho. Rev Bras Ortop. 1998;33(03):199–201. [Google Scholar]
- 16.Mathoulin C, Gras M. Arthroscopic Management of Dorsal and Volar Wrist Ganglion. Hand Clin. 2017;33(04):769–777. doi: 10.1016/j.hcl.2017.07.012. [DOI] [PubMed] [Google Scholar]
- 17.Oliveira R K, Praetzel R P, Bayer L R, Delgado P J. Artroscopia e osteotomia extensora do primeiro metacarpo para tratamento da rizartrose nos estágios iniciais. Rev Bras Ortop. 2016;51 01:S24–S31. [Google Scholar]
- 18.Chloros G D, Wiesler E R, Poehling G G. Current concepts in wrist arthroscopy. Arthroscopy. 2008;24(03):343–354. doi: 10.1016/j.arthro.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 19.Chung S R, Tay S C. Audit of Clinical and Functional Outcomes of Arthroscopic Resection of Wrist Ganglions. Hand Surg. 2015;20(03):415–420. doi: 10.1142/S0218810415500331. [DOI] [PubMed] [Google Scholar]
- 20.Atzei A, Luchetti R, Sgarbossa A, Carità E, Llusà M. [Set-up, portals and normal exploration in wrist arthroscopy] Chir Main. 2006;25 01:S131–S144. doi: 10.1016/j.main.2006.07.029. [DOI] [PubMed] [Google Scholar]
- 21.Ahsan Z S, Yao J. Complications of wrist arthroscopy. Arthroscopy. 2012;28(06):855–859. doi: 10.1016/j.arthro.2012.01.008. [DOI] [PubMed] [Google Scholar]
- 22.Chen A C, Lee W C, Hsu K Y, Chan Y S, Yuan L J, Chang C H. Arthroscopic ganglionectomy through an intrafocal cystic portal for wrist ganglia. Arthroscopy. 2010;26(05):617–622. doi: 10.1016/j.arthro.2009.08.021. [DOI] [PubMed] [Google Scholar]