Abstract
Background and Objectives.
Although trauma research/therapy primarily focuses on traumatic memories, recent evidence indicates positive memory processes play a role in the etiology/maintenance of posttraumatic stress disorder (PTSD) symptom severity. We examined the effects of a novel positive memory processing technique on PTSD symptom severity, depression symptom severity, affect, posttrauma cognitions, and self-esteem.
Methods.
Sixty-five trauma-exposed participants were randomly assigned to one of three conditions (narrating/processing vs. writing/processing two specific positive memories, time-matched control) and completed self-report measures pre- and post-task (T0). About one week later, participants repeated their assigned task condition and completed self-report measures (T1). We conducted mixed ANOVAs to examine the impact of the technique on study variables over time.
Results.
The narrating condition had significant decreases in PTSD symptom severity, posttrauma cognitions, and negative affect from T0 pre-task to T1 post-task; and significant increases in positive affect from T0 pre-to-post-task and from T1 pre-to-post-task. The writing condition had significant increases in positive affect from T0 pre-to-post-task, but a significant decrease from T0 post-task to T1 post-task; and significant decreases in negative affect from T0 pre-to-post-task with an increase from T0 post-task to T1 post-task.
Limitations.
Use of self-report measures, non-clinical convenience sample with less gender/ethnic/racial diversity, small sample size, methodological differences in time frames for measures, and no examination of follow-up effects.
Conclusions.
Narrating and processing specific positive memories had a beneficial impact on PTSD symptom severity, posttrauma maladaptive cognitions, and affect; such results provide an impetus to examine positive memory interventions in trauma clinical work.
Keywords: Processing positive memories, PTSD symptom severity, post-trauma mental health, trauma-exposed college students, non-clinical sample
1. Introduction
Trauma-exposed individuals may experience symptoms of posttraumatic stress disorder (PTSD), including intrusive trauma-related thoughts/memories, avoidance of trauma reminders, negative alterations in cognitions and mood (NACM), and alterations in arousal and reactivity (AAR; American Psychiatric Association, 2013). Conceptualizing PTSD as a memory encoding- and retrieval-based disorder, trauma theorists have highlighted understanding and addressing traumatic and positive memories among individuals with PTSD symptoms (Brewin, 2014; Ehlers & Clark, 2000; Foa & Kozak, 1986; Horowitz, 1986; Rubin, Berntsen, & Bohni, 2008). Recent evidence indicates that positive memories and related processes also may influence the etiology (e.g., De Quervain et al., 2012; Hauer, Wessel, Engelhard, Peeters, & Dalgleish, 2009) and/or maintenance (e.g., Porter & Peace, 2007) of PTSD symptom severity. In fact, recent work demonstrated that the number of specific positive memories individuals were able to recall was negatively associated with PTSD symptom severity, self-blame, and positive affect; while individuals’ ease in recalling details of positive memories was negatively associated with PTSD symptom severity, negative cognitions about self, and negative affect (Contractor, Banducci, Dolan, Keegan, & Weiss, 2019). Indeed, individuals with PTSD symptoms have difficulty accessing autobiographical (Bryant, Sutherland, & Guthrie, 2007; Nixon, Ball, Sterk, Best, & Beatty, 2013; Sutherland & Bryant, 2008) and specific positive memories (McNally, Lasko, Macklin, & Pitman, 1995; McNally, Litz, Prassas, Shin, & Weathers, 1994). Despite the theoretical support and empirical evidence linking PTSD symptom severity to positive memories (Contractor, Brown, et al., 2018) and interest/willingness to therapeutically focus on positive memories by trauma-exposed clients (Caldas, Jin, Dolan, Dranger, & Contractor, in press), current trauma research and clinical work primarily targets traumatic memories (e.g., Bernsten & Rubin, 2007; Schnurr, 2017).
To address this gap, Contractor and colleagues (2018) proposed a conceptual model to outline hypothesized mechanisms underlying the effect of positive memory processing on PTSD symptom severity and related post-trauma outcomes (affect, cognitions, and memory specificity). Therapeutically, focusing on positive memories may serve as a mood regulation strategy by reducing an over-focus on negative memories and increasing attention to positive memories and related content (Joormann, Siemer, & Gotlib, 2007; Quoidbach, Mikolajczak, & Gross, 2015; Rusting & DeHart, 2000). This enhanced positive affect and reduced negative affect, in turn, may augment health-protective biological responses, positive health behaviors, adaptive coping, better mental health (reviewed in Fredrickson, 2000; Lyubomirsky, King, & Diener, 2005; Steptoe, Dockray, & Wardle, 2009), positive interpretations of events (Blaney, 1986; Rusting & DeHart, 2000), self-esteem (Steel et al., 2015), and positive content in thoughts (broaden-and-build theory; Fredrickson, 2001). Consistent with these findings, research indicates that integration of a positive memory focus within certain interventions positively influences PTSD severity (Moradi et al., 2014; Sutherland & Bryant, 2007; Tarrier, 2010). However, no study has examined the specific mechanisms underlying the effects of positive memory processing on PTSD symptom severity; such information could aid the development of a PTSD-specific positive memory therapeutic technique.
Addressing this empirical gap, the current study examined the effects of processing positive memories on post-trauma mental health among a non-clinical sample of trauma-exposed college students. Drawing from the Contractor, Brown, et al. (2018) model, processing of positive memories was conceptualized as (1) recalling (Arditte Hall, De Raedt, Timpano, & Joormann, 2018), (2) writing (Burton & King, 2004) or narrating (drawing from trauma-focused treatments; Foa, 2011; Foa & Kozak, 1986) two different specific (experiences that occurred within a 24-hour period of time; Williams & Broadbent, 1986) positive event memories, and (3) identifying thoughts, feelings, values, strengths, and importance related to each positive memory. Narrating a memory, one of the important activities of rehearsal (Smorti & Fioretti, 2016), is associated with self-concept development, especially when the memory is self-relevant and has altered one’s sense of self in a critical manner (McLean, Pasupathi, & Pals, 2007). In fact, repeated narrating of a positive memory may help to refine details, give it meaning and coherence, and increase the longitudinal continuity of that recollection (Conway, 1997; McAdams et al., 2006). Writing about positive experiences is significantly associated with long-term positive mood (Burton & King, 2004) and physical and emotional health benefits (King, 2001). Further, identifying positive values, affect, strengths, and thoughts related to a memory may solidify and render them integral to one’s identity (Contractor, Brown, et al., 2018; Hitlin, 2003; King, Hicks, Krull, & Del Gaiso, 2006).
We specifically examined the effects of processing positive memories via different methodologies on PTSD symptom severity, depression symptom severity, affect, and cognitions (including self-esteem). We hypothesized that individuals participating in the conditions of positive memory processing (narrating and writing each), as compared to those in the control condition, would experience significant reductions in PTSD symptom severity (Contractor, Brown, et al., 2018) and depression symptom severity (Arditte Hall et al., 2018; McNally et al., 1994; Neshat-Doost et al., 2013), given its comorbidity with PTSD symptom severity (Bonde et al., 2016; Rytwinski, Scur, Feeny, & Youngstrom, 2013), as well as negative affect (Joormann et al., 2007; Josephson, 1996; Rusting & DeHart, 2000) and maladaptive cognitions (Blaney, 1986; Fredrickson, 2001; Rusting & Larsen, 1998), Further, we hypothesized that individuals participating in the conditions of positive memory processing (narrating and writing each), as compared to those in the control condition, would experience a significant increase in positive affect (Joormann et al., 2007; Josephson, 1996; Rusting & DeHart, 2000) and self-esteem (Korrelboom, de Jong, Huijbrechts, & Daansen, 2009; Korrelboom, Maarsingh, & Huijbrechts, 2012; Korrelboom, Marissen, & van Assendelft, 2011). Broadly, the writing and narrating conditions were compared to each other, and independently to the control (no processing) condition. Lastly, we hypothesized that the writing and narrating conditions would not differ in their impact on assessed post-trauma indicators based on research indicating beneficial impacts of both processing methodologies for trauma treatment (Foa et al., 2018; Sloan, Marx, Bovin, Feinstein, & Gallagher, 2012).
2. Methods
2.1. Procedure and Participants
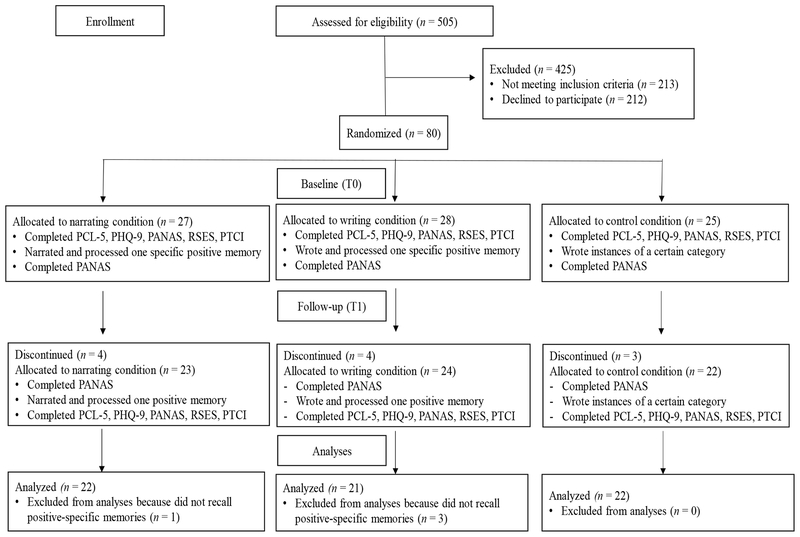
The study was approved by a [redacted] Institutional Review Board. We recruited a non-clinical sample of students through the University’s psychology research participation portal (SONA system). The study was described as an examination of the relation between stressful life experiences, emotional distress, and positive memories. The three phases of the study are described below (see Figure 1).
Figure 1.
Recruitment, Retention, and Procedural Information of the Study Phases
Note. PCL-5 is PTSD Checklist for DSM-5; PHQ-9 is Patient Health Questionnaire-9; PANAS is Positive and Negative Affect Schedule; RSES is Rosenberg Self-Esteem Scale; PTCI is Posttraumatic Cognitions Inventory.
2.1.1. Screening Phase.
All participants provided informed consent prior to participation. Participants were assessed for inclusion criteria: age 18 years and older, working knowledge of the English language, endorsing a traumatic event (first item of the Primary Care PTSD Screen for DSM-5; Prins et al., 2015; Prins et al., 2016), and not endorsing a “no trauma” option on the Life Events Checklist for DSM-5 (LEC-5; Weathers et al., 2013). Participants who completed the screening phase received one course credit.
2.1.2. Baseline Phase (T0).
Eligible participants first completed pre-task questionnaires on Qualtrics (Qualtrics, 2018): demographic survey, PTSD Checklist for DSM-5 (PCL-5; Weathers et al., 2013), Patient Health Questionnaire-9 (PHQ-9; Kroenke, Spitzer, & Williams, 2001), Positive and Negative Affect Schedule (PANAS; Watson, Clark, & Tellegen, 1988), Posttraumatic Cognitions Inventory (PTCI; Foa, Ehlers, Clark, Tolin, & Orsillo, 1999), and Rosenberg Self-Esteem Scale (RSES; Rosenberg, 1965; Rosenberg, 1979). Next, participants were randomly assigned to time-matched (30-minutes) conditions (i.e., writing/processing a specific positive memory, narrating/processing a specific positive memory, or control). In the “writing” condition, trained research assistants provided scripted instructions to each participant to process a specific positive memory and participants typed their recollections into a laboratory computer. In the “narrating” condition, trained research assistants followed a script asking participants to narrate and process a specific positive memory (audio-recorded). Instructions for the “writing” and “narrating” conditions were adapted from prior studies (Boyacioglu & Akfirat, 2015; Janssen, Hearne, & Takarangi, 2015; Sutin & Robins, 2007; Williams & Broadbent, 1986). See Appendix A for the instructions given to participants to narrate/write and process a specific positive memory. In the “control” condition, participants typed the maximum number of examples they could think of in response to provided categories on a computer. Examples of provided categories included trees, fruits, flowers, four-footed animals, countries, body parts, birds, sports, colors, articles of furniture, liquids, and things that fly (Van Overschelde, Rawson, & Dunlosky, 2004). It was emphasized that participants were to do their best for each category and that they did not have to complete all tasks (i.e., give responses to all provided categories). Post-task, participants in all conditions completed the PANAS. They received three course credits for completing T0, which spanned approximately one and a half hours.
2.1.3. Follow-up phase (T1).
The follow-up appointment was scheduled six to eight days from the T0 completion. At pre-task, participants again provided informed consent and completed the PANAS on Qualtrics (Qualtrics, 2018). Next, they participated in the same condition (writing, narrating, or control) as they did during baseline. Notably, participants in the narrating and writing conditions discussed a positive memory that was different from what they discussed at T0. Post-task, participants in all conditions completed the PCL-5, PHQ-9, PANAS, PTCI, and RSES. Participants received three course credits for completing T1, which spanned approximately one hour.
2.2. Exclusions, Missing Data, and Sample Characteristics
See Figure 1 for a diagrammatic representation of recruitment and retention numbers, and procedural information for the study phases. Among the 505 participants who completed the screening phase, 292 participants (57.82%) were eligible for the study. Among these 292 eligible participants, 80 participants (27.40% of eligible participants) completed the baseline (T0) phase and 69 participants (23.63% of eligible participants) also completed the follow-up (T1) phase. From this sample of 69 participants completing both T0 and T1, we excluded four participants who did not follow instructions to recall positive and specific memories (writing and narrating conditions) across any/both time points (see Memory Coding section for additional information). The final sample, thus, included 65 participants (Mage = 22.52 years, SD = 4.78; 54 women and 11 men). This sample size was considered adequate based on the a priori power analyses conducted with the GPower program (Faul, Erdfelder, Lang, & Buchner, 2007). To detect medium effects (partial eta square [partial η2] = .06 parallel to effect size f = .25; Cohen, 1988) with 80% power and at an alpha set to .05, a sample of 42 individuals was needed for a mixed between-within subjects ANOVA analyzing three groups and two time points, and a sample of 30 individuals was needed for a mixed between-within subjects ANOVA analyzing three groups and four time points. No prior study has examined a similar research question making it difficult to hypothesize a certain effect size estimate; we chose a medium effect size estimate for power analyses to ensure clinical meaning.
In the final sample of 65 participants, missing data was minimal, with only one participant (control condition) missing two items (one item each on the T1 pre- and post-task PANAS measures). We aimed to exclude individuals missing >30% data on any measure of interest to ensure that any applied missing data imputation/estimation had sufficient existing data (Graham, 2009; Schafer & Graham, 2002); no participants were missing >30% data on any primary measure. The final sample for the narrating, writing, and control conditions included 22, 21, and 22 participants, respectively. Detailed demographic and psychopathology information is provided in Table 1. Results of point-biserial correlations indicated that demographic variables of age, gender, years of schooling, relationship status, income, ethnicity, and employment status were not significantly associated with any outcome variables (rpb = −.002 to .20; p = .990 - .135).
Table 1.
Demographic and Psychopathology Information for the Entire Sample and Three Subsamples.
| Full Sample (n = 65) | Writing Condition (n = 21) | Narrating Condition (n = 22) | Control Condition (n = 22) | |
|---|---|---|---|---|
| Mean (SD) | ||||
| Age | 22.52 (4.78) | 22 (2.88) | 22.55 (4.85) | 23 (6.15) |
| Years of schooling | 14.18 (1.68) | 14 (1.41) | 14.18 (1.84) | 14.36 (1.79) |
| T0 pre-task PTSD symptom severity | 23.92 (18.33) | 23.90 (18.58) | 24.68 (20.58) | 23.18 (16.44) |
| T1 post-task PTSD symptom severity | 19.97 (16.30) | 23 (18.07) | 15.68 (15.66) | 21.36 (14.94) |
| T0 pre-task depression symptom severity | 7.86 (5.41) | 8.52 (5.74) | 7.68 (5.54) | 7.41 (5.15) |
| T1 post-task depression symptom severity | 7.98 (5.61) | 9.67 (6.40) | 6.86 (5.43) | 7.50 (4.81) |
| T0 pre-task negative affect | 16.52 (5.88) | 17.71 (6.52) | 16.36 (5.21) | 15.55 (5.94) |
| T0 post-task negative affect | 14.12 (5.25) | 13.24 (4.05) | 14.77 (5.85) | 14.32 (5.74) |
| T1 pre-task negative affect | 14.46 (4.53) | 15.57 (4.24) | 13.55 (3.81) | 14.32 (5.37) |
| T1 post-task negative affect | 14.77 (6.11) | 16 (7.01) | 13.23 (4.33) | 15.14 (6.59) |
| T0 pre-task maladaptive cognitions | 105.32 (46.50) | 116.67 (55.37) | 102.86 (48.59) | 96.95 (38.82) |
| T1 post-task maladaptive cognitions | 102.28 (44.41) | 104.67 (43.43) | 98.64 (47.82) | 103.64 (43.67) |
| T0 pre-task positive affect | 22.25 (8.88) | 23.86 (7.79) | 21.82 (8.99) | 21.14 (9.89) |
| T0 post-task positive affect | 25.58 (10.23) | 30 (8.53) | 25.18 (10.55) | 21.77 (10.16) |
| T1 pre-task positive affect | 22.97 (9.43) | 24.10 (7.56) | 21.82 (10.72) | 23.05 (9.94) |
| T1 post-task positive affect | 22.17 (9.95) | 22.29 (7.89) | 23.50 (11.25) | 20.73 (10.56) |
| T0 pre-task self-esteem | 27.52 (6.73) | 27.38 (7.28) | 28.09 (7.30) | 27.09 (5.81) |
| T1 post-task self-esteem | 28.06 (6.62) | 27.14 (7.15) | 29.23 (7.03) | 27.77 (5.74) |
| n (% of total sample)* | ||||
| Gender | ||||
| Female | 54 (83.10) | 15 (71.40) | 18 (81.80) | 21 (95.50) |
| Male | 11 (16.90) | 6 (28.60) | 4 (18.20) | 1 (4.50) |
| Other | 0 | 0 | 0 | 0 |
| Employment Status | ||||
| Part time | 24 (36.90) | 12 (57.10) | 6 (27.30) | 6 (27.30) |
| Full time | 9 (13.80) | 1 (4.80) | 6 (27.30) | 2 (9.10) |
| Unemployed | 4 (6.20) | 0 (0) | 0 (0) | 4 (18.20) |
| Unemployed Student | 28 (43.10) | 8 (38.10) | 10 (45.50) | 10 (45.50) |
| Retired | 0 | 0 | 0 | 0 |
| Relationship Status | ||||
| Single | 43 (66.20) | 15 (71.40) | 15 (68.20) | 13 (59.10) |
| Living with significant other | 14 (21.50) | 4 (19) | 5 (22.70) | 5 (22.70) |
| Married | 7 (10.80) | 2 (9.50) | 2 (9.10) | 3 (13.60) |
| Divorced, separated, or widowed | 1 (1.50) | 0 | 0 (0) | 1 (4.50) |
| Racial Status | ||||
| White/Caucasian | 48 (82.80) | 18 (85.70) | 16 (88.90) | 14 (73.70) |
| African American/Black | 11 (26.20) | 0 (0) | 6 (33.30) | 5 (38.50) |
| Asian | 3 (8.30) | 0 (0) | 1 (7.70) | 2 (16.70) |
| American Indian or Alaskan Native | 6 (15.40) | 0 (0) | 4 (26.70) | 2 (15.40) |
| Native Hawaiian/other Pacific Islander | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Unknown | 4 (11.40) | 1 (9.10) | 2 (15.40) | 1 (9.10) |
| Ethnicity | ||||
| Hispanic or Latino | 17 (26.20) | 7 (33.30) | 5 (22.70) | 5 (22.70) |
| Not Hispanic or Latino | 48 (73.80) | 14 (66.70) | 17 (77.30) | 17 (77.30) |
| Income | ||||
| Less than $15,000 | 12 (18.80) | 5 (23.80) | 4 (19) | 3 (13.60) |
| $15,000 - $24,999 | 10 (15.60) | 4 (19) | 4 (19) | 2 (9.10) |
| $25,000 - $34,999 | 9 (14.10) | 1 (4.80) | 4 (19) | 4 (18.20) |
| $35,000 - $49,999 | 10 (15.60) | 5 (23.80) | 1 (4.80) | 4 (18.20) |
| $50,000 - $64,999 | 7 (10.90) | 3 (14.30) | 2 (9.50) | 2 (9.10) |
| $65,000 - $79,999 | 5 (7.80) | 1 (4.80) | 2 (9.50) | 2 (9.10) |
| $80,000 and higher | 11 (17.20) | 2 (9.50) | 4 (19) | 5 (22.70) |
| Traumas Endorsed on the LEC-5 | ||||
| Natural disaster | 47 (72.30) | 17 (81) | 12 (54.50) | 18 (81.80) |
| Fire or explosion | 31 (47.70) | 13 (61.90) | 8 (36.40) | 10 (45.50) |
| Transportation accident | 51 (78.50) | 20 (95.20) | 15 (68.20) | 16 (72.70) |
| Serious accident at work, home, or during recreational activity | 33 (50.80) | 12 (57.10) | 10 (45.50) | 11 (50) |
| Exposure to toxic substance | 19 (29.20) | 7 (33.30) | 2 (9.10) | 10 (45.50) |
| Physical assault | 47 (72.30) | 17 (81) | 15 (68.20) | 15 (68.20) |
| Assault with a weapon | 36 (55.40) | 14 (66.70) | 9 (40.90) | 13 (59.10) |
| Sexual assault | 42 (64.60) | 17 (81) | 12 (54.50) | 13 (59.10) |
| Other unwanted or uncomfortable sexual experience | 48 (73.80) | 16 (76.20) | 16 (72.70) | 16 (72.70) |
| Combat or exposure to a war-zone | 23 (35.40) | 11 (52.40) | 5 (22.70) | 7 (31.80) |
| Captivity (being kidnapped, abducted, held hostage) | 17 (26.20) | 7 (33.30) | 3 (13.60) | 7 (31.80) |
| Life threatening illness or injury | 42 (64.60) | 14 (66.70) | 15 (68.20) | 13 (59.10) |
| Severe human suffering | 23 (35.40) | 8 (38.10) | 7 (31.80) | 8 (36.40) |
| Sudden violent death | 39 (60) | 16 (76.20) | 12 (54.50) | 11 (50) |
| Sudden accidental death | 36 (55.40) | 16 (76.20) | 8 (36.40) | 12 (54.50) |
| Serious injury, harm, or death you caused to someone | 11 (16.90) | 2 (9.50) | 5 (22.70) | 4 (18.20) |
| Other stressful event or experience | 37 (56.90) | 13 (61.90) | 11 (50) | 13 (59.10) |
| Probable PTSD (score ≥31 on the PTSD Checklist for DSM-5 administered at T0 pre-task) | ||||
| 20 (30.80) | 7 (33.30) | 6 (27.30) | 7 (31.80) | |
| Probable PTSD (score ≥31 on the PTSD Checklist for DSM-5 administered at T1 post-task) | ||||
| 17 (26.20) | 7 (33.30) | 3 (13.60) | 7 (31.80) | |
Note. PTSD is posttraumatic stress disorder; LEC-5 is Life Events Checklist for DSM-5;
accounts for missing data.
2.3. Measures
2.3.1. Demographic information.
We obtained information on age, years of schooling, gender, income, relationship status, employment status, and racial/ethnic status.
2.3.2. Life Events Checklist for DSM-5 (LEC-5; Weathers et al., 2013).
The LEC-5 is a 17-item self-report measure assessing lifetime traumatic events using a six-point nominal scale (happened to me, witnessed it, learned about it, part of my job, not sure, or does not apply). Participants endorsing one of the first four response options were considered trauma-exposed according to the DSM-5 PTSD Criterion A (American Psychiatric Association, 2013). The LEC for DSM-IV has demonstrated adequate psychometric properties (Gray, Litz, Hsu, & Lombardo, 2004).
2.3.3. PTSD Checklist for DSM-5 (PCL-5; Weathers et al., 2013).
The PCL-5 is a 20-item self-report measure assessing PTSD symptom severity in the past month referencing the most traumatic event endorsed on the LEC-5. The PCL-5 administered at T1 assessed PTSD symptom severity in the past week referencing the most traumatic event endorsed on the LEC-5. Response options range from 0 (not at all) to 4 (extremely). The PCL-5 has excellent psychometric properties; a cut-off score of ≥31 indicates probable PTSD (Bovin et al., 2016; Wortmann et al., 2016). A decrease of at least 10 points on the PCL is considered clinically significant change (Monson et al., 2008); a decrease of this magnitude is similar to that observed in clinical samples participating in PTSD treatment (e.g., Banducci, Bonn-Miller, Timko, & Rosen, 2018). In the current study, Cronbach’s α was .95 and .94 for the T0 pre-task and T1 post-task administrations, respectively.
2.3.4. Patient Health Questionnaire-9 (PHQ-9; Kroenke & Spitzer, 2002).
The PHQ-9 is a nine-item self-report measure assessing the severity of depression symptoms within the past two weeks. Response options range from 0 (not at all) to 3 (nearly every day). The PHQ-9 has excellent psychometric properties (Kroenke & Spitzer, 2002; Kroenke et al., 2001). In the current study, Cronbach’s α was .87 for both T0 pre-task and T1 post-task administrations.
2.3.5. Positive and Negative Affect Schedule (PANAS; Watson et al., 1988).
The PANAS is a self-report measure consisting of two 10-item subscales, one assessing positive affect and the other assessing negative affect. Participants rated the degree to which they currently experience positive or negative affect on a five-point Likert scale ranging from 1 (very slightly or not at all) to 5 (extremely). The PANAS demonstrates adequate psychometric properties (Crawford & Henry, 2004). In the current study, Cronbach’s α for the PANAS negative was .86, .89, .82, and .91 for T0 pre-task, T0 post-task, T1 pre-task, and T1 post-task administrations, respectively; Cronbach’s α for the PANAS positive was .94, .94, .95, and .95 for T0 pre-task, T0 post-task, T1 pre-task, and T1 post-task administrations, respectively.
2.3.6. Posttraumatic Cognitions Inventory (PTCI; Foa et al., 1999).
The PTCI is a 36-item self-report measure that assesses trauma-related patterns of thinking. Response options range from 1 (totally disagree) to 7 (totally agree). The measure yields three subscales: Negative Cognitions about the Self, Negative Cognitions about the World, and Self-Blame. The PTCI has demonstrated adequate psychometric properties (Beck et al., 2004). In the current study, Cronbach’s α was .97 for each of the T0 pre-task and T1 post-task administrations.
2.3.7. Rosenberg Self-Esteem Scale (RSES; Rosenberg, 1965; Rosenberg, 1979).
The RSES is a 10-item self-report measure assessing global self-esteem. Response options range from 1 (strongly agree) to 4 (strongly disagree). The RSES has good psychometric properties (Gray-Little, Williams, & Hancock, 1997). In the current study, Cronbach’s α was .93 and .92 for T0 pre-task and T1 post-task administrations, respectively.
2.4. Statistical Analyses
2.4.1. Memory Coding.
We examined whether participants were able to follow instructions to recall a specific (memory of an event that occurred at a specific place within 24 hours; Williams & Broadbent, 1986) positive memory. To determine whether the valence of the memory was positive, we adapted coding procedures based on the Coding and Assessment System for Narratives of Trauma (CASNOT; Fernández-Lansac & Crespo, 2017). In this two-step procedure, trained research assistants first coded the emotional tone (five-point rating scale from 0 [completely positive] to 4 [completely negative]) and the emotional valence (five-point rating scale from 0 [completely positive] to 4 [completely negative]) of the memory; next they coded a memory as positive if both emotional tone and emotional valence ratings were positive (i.e., coder ratings of 0, 1, or 2). The Affective Norms for English Words (ANEW) system (Bradley & Lang, 2017) was utilized as supplemental material to assist coders in rating emotional valence and emotional tone. In addition, trained research assistants examined specificity by coding each memory as specific (code of 1) vs. not specific (code of 0).
Following recommendations (Hallgren, 2012; McHugh, 2012), three trained independent raters comprising of two teams (one team had two raters) coded 25% of audio-recorded and written memories for valence and specificity. Assessing inter-rater reliability with Siegel and Castellan’s (1988) variant of Cohen’s kappa coefficient (Cohen, 1960; Hallgren, 2012), results indicated 100% agreement between raters for coded valence and specificity. Hence, we could not compute kappa; Cohen’s kappa coefficient is undefined with no variation between coder ratings (Christensen, Margolin, & Sullaway, 1992; Rowsome, Comerford, Mottram, Samuel, & Stokes, 2016). Next, two research assistants (who comprised of one team initially) independently coded the remainder of elicited memories for valence and specificity.
2.4.2. Preliminary Analyses.
We checked for violation of normality (skewness >2 and/or kurtosis > 7; Curran, West, & Finch, 1996), sphericity (p < .05; Mauchly, 1940), and homogeneity of variances (p < .05; Levene, 1960) for each dependent variable in each condition.
2.4.3. Primary Hypotheses.
We conducted four mixed between-within subjects ANOVAs to assess the impact of our conditions (processing specific positive memories via writing or narrating, control) on PTSD symptom severity, depression symptom severity, post-trauma maladaptive cognitions, and self-esteem across two time points (T0 pre-task and T1 post-task). Two additional mixed between-within subjects ANOVAs were conducted to assess the impact of our conditions on positive and negative affect across four time points (T0 pre-task, T0 post-task, T1 pre-task, and T1 post-task). Thus, the within-subjects factor was T0 pre-task, T0 post-task, T1 pre-task, and/or T1 post-task scores; the between-subjects factor was the condition assigned to each participant (writing, narrating, control); and the dependent variables included PTSD symptom severity, depression symptom severity, negative and positive affect, post-trauma maladaptive cognitions, and self-esteem analyzed separately in each model. For significant interaction effects, we ran analyses of simple effects; this included either a paired samples t test (two time points; Cohen’s d effect size estimates) or a one-way ANOVA (four time points; Fisher’s Least Significant Difference [LSD] post-hoc tests; partial η2 effect size estimates) for the dependent variable of each post-trauma mental health indicator for each condition. For non-significant interactions, we examined the main effects of time and condition independently using partial η2 effect size estimates and Tukey’s honestly significant difference (HSD) post-hoc tests (Tukey, 1949).
3. Results
3.1. Preliminary Analyses
In regards to assumptions, all outcome variables were normally distributed with no significant outliers. Further, the assumption of sphericity was met in all analyses excluding those for positive affect (Mauchly’s W = .70, p = .001) and negative affect (Mauchly’s W = .73, p = .002); in these situations we utilized Greenhouse-Geisser estimates (Greenhouse & Geisser, 1959). Lastly, Levene’s test estimates (Levene, 1960) indicated homogeneity of variances. The Benjamini and Hochberg correction (B-H; Benjamini & Hochberg, 1995) was used to account for Type I error for the interaction effects, which paralleled the primary analyses of the current study (critical value of .008).
3.2. Primary Hypotheses (see Table 1 for means and standard deviations, Table 2 for correlations, and Table 3 for ANOVA results)
Table 2.
Pearson Bivariate Correlation Table.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. T0 pre-task PTSD symptom severity | – | |||||||||||||||
| 2. T1 post-task PTSD symptom severity | .75** | – | ||||||||||||||
| 3. T0 pre-task depression symptom severity | .68** | .57** | – | |||||||||||||
| 4. T1 post-task depression symptom severity | .61** | .75** | .82** | – | ||||||||||||
| 5. T0 pre-task negative affect | .63** | .57** | .53** | .61** | – | |||||||||||
| 6. T0 post-task negative affect | .59** | .59** | .46** | .53** | .66** | – | ||||||||||
| 7. T1 pre-task negative affect | .25* | .36** | .26* | .43** | .40** | .47** | – | |||||||||
| 8. T1 post-task negative affect | .42** | .64** | .32** | .58** | .63** | .63** | .79** | – | ||||||||
| 9. T0 pre-task maladaptive cognitions | .59** | .58** | .71** | .69** | .57** | .37** | .19 | .31* | – | |||||||
| 10. T1 post-task maladaptive cognitions | .61** | .67** | .63** | .71** | .54** | .48** | .31* | .46** | .84** | – | ||||||
| 11. T0 pre-task positive affect | −.21 | −.20 | −.36** | −.32** | −.12 | −.13 | −.05 | −.04 | −.50** | −.47** | – | |||||
| 12. T0 post-task positive affect | −.18 | −.19 | −.26* | −.20 | −.06 | −.19 | .04 | .06 | −.39** | −.40** | .87** | – | ||||
| 13. T1 pre-task positive affect | −.20 | −.21 | −.38** | −.30* | −.12 | −.18 | −.01 | −.03 | .−.39** | −.36** | .80** | .76** | – | |||
| 14. T1 post-task positive affect | −.21 | −.29* | −.43** | −.37** | −.20 | −.21 | −.03 | −.14 | −.47** | −.45** | .82** | .78** | .89** | – | ||
| 15. T0 pre-task self-esteem | −.51** | −.53** | −.67** | −.69** | −.54** | −.45** | −.30* | −.37** | −.69** | −.73** | .47** | .46** | .49** | .54** | – | |
| 16. T1 post-task self-esteem | −.50** | −.55** | −.61** | −.68 ** | −.56** | −.40** | −.31* | −.44** | −.68** | −.72** | .48** | .44** | .50** | .60** | .88** | – |
| Mean | 23.92 | 19.97 | 7.86 | 7.98 | 16.52 | 14.12 | 14.46 | 14.77 | 105.32 | 102.28 | 22.25 | 25.58 | 22.97 | 22.17 | 27.52 | 28.06 |
| SD | 18.33 | 16.30 | 5.41 | 5.61 | 5.88 | 5.25 | 4.53 | 6.10 | 46.50 | 44.41 | 8.88 | 10.23 | 9.43 | 9.95 | 6.73 | 6.62 |
Note.
Correlation is significant at the 0.01 level;
Correlation is significant at the 0.05 level.
Table 3.
ANOVA Results for All Outcome Variables.
| Dependent Variables | Main Effect of Condition | Main Effect of Time | Interaction Effect | ||||
|---|---|---|---|---|---|---|---|
| F(df) | ηp2 | F(df) | ηp2 | Wilks’ λ | F(df) | ηp2 | |
| PTSD symptom severity | .22 (2,62) p = .803 | .01 | 6.74 (1,62) p = .012 | .10 | .91 | 2.91 (2,62) p = .062 | .09 |
| Depression symptom severity | .77 (2,62) p = .466 | .02 | .11 (1,62) p = .736 | .002 | .94 | 1.90 (2,62) p = .159 | .06 |
| Negative affect | .35 (2,62) p = .705 | .01 | 6.41 (2.46,152.27) p = .001 | .09 | .81 | 2.25 (6,120) p = .043 | .10 |
| Maladaptive cognitions | .38 (2,62) p = .687 | .01 | 1.06 (1,62) p = .307 | .02 | .91 | 3.06 (2,62) p = .054 | .09 |
| Positive affect | .77 (2,62) p = .466 | .02 | 11.22 (2.38, 147.42) p < .001 | .15 | .63 | 5.15 (6, 120) p < .001 | .21 |
| Self-esteem | .30 (2,62) p = .745 | .01 | 1.68 (1,62) p = .200 | .03 | .97 | .98 (2, 62) p = .383 | .03 |
Note. Bold indicates significant/marginally significant results; ηp2 is partial η2.
3.2.1. Psychopathology symptoms.
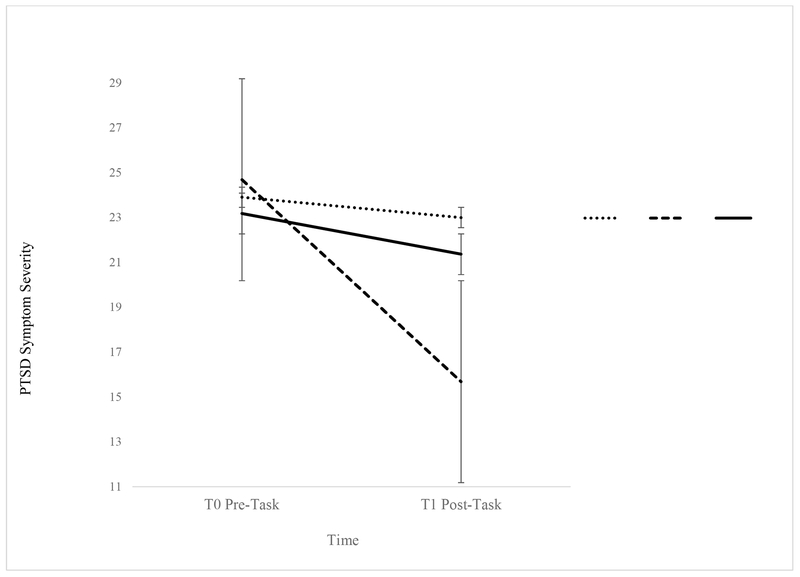
For PTSD symptom severity, results indicated that a marginally significant interaction effect between condition and time explained 9% of the variance. Analysis of simple effects using paired samples t tests indicated a significant difference in PTSD symptom severity across T0 pre-task and T1 post-task for the narrating condition only, t(21) = 3.18, p = .005, Cohen’s d = .68. Visual inspection of the plot (Figure 2) indicated a trend of decreasing PTSD symptom severity scores in the narrating condition from T0 pre-task to T1 post-task; PTSD symptom severity scores declined less in the writing and control conditions.1 From pre- to post-task in the narrating condition, 50% fewer participants were above the diagnostic threshold for probable PTSD, and PTSD symptom severity scores dropped by nine points, which approaches clinically significant change (Monson et al., 2008). For depression symptom severity, results indicated no significant interaction effect between condition and time (6% of variance in depression symptom severity was explained by the interaction effect), and no significant main effects for time and condition.
Figure 2.
Marginally Significant Interaction Effect of Time and Condition on PTSD Symptom Severity
Note. Error bars represent standard errors.
3.2.2. Affect.
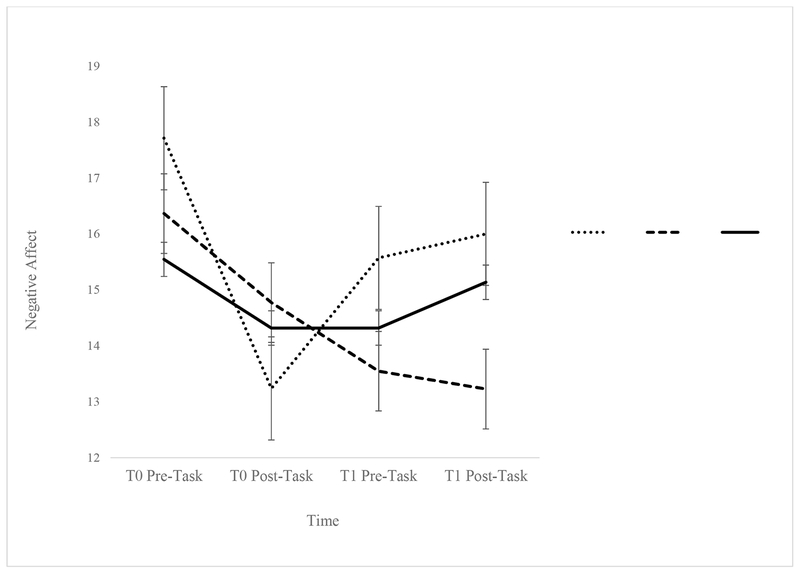
For negative affect, results indicated that a marginally significant interaction between condition and time explained 10% of the variance. Analysis of simple effects using repeated measures ANOVA indicated a significant difference in negative affect scores across T0 pre-task, T0 post-task, T1 pre-task, and T1 post-task for the narrating (F [3, 19] = 5.33, p = .008, partial η2 = .46) and writing conditions (F [3, 18] = 5.61, p = .007, partial η2 = .48) as opposed to the control condition (F [3, 19] = 1.68, p = .204, partial η2 = .21). Specifically, in the writing condition, Fisher’s LSD post-hoc tests indicated that the negative affect scores significantly decreased from T0 pre-task to T0 post-task (p = .001); significantly increased from T0 post-task to T1 pre-task (p = .034); and significantly increased from T0 post-task to T1 post-task (p = .031); no other comparisons were significant. In the narrating condition, Fisher’s LSD post-hoc tests indicated that the negative affect scores significantly decreased from T0 pre-task to T1 pre-task (p = .015) and significantly decreased from T0 pre-task to T1 post-task (p = .001). Visual inspection of the plot (Figure 3) indicated a trend of decreasing negative affect scores in the narrating condition across all time points; whereas in the writing and control conditions, there was a decline and then an increase in negative affect scores.2
Figure 3.
Marginally Significant Interaction Effect of Time and Condition on Negative Affect
Note. Error bars represent standard errors.
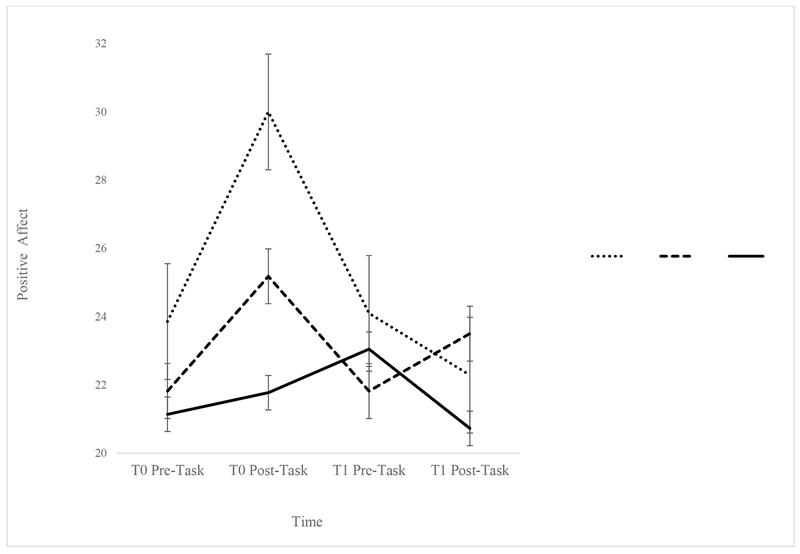
For positive affect, results indicated that a significant interaction effect between condition and time explained 21% of the variance in positive affect scores. Analysis of simple effects using repeated measures ANOVA indicated a significant difference in positive affect across T0 pre-task, T0 post-task, T1 pre-task, and T1 post-task for the writing (F [3, 18] = 9.14, p = .001, partial η2 = .60), narrating (F [3, 19] = 4.74, p = .012, partial η2 = .43), and control conditions (F [3, 19] = 3.65, p = .031, partial η2 = .33). In the narrating condition, Fisher’s LSD post-hoc tests indicated that the positive affect scores significantly increased from T0 pre-task to T0 post-task (p = .005); significantly decreased from T0 post-task to T1 pre-task (p = .009); and marginally, significantly increased from T1 pre-task to T1 post-task (p = .073). In the writing condition, Fisher’s LSD post-hoc tests indicated that the positive affect scores significantly increased from T0 pre-task to T0 post-task (p < .001); significantly decreased from T0 post-task to T1 pre-task (p = .002); and significantly decreased from TO post-task to T1 post-task (p < .001). In the control condition, Fisher’s LSD post-hoc tests indicated that the positive affect scores significantly decreased from T1 pre-task to T1 post-task (p = .007). Visual inspection of the plot (Figure 4) indicated a trend of increase in positive affect pre-to-post task for each time point only for the narrating condition; positive affect scores increased from T0 pre-to-post task but decreased from T1 pre-to-post task in the writing and control conditions. These results support an overall significant cubic model (F [2, 62] = 8.43, p = .001, partial η2 = .21).3
Figure 4.
Significant Interaction Effect of Time and Condition on Positive Affect
Note. Error bars represent standard errors.
3.2.3. Cognitions.
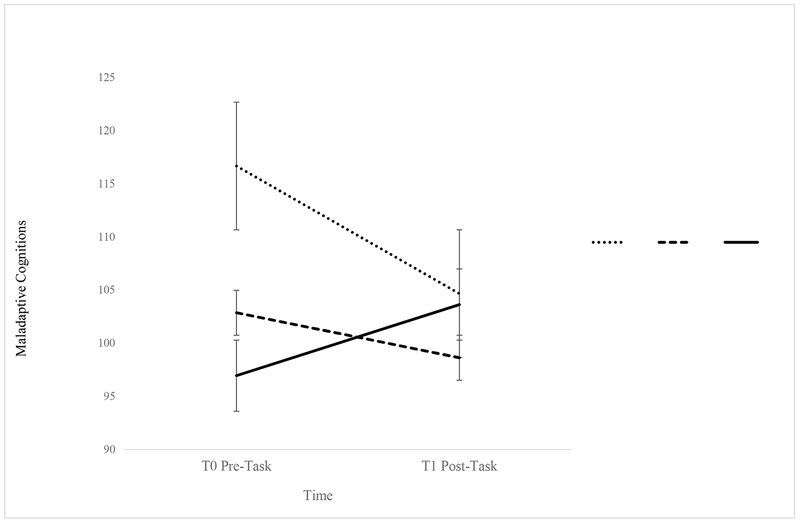
For post-trauma maladaptive cognitions, results indicated that a marginally significant interaction effect between condition and time explained 9% of the variance. Analysis of simple effects using paired samples t tests indicated a marginally significant difference in maladaptive cognition scores between T0 pre-task and T1 post-task for the narrating condition only, t(21) = 1.96, p = .063, Cohen’s d = .42. Visual inspection of the plot (Figure 5) indicated a trend of decreasing maladaptive cognition scores in the writing and narrating conditions from T0 pre-task to T1 post-task; on the other hand, maladaptive cognition scores seem to increase in the control condition from T0 pre-task to T1 post-task. For self-esteem, results indicated no significant interaction effect (3% of the variance in self-esteem scores was explained by the interaction effect) and no significant main effects for time and condition.
Figure 5.
Marginally Significant Interaction Effect of Time and Condition on Post-Trauma Maladaptive Cognitions.
Note. Error bars represent standard errors.
4. Discussion
4.1. Overview
Within the current study, we examined the effects of processing positive memories on PTSD symptom severity, depression symptom severity, affect, and cognitions in a non-clinical sample of trauma-exposed college students. In line with prior work, we hypothesized that those participating in our positive memory interventions (i.e., writing or narrating) would experience substantial reductions in PTSD symptom severity (Contractor, Brown, et al., 2018), depression symptom severity (Arditte Hall et al., 2018; Neshat-Doost et al., 2013), negative affect (Joormann et al., 2007; Rusting & DeHart, 2000), and maladaptive cognitions (Blaney, 1986; Rusting & Larsen, 1998), as well as substantial increases in positive affect (Joormann et al., 2007; Rusting & DeHart, 2000) and self-esteem (Korrelboom et al., 2012; Korrelboom et al., 2011). In line with these hypotheses, broadly, the positive memory processing conditions (especially narrating) positively impacted symptomatology, affect, and cognitions.
4.2. Changes in Symptomatology, Affect, and Cognitions over Time
Overall, the impact differed by the positive memory processing condition, such that the narrating condition generally had greater and more beneficial impacts on outcomes of interest than the writing condition. For example, there were reductions in PTSD symptom severity and post-trauma maladaptive cognitions among those who participated in the narrating condition, but not in the writing or control conditions. Further, the narrating condition was differentially associated with continued increases in positive affect and decreases in negative affect (Joormann et al., 2007; Josephson, 1996; Rusting & DeHart, 2000) across the two sessions.
The differential pattern of findings for affect may reflect the transient nature of affect evoked by recalling positive memories. In the narrating condition, participants had a pattern of decreases in negative affect over time, which was in line with study hypotheses. For positive affect, in contrast, the effects were more transitory, in that affect was elevated post-task on both occasions, but returned to baseline between the two sessions. In this case, it is likely that between-session factors may have impacted participants’ moods. Moreover, these effects may not be particularly surprising, as research demonstrates that positive affect following a positive mood induction is generally quite transitory (Horner et al., 2014). In regards to the writing condition, writing about positive memories initially led to an increase in positive affect and a decrease in negative affect, but these changes were not sustained over time, differing from some prior work (Burton & King, 2004). These findings may primarily be driven by how the structure of the writing task differed from the narrating task (see Section 4.3 below for additional details).
Unexpectedly, depression symptom severity did not change during the course of the study, or as a function of the assigned condition, which differs from prior work suggesting that processing positive memories does have a positive impact on depression symptom severity (Arditte Hall et al., 2018; McNally et al., 1994; Neshat-Doost et al., 2013). One factor impacting these findings may be the time frame of the PHQ-9 as used in the current study wherein the T1 PHQ-9 referenced the past two weeks rather than time since T0 assessment; such a procedure may have not allowed us to capture change effectively within the current study. Similarly, positive memory processing did not impact self-esteem contrary to existing research (Korrelboom et al., 2009; Korrelboom et al., 2012; Korrelboom et al., 2011). Future research needs to examine potential mediating or moderating factors that may account for these results, such as trauma types (Briere & Runtz, 1990; Contractor, Caldas, Fletcher, Shea, & Armour,2018), extent of meaning-making derived from memory narratives (Singer, Blagov, Berry, & Oost, 2013), centrality of the event to one’s identity (akin to traumatic memories; Berntsen & Rubin, 2006), and number and characteristics (e.g., related or unrelated to trauma) of the elicited positive memories (Contractor, Brown, et al., 2018). Separately, perhaps, results would differ within a sample of individuals reporting clinically significant depression or PTSD symptom severity, who differ meaningfully from this non-clinical student sample.
Taken together, the narrating condition appears to have a more substantial and beneficial impact on decreasing PTSD symptom severity, negative affect, and maladaptive post-trauma cognitions, as well as on increasing positive affect, within this controlled pilot study, as compared to the writing and control conditions. Thus, talking about positive memories appears to more substantially affect PTSD-related symptoms, as compared to writing about positive memories. Moving forward, we argue for the use of the narrating procedure, rather than the writing procedure, for processing positive memories.
4.3. Unpacking the Differential Impacts of Writing versus Narrating
There are some potential explanations for the differential impact of narrating versus writing about positive memories on the assessed outcomes. First, it is possible that the writing methodology lessened the impact of this intervention (i.e., typing on a computer, rather than hand writing). For example, within cognitive processing therapy (CPT; with a trauma account), participants are directed to handwrite their trauma account, given that research suggests the use of word processing software impedes emotional engagement in the task, due to an over-focus on spelling and grammar (Resick, Monson, & Chard, 2016). This may also explain the unexpected pattern of findings for positive and negative affect, particularly in the writing condition. Perhaps writing about positive memories became less engaging over time and felt less enjoyable, leading to decreases in positive affect and increases in negative affect across the course of the task. Additionally, research demonstrates using long-hand writing, as compared to typing on computers, leads to deeper processing and understanding (Mueller & Oppenheimer, 2014). Perhaps using computers to type positive memories impacted participants’ degree of emotional engagement and processing in the task within the current study, additionally impacting symptomatology and affect. Second, it is possible that memory is differentially processed when discussing memories aloud versus writing about them (Lyubomirsky, Sousa, & Dickerhoof, 2006). Research examining the impact of processing positive memories via writing, talking, or thinking demonstrates that individuals who write about positive memories in an analytical fashion experience decreases in well-being, relative to individuals who process these memories via rehearsing and replaying the experiences more vividly (Lyubomirsky, Sousa, & Dickerhoof, 2006). Following from this, Lyubomirsky and colleagues (2006) suggest that the narrative-based and analytical nature often inherent in writing can be counterproductive when attempting to increase positive affect via writing about positive memories. Indeed, it is possible that a more circular or disorganized narrative that can come from discussing a memory aloud allows individuals to savor and capitalize on positive memories, as well as to retain a sense of mystery or thrill, which is diminished when memories are examined analytically and critically.
Third, it is possible that discussing positive memories with others (as in the narrating task) may have a substantial positive benefit on mood (Reis et al., 2010) via the process of sharing with another individual; participants in the writing condition did not have the opportunity to share their memory during the processing task. Finally, it is noteworthy that both the writing and narrating conditions had similarly beneficial impacts on affect following the processing of one positive memory; the differential impact was apparent following the processing of the second positive memory, which suggests participants in the writing condition may have focused more on “correctly” writing the content of the memory, rather than fully emotionally engaging with the memory. Thus, it may not be surprising that these individuals did not feel better after typing out the memory during the second session. Alternatively, such results may also indicate a potentially greater practice effect for the narrating condition, or a perceived beneficial, immediate impact after the first session, which could have cumulatively impacted the results for the second memory account.
4.4. Limitations and Future Directions
Some limitations must be considered when interpreting our findings. First, we utilized self-report assessments of symptomatology, affect, and cognitions; these could be subject to information biases or inaccurate reporting. Future research would benefit from using clinician-administered and/or objective (e.g., psychophysiological) measures. Second, we used a convenience-based, non-clinical sample, comprised of students reporting traumatic experiences (30.80% with probable PTSD); this sample had more females and less racial/ethnic diversity. Importantly, despite this being a non-clinical sample, research has indicated high rates of trauma exposure among college students, which is related to poor post-trauma mental health, including greater PTSD symptom severity (Elhai et al., 2012; Frazier et al., 2009; Read, Radomski, & Borsari, 2015). Such analogue samples are important to advance the scientific field of trauma; they are especially relevant to the current study, which is testing a novel methodology with potential clinical impact and is the first empirical test of a conceptual model (Tull, Bornovalova, Patterson, Hopko, & Lejuez, 2008). This being said, it will be necessary to determine whether these results generalize to more diverse and clinically-severe samples in future work.
Third, given that this was a pilot study, our sample size was small and we had limited power, precluding exploration of some associations within our data. Further replications and extensions of this work with larger sample sizes (and consequently greater power to detect clinically meaningful results) are necessary to better understand causality and determine mechanisms underlying obtained patterns. Fourth, we used a correction factor for multiple comparisons to protect against Type I error for our primary analyses (i.e., interaction effects). Using this approach is debated because it increases the risk of Type II errors, and there is ambiguity on what/how to determine the number of outcome measures to be used in computing the correction factor (Hochberg & Tamhane, 1987; Rothman, 1990; Savitz & Olshan, 1995). Hence, we focused more on effect sizes (Feise, 2002) in the process of emphasizing worthwhile results. The partial η2 range for significant/marginally effect interaction effects (.09-.21) and for significant post-hoc tests (.33-.60) represented medium-large effect sizes (Cohen, 1988; Richardson, 2011); and Cohen’s d range for significant post-hoc tests (.42-.68) represented small-medium effect sizes (Cohen, 1988). Overall, these conclusions are considered tentative and need to be replicated in future studies. Fifth, methodologically, measures had different time frames for their questions (past month/week for the PCL-5 vs. past two weeks for the PHQ-9), and some measures did not reference time elapsed since the first baseline session (e.g., the PHQ-9 administered at T1 referenced the past two weeks). That being said, significant differences in post-trauma indicators across time points reflect meaningful results to be explored in future research. Finally, we did not examine whether the observed changes persisted over time, or whether the experience of significant events between tasks impacted study findings; these are important to examine in future research.
Despite these limitations, the present study advances the field by serving as the first rigorous and experimental comparison of the impact of narrating versus writing about positive memories on outcomes relevant to PTSD symptom severity, with a contact-time matched control condition. To our knowledge, the current study is also the first empirical examination of, and provides empirical support to, the conceptual model proposed by Contractor and colleagues (2018). In terms of clinical implications, therapists may benefit from integrating a focus on positive memories into their trauma work to decrease PTSD symptom severity, negative affect, and maladaptive cognitions, as well as to increase positive affect. Further, verbally discussing and processing positive memories seems optimal, as compared to writing and processing positive memories; this fits well with the narrative processing approach of several trauma-focused treatments such as Prolonged Exposure (Foa, Hembree, & Rothbaum, 2007). By highlighting the utility of focusing on processing positive memories among trauma-exposed individuals, this study sets the stage for future work targeting positive memory processing. As an example, given that increases in positive affect were not sustained between sessions (in the interim), it may be necessary to add between-session exercises to maintain improved mood, as well as to sustain change over time. Further developing strategies to support individuals in savoring and capitalizing (Lyubomirsky et al., 2006) on their positive memories may further enhance observed effects. Taken together, trauma-exposed individuals may benefit substantially from engaging emotionally with positive memories via discussing these memories, suggesting the importance of targeting this process parallel to traumatic memories. Our conclusions are with the caveat that this is a pilot study in a relatively unexplored area; thus, further exploration and replication is necessary to conclude a significant clinical impact.
Supplementary Material
Highlights:
We examined the effects of positive memory processing on posttrauma mental health.
We randomized 65 students to narrating, writing, or control conditions.
Narrating had lower PTSD symptom severity, posttrauma cognitions, and negative affect.
Narrating had greater positive affect.
Writing had an increase then a decrease in positive (reverse for negative) affect.
Acknowledgements:
We acknowlege the contributions of Ms. Seanne OHara, Ms. Shelby Thornton, Ms. Christina Cantu, Ms. Megan Dolan, Ms. Stephanie Caldas, and Mr. Joseph Koh for data collection.
Funding Organizations: The research described here was supported, in part, by grants from the National Institute on Drug Abuse (K23DA039327) awarded to the last author.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
For the main effect for time, post-hoc tests indicated a significant decrease in PTSD symptom severity scores from T0 pre-task to T1 post-task (p = .012).
For the main effect for time, post-hoc tests showed that the T0 pre-task negative affect score was statistically higher than negative affect scores at T0 post-task (p < .001), T1 pre-task (p = .038), and T1 post-task (p = .046).
For the main effect of time, post-hoc test results indicated a significant increase in positive affect score from T0 pre-task to T0 post-task (p < .001), from T0 post-task to T1 pre-task (p = .007), and from T0 post-task to T1 post-task (p < .001).
Declaration of Interest: All authors declare that they have no conflict of interest.
Contributor Information
Ateka A. Contractor, Department of Psychology, University of North Texas, Denton, TX, USA
Anne N. Banducci, VA Boston Healthcare System, Boston, MA, USA; Boston University School of Medicine, Boston, MA, USA
Ling Jin, Department of Psychology, University of North Texas, Denton, TX, USA.
Fallon Keegan, Department of Psychology, University of North Texas, Denton, TX, USA.
Nicole H. Weiss, Department of Psychology, University of Rhode Island, Kingston, RI, USA
References
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Washington, DC: American Psychiatric Association. [Google Scholar]
- Arditte Hall KA, De Raedt R, Timpano KR, & Joormann J (2018). Positive memory enhancement training for individuals with major depressive disorder. Cognitive Behaviour Therapy, 47, 155–168. doi: 10.1080/16506073.2017.136429 [DOI] [PubMed] [Google Scholar]
- Banducci AN, Bonn-Miller MO, Timko C, & Rosen CS (2018). Associations between residential treatment length, PTSD, and outpatient healthcare utilization among veterans. Psychological Services, 15, 529–535. doi: 10.1037/ser0000204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck JG, Coffey SF, Palyo SA, Gudmundsdottir B, Miller LM, & Colder CR (2004). Psychometric properties of the Posttraumatic Cognitions Inventory (PTCI): A replication with motor vehicle accident survivors. Psychological Assessment, 16, 289–298. doi: 0.1037/1040-3590.16.3.289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benjamini Y, & Hochberg Y (1995). Controlling the false discovery rate: A practical and powerful approach to multiple testing. Journal of the Royal Statistical Society. Series B (Methodological), 57, 289–300. [Google Scholar]
- Bernsten D, & Rubin DC (2007). When a trauma becomes a key to identity: Enhanced integration of trauma memories predicts posttraumatic stress disorder symptoms. Applied Cognitive Psychology, 21, 417–431. doi: 10.1002/acp.1290 [DOI] [Google Scholar]
- Berntsen D, & Rubin DC (2006). The Centrality of Event Scale: A measure of integrating a trauma into one’s identity and its relation to post-traumatic stress disorder symptoms. Behavior Research and Therapy, 44, 219–231. doi: 10.1016/j.brat.2005.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blaney PH (1986). Affect and memory: A review. Psychological Bulletin, 99, 229–246. doi: 10.1037/0033-2909.99.2.229 [DOI] [PubMed] [Google Scholar]
- Bonde JP, Utzon-Frank N, Bertelsen M, Borritz M, Eller NH, & Nordentoft M (2016). Risk of depressive disorder following disasters and military deployment: Systematic review with meta-analysis. The British Journal of Psychiatry, 208, 330–336. doi: 10.1192/bjp.bp.114.157859 [DOI] [PubMed] [Google Scholar]
- Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, et al. (2016). Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition (PCL-5) in veterans. Psychological Assessment, 28, 1379–1391. doi: 10.1037/pas0000254 [DOI] [PubMed] [Google Scholar]
- Boyacioglu I, & Akfirat S (2015). Development and psychometric properties of a new measure for memory phenomenology: The Autobiographical Memory Characteristics Questionnaire. Memory, 23, 1070–1092. doi: 10.1080/09658211.2014.953960 [DOI] [PubMed] [Google Scholar]
- Bradley MM, & Lang PJ (2017). Affective Norms for English Words (ANEW): Instruction manual and affective ratings Technical Report C-3. Gainesville, FL: University of Florida Center for the Study of Emotion and Attention. [Google Scholar]
- Brewin CR (2014). Episodic memory, perceptual memory, and their interaction: Foundations for a theory of posttraumatic stress disorder. Psychological Bulletin, 140, 69–97. doi: 10.1037/a0033722 [DOI] [PubMed] [Google Scholar]
- Briere J, & Runtz M (1990). Differential adult symptomatology associated with three types of child abuse histories. Child Abuse & Neglect, 14, 357–364. [DOI] [PubMed] [Google Scholar]
- Bryant RA, Sutherland K, & Guthrie RM (2007). Impaired specific autobiographical memory as a risk factor for posttraumatic stress after trauma. Journal of Abnormal Psychology, 116, 837–841. doi: 10.1037/0021-843X.116.4.837 [DOI] [PubMed] [Google Scholar]
- Burton CM, & King LA (2004). The health benefits of writing about intensely positive experiences. Journal of Research in Personality, 38, 150–163. doi: 10.1016/S0092-6566(03)00058-8 [DOI] [Google Scholar]
- Caldas SV, Jin L, Dolan M, Dranger P, & Contractor AA (in press). An exploratory examination of client perspectives on a positive memory technique for PTSD. Journal of Nervous and Mental Disease. [DOI] [PubMed] [Google Scholar]
- Christensen A, Margolin G, & Sullaway M (1992). Interparental agreement on child behavior problems. Psychological Assessment, 4, 419–425. doi: 10.1037/1040-3590.4.4.419 [DOI] [Google Scholar]
- Cohen J (1960). A coefficient of agreement for nominal scales. Educational and Psychological Measurement, 20, 37–46. doi: 10.1177/001316446002000104 [DOI] [Google Scholar]
- Cohen J (1988). Statistical power analysis for the behavioral sciences. (2nd ed.). Hillside, New Jersey: Erlbaum. [Google Scholar]
- Contractor AA, Banducci AN, Dolan M, Keegan F, & Weiss NH (2019). Relation of positive memory recall count and accessibility with posttrauma mental health. Memory, 27, 1130–1143. doi: 10.1080/09658211.2019.1628994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Contractor AA, Brown LA, Caldas S, Banducci AN, Taylor DJ, Armour C, et al. (2018). Posttraumatic stress disorder and positive memories: Clinical considerations. Journal of Anxiety Disorders, 58, 22–32. doi: 10.1016/j.janxdis.2018.06.007 [DOI] [PubMed] [Google Scholar]
- Contractor AA, Caldas S, Fletcher S, Shea MT, & Armour C (2018). Empirically-derived lifespan polytraumatization typologies: A systematic review. Journal of Clinical Psychology, 74, 1137–1159. doi: 10.1002/jclp.22586 [DOI] [PubMed] [Google Scholar]
- Conway MA (1997). Recovered memories and false memories. New York: Oxford University Press. [Google Scholar]
- Crawford JR, & Henry JD (2004). The Positive and Negative Affect Schedule (PANAS): Construct validity, measurement properties and normative data in a large non-clinical sample. British Journal of Clinical Psychology, 43, 245–265. doi: 10.1348/0144665031752934 [DOI] [PubMed] [Google Scholar]
- Curran PJ, West SG, & Finch JF (1996). The robustness of test statistics to nonnormality and specification error in confirmatory factor analysis. Psychological Methods, 1, 16–29. doi: 10.1037/1082-989X.1.1.16 [DOI] [Google Scholar]
- De Quervain DJF, Kolassa IT, Ackermann S, Aerni A, Boesiger P, Demougin P, et al. (2012). PKCα is genetically linked to memory capacity in healthy subjects and to risk for posttraumatic stress disorder in genocide survivors. Proceedings of the National Academy of Sciences, 109, 8746–8751. doi: 10.1073/pnas.1200857109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehlers A, & Clark DM (2000). A cognitive model of posttraumatic stress disorder. Behavior Research and Therapy, 38, 319–324. doi: 10.1016/S0005-7967(99)00123-0 [DOI] [PubMed] [Google Scholar]
- Elhai JD, Miller ME, Ford JD, Biehn TL, Palmieri PA, & Frueh BC (2012). Posttraumatic stress disorder in DSM-5: Estimates of prevalence and symptom structure in a nonclinical sample of college students. Journal of Anxiety Disorders, 26, 58–64. doi: 10.1016/j.janxdis.2011.08.013 [DOI] [PubMed] [Google Scholar]
- Faul F, Erdfelder E, Lang A-G, & Buchner A (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39, 175–191. [DOI] [PubMed] [Google Scholar]
- Feise RJ (2002). Do multiple outcome measures require p-value adjustment? BMC Medical Research Methodology, 8. doi: 10.1186/1471-2288-2-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernández-Lansac V, & Crespo M (2017). Presentation of the Coding and Assessment System for Narratives of Trauma (CASNOT): Application in Spanish battered women and preliminary analyses. The Spanish Journal of Psychology, 20, 1–12. doi: 10.1017/sjp.2017.31 [DOI] [PubMed] [Google Scholar]
- Foa EB (2011). Prolonged exposure therapy: Past, present, and future. Depression and Anxiety, 28, 1043–1047. doi: 10.1002/da.20907 [DOI] [PubMed] [Google Scholar]
- Foa EB, Ehlers A, Clark DM, Tolin DF, & Orsillo SM (1999). The Posttraumatic Cognitions Inventory (PTCI): Development and validation. Psychological Assessment, 11, 303–314. doi: 10.1037/1040-3590.11.3.303 [DOI] [Google Scholar]
- Foa EB, Hembree EA, & Rothbaum BO (2007). Prolonged exposure therapy for PTSD: Emotional processing of traumatic experiences: Therapist guide. New York, NY: Oxford University Press. [Google Scholar]
- Foa EB, & Kozak MJ (1986). Emotional processing of fear: Exposure to corrective information. Psychological Bulletin, 99, 20–35. doi: 10.1037//0033-2909.99.1.20 [DOI] [PubMed] [Google Scholar]
- Foa EB, McLean CP, Zang Y, Rosenfield D, Yadin E, Yarvis JS, et al. (2018). Effect of prolonged exposure therapy delivered over 2 weeks vs 8 weeks vs present-centered therapy on PTSD symptom severity in military personnel: A randomized clinical trial. JAMA, 319, 354–364. doi: 10.1001/jama.2017.21242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frazier P, Anders S, Perera S, Tomich P, Tennen H, Park C, et al. (2009). Traumatic events among undergraduate students: Prevalence and associated symptoms. Journal of Counseling Psychology, 56, 450–460. doi: 10.1037/a0016412 [DOI] [Google Scholar]
- Fredrickson BL (2000). Cultivating positive emotions to optimize health and well-being. Prevention and Treatment, 3(1). doi: 0.1037/1522-3736.3.1.31a [Google Scholar]
- Fredrickson BL (2001). The role of positive emotions in positive psychology: The broaden-and-build theory of positive emotions. American Psychologist, 56, 218–226. doi: 10.1037/0003-066X.56.3.218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham JW (2009). Missing data analysis: Making it work in the real world. Annual Review of Psychology, 60, 549–576. doi: 10.1146/annurev.psych.58.110405.085530 [DOI] [PubMed] [Google Scholar]
- Gray-Little B, Williams VS, & Hancock TD (1997). An item response theory analysis of the Rosenberg Self-Esteem Scale. Personality and Social Psychology Bulletin, 23, 443–451. doi: 10.1177/0146167297235001 [DOI] [Google Scholar]
- Gray MJ, Litz BT, Hsu JL, & Lombardo TW (2004). Psychometric properties of the Life Events Checklist. Assessment, 11(4), 330–341. doi: 10.1177/1073191104269954 [DOI] [PubMed] [Google Scholar]
- Greenhouse SW, & Geisser S (1959). On methods in the analysis of profile data. Psychometrika, 24, 95–112. doi: 10.1007/BF02289823 [DOI] [Google Scholar]
- Hallgren KA (2012). Computing inter-rater reliability for observational data: An overview and tutorial. Tutorials in Quantitative Methods for Psychology, 8, 23–34. doi: 10.20982/tqmp.08.1.p023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hauer BJ, Wessel I, Engelhard IM, Peeters LL, & Dalgleish T (2009). Prepartum autobiographical memory specificity predicts post-traumatic stress symptoms following complicated pregnancy. Memory, 17, 544–556. doi: 10.1080/09658210902953836 [DOI] [PubMed] [Google Scholar]
- Hitlin S (2003). Values as the core of personal identity: Drawing links between two theories of self. Social Psychology Quarterly, 66, 118–137. doi: 10.2307/1519843 [DOI] [Google Scholar]
- Hochberg Y, & Tamhane AC (1987). Multiple comparison procedures. New York, NY: John Wiley. [Google Scholar]
- Horner MS, Siegle GJ, Schwartz RM, Price RB, Haggerty AE, Collier A, et al. (2014). C’mon get happy: Reduced magnitude and duration of response during a positive-affect induction in depression. Depression and Anxiety, 31, 952–960. doi: 10.1002/da.22244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horowitz MJ (1986). Stress response syndromes (2nd ed.). Northvale, N.J.: Aronson. [Google Scholar]
- Janssen SM, Hearne TL, & Takarangi MK (2015). The relation between self-reported PTSD and depression symptoms and the psychological distance of positive and negative events. Journal of Behavior Therapy and Experimental Psychiatry, 48, 177–184. doi: 10.1016/j.jbtep.2015.04.002 [DOI] [PubMed] [Google Scholar]
- Joormann J, Siemer M, & Gotlib IH (2007). Mood regulation in depression: Differential effects of distraction and recall of happy memories on sad mood. Journal of Abnormal Psychology, 116, 484–490. doi: 10.1037/0021-843X.116.3.484 [DOI] [PubMed] [Google Scholar]
- Josephson BR (1996). Mood regulation and memory: Repairing sad moods with happy memories. Cognition and Emotion, 10, 437–444. doi: 10.1080/026999396380222 [DOI] [Google Scholar]
- King LA (2001). The health benefits of writing about life goals. Personality and Social Psychology Bulletin, 27, 798–807. doi: 10.1177/0146167201277003 [DOI] [Google Scholar]
- King LA, Hicks JA, Krull JL, & Del Gaiso AK (2006). Positive affect and the experience of meaning in life. Journal of Personality and Social Psychology, 90, 179–196. doi: 10.1037/0022-3514.90.1.179 [DOI] [PubMed] [Google Scholar]
- Korrelboom K, de Jong M, Huijbrechts I, & Daansen P (2009). Competitive Memory Training (COMET) for treating low self-esteem in patients with eating disorders: A randomized clinical trial. Journal of Consulting and Clinical Psychology, 77, 974–980. doi: 10.1037/a0016742 [DOI] [PubMed] [Google Scholar]
- Korrelboom K, Maarsingh M, & Huijbrechts I (2012). Competitive Memory Training (COMET) for treating low self-esteem in patients with depressive disorders: A randomized clinical trial. Depression and Anxiety, 29, 102–110. doi: 10.1002/da.20921 [DOI] [PubMed] [Google Scholar]
- Korrelboom K, Marissen M, & van Assendelft T (2011). Competitive Memory Training (COMET) for low self-esteem in patients with personality disorders: A randomized effectiveness study. Behavioural and Cognitive Psychotherapy, 30, 1–19. doi: 10.1017/S1352465810000469 [DOI] [PubMed] [Google Scholar]
- Kroenke K, & Spitzer RL (2002). The PHQ-9: A new depression diagnostic and severity measure. Psychiatric Annals, 32, 509–515. doi: 10.3928/0048-5713-20020901-06 [DOI] [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JBW (2001). The PHQ 9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16, 606–613. doi: 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levene H (1960). Robust tests for equality of variances In Olkin I (Ed.), Contributions to Probability and Statistics (pp. 278–292). Palo Alto, CA: Stanford University Press. [Google Scholar]
- Lyubomirsky S, King L, & Diener E (2005). The benefits of frequent positive affect: Does happiness lead to success? Psychological Bulletin, 131, 803–855. doi: 10.1037/0033-2909.131.6.803 [DOI] [PubMed] [Google Scholar]
- Lyubomirsky S, Sousa L, & Dickerhoof R (2006). The costs and benefits of writing, talking, and thinking about life’s triumphs and defeats. Journal of Personality and Social Psychology, 90, 692–708. doi: 10.1037/0022-3514.90.4.692 [DOI] [PubMed] [Google Scholar]
- Mauchly JW (1940). Significance test for sphericity of a normal n-variate distribution. Annals of Mathematical Statistics, 11, 204–209. doi: 10.1214/aoms/1177731915 [DOI] [Google Scholar]
- McAdams DP, Bauer JJ, Sakaeda AR, Anyidoho NA, Machado MA, Magrino-Failla K, et al. (2006). Continuity and change in the life story: A longitudinal study of autobiographical memories in emerging adulthood. Journal of Personality, 74, 1371–1400. doi: 10.1111/j.1467-6494.2006.00412.x [DOI] [PubMed] [Google Scholar]
- McHugh ML (2012). Interrater reliability: The kappa statistic. Biochemia Medica, 22, 276–282. doi: 10.11613/BM.2012.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLean KC, Pasupathi M, & Pals JL (2007). Selves creating stories creating selves: A process model of self-development. Personality and Social Psychology Review, 11, 262–278. doi: 10.1177/1088868307301034 [DOI] [PubMed] [Google Scholar]
- McNally RJ, Lasko NB, Macklin ML, & Pitman RK (1995). Autobiographical memory disturbance in combat-related posttraumatic stress disorder. Behavior Research and Therapy, 33, 619–630. doi: 10.1016/0005-7967(95)00007-K [DOI] [PubMed] [Google Scholar]
- McNally RJ, Litz BT, Prassas A, Shin LM, & Weathers FW (1994). Emotional priming of autobiographical memory in post-traumatic stress disorder. Cognition and Emotion, 8, 351–367. doi: 10.1080/02699939408408946 [DOI] [Google Scholar]
- Monson CM, Gradus JL, Young-Xu Y, Schnurr PP, Price JL, & Schumm JA (2008). Change in posttraumatic stress disorder symptoms: Do clinicians and patients agree? Psychological Assessment, 20, 131–138. doi: 10.1037/1040-3590.20.2.131 [DOI] [PubMed] [Google Scholar]
- Moradi AR, Moshirpanahi S, Parhon H, Mirzaei J, Dalgleish T, & Jobson L (2014). A pilot randomized controlled trial investigating the efficacy of MEmory Specificity Training in improving symptoms of posttraumatic stress disorder. Behavior Research and Therapy, 56, 68–74. doi: 10.1016/j.brat.2014.03.002 [DOI] [PubMed] [Google Scholar]
- Mueller PA, & Oppenheimer DM (2014). The pen is mightier than the keyboard: Advantages of longhand over laptop note taking. Psychological Science, 25, 1159–1168. doi: 10.1177/0956797614524581 [DOI] [PubMed] [Google Scholar]
- Neshat-Doost HT, Dalgleish T, Yule W, Kalantari M, Ahmadi SJ, Dyregrov A, et al. (2013). Enhancing autobiographical memory specificity through cognitive training: An intervention for depression translated from basic science. Clinical Psychological Science, 1, 84–92. doi: 10.1177/2167702612454613 [DOI] [Google Scholar]
- Nixon RD, Ball SA, Sterk J, Best T, & Beatty L (2013). Autobiographical memory in children and adolescents with acute stress and chronic posttraumatic stress disorder. Behaviour Change, 30, 180–198. doi: 10.1017/bec.2013.17 [DOI] [Google Scholar]
- Porter S, & Peace KA (2007). The scars of memory: A prospective, longitudinal investigation of the consistency of traumatic and positive emotional memories in adulthood. Psychological Science, 18, 435–441. doi: 10.1111/j.1467-9280.2007.01918.x [DOI] [PubMed] [Google Scholar]
- Prins A, Bovin MJ, Kimerling R, Kaloupek DG, Marx BP, Pless Kaiser A, et al. (2015). The Primary Care PTSD Screen for DSM-5 (PC-PTSD-5). Instrument available from the National Center for PTSD; at www.ptsd.va.gov. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prins A, Bovin MJ, Smolenski DJ, Mark BP, Kimerling R, Jenkins-Guarnieri MA, et al. (2016). The Primary Care PTSD Screen for DSM-5 (PC-PTSD-5): Development and evaluation within a veteran primary care sample. Journal of General Internal Medicine, 31, 1206–1211. doi: 10.1007/s11606-016-3703-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qualtrics. (2018). Qualtrics [computer software], 2018, from https://www.qualtrics.com
- Quoidbach J, Mikolajczak M, & Gross JJ (2015). Positive interventions: An emotion regulation perspective. Psychological Bulletin, 141, 655–693. doi: 10.1037/a0038648 [DOI] [PubMed] [Google Scholar]
- Read JP, Radomski S, & Borsari B (2015). Associations among trauma, posttraumatic stress, and hazardous drinking in college students: Considerations for intervention. Current Addiction Reports, 2, 58–67. doi: 10.1007/s40429-015-0044-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reis HT, Smith SM, Carmichael CL, Caprariello PA, Tsai F-F, Rodrigues A, et al. (2010). Are you happy for me? How sharing positive events with others provides personal and interpersonal benefits. Journal of Personality and Social Psychology, 99, 311–329. doi: 10.1037/a0018344 [DOI] [PubMed] [Google Scholar]
- Resick PA, Monson CM, & Chard KM (2016). Cognitive Processing Therapy veteran/military version: Therapist’s manual. [Google Scholar]
- Richardson JTE (2011). Eta squared and partial eta squared as measures of effect size in educational research. Educational Research Review, 6, 135–147. doi: 10.1016/j.edurev.2010.12.001 [DOI] [Google Scholar]
- Rosenberg M (1965). Society and the adolescent self-image. Princeton, NJ: Princeton University Press. [Google Scholar]
- Rosenberg M (1979). Conceiving the self New York: Basic Books. [Google Scholar]
- Rothman KJ (1990). No adjustments are needed for multiple comparisons. Epidemiology, 1, 43–46. [PubMed] [Google Scholar]
- Rowsome K, Comerford M, Mottram S, Samuel D, & Stokes M (2016). Movement control testing of older people in community settings: Description of a screening tool and intrarater reliability. Working Papers in Health Sciences, 1, 1–12. [Google Scholar]
- Rubin DC, Berntsen D, & Bohni MK (2008). A memory-based model of posttraumatic stress disorder: Evaluating basic assumptions underlying the PTSD diagnosis. Psychological Review, 115, 985–1011. doi: 10.1037/a0013397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rusting CL, & DeHart T (2000). Retrieving positive memories to regulate negative mood: Consequences for mood-congruent memory. Journal of Personality and Social Psychology, 78, 737–752. doi: 10.1037/0022-3514.78.4.737 [DOI] [PubMed] [Google Scholar]
- Rusting CL, & Larsen RJ (1998). Personality and cognitive processing of affective information. Personality and Social Psychology Bulletin, 24, 200–213. doi: 10.1177/0146167298242008 [DOI] [Google Scholar]
- Rytwinski NK, Scur MD, Feeny NC, & Youngstrom EA (2013). The co-occurrence of major depressive disorder among individuals with posttraumatic stress disorder: A meta-analysis. Journal of Traumatic Stress, 26, 299–309. doi: 10.1002/jts.21814 [DOI] [PubMed] [Google Scholar]
- Savitz DA, & Olshan AF (1995). Multiple comparisons and related issues in the interpretation of epidemiologic data. American Journal of Epidemiology, 142, 904–908. doi: 10.1093/oxfordjournals.aje.a117737 [DOI] [PubMed] [Google Scholar]
- Schafer JL, & Graham JW (2002). Missing data: Our view of the state of the art. Psychological Methods, 7, 147–177. doi: 10.1037//1082-989X.7.2.147 [DOI] [PubMed] [Google Scholar]
- Schnurr PP (2017). Focusing on trauma-focused psychotherapy for posttraumatic stress disorder. Current Opinion in Psychology, 14, 56–60. doi: 10.1016/j.copsyc.2016.11.005 [DOI] [PubMed] [Google Scholar]
- Siegel S, & Castellan NJ (1988). Nonparametric statistics for the behavioral sciences (2nd ed.). New York: NY: McGraw-Hill. [Google Scholar]
- Singer JA, Blagov P, Berry M, & Oost KM (2013). Self-defining memories, scripts, and the life story: Narrative identity in personality and psychotherapy. Journal of Personality, 81, 569–582. doi: 10.1111/jopy.12005 [DOI] [PubMed] [Google Scholar]
- Sloan DM, Marx BP, Bovin MJ, Feinstein BA, & Gallagher MW (2012). Written exposure as an intervention for PTSD: A randomized clinical trial with motor vehicle accident survivors. Behaviour Research and Therapy, 50, 627–635. doi: 10.1016/j.brat.2012.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smorti A, & Fioretti C (2016). Why narrating changes memory: A contribution to an integrative model of memory and narrative processes. Integrative Psychological and Behavioral Science, 50, 296–319. doi: 10.1007/s12124-015-9330-6 [DOI] [PubMed] [Google Scholar]
- Steel C, van der Gaag M, Korrelboom K, Simon J, Phiri P, Baksh MF, et al. (2015). A randomised controlled trial of positive memory training for the treatment of depression within schizophrenia. BMC Psychiatry, 15, 85–90. doi: 10.1186/s12888-015-0453-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steptoe A, Dockray S, & Wardle J (2009). Positive affect and psychobiological processes relevant to health. Journal of Personality, 77, 1147–1176. doi: 10.1111/j.1467-6494.2009.00599.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutherland K, & Bryant RA (2007). Autobiographical memory in posttraumatic stress disorder before and after treatment. Behavior Research and Therapy, 45, 2915–2923. doi: 10.1016/j.brat.2007.08.009 [DOI] [PubMed] [Google Scholar]
- Sutherland K, & Bryant RA (2008). Autobiographical memory and the self-memory system in posttraumatic stress disorder. Journal of Anxiety Disorders, 22, 555–560. doi: 10.1016/j.janxdis.2007.03.008 [DOI] [PubMed] [Google Scholar]
- Sutin AR, & Robins RW (2007). Phenomenology of autobiographical memories: The Memory Experiences Questionnaire. Memory, 15, 390–314. doi: 10.1080/09658210701256654 [DOI] [PubMed] [Google Scholar]
- Tarrier N (2010). Broad Minded Affective Coping (BMAC): A “positive” CBT approach to facilitating positive emotions. International Journal of Cognitive Therapy, 3, 64–76. doi: 10.1521/ijct.2010.3.1.64 [DOI] [Google Scholar]
- Tukey JW (1949). Comparing individual means in the analysis of variance. Biometrics, 99–114. doi: 10.2307/3001913 [DOI] [PubMed] [Google Scholar]
- Tull MT, Bornovalova MA, Patterson R, Hopko DR, & Lejuez CW (2008). Analogue research In McKay D (Ed.), Handbook of Research Methods in Abnormal and Clinical Psychology (pp. 61–78). Thousand Oaks, CA: Sage Publications, Inc. [Google Scholar]
- Van Overschelde JP, Rawson KA, & Dunlosky J (2004). Category norms: An updated and expanded version of the norms. Journal of Memory and Language, 50, 289–335. doi: 10.1016/j.jml.2003.10.003 [DOI] [Google Scholar]
- Watson D, Clark LA, & Tellegen A (1988). Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology, 54, 1063–1070. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Blake DD, Schnurr PP, Kaloupek DG, Marx BP, & Keane TM (2013). The Life Events Checklist for DSM-5 (LEC-5). Instrument available from the National Center for PTSD; at www.ptsd.va.gov. [Google Scholar]
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, & Schnurr PP (2013). The PTSD Checklist for DSM-5 (PCL-5). Scale available from the National Center for PTSD; at www.ptsd.va.gov. [Google Scholar]
- Williams JM, & Broadbent K (1986). Autobiographical memory in suicide attempters. Journal of Abnormal Psychology, 95, 144–149. doi: 10.1037/0021-843X.95.2.144 [DOI] [PubMed] [Google Scholar]
- Wortmann JH, Jordan AH, Weathers FW, Resick PA, Dondanville KA, Hall-Clark B, et al. (2016). Psychometric analysis of the PTSD Checklist-5 (PCL-5) among treatment-seeking military service members. Psychological Assessment, 28, 1392–1403. doi: 10.1037/pas0000260 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.