Abstract
Background
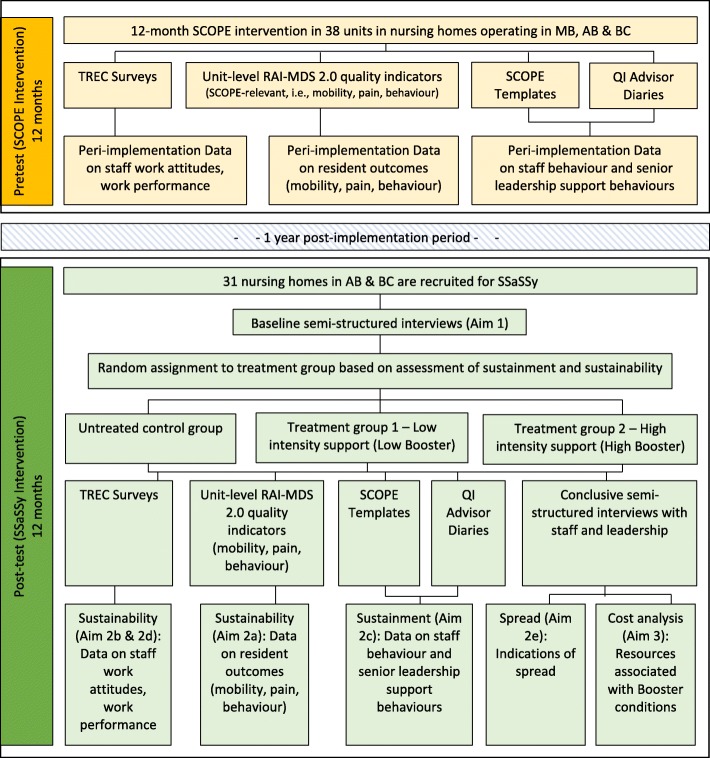
Implementation scientists and practitioners, alike, recognize the importance of sustaining practice change, however post-implementation studies of interventions are rare. This is a protocol for the Sustainment, Sustainability and Spread Study (SSaSSy). The purpose of this study is to contribute to knowledge on the sustainment (sustained use), sustainability (sustained benefits), and spread of evidence-based practice innovations in health care. Specifically, this is a post-implementation study of an evidence-informed, Care Aide-led, facilitation-based quality-improvement intervention called SCOPE (Safer Care for Older Persons (in long-term care) Environments). SCOPE has been implemented in nursing homes in the Canadian Provinces of Manitoba (MB), Alberta (AB) and British Columbia (BC). Our study has three aims: (i) to determine the role that adaptation/contextualization plays in sustainment, sustainability and spread of the SCOPE intervention; (ii) to study the relative effects on sustainment, sustainability and intra-organizational spread of high-intensity and low-intensity post-implementation “boosters”, and a “no booster” condition, and (iii) to compare the relative costs and impacts of each booster condition.
Methods/design
SSaSSy is a two-phase mixed methods study. The overarching design is convergent, with qualitative and quantitative data collected over a similar timeframe in each of the two phases, analyzed independently, then merged for analysis and interpretation. Phase 1 is a pilot involving up to 7 units in 7 MB nursing homes in which SCOPE was piloted in 2016 to 2017, in preparation for phase 2. Phase 2 will comprise a quasi-experiment with two treatment groups of low- and high-intensity post-implementation “boosters”, and an untreated control group (no booster), using pretests and post-tests of the dependent variables relating to sustained care and management practices, and resident outcomes. Phase 2 will involve 31 trial sites in BC (17 units) and AB (14 units) nursing homes, where the SCOPE trial concluded in May 2019.
Discussion
This project stands to advance understanding of the factors that influence the sustainment of practice changes introduced through evidence-informed practice change interventions, and their associated sustainability. Findings will inform our understanding of the nature of the relationship of fidelity and adaptation to sustainment and sustainability, and afford insights into factors that influence the intra-organizational spread of practice changes introduced through complex interventions.
Keywords: Long-term care, Nursing homes, Sustainability, Quality improvement, Evidence-based care practice
Contributions to the literature.
Post-implementation studies of intervention sustainability, like that described in this protocol, are rare.
Once intervention implementation supports are removed, the effects of interventions are susceptible to natural decay and our understanding of how to sustain the use of the new knowledge conveyed in interventions, post-implementation and long-term, is poor.
This protocol describes a study that will contribute to knowledge on the sustainment (sustained use), sustainability (sustained benefits), and spread of evidence-based practice innovations in health care.
The study will be situated in the under-studied institutional long-term care sector.
Background
Considerable investment is made to generate research knowledge intended to improve the quality and delivery of health care. Knowledge of this type, particularly when it is complex, is frequently conveyed via evidence-based practice interventions, and the costs expended to implement these interventions are similarly substantial [1]. Once intervention implementation “supports” are removed, the initial effects obtained through these interventions are susceptible to natural decay [2–4]. The long-term durable sustainment of evidence-based changes to practice is challenging [1, 5, 6].
While sustainability has been identified as “one of the most significant translational research problems of our time” (1: 2), post-implementation studies of practice change sustainability in health care are rare [7–11] and so it follows that our understanding of the factors that influence sustainability is generally poor. Failure to sustain evidence-based changes or innovations to practice means that the intended improvements to care are short-lived, that the practice innovations’ further scale-up and spread is unlikely, and that real losses are incurred on research investment, often made with public funds. This protocol describes a study that aims to contribute to our understanding of the inter-related phenomena of sustainability, sustainment, and spread of evidence-informed, complex practice change interventions.
Unpacking the concept of sustainability
While the concept of sustainability is still maturing [3, 4, 12], work in this area has recently acknowledged a useful distinction between sustainability and sustainment [4, 8]. With a focus on lasting benefits, sustainability generally refers to the extent to which “an evidence-based intervention can deliver its intended benefits over an extended period of time after external support from the donor agency is terminated” ([13]: 118); whereas, sustainment refers to the continued enactment of processes, practices, or work routines that are conveyed and learned through an intervention [4, 8]. While the concept of spread is generally discussed separately [14], we suggest that there is likely a link between spread and the concepts of sustainability and sustainment, given that the spread of the practices and benefits introduced through an intervention, from one part of an organization to other parts or from one organization to another, is unlikely to take place without some degree of retention of these processes and benefits within the originating unit or organization. As with sustainability, the importance of understanding the processes and factors that influence the spread of healthcare innovations, including practice innovations, are highlighted in the implementation literature, albeit separate from the literature on sustainability [9, 15, 16].
Approaches to studying sustainability: fidelity versus adaptation
To date, studies of sustainment and sustainability invoke one of two dominant and competing approaches: the fidelity approach, and the adaptation approach [3, 7]. The fidelity approach focuses on implementation fidelity and is the most common approach used to examine sustainability. Fidelity is defined as the extent to which an intervention program follows the originally intended implementation plan and faithfully delivers the research-informed components of the intervention [11, 17]. This approach contends that deviation from the intended intervention content and delivery protocols during implementation—that is, “program drift” and “low fidelity”—will inevitably lead to diminished benefits/outcomes both during and after implementation, once intervention support is withdrawn [8, 18].
By contrast, the adaptive approach ascribes importance to the co-evolution of the intervention and the organizational context into which it is introduced [7]. This approach suggests that overemphasis on fidelity and adherence, “relative to generalizability and adaptation”, increases the risk of creating interventions—including practice changes and the processes to effect them—that will not “fit” within complex or changeable settings ([8]: 2), and that while changes to the intervention may reduce fidelity they may lead to improved fit to local context and enhanced outcomes/benefits [8, 9, 18, 19].
In this study, fidelity versus adaptation is of interest to us to the extent that it is, or is not, related to post-implementation sustainment and sustainability of practice change. High implementation fidelity during an intervention may contribute to sustained use and benefits. Conversely, the adaptive perspective suggests that sustainability and sustainment is achieved in organizations that are adept at striking a balance between fidelity and responsiveness to the implementation context. The bottom line is that what is done during implementation, in addition to what is done afterwards, is thought to affect the sustainment, sustainability and spread of practice changes conveyed through an intervention—but we do not know precisely how. Work to further our understanding of relationships amongst fidelity, adaptation, sustainment, sustainability, and spread is needed and there is almost no literature on these dynamics. SSaSSy will contribute to this understanding.
Study context
SSaSSy is a post-implementation study of sustainment (continued use), sustainability (lasting benefits), and spread (beyond the initial implementation setting) of the practice changes conveyed through an evidence-informed, Care Aide-led, facilitation-based quality-improvement intervention called SCOPE (Safer Care for Older Persons (in long-term care) Environments) that is the focus of a clinical trial being conducted in in Canadian nursing homes operating in the Provinces of Manitoba (MB), Alberta (AB) and British Columbia (BC) [NCT03426072]. In SCOPE, HCA-led teams lead quality-improvement initiatives focussing on one of three resident care areas identified as priorities by experts in long-term care, i.e., mobility, pain, and behavior [20]. The SCOPE intervention was piloted in nursing homes in AB and BC over 2010-2011. The impacts of the SCOPE intervention are described in several published articles:
In Norton et al. [21], the SCOPE pilot was shown to meet its primary objective of demonstrating the feasibility and utility of implementing the intervention in nursing homes relying upon the leadership of HCAs, and engagement of professional staff and leadership in facilitative roles. Specifically, of the 10 HCA-led QI teams in nursing homes that participated in the SCOPE pilot, 7 succeeded in learning and applying the improvement model and methods for local measurement, with 5 of the 10 teams showing measurable improvement in the chosen clinical areas.
These impacts were corroborated in a follow-up study that examined the sustainability of elements of the SCOPE pilot [22]. In this article, sustained differences between participating/intervention units, and non-participating units, were observed in outcomes relating to quality-improvement activities (i.e., continuation of work according to the improvement model and principles learned in SCOPE), HCA empowerment, and satisfaction with quality of work life.
As part of the SCOPE clinical trial, SCOPE was implemented in 7 units in MB nursing homes over 2017, somewhat earlier than the intervention was implementation in participating BC and AB units/homes. While the data for the MB homes will be analyzed in conjunction with that collected for homes in BC and AB, a recent retrospective qualitative analysis of the implementation experiences [23] of administrative leaders (sponsors), professional staff, and QI team participants in MB homes demonstrates effects akin to those observed in the SCOPE pilot. In addition to accruing observable benefits to residents who were the subjects of the QI initiatives formulated by the HCA-led QI teams in participating units in each MB home, SCOPE was observed to change the expectations and behaviors on the part of administrative leaders, professional staff, and—importantly—HCAs relating to their abilities to conduct small-scale, unit-level, evidence-informed quality-improvement initiatives [23].
Both SCOPE and SSaSSy are situated within a larger program of research, Translating Research in Elder Care (TREC) [24]. TREC was initiated in 2007 and focuses on the influence of organizational context on resident quality of care and safety in 94 nursing homes in the three Western Canadian Provinces [24]. Both SCOPE and SSaSSy rely on TREC’s longitudinal database that includes data on staff behavior, attitudes and quality of worklife; leader behavior; work environment (context); and care unit and nursing home characteristics (e.g., unit size, facility owner-operator model). Data are collected routinely from all levels of nursing home staff, and quality of care measures are collected on a quarterly basis across the 94 homes at the unit level [25] via the Resident Assessment Instrument—Minimum Data Set, version 2.0 (RAI-MDS 2.0).
Study purpose and aims
SSaSSy focusses on a 1-year interval, 1 year after SCOPE implementation concludes. Phase 1 of SSaSSy is a pilot that will occur in 7 units in MB nursing homes where SCOPE was piloted over 2016–2017. The results of this pilot will inform the content of post-implementation “boosters”, designed to sustain or renew the application of the QI techniques and tools—the changes to care practice—conveyed through SCOPE. The relative effectiveness of the boosters compared to a no booster control will be tested in phase 2 in 31 more units in nursing homes in BC and AB, where SCOPE concluded in May 2019.
As a post-implementation study, SSaSSy presents a rare opportunity to systematically contribute to knowledge [22] on the sustainment and sustainability of complex practice changes conveyed through evidence-based interventions, and to examine spread—first, in the SCOPE pilot sites in MB and subsequently in the trial sites in BC and AB.
Specific aims of SSaSSy are:
To determine whether fidelity, site- or facility-initiated adaptation of aspects of the intervention, aspects of the implementing unit, and/or other aspects of nursing homes’ operations or structures, are associated with sustainment, sustainability and spread one year following implementation of practice changes conveyed through SCOPE.
- To explore the relative effects on sustainment, sustainability and intra-organizational spread of high- and low-intensity post-implementation “boosters” compared to “no booster”/natural decay; specifically, the extent to which there are:
- sustained or renewed improvements in resident outcomes in clinical areas of focus targeted by the SCOPE intervention (deteriorating mobility, pain, responsive behavior) (sustainability),
- sustained or renewed changes in staff behaviors (reported use of best practices, use of SCOPE components and processes) (sustainment),
- sustained or renewed changes to staff work attitudes (work engagement, psychological empowerment, burnout, job satisfaction) and outcomes (organizational citizenship behaviors) related to work performance (sustainability),
- sustained or renewed changes to senior leadership support behaviors relating to staff engagement in SCOPE (sustainment),
- indications of spread to other units within the SCOPE intervention sites, and its extent.
To compare the costs and effectiveness of each post-implementation support condition.
Approach/methods
SSaSSy is a two-phase mixed methods study. The overarching design is convergent, with qualitative and quantitative data collected over a similar timeframe in each of the two phases, analyzed independently, then merged, interpreted and reported by means of joint display [26].
Participating nursing home sites
SSaSSy will first take place in the nursing home units in MB that participated in the SCOPE pilot, and then in those in AB and BC that participated in the full SCOPE trial. These homes meet the inclusion criteria applied to the original SCOPE pilot, and trial: (i) the facility provides 24-h on-site housing and health care services care for older adults by professional (nursing) staff and others; (ii) the facility is registered with the provincial government; (iii) 90% of residents are aged 65 or over; (iv) RAI-MDS 2.0 has implemented since January 2011; (v) facility operations are conducted in the English language; (vi) urban facilities are located within designated health regions and within 110 km of the TREC-designated hub for the health region.
Phase 1
The first study phase, in MB, entails developing the content of the two post-implementation support conditions—low- and high-intensity “boosters”—through consultation with participants in the SCOPE pilot sites in MB nursing homes; piloting data collection instruments with SCOPE pilot site participants that explore factors relating to sustainability, sustainment and spread including fidelity and adaptation relevant to aim 1; piloting the low- and high-intensity “boosters” in up to 7 SCOPE pilot sites in MB while collecting quantitative and qualitative data relevant to aim 2 (sustainability, sustainment, spread); and piloting a data collection instrument intended to capture the costs related to each of the post-implementation support conditions.
SSaSSy booster content
The preliminary content of the low- and high-intensity boosters is informed by three prior studies relating to the SCOPE intervention [22, 23, 27] that highlight four components of the SCOPE pilot that appear to be highly relevant to its implementation: (i) the presence of team and senior sponsors who learn leadership skills intended for use in supporting the Care Aide-led unit QI Teams by securing resources; (ii) face-to-face “Learning Congresses” in which Teams build QI-related skills and where exchanges with care teams from other facilities enhance learning and team efficacy; (iii) quality advisors who fill both supportive and educational roles relating to applying QI techniques on the part of the QI Teams, and change management leadership coaching of sponsors; and (iv) the use of “setting aims” as an effective mechanism for changing QI Team members’ behavior. The mix of these booster components, and their intensities, will be further informed through a focus group consultation of 2–3 decision-makers familiar with the MB SCOPE pilot, 2–3 QI experts, and 2 researchers with expertise in implementation science.
SSaSSy booster pilot
The low- and high-intensity boosters will be piloted in up to 7 units in 7 MB homes (potentially 3 low-intensity booster units, 4 high-intensity booster units) for 7 months, starting June 2019. The pilot interval will be followed by data analysis and refinement of boosters where we will focus on: (i) assessing relationships between the boosters’ contents and sustainment, sustainability, and spread; (ii) the clarity of the booster content from the perspective of the QI Teams; and (iii) the adequacy of the modes of delivery. Quantitative and qualitative data will be collected during the pilot; see Table 1 for a summary of measures relevant to each study aim.
Table 1.
SSaSSy aims, measures and analyses
| Aim | Data/measures | Analysis | |
|---|---|---|---|
| Aim 1. Explore site adaptation and/or contextualization | Semi-structured in-person interviews with the QI Team lead, senior sponsor, and QI advisor | A hybrid approach of qualitative methods will be used, thematic analysis [28], which incorporates both an inductive approach that allows themes to emerge from the data [29] and a deductive a priori template-of-codes approach [30] based on research we review above. Audiotapes of the interviews will be transcribed verbatim and data analysis will be completed using line-by-line coding and constant comparative methods [31] | |
| Aim 2: Explore the relative effects of the high- and low-intensity boosters | 2a: Sustainability: Sustained or renewed improvements to quality of resident care | Unit-level quality indicators generated using RAI-MDS 2.0 data on resident outcomes (mobility, pain, behavior) | Run charts will be generated for the RAI-MDS data(i) collected SSaSSy start for each of the three quality indicators for each unit (RAI data elements MOB01/MOB1A; PAI0X/PAN01; BEHD4/BEHI4). For the clinical area on which QI Teams focus, we will analyze the relevant RAI-MDS quality indicator using statistical process control methods [32] and a procedure that members of our research team developed for the SCOPE proof of principle study [21] which categorizes control charts in terms of demonstrated changes to performance. |
| Notes: | |||
| (i) RAI-MDS 2.0 is a valid, reliable standardized assessment of resident outcomes that includes a comprehensive set of clinical outcomes and captures characteristics of nursing home residents and their care [33]. Each resident has a full assessment (~450 items) performed on admission, and a shorter (300 item) assessment is performed quarterly. These data are routinely collected from all 94 participating TREC sites, from which SCOPE study sites were drawn, and are the source of SSaSSy’s resident outcome data | |||
| 2b & 2d: Sustainment: Sustained or renewed changes in staff behavior and senior leadership support behaviors | SCOPE templates completed by QI Team leads. diaries and feedback reports completed by QI Advisors | SCOPE Templates(ii) will be analyzed, using document analysis [34, 35], at two junctures: analysis of the SCOPE Templates accrued over SCOPE implementation, and over the SSaSSy booster interval to determine peri-intervention fidelity and post-intervention fidelity, respectively. First, gross-grained assessments of the use/non-use of the templates (sustainment) by each QI Team will be made (i.e., were templates complete and posted on intranet site available to Teams). Thematic analysis (see above) will then be used to analyze the contents of the QI Team templates, as well as the QI advisor diaries and feedback reports(iii) | |
| 2c: Sustainability: Sustained or renewed changes to staff work attitudes and outcomes related to work performance | TREC HCA Survey [36] | While quantitative data will be collected and analyzed over the course of the project, SSaSSy likely will not be adequately powered for statistical inference. Descriptive statistics including statistics of central tendency, dispersion, and standard deviation will be computed for each unit-level variable, for each booster arm collected through the TREC Survey waves. However, if changes in the primary outcome of the SCOPE intervention, Care Aide-reported conceptual use of best practices, are sufficient over the booster interval (e.g., an effect size of 0.29), we will use one-way ANOVA (repeated measures, within-between interaction) to test for “pre–post” differences in the means of each variable within and between groups/booster arms, followed by Tukey–Kramer test for significant differences between all pairs of groups if appropriate (where distributions are not normal the Kruskal–Wallis test will be used, and where data are heteroscedastic Welch's ANOVA will be used). In the more likely event that changes of this magnitude do not occur, we will compute p-values by time point before and after the SSaSSy booster interval. We are constrained in our sample size because we are studying the post-implementation of a trial with a fixed number of experimental sites. | |
| (ii) SCOPE Templates refer to documents introduced during SCOPE implementation, in the all-team Learning Congresses, that are designed to assist care aide-led QI Teams in planning and managing their QI projects, and measuring and reporting their progress against their project aims | |||
| (iii) The quality advisors keep diaries in which they prepared structured summaries of each interaction with the QI Teams, whether face-to-face or telephone, outside of the all-team Learning Congresses. Quality advisors also prepare written, structured, quarterly feedback reports for each QI Team | |||
| 2e: Spread: Indications of spread to other units within the SCOPE intervention sites | Semi-structured in-person interview with the QI Team lead, senior sponsor, and QI advisor | As above | |
| Aim 3: Compare the effectiveness and costs of post-implementation support arms | Documentation of resources and associated costs for low- and high-booster conditions | This cost analysis is exploratory in nature. We plan a simple, disaggregated reporting of costs. We will report the intervention costs (costs to deliver the boosters) separately from the costs incurred by the participating units. Each unit will report their incurred costs for staff, training and materials and supplies. Disaggregated presentation will allow units to understand what is driving the costs and identify possible areas where costs could be modified within the overall intervention | |
Phase 2
The second study phase will use a quasi-experimental design [37] to evaluate the relative effectiveness of the three post-implementation support conditions: two treatment groups (low-, and high-intensity post-implementation boosters) and an untreated control group (no booster). Pretest and post-test data [37] relating to sustainment and sustainability will be collected through TREC surveys and via unit-level RAI-MDS 2.0 quality indicators. Phase 2 will begin in June 2020 and involve trial sites in BC (17 units) and AB (14 units), where SCOPE implementation concluded in May 2019. Specifically, the untreated control group (10 units) will receive no post-implementation support, one treatment group (10 units) will be provided with a low-intensity booster, and the second treatment group (11 units) will receive a high-intensity booster.
Assignment to treatment and control groups
We plan to use a cut-off-based random assignment strategy [37]. First, the extent to which SCOPE-conveyed practices have been sustained just prior to SSaSSy start-up in BC and AB, nursing homes will be assessed through “baseline interviews” with the team and senior sponsors. This will be followed by random assignment of those with high levels of sustained activity, and those with low levels, to each of the low-intensity booster, high-intensity booster, and untreated control groups. This approach will be piloted in phase 1 amongst participating units in MB nursing homes.
Inclusion of non-equivalent dependent variables for each group
The quasi-experiment design will be further strengthened by including non-equivalent dependent variables, in addition to the target outcomes variables. We have a ready way in which to do this: each QI Team is instructed to focus on one of either resident mobility, pain management or reducing responsive behaviors, and we collect RAI-MDS 2.0 quality indicator data (see Table 1, aim 2a) on each of these clinical areas. For a QI Team focussing on mobility, for example, we consider the measure based on mobility indicators MOB01 and MOB1A to be our target outcome variable, while PAI0X/PAN01; and BEHD4/BEHI4 will serve as our non-equivalent dependent variables. That is, while in this example neither the pain nor behavior measures would be predicted to change because of the treatment (SSaSSy), they would be expected to respond similarly to contextually important internal validity threats in the same way as the mobility target outcome.
Measures and analysis
The relationships among the study aims, measures and analyses are summarized in Table 1.
Integration
In this mixed methods study, quantitative and qualitative findings will be integrated at the interpretation and reporting stage [26, 38]. Independent analyses of the qualitative and quantitative data will serve to organize the data in a format based on thematic relevance (sustainability, sustainment, spread, influencing factors) that permit merging and subsequent higher order integration. This will be accomplished in two ways: first, the quantitative and qualitative data will be integrated using a joint display. Second, a narrative approach will be used to describe the quantitative and qualitative results thematically. The narrative will offer intra-group and inter-group comparisons within and between booster arms. Figure 1 offers a flow diagram for phase 2.
Fig. 1.
Phase 2 flow diagram
Discussion
This study was developed in response to calls for studies that advance our understanding of the phenomena of post-implementation sustainability and sustainment of knowledge conveyed through evidence-based interventions [7, 8]. Failure to sustain evidence-based innovations to practice means that the intended improvements to care are short-lived, and that often considerable investments of health human resources are forfeit. We will also examine the phenomena of spread, as it seems reasonable to expect spread to be associated with sustainability and/or sustainment.
Strengths and limitations
A significant strength of this study is that it relies upon multiple methods and multiple and diverse sources of data, with the survey and indicator data relying upon well-established, validated instruments with good psychometric properties. The quasi-experiment in phase 2 is strengthened by: a cut-off-based random assignment of units to treatment and untreated control groups; pretest and post-test measures; the inclusion of non-equivalent dependent variables for each of the three groups; and the inclusion of two comparison treatment groups and an untreated control group.
We are constrained in our sample size, because we are studying the post-implementation of a trial with a fixed number of experimental sites and therefore will not be adequately powered for statistical inference and must rely on descriptive statistics to examine the relative effectiveness of the booster and no booster control groups in phase 2.
Conclusion
This project stands to advance the state of the science about factors that influence the sustained use (sustainment) of practice changes conveyed through interventions, and the associated sustained benefits of those changes to resident and staff outcomes (sustainability). Our findings will also inform discussion of the relevance of fidelity and adaptation to sustainment and sustainability, and offer insights into the factors that influence intra-organizational spread of complex interventions [39]. Finally, we will gain insights into the relative effects of differing intensities of post-implementation boosters vs. a no-booster untreated group, on the sustainment, sustainability and intra-organizational spread of practice changes introduced through SCOPE, in addition to the relative costs of these booster treatments. Importantly, SSaSSy focusses on the long-term effectiveness and sustainability of an intervention applied to long-term care settings, where post-implementation phenomena have not been studied, and where there is increasing concern for the costs, quality and sustainability of older adult care [40].
Acknowledgements
We extend our sincere thanks to Ms. Jennifer Pietracci, Mr. Don McLeod, and Dr. Charlotte Berendonk for their thoughtful inputs into the logistics and operational planning for phase 1.
Abbreviations
- AB
Alberta
- BC
British Columbia
- HCA
Health care aid
- MB
Manitoba
- SCOPE
Safer Care for Older Persons (in long-term care) Environments
- SSaSSy
Sustainment, Sustainability, and Spread Study
- TREC
Translating Research in Elder Care
Authors’ contributions
WB, AW, and CE designed the study with significant input from LG, MD, and LC. AW and CE lead the SCOPE trial study that SSaSSy follows upon; CE leads the TREC program of research. LC, MH, CE, PN, and AW prepared a report on sustainability and spread of the original pilot of the SCOPE intervention that informed the original grant proposal on which this protocol is based. LG, CE, WB, PN, MD, JKS, AE, and AW prepared a paper on the implementation of the SCOPE pilot which informs the booster content. MD, LG, PN, MH, LC, JK, AE, FC, CR, and SC contributed to the design of the study, to the revisions and grant proposal resubmissions to the funder, and to multiple versions of this protocol prior to its submission for publication. LM, MD, YS, LG, JKS, JK, and MH contributed importantly to the theoretical and practical considerations relating to phase 1; MD and LM in particular played a major role in the conceptualization of this phase. All authors read and approved the final manuscript prior to submission.
Funding
Funding for this study has been provided by the Canadian Institutes for Health Research (CIHR), Grant # 201803PJT-400653-KTR-CEAA-107836.
Availability of data and materials
Not applicable.
Ethics approval and consent to participate
Ethics approval for phase 1 of this study has been obtained from the University of Toronto, University of Manitoba, and the Winnipeg Regional Health Authority research ethics boards. In phase 2, we will seek ethics approval from the University of Alberta, the University of British Columbia, and applicable regional operational review boards.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Proctor E, Luke D, Calhoun A, McMillen C, Brownson R, McCrary S, Padek M. Sustainability of evidence-based healthcare: Research agenda, methodological advances, and infrastructure support. Implement Sci. 2015;10:88. doi: 10.1186/s13012-015-0274-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Scheirer M. Is sustainability possible? A review and commentary on empirical studies of program sustainability. Am J Eval. 2005;26:3. doi: 10.1177/1098214005278752. [DOI] [Google Scholar]
- 3.Stirman SW, Kimberly J, Cook N, Calloway A, Castro F, Charns M. The sustainability of new programs and innovations: A review of the empirical literature and recommendations for future research. Implement Sci. 2012;7:17. doi: 10.1186/1748-5908-7-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fleiszer A, Semenic S, Ritchie J, Richer M-C, Denis J-L. An organizational perspective on the long-term sustainability of nursing best practice guidelines program: A case study. BMC Health Serv Res. 2015;15:535. doi: 10.1186/s12913-015-1192-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Davies B, Tremblay D, Edwards N. Sustaining evidence-based practice systems and measuring the impacts. Eval Impact Implement Evid-Based Pract. 2010;17:166–188. [Google Scholar]
- 6.Virani T, Lemieux-Charles L, Davis D, Berta W. Sustaining change: Once evidence-based practices are transferred, what then? Healthc Q. 2009;12:1. doi: 10.12927/hcq.2009.20420. [DOI] [PubMed] [Google Scholar]
- 7.Shelton RC, Cooper BR, Stirman SW. The sustainability of evidence-based interventions and practices in public health and health care. Annu Rev Public Health. 2018;39:55–76. doi: 10.1146/annurev-publhealth-040617-014731. [DOI] [PubMed] [Google Scholar]
- 8.Chambers DA, Glasgow RE, Stange KC. The dynamic sustainability framework: addressing the paradox of sustainment amid ongoing change. Implement Sci. 2013;8:117. doi: 10.1186/1748-5908-8-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Greenhalgh T, Glen R, MacFarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q. 2004;82(4):581–629. doi: 10.1111/j.0887-378X.2004.00325.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Duckers MLA, Wagner C, Vos L, Groenewegen PP. Understanding organisational development, sustainability, and diffusion of innovations within hospitals participating in a multilevel quality collaborative. Implement Sci. 2011;6:18. doi: 10.1186/1748-5908-6-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Carroll C, Patterson M, Wood S, Booth A, Rick J, Balain S. A conceptual framework for implementation fidelity. Implement Sci. 2007;2:40. doi: 10.1186/1748-5908-2-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Johnson AM, Moore JE, Chambers DA, Rup J, Dinyarian C, Straus SE. How do researchers conceptualize and plan for the sustainability of their NIH R01 implementation projects? Implement Sci. 2019;14(1):50. doi: 10.1186/s13012-019-0895-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rabin BA, Brownson RC, Haire-Joshu D, Kreuter MW, Weaver NL. A glossary for dissemination and implementation research in health. J Public Health Manag Pract. 2008;14(2):117–123. doi: 10.1097/01.PHH.0000311888.06252.bb. [DOI] [PubMed] [Google Scholar]
- 14.Davies B, Edwards N. Sustaining knowledge use. Knowledge Transl Health Care. 2013;2:237–248. doi: 10.1002/9781118413555.ch23. [DOI] [Google Scholar]
- 15.Dearing JW. Evolution of diffusion and dissemination theory. J Public Health Manag Pract. 2008;14(2):99–108. doi: 10.1097/01.PHH.0000311886.98627.b7. [DOI] [PubMed] [Google Scholar]
- 16.Dearing JW. Applying diffusion of innovation theory to intervention development. Res Soc Work Pract. 2009;19(5):503–518. doi: 10.1177/1049731509335569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dusenbury L, Brannigan R, Falco M, Hansen WB. A review of research on fidelity of implementation: implications for drug abuse prevention in school settings. Health Educ Res. 2003;18(2):237–256. doi: 10.1093/her/18.2.237. [DOI] [PubMed] [Google Scholar]
- 18.Hasson H, Blomberg S, Dunér A. Fidelity and moderating factors in complex interventions: a case study of a continuum of care program for frail elderly people in health and social care. Implement Sci. 2012;7(1):23. doi: 10.1186/1748-5908-7-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fraser MW, Richman JM, Galinsky MJ, Day SH. Intervention research: Developing social programs. Oxford university press; 2009.
- 20.Cranley LA, Norton PG, Cummings GG, Barnard D, Batra-Garga N, Estabrooks CA. Identifying resident care areas for a quality improvement intervention in long-term care: a collaborative approach. BMC Geriatr. 2012. 10.1186/1471-2318-12-59. [DOI] [PMC free article] [PubMed]
- 21.Norton Peter, Cranley Lisa, Cummings Greta, Estabrooks Carole. Report of a pilot study of quality improvement in nursing homes led by healthcare aides. European Journal for Person Centered Healthcare. 2013;1(1):255. doi: 10.5750/ejpch.v1i1.658. [DOI] [Google Scholar]
- 22.Cranley LA, Hoben M, Yeung J, Estabrooks CA, Norton PG, Wagg A. SCOPEOUT: sustainability and spread of quality improvement activities in long-term care-a mixed methods approach. BMC Health Serv Res. 2018;18(1):174. doi: 10.1186/s12913-018-2978-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ginsburg L, Easterbrook A, Berta W, Norton P, Doupe M, Knopp-Sihota J, et al. Implementing frontline worker–led quality improvement in nursing homes: getting to “how”. Jt Comm J Qual Patient Saf. 2018;44(9):526–535. doi: 10.1016/j.jcjq.2018.04.009. [DOI] [PubMed] [Google Scholar]
- 24.Estabrooks CE, Squires JE, Cummings GG, Teare GF, Norton PG. Study protocol for the translating research in elder care (TREC): building context – an organizational monitoring program in long-term care project (project one) Implement Sci. 2009;4:52. doi: 10.1186/1748-5908-4-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Estabrooks CE, Morgan DG, Squires JE, Boström A-M, Slaughter SE, Cummings GG, Norton PG. The care unit in nursing home research: Evidence in support of a definition. BMC Med Res Methodol. 2011;11:46. doi: 10.1186/1471-2288-11-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fetters MD, Curry LA, Creswell JW. Achieving integration in mixed methods designs-principles and practices. Health Serv Res. 2013;48(6 Pt 2):2134–2156. doi: 10.1111/1475-6773.12117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hoben M, Norton PG, Ginsburg LR, Anderson RA, Cummings GG, Lanham HJ, et al. Improving nursing home care through feedback on PerfoRMance data (INFORM): protocol for a cluster-randomized trial. Trials. 2017;18(1):9. doi: 10.1186/s13063-016-1748-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fereday J, Muir-Cochrane E. Demonstrating rigor using thematic analysis: A hybrid approach of inductive and deductive coding and theme development. Int J Qual Methods. 2006;5(1):1–11. doi: 10.1177/160940690600500107. [DOI] [Google Scholar]
- 29.Boyatzis R. Transforming qualitative information: Thematic analysis and code development. Thousand Oaks, CA: Sage; 1998. [Google Scholar]
- 30.Crabtree B, Miller W. A template approach to text analysis: Developing and using codebooks. In: Crabtree B, Miller W, editors. Doing qualitative research. Newbury Park, CA: Sage; 1999. pp. 163–177. [Google Scholar]
- 31.Auerbach C, Silverstein LB. Qualitative data: An introduction to coding and analysis. NYU press; 2003.
- 32.Thor J, Lundberg J, Ask J, Olsson J, Carli C, Harenstam KP, Brommels M. Application of statistical process control in healthcare improvement: Systematic Review. Qual Safety Health Care. 2007;16(5):387–399. doi: 10.1136/qshc.2006.022194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Poss J, Jutan N, Hirdes J, Fries BE, Morris JN, Teare G, Reidel K. A review of evidence on the reliability and validity of Minimum Data Set data. Healthc Manag Forum. 2008;21(1):33–39. doi: 10.1016/S0840-4704(10)60127-5. [DOI] [PubMed] [Google Scholar]
- 34.Saldana J. Fundamentals of qualitative research. 2011. [Google Scholar]
- 35.Miles MB, Huberman AM, Huberman MA, Huberman M. Qualitative data analysis: An expanded sourcebook. 1994. [Google Scholar]
- 36.Cranley LA, Norton PG, Cummings GG, Barnard D, Estabrooks CA. SCOPE: Safer care for older persons (in residential) environments: A study protocol. Implement Sci. 2011;6(1):71. doi: 10.1186/1748-5908-6-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shadish WR, Cook TD, Campbell DT. Experimental and quasi-experimental designs for generalized causal inference. 2002. [Google Scholar]
- 38.Creswell JW, Clark VL. Designing and conducting mixed methods research. Sage publications; 2017.
- 39.Scheirer M, Dearing J. An agenda for research on the sustainability of public health programs. Am J Public Health. 2011;101:11. doi: 10.2105/AJPH.2011.300193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hébert R. Research on aging: Providing evidence for rescuing the Canadian health care system: (Brief submitted to the Commission on the Future of Health Care in Canada May 28, 2002) Can J Aging. 2002;21(3):343–347. doi: 10.1017/S0714980800001665. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.