Abstract
Purpose
The main objective of this study was to retrospectively evaluate the clinical and radiological outcomes of acute (AMF) and chronic Monteggia fractures (CMF) in children treated by closed or open reduction and external fixation (EF).
Methods
This is a retrospective review of 26 patients with Monteggia fracture. Patients with AMF (time between trauma and surgery less than two weeks) were treated by closed reduction and EF of the ulna (Group A; 15 patients) while those with CMF (time between trauma and surgery more than three weeks) were managed by closed or open reduction and EF of the ulna (Group B; 11 patients). Clinical outcome was evaluated with radiography and the short version of the Disabilities of the Arm, Shoulder and Hand outcome questionnaire (Quick DASH). Complications were recorded in both groups.
Results
No secondary displacement, wire migration, consolidation delays, nonunion, malunion or re-fracture was noted. However, one patient in Group A (6.7%) developed heterotopic ossification of the ulna; the final functional outcome was good (Quick DASH score: 18.2). One case of postoperative redislocation of the radial head was detected in Group B (9.1%). Two patients (7.6%) developed transient pin tract infection. Despite the fact that 16 out of 26 patients (six in Group A and ten in Group B) complained of the clinical appearance and/or had intermittent residual pain on the injured side, the results were essentially the same between the two groups of patients (p > 0.05).
Conclusion
EF is an alternative for the management of acute and chronic paediatric Monteggia fractures. It provides satisfactory radiological and clinical outcomes with relatively low rates of complications.
Level of evidence
IV
Keywords: Monteggia fracture, acute, chronic, children, functional outcome
Introduction
Giovanni Battista Monteggia (1762 to 1815) first described the association between ulnar fracture and radial head dislocation.1 The Monteggia fracture is a relatively rare injury accounting for approximately 1% of all paediatric upper extremity fractures.2Acute Monteggia fracture (AMF) should be treated once detected.3 If the fracture goes undetected and/or is not promptly treated, it may lead to ulnar malunion and persistent radial head dislocation with subsequent loss of function, pain, degenerative arthritis and, in some cases, late neuropathy.4,5 Moreover, if surgical treatment is performed at this late stage, outcome is generally poorer compared with acute lesions treated promptly.6
The main goals of treatment of both AMF and chronic Monteggia fracture (CMF) are to achieve stable reduction of radial head dislocation and to restore elbow movement.5-7 In order to achieve such goals, several surgical techniques are available depending on the timing of surgery. In particular, reduction and ulnar fixation by casting, elastic stable intramedullary nailing or screw and plate are the treatment of choice for acute lesions.5,8,9 On the other hand, closed or open reduction and ulnar osteotomy with or without annular ligament reconstruction are often required for CMF.10-13
There are a few reports describing the management of AMF and CMF in children by closed or open reduction and lengthening and/or angulation of the ulna with an external fixator (EF).14-19 Moreover, no published studies on the surgical management of AMF and CMF in children have evaluated or compared the functional outcomes of treatment by EF using a uniform evaluation scale such as the short version of the Disabilities of the Arm, Shoulder and Hand outcome questionnaire (Quick DASH).20 The Quick DASH questionnaire has been successfully used to evaluate functional outcomes after surgical treatment of various upper extremity fractures in children, and it allows for homogeneous evaluation and comparison of varied paediatric patient populations.21-25
The main objective of this study was to retrospectively evaluate the clinical and radiological outcomes of AMF and CMF in children treated by closed or open reduction and EF. The secondary aim was to evaluate upper extremity function with the Quick DASH.
Materials and methods
The institutional review board approved this study.
Between November 2013 and November 2017, 63 children with AMF or CMF were treated at Guangzhou Women and Children’s Medical Center.
All patients were admitted through the emergency department (AMF) or through the outpatient clinic (CMF) with the following demographic and clinical data captured: sex, age at the time of trauma, mechanism of accident, the involved side, presence or absence of associated neurovascular injury and whether it was closed or open. In addition, information such as time between trauma and surgery; and length of postoperative follow-up was collected from the medical records.
The inclusion criteria were as follows: 1) confirmed diagnosis of AMF (the time period between trauma and surgery is less than two weeks) or CMF (the time period between trauma and surgery more than three weeks);6,26 2) chronological age below 15 years; 3) surgical treatment by closed or open reduction and EF of the ulna; 4) follow-up more than six months; 5) complete radiological data.
A total of 37 patients were excluded, including 21 patients with AMF treated by closed reduction and cast fixation (ten cases) or elastic stable intramedullary nailing (11 cases), one patient with CMF treated by elastic stable intramedullary nailing and 15 cases with a follow-up less than six months.
The included patients were divided into two groups according to treatment modality. In particular, patients with AMF were treated by closed reduction and EF of the ulna (Group A; 15 patients) while those with CMF were managed by closed or open reduction and EF of the ulna (Group B; 11 patients).
Surgical technique
All patients underwent surgery at our institution by the same experienced paediatric orthopedic surgical team. Two advanced paediatric orthopaedic doctors (Hong wen Xu and Qinghe Zhou) in our department performed the operations.
AMF
All patients with AMF were treated by closed reduction and EF of the ulna. Patients were given general anaesthesia and were placed in the decubitus position. According to the angulation of the ulnar fracture and the size of the fragment, four to five pins were introduced under fluoroscopy perpendicularly to the ulnar axis in the proximal (two or three pins) and distal fragment (two pins) of the fracture; pins were directed towards the opposite cortex. After reduction of the ulnar fracture and radial head dislocation, a mini-EF (Orthofix, Verona, Italy) was adjusted to the pins and fixed; fluoroscopic imaging confirmed proper radial head reduction in all projections. No other hardware was used to maintain the reduction of the radial head.
Postoperatively, all patients were encouraged to start elbow movement the day following surgery. Dressings were changed regularly. EF was removed three months after the index procedure.
Closed or open reduction and ulnar osteotomy
For patients with CMF, ulnar osteotomy was performed prior to reduction through a posterior approach. The proximal ulnar was exposed and a transverse cut made. Five to six pins were introduced under fluoroscopy perpendicularly to the ulnar axis in the proximal (two to three pins) and distal fragment (three pins) of the fracture; pins were directed towards the opposite cortex. Then closed reduction was attempted under the lengthening and angulating of the EF (Orthofix, Verona, Italy). If closed reduction could be achieved, the EF was adjusted until stable reduction of the radial head was achieved and fluoroscopic imaging confirmed proper radial head reduction in all projections. Otherwise, open reduction was performed. Open reduction was performed through the modified Kocher approach.13 Firstly we exposed the radial head and tried to find the annular ligament; if possible the ligament was repaired and was pulled over the radial neck. However, if this was not possible, the remnants of the annular ligament and surrounding fibrous tissues were removed prior to radial head reduction. Once successful open reduction was achieved, the EF was lengthened and angulated to maintain the achieved reduction of the radial head and confirmed by fluoroscopic imaging.
At 24 to 48 hours after surgery, prior to discharge, full-length anteroposterior (AP) and lateral radiographs of the affected forearm (elbow joint included) were taken to detect possible radial head dislocation. If the radial head was found to be dislocated, the EF was lengthened until reduction of the radial head was judged as satisfactory in all projections.27
Postoperatively, all patients were encouraged to start movement immediately. Hardware was removed three to six months after the index surgery.
Radiological evaluation
The injured forearms and elbows were imaged with full-length AP and lateral radiographs to evaluate the location of the ulnar fractures and direction of dislocation of the radial heads.28
In addition, radiological examination was performed at each follow-up visit. The following parameters were measured on AP radiographs: 1) carrying angle (CA);29 2) the angle between the axis of the proximal and distal fragments of the fractured ulna on both AP (AUPA) and lateral view (AUPL), preoperatively, postoperatively and at last follow-up visit; 3) the angle between the line passing at the level of the coronoid and the posterior apex of the olecranon and the axis of ulna on lateral radiographs (OAUL) was also measured (Fig. 1). CA was used to assess if the patient had cubitus varus; AUPA, AUPL and OAUL were used to evaluate the ulnar angulation deformity in AP and lateral view.
Fig. 1.
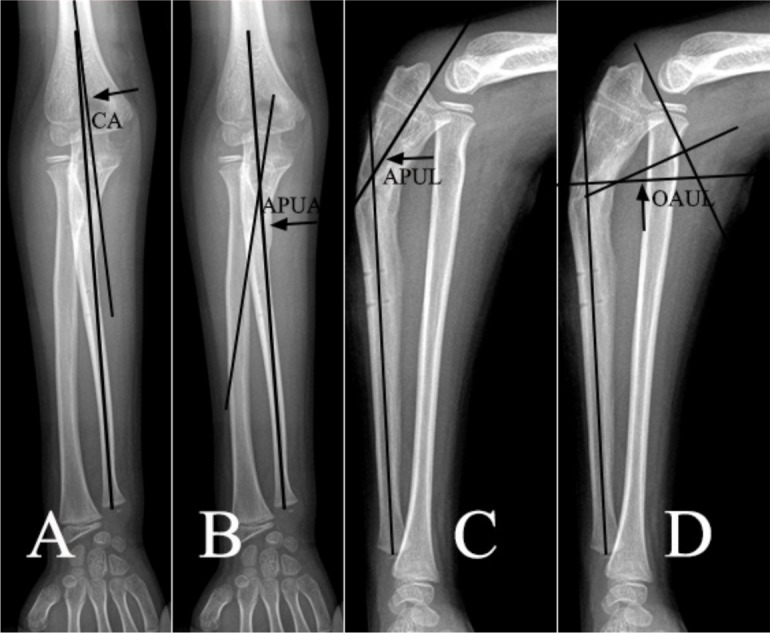
Radiological measurements (CA, carrying angle (a); AUPA, angle between the axis of proximal and distal fragments of fractured ulna on anteroposterior radiographs (b); AUPL, angle between the axis of proximal and distal fragments of fractured ulna on lateral radiographs (c); OAUL, angle between the line passing at the level of the coronoid and the posterior apex of the olecranon and axis of ulna on lateral radiographs (d)).
Functional evaluation
At the last follow-up visit, the patients were asked to complete Quick DASH at the outpatient clinic or by telephone. Quick DASH is a self-reported questionnaire consisting of 11 items corresponding to various activities of daily living and symptoms experienced by the patient. The patient rates each item according to the perceived degree of severity ranging from 1 (no discomfort or symptoms) to 5 (major discomfort or severe symptoms). The final score is calculated according to the algorithm [(sum of responses N / N) -1] × 25, where N is the number of responses. The Quick DASH score ranges from 0 (least disability) to 100 points (most disability) and allows evaluation of the overall performance of the upper limb.20-24
Follow-up
All patients underwent regular clinical and radiological follow-up for at least six months after their index surgery (mean 32.1, range 7 to 65). At each follow-up visit, full-length AP and lateral radiographs of the affected forearm (elbow joint included) were taken to assess fracture consolidation and to detect complications such as radial head dislocation, secondary displacement, re-fracture, hardware migration, nonunion or malunion.
Complete fracture healing was defined as full return to activities of daily living and sports.
Statistical analysis
Categorical parameters were expressed as frequencies and percentages. Quantitative data were expressed as the means, ranges and sd. Statistical analysis was performed using Fisher’s exact test for categorical variables and the unpaired t-test for quantitative parameters. The threshold for statistical significance was set at p < 0.05.
Results
A total of 26 children (20 males, six females) met the inclusion criteria. The right side was involved in 13 cases (50%) and the left side in 13 cases (50%). According to Bado’s classification,25 15 cases (57.7%) were type I, one case was type II (3.8%) and ten cases were type III (38.5%). Table 1 shows patient demographics; Group A and Group B did not significantly differ in terms of demographics (p > 0.05) (Table 1). In patients with CMF, the mean time between injury and surgery was 8.5 months (sd 8.1). The mean time in patients treated by open reduction (11.8 months; sd 10.4) was significantly longer than the patients treated by closed reduction (5.7 months; sd 5.1) (Table 2).
Table 1.
Demographic of patients
| % | Group A, n | Group B, n | χ2/t | p-value | |
|---|---|---|---|---|---|
| Sex | |||||
| Male | 76.9 | 12 | 8 | N/A | 0.664 |
| Female | 23.1 | 3 | 3 | ||
| Side | |||||
| Left | 50 | 7 | 6 | N/A | 0.691 |
| Right | 50 | 8 | 5 | ||
| Bado type | |||||
| I | 57.7 | 7 | 8 | N/A | N/A |
| II | 3.8 | 1 | 0 | ||
| III | 38.5 | 7 | 3 | ||
| Mean age, years | 6.8 ± 3.5 | 6.5 ± 2.9 | 0.221 | 0.827 | |
| Mean follow-up, months | 36.6 (7 to 65) | 25.9 (13 to 41) | 1.844 | 0.078 |
N/A, not applicable
Table 2.
Radiological and functional outcomes of patients with Chronic Monteggia (Group B) treated by open or closed reduction
| Closed reduction | Open reduction | t/Fisher’s | p-value | |
|---|---|---|---|---|
| Patients, n | 6 | 5 | N/A | N/A |
| Mean time between injury and surgery, months | 5.7± 5.1 | 11.8± 10.4 | 3.485 | 0.231 |
| Mean CA | 15.5°± 16.4° | 15.6°± 7.4° | 0.014 | 0.990 |
| Mean AUPA | 7.0°± 11.8° | 6.6°± 6.1° | 0.070 | 0.946 |
| Mean AUPL | 22.9°± 7.7° | 21.3°± 6.7° | 0.040 | 0.969 |
| Mean OAUL | 26.3°± 6.7° | 25.1°±9.1° | 0.246 | 0.811 |
| Quick DASH score | ||||
| 0 | 5 | 5 | N/A | 1 |
| > 1 | 0 | 1 (score: 13.6) | N/A | N/A |
N/A, not applicable; CA, carrying angle; AUPA, angle between the axis of proximal and distal fragments of fractured ulna on anteroposterior radiographs; AUPL, angle between the axis of proximal and distal fragments of fractured ulna on lateral radiographs; OAUL, angle between the line passing at the level of the coronoid and the posterior apex of the olecranon and axis of ulna on lateral radiographs; Quick DASH, short version of the Disabilities of the Arm, Shoulder and Hand outcome questionnaire
Group A: AMF
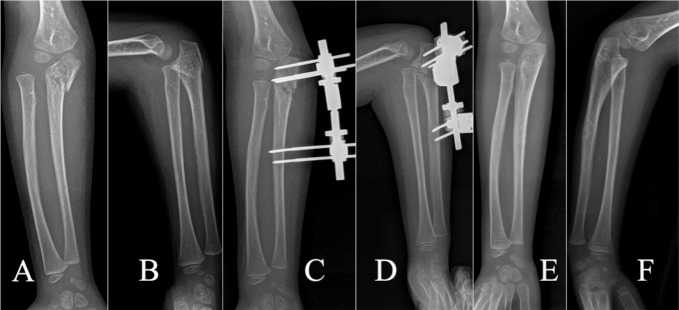
In total, 15 out of 26 patients underwent closed reduction and EF of the ulna (57.7%); the mean age at the time of injury was 6.8 years (2 to 13). According to Bado’s classification,3 seven cases (46.7%) were type I, one case was type II (6.6%) and seven cases were type III (46.7%). The mean follow-up was 36.6 months (7 to 65) (Table 1) (Fig. 2).
Fig. 2.
Acute Monteggia fracture treated by closed reduction and external fixation; preoperative (a, b), postoperative (c, d) and final follow-up (e, f) radiographs.
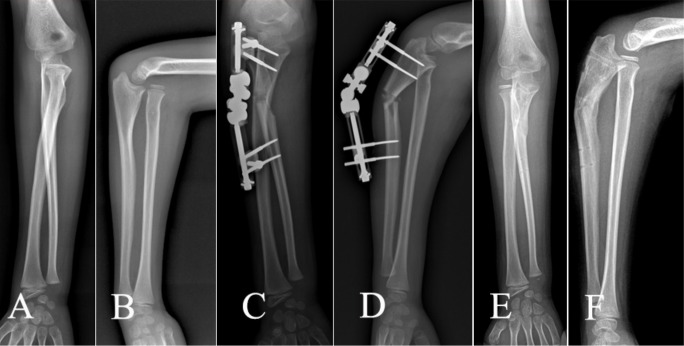
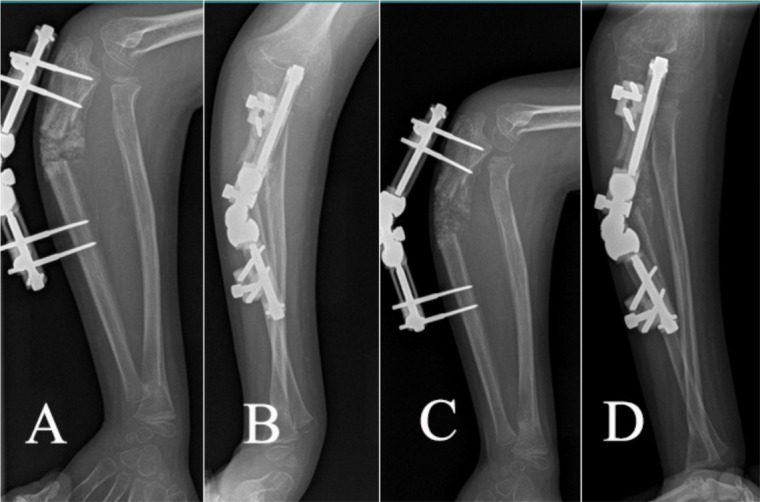
Group B: CMF
In total, 11 out of 26 patients (42.3%) were treated with closed (five patients) or open reduction (six reduction), ulnar osteotomy and EF; the mean age at the time of injury was 6.5 years (2 to 12). According to Bado’s classification3, eight cases (72.7%) were type I and three cases were type III (27.3%). The mean follow-up was 25.9 months (13 to 41) for Group B (Table 1) (Fig. 3).
Fig. 3.
Chronic Monteggia fracture treated by closed reduction and external fixation; preoperative (a, b), postoperative (c, d) and final follow-up (e, f) radiographs.
Radiological outcome
Group A patients had lower CA and AUPL than Group B, 7.1° (sd 6.8°) and 17° (sd 6.1°) and 15.6° (sd 11.6°) and 25.6° (sd 7.7°), respectively (Table 3).
Table 3.
Radiological outcome
| Group A | Group B | t | p-value | |
|---|---|---|---|---|
| Mean CA | 7.1 ± 6.8 | 15.6 ± 11.6 | 2.341 | 0.028 |
| Mean AUPA | 11.8 ± 6.5 | 6.8 ± 8.6 | 1.686 | 0.105 |
| Mean AUPL | 17.0 ± 6.1 | 25.6 ± 7.7 | 3.165 | 0.004 |
| Mean OAUL | 32.4 ± 7.9 | 23.1 ± 6.8 | 3.153 | 0.004 |
| Heterotopic ossification, n/N (%) | 1/15 (6.7) | 0/11 (0) | N/A | N/A |
| Redislocation, n/N (%) | 0/15 (0) | 1/11 (9.1) | N/A | N/A |
CA, carrying angle; AUPA, angle between the axis of proximal and distal fragments of fractured ulna on anteroposterior radiographs; AUPL, angle between the axis of proximal and distal fragments of fractured ulna on lateral radiographs; OAUL, angle between the line passing at the level of the coronoid and the posterior apex of the olecranon and axis of ulna on lateral radiographs; N/A, not applicable
Group A patients had higher AUPA and OAUL than Group B, 11.8° (sd 6.5°) and 32.4° (sd 7.9°) and 6.8° (sd 8.6°) and 23.1° (sd 6.8°), respectively (Table 3). Moreover, among patients with CMF (Group B), those treated by closed reduction and EF had similar CA (p = 0.990), AUPA (p = 0.946), AUPL (p = 0.969) and OAUL (p = 0.811) compared with those treated by open reduction and EF (Table 2).
Despite the fact that CA (p = 0.028), AUPL (p = 0.004) and OAUL (p = 0.004) were significantly different between the two groups of patients, this was not clinically relevant as all patients had low Quick Dash scores (Table 4).
Table 4.
Clinical outcome
| % | Group A | Group B | p-value | |
|---|---|---|---|---|
| Quick DASH score, n | ||||
| 0 | 88.5 | 13 | 10 | 0.738 |
| > 1 | 11.5 | 2 | 1 | |
| Mean Quick DASH | N/A | 1.37 (0 to 18.2) | 1.24 (0 to 13.6) | |
| Complaints | ||||
| Yes | 61.5 | 6 | 10 | 0.014 |
| No | 38.5 | 9 | 1 | |
| Range of movement*, n | ||||
| Comparable | 88.5 | 15 | 8 | 0.063 |
| Not comparable | 11.5 | 0 | 3 |
injured versus not-injured side
Quick DASH, short version of the Disabilities of the Arm, Shoulder and Hand outcome questionnaire; N/A, not applicable
Radiologically, no secondary displacement, wire migration, consolidation delays, nonunion, malunion or re-fracture were noted. However, one patient’s Bado type I fracture (6.7%) developed heterotopic ossification of the ulna (Fig. 4). One case of postoperative redislocation of the radial head was detected in Group B (9.1%); after one month lengthening, the radial head was reduced and the final functional outcome was excellent (Quick DASH score: 0) (Fig. 5).
Fig. 4.
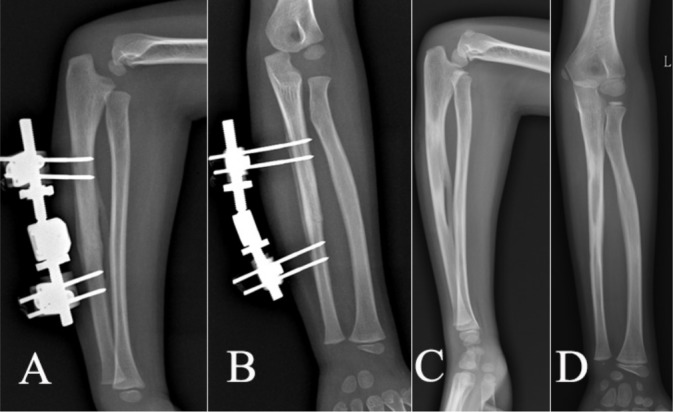
Heterotopic ossification of the ulna was developed during treatment of acute Monteggia fracture treated by closed reduction and external fixation (a, b). At last follow-up visit, the ossification is still visible although reduced in size (c, d).
Fig. 5.
Redislocation of the radial head during early postoperative period (a, b). Lengthening of the external fixation allowed progressive reduction of the radial head (c, d).
Clinical outcome and complications
Clinical outcome was similar between the two groups of patients (p = 0.738). The overall mean Quick DASH score was 1.31 (0 to 18.2). Specifically, the mean Quick DASH score was 1.37 (0 to 18.2) for Group A and 1.24 (0 to 13.6) for Group B patients (Table 4). Moreover, among patients with CMF (Group B), those treated by closed reduction and EF had similar Quick DASH score compared with those treated by open reduction and EF (p = 1) (Table 3).
The patient who developed heterotopic ossification of the ulna had satisfactory functional outcome although they had transient limitation of supination. Two patients (7.6%), one in group A (1/15; 6.7%) and one in group B (1/11; 9.1%) developed transient pin tract infection.
During the postoperative period, three patients experienced dysesthesias in the radial nerve territory (Group A: two cases; Group B: one case). All patients had recovered completely by the last follow-up visit.
At last follow-up visit, the range of movement of the injured elbow was similar compared with the contralateral side in all patients. Six out of 15 (40%) patients with AMF (Group A) were not fully satisfied with the clinical appearance of their upper extremity due to decreased CA, scarring and/or residual pain. Ten out of 11 patients (91%) in Group B complained about clinical appearance of the upper extremity, in particular the bowing of the proximal ulna (p = 0.014) (Table 4). However, all patients returned to their previous daily and sport activities.
None of the patients showed signs of growth arrest or disturbances by both radiological and clinical assessment.
Discussion
We reviewed 26 patients with AMF and CMF treated by closed or open reduction and EF of the ulna. All ulna fractures consolidated and one case of radial head redislocation was recorded during follow-up. These positive results were confirmed functionally with low Quick Dash scores in both groups of patients. It appears that EF is not contraindicated to manage both AMF and CMF in children.
Several works have shown that elastic stable intramedullary nailing is a minimally invasive and reliable technique with a low complication rate that can be used as primary treatment option in children with AMF requiring surgical management.5,8,26
On the other hand, very few studies have reported on the use of EF in the management of Monteggia fractures. Henman used EF to manage AMF secondary to a gun-related wound.18 In 2008, Tan et al19 reported the outcome of AMF treated by EF. They treated six patients with AMF with green-stick fractures of the ulna. All patients were treated by closed reduction and EF and the final outcomes were rated as excellent, both clinically and radiologically. Our findings corroborate those by Tan et al19 as the mean Quick DASH score of patients with AMF was 1.37. In our institution, we preferred to use EF for the patients with AMF who had significant angulation of the proximal ulna fracture or unreducible bowing deformity of the ulna which caused unstable reduction of the radial head.
Several authors have reported the use of EF to manage CMF.11,17,30,31 Exner30 reported two cases of CMF treated by closed reduction and EF with progressive lengthening and angulation of the ulna. At the last follow-up visit, nine years and eight months after index procedure, clinical outcome was satisfactory. Bor et al17 evaluated four patients treated by closed reduction, proximal ulna osteotomy and Ilizarov EF and reported similarly good clinical outcomes. On the other hand, Hasler et al31 reviewed 15 patients with CMF treated by open reduction, proximal ulnar osteotomy and EF. Reduction of the radial head could be achieved in all patients and function improved in 93% of cases. Lu et al11 evaluated the clinical and radiological outcome of 33 patients with CMF treated by open reduction, ulnar osteotomy and dual-socket external fixation. They reported two cases of delayed union of the ulna (6.1%) and three cases of radial head re-dislocation (9.1%) during the early postoperative period. However, none of these authors evaluated functional outcome using a uniform evaluation scale such as Quick DASH. Quick DASH has been used by several authors to evaluate functional outcome of a variety of upper extremity paediatric fractures treated surgically and conservatively.21-25 In particular, Pavone et al21 used Quick DASH to evaluate function in 131 children with clavicle fractures treated conservatively. Canavese et al22 used it in 52 children with displaced proximal humerus fractures treated by ESIN fixation. Wang et al23 applied it to children treated surgically for supracondylar humerus fractures. Guyonnet et al24 used it in children with radial head fractures treated by elastic stable intramedullary nails and Corradin et al25 used it in children with isolated olecranon fractures treated surgically.
We found that functional and radiological outcome were good in both groups of patients. Regardless of the surgical technique used, if anatomical and stable reduction is obtained, good functional outcome should be expected in patients with AMF and CMF. Moreover, patients with CMF that were treated by open or closed reduction showed similar good outcomes (Table 2).
However, we found that patients with CMF were less satisfied with the clinical appearance of their upper extremity than AMF patients. This was probably related to the fact that in CMF patients more angulation of the proximal ulna was needed in order to reduce the radial head resulting in reduced CA on the frontal plane and increase proximal ulna bowing on the sagittal plane. However, at last follow-up visit, clinical outcome was not significantly different between the two groups of similar patients, irrespective of CA, AUPA, AUPL and OAUL values (Table 3).
During the analysis of our results, we identified some limitations of this study. We conducted a retrospective evaluation of surgically treated patients only; patients treated by closed reduction and cast immobilization or elastic stable intramedullary nailing of the ulna were not included as surgery with EF technique is the preferred treatment of choice at our institution. However, all patients came from a single institution and the total number of cases was similar to those in other published studies. Finally, at last follow-up, each patient was asked to complete the Quick DASH questionnaire, allowing for homogeneous evaluation and comparison of various paediatric patient populations.20 Despite these limitations, the study demonstrated good functional and radiological outcomes in children with AMF or CMF treated by EF.
In conclusion, EF is an alternative option for the management of AMFs and CMFs. In a trained surgeon’s hands it can achieve satisfactory radiological and clinical outcomes with relative low rates of complications.
Open access
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) licence (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Compliance with ethical standards
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Ethical statement
Ethical approval: Approval from our institutional review board was obtained for this retrospective study.
Informed consent: Informed consent was not required from all individual participants included in the study.
ICMJE Conflict of interest statement
None declared.
Author Contributions
ZY: Study design, Performed measurements, Data analysis, Manuscript preparation.
HWX: Study design, Performed measurements, Manuscript preparation.
YZL: Statistical analysis, Manuscript preparation.
YQL: Statistical analysis, Performed measurements, Manuscript preparation.
JCL: Performed measurements, Manuscript preparation.
FC: Study design, Manuscript modification.
References
- 1.Rehim SA, Maynard MA, Sebastin SJ, Chung KC. Monteggia fracture dislocations: a historical review. J Hand Surg Am 2014;39:1384-1394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Joeris A, Lutz N, Blumenthal A, Slongo T, Audigé L. The AO Pediatric Comprehensive Classification of Long Bone Fractures (PCCF). Acta Orthop 2017;88:123-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wilkins KE. Changes in the management of monteggia fractures. J Pediatr Orthop 2002;22:548-554. [PubMed] [Google Scholar]
- 4.Kontakis GM, Pasku D, Pagkalos J, Katonis PG. The natural history of a mistreated ipsilateral Galeazzi and Monteggia lesion: report of a case 39 years post-injury. Acta Orthop Belg 2008;74:546-549. [PubMed] [Google Scholar]
- 5.Ring D. Monteggia fractures. Orthop Clin North Am 2013;44:59-66. [DOI] [PubMed] [Google Scholar]
- 6.David-West KS, Wilson NI, Sherlock DA, Bennet GC. Missed Monteggia injuries. Injury 2005;36:1206-1209. [DOI] [PubMed] [Google Scholar]
- 7.Lädermann A, Ceroni D, Lefèvre Y, et al. . Surgical treatment of missed Monteggia lesions in children. J Child Orthop 2007;1:237-242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ramski DE, Hennrikus WP, Bae DS, et al. . Pediatric monteggia fractures: a multicenter examination of treatment strategy and early clinical and radiographic results. J Pediatr Orthop 2015;35:115-120. [DOI] [PubMed] [Google Scholar]
- 9.Bae DS. Successful strategies for managing Monteggia injuries. J Pediatr Orthop 2016;36(suppl 1):S67-S70. [DOI] [PubMed] [Google Scholar]
- 10.Nakamura K, Hirachi K, Uchiyama S, et al. . Long-term clinical and radiographic outcomes after open reduction for missed Monteggia fracture-dislocations in children. J Bone Joint Surg [Am] 2009;91-A:1394-1404. [DOI] [PubMed] [Google Scholar]
- 11.Lu X, Kun Wang Y, Zhang J, et al. . Management of missed Monteggia fractures with ulnar osteotomy, open reduction, and dual-socket external fixation. J Pediatr Orthop 2013;33:398-402. [DOI] [PubMed] [Google Scholar]
- 12.Datta T, Chatterjee N, Pal AK, Das SK. Evaluation of outcome of corrective ulnar osteotomy with bone grafting and annular ligament reconstruction in neglected monteggia fracture dislocation in children. J Clin Diagn Res 2014;8:LC01-LC04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Park H, Park KW, Park KB, et al. . Impact of open reduction on surgical strategies for missed Monteggia fracture in children. Yonsei Med J 2017;58:829-836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Slongo TF. Correction osteotomy of neglected ‘monteggia’ lesion with an external fixator. Oper Orthop Traumatol 2008;20:435-449. [DOI] [PubMed] [Google Scholar]
- 15.Bilen FE, Kocaoğlu M, Eralp L. Indirect reduction of the radial head using an external fixator to treat chronic radial head dislocations. Acta Orthop Traumatol Turc 2010;44:14-19. [DOI] [PubMed] [Google Scholar]
- 16.Ray R, Gaston M. Treatment of late-presenting Monteggia variant with an isolated, simple flexion ulnar osteotomy. J Pediatr Orthop B 2014;23:472-476. [DOI] [PubMed] [Google Scholar]
- 17.Bor N, Rubin G, Rozen N, Herzenberg JE. Chronic anterior monteggia lesions in children: report of 4 cases treated with closed reduction by ulnar osteotomy and external fixation. J Pediatr Orthop 2015;35:7-10. [DOI] [PubMed] [Google Scholar]
- 18.Henman PD. A year behind bars: treatment of compound Monteggia fracture by external fixation. J R Soc Med 1997;90:499-500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tan JW, Mu MZ, Liao GJ Li JM. Pathology of the annular ligament in paediatric Monteggia fractures. Injury 2008;39:451-455. [DOI] [PubMed] [Google Scholar]
- 20.Beaton DE, Wright JG, Katz JN, Upper Extremity Collaborative Group . Development of the QuickDASH: comparison of three item-reduction approaches. J Bone Joint Surg [Am] 2005;87-A:1038-1046. [DOI] [PubMed] [Google Scholar]
- 21.Pavone V, DE Cristo C, Testa G, et al. . Does age affect outcome in children with clavicle fracture treated conservatively? QuickDash and MRC evaluation of 131 consecutive cases. Minerva Pediatr 2018. (Epub ahead of print). [DOI] [PubMed] [Google Scholar]
- 22.Canavese F, Athlani L, Marengo L, et al. . Evaluation of upper-extremity function following surgical treatment of displaced proximal humerus fractures in children. J Pediatr Orthop B 2014;23:144-149. [DOI] [PubMed] [Google Scholar]
- 23.Wang SI, Kwon TY, Hwang HP, Kim JR. Functional outcomes of Gartland III supracondylar humerus fractures with early neurovascular complications in children: A retrospective observational study. Medicine (Baltimore) 2017;96:e7148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guyonnet C, Martins A, Marengo L, et al. . Functional outcome of displaced radial head fractures in children treated by elastic stable intramedullary nailing. J Pediatr Orthop B 2018;27:296-303. [DOI] [PubMed] [Google Scholar]
- 25.Corradin M, Marengo L, Andreacchio A, et al. . Outcome of isolated olecranon fractures in skeletally immature patients: comparison of open reduction and tension band wiring fixation versus closed reduction and percutaneous screw fixation. Eur J Orthop Surg Traumatol 2016;26:469-476. [DOI] [PubMed] [Google Scholar]
- 26.Letts M, Locht R, Wiens J. Monteggia fracture-dislocations in children. J Bone Joint Surg [Br] 1985;67-B:724-727. [DOI] [PubMed] [Google Scholar]
- 27.Delpont M, Jouve JL, Sales de Gauzy J, et al. . Proximal ulnar osteotomy in the treatment of neglected childhood Monteggia lesion. Orthop Traumatol Surg Res 2014;100:803-807. [DOI] [PubMed] [Google Scholar]
- 28.Bado JL. The Monteggia lesion. Clin Orthop Relat Res 1967;50:71-86. [PubMed] [Google Scholar]
- 29.Balasubramanian P, Madhuri V, Muliyil J. Carrying angle in children: a normative study. J Pediatr Orthop B 2006;15:37-40. [DOI] [PubMed] [Google Scholar]
- 30.Exner GU. Missed chronic anterior Monteggia lesion. Closed reduction by gradual lengthening and angulation of the ulna. J Bone Joint Surg [Br] 2001;83-B:547-550. [DOI] [PubMed] [Google Scholar]
- 31.Hasler CC, Von Laer L, Hell AK. Open reduction, ulnar osteotomy and external fixation for chronic anterior dislocation of the head of the radius. J Bone Joint Surg [Br] 2005;87-B:88-94. [PubMed] [Google Scholar]