Abstract
Objectives:
Aim of this study was to characterize acute poisoning and snakebite cases and their outcome in the Emergency Department (ED).
Methods:
This was a prospective study done in the ED of a tertiary healthcare center. Study included 184 patients of acute poisoning and 16 cases of snakebite. Data regarding demographics, type, time, and mode of poisoning, lag time in reaching the hospital, initiation of treatment, first aid, in-hospital treatment, and comorbid illness were obtained. Data regarding requirement of antidote, duration of hospitalization, and outcome were also obtained.
Results:
Out of 200 cases, 181 (90.5%) were adults and 19 (9.5%) were of pediatric age group. Poisoning was common among males (57%) than females (43%). Majority (40%) were from the age group of 21–30 years. Out of 200, 115 (57.5%) poisonings were suicidal, 68 (34%) were accidental, and 17 (8.5%) were homicidal. Acute poisonings included corrosive 54 (27%), drug overdose 26 (13%), organophosphorus compounds 20 (10%), rodenticides 20 (10%), and symptomatic snakebite 16 (8%). Seventy-two (36%) were admitted with a median hospital stay of 6 days with 5 (2.5%) deaths. Logistic regression analysis revealed poorer outcome for 15–30 years age [OR 12.6 (1.6–97.5), P = 0.015], males [OR 2.5 (1.4–4.4) P = 0.04], patients coming from >30 km [OR 4.3 (1.5–12.1), P = 0.006].
Conclusion:
Our study demonstrated an increased incidence of corrosive ingestion. With increasing rates of suicidal ingestions, there is a need for holistic approach to manage mental health issues at primary care level.
Keywords: Acute poisoning, corrosive, emergency department (ED), north India, snakebite
Introduction
Acute poisoning is the major cause of morbidity and mortality worldwide, with 90% of the burden of fatal poisoning coming from developing countries.[1] In developed countries, the rate of mortality from poisoning is 1–2%, but in India, it varies around 20%.[2] The nature of poisoning shows a regional variation depending upon the agent predominantly in use. Use of poisons with suicidal ideation is common. An increased incidence of depression compounds the problem of poisoning in India. Fifty-seven million people (18% of the global estimate) in India are affected by depression.[3] Snakebite is also a major problem worldwide with data showing evidence that snakes bite 4.5–5.4 million people a year out of which 1.8–2.7 million of them develop clinical illness (envenoming) after snakebite, and the death toll ranges from 81,000 to 138,000. In India alone, it has been estimated that as many as 2.8 million people are bitten by snakes, and 46,900 people die from snakebite every year.[4] The colossal burden of poisoning and snakebite cases requires comprehensive strategies for reducing deaths. Hence, this prospective observational study was conducted to identify factors related to outcomes in such cases and to suggest strategies to reduce associated morbidity and mortality.
Methods
The study was conducted in the emergency department of a tertiary care hospital in New Delhi, India. Data were collected prospectively for a duration of 15 months from July 2016 to March 2018. We included patients of all age group coming to ER with acute ingestion of poisonous substance and snakebite cases who were symptomatic or having increased whole blood clotting time. Patients with chronic toxicity and those who refused to give consent were excluded from the study. Data obtained included demographic details such as age, sex, marital status, educational qualification, and occupation. The time of poisoning/snakebite, time of hospital arrival, the lag time in reaching the hospital, and reasons for the same, and mode of transportation were noted. Data about diagnosis, any co-morbid illness, any previous history of poisoning, mode of poisoning, whether accidental/suicidal/homicidal, and any recent precipitating event were also recorded. The patients/attendants were asked about details of first aid received prior coming to institute. The details of door-to-needle time (defined as the time from hospital arrival to administration of first treatment) and requirement of antidote were recorded. Finally, the duration of hospital stay and recovery status were noted.
Statistical analysis
A sample size of 196 was determined as adequate, assuming a confidence level of 95%, 80% power, and anticipating incidence of snakebite cases as 15% in our emergency department. All data were presented as numbers, percentages, mean ± standard deviation (SD), and median (interquartile range (IQR)). Univariate and multivariate logistic regression analyses were used to predict the effect of different variables on the outcome and duration of hospital stay, respectively. Good outcome was taken as patients who were discharged from emergency and poor outcome was taken as patients who got admitted or died in the emergency. A P value < 0.05 was considered statistically significant. The study was conducted after getting approval from Institute Ethics Committee in June 2016 (IECPG-353/29.06.2016) and confidentiality of the data was ensured.
Results
Majority of the cases were due to poisoning from a toxic agent (92%). Out of 200 cases, 19 (9.5%) were children below the age of 15 years with 15 (79%) cases being below the age of 5 years. Approximately, 60% were males. The percentage of illiterate people were 18% and 53% were unemployed [Table 1].
Table 1.
Demographic profile of the patients presenting with acute poisonings and snakebite
| n=200 | |
|---|---|
| Poisoning n (%) | 184 (92) |
| Snakebite n (%) | 16 (8) |
| Age (years), mean±SD | 26.8±14 |
| Male/Female, n (%) | 114 (57)/86 (43) |
| Married, n (%) | 92 (46) |
| Distance traveled n (%) | |
| 0-10 km | 95 (47.5) |
| 10-30 km | 86 (43) |
| >30 km | 19 (9.5) |
| Education n (%) | |
| Illiterate | 36 (18) |
| Primary school (up to 5th class) | 8 (4) |
| Middle school (up to 8th class) | 25 (12.5) |
| High school (up to 10th class) | 48 (24) |
| Post high school (up to 12th class) | 49 (24.5) |
| Graduate/Postgraduate | 34 (17) |
| Occupation n (%) | |
| Unemployed | 106 (53) |
| Unskilled worker | 27 (13.5) |
| Semiskilled worker | 16 (8) |
| Skilled worker | 34 (17) |
| Professional | 17 (8.5) |
n=numbers, % = percentage, SD=standard deviation, Km=kilometer
Distribution of cases
Distribution of cases is depicted in Figure 1. Major types of poisoning included corrosives (26.5%), drugs (13.5%), rodenticides (10.5%), organophosphates (10%), and snakebite (8%). In 30 (15%) cases, the agents could not be identified by the patients or their relatives. Some miscellaneous (34/200) causes of poisoning included hydrocarbons (9), pyrethroids (9), alcohol intoxication (6), methanol (2), and one case each of diethyl ether, hydrogen peroxide, potassium chlorate, chlorhexidine, isopropyl alcohol, paraquat, and acetone. Of the 16 cases of snakebite, 8 (50%) were vasculotoxic, 5 (31%) neurotoxic, and 3 had only local symptoms.
Figure 1.
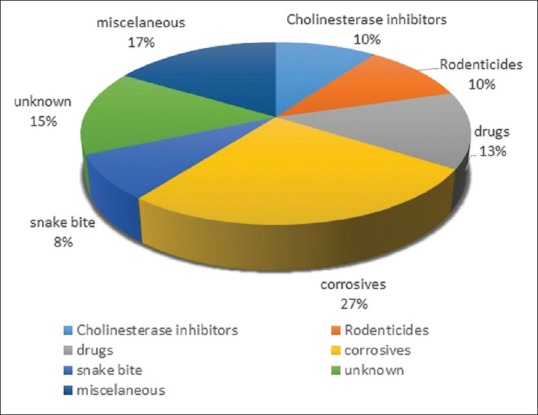
Distribution (percentage) of various acute poisoning and snakebite cases in the studied population
The major mode of poisoning were suicidal 115 (57%), while accidental poisonings were seen in 68 (34%) cases. In 17 (8.5%) cases, poison was given by others to harm (classified as homicidal). Out of the 115 suicidal poisoning, 80 patients were in the age group of 15–30 years. The reasons given for suicidal ingestion were familial conflict (52.7%), stress related to studies in young people (23.4%), unemployment (16%), and stress related to their jobs (12%). In cases of accidental poisonings, wrongly labeled bottles were the major reason. Forty percent (80/200) of the patient received primary treatment in other healthcare facilities before coming to our hospital. Major means of transport while transporting to other facilities initially and to the hospital was three-wheeler (67.5% and 52%, respectively).
Most common clinical features were vomiting (65%) followed by pain in abdomen (40%). Around 45 cases came in altered sensorium out of which 11 cases were from a drug overdose, and 7 cases were due to organophosphate poisoning.
In 29 cases, relatives used fingers to induce vomiting after the alleged consumption and in 6 patients, lemon water/saline water was used to induce emesis. In 9 out of the 16 snakebite cases, relatives applied a tight tourniquet made up of cloth proximal to the site of bite mark.
Median time (IQR) for point of first medical contact after exposure for a patient coming directly to our institute and those going to other hospitals was 60 (51.25–120) min.
On arrival to our institute, 18 (9%) patients had compromised airway, 33 (17%) had compromised breathing, and 9 (4.5%) had a circulatory compromise for which appropriate intervention was done. Twenty patients (10%) required intubation followed by mechanical ventilation. Gastric lavage was done for 86 (43%) patients mostly within 1 h of their arrival. An antidote was given to 21 patients of poisoning and 15 snakebite cases [Table 2].
Table 2.
Use of antidote in acute poisoning and snakebite (Numbers)
| Poisoning (n) | Antidote (n) |
|---|---|
| Organophosphate (20) | Pralidoxime (12) Atropine (14) |
| Paracetamol (4) | N-Acetylcystiene (4) |
| Methanol (2) | Alcohol (2) |
| Opioid (1) | Naloxone (1) |
| Snakebite (16) | ASV (15) |
ASV=antisnake venom
Median length of stay (IQR) in the emergency was 14 (6–22.8) h. One hundred and two (51%) patients were discharged from emergency itself after primary treatment and observation; 72 (36%) were admitted in the hospital for further workup and treatment. Twenty four (12%) of them absconded from the emergency. Of the 72 patients admitted, 67 (89%) were discharged and 5 (11%) died. The median duration of stay after admission in hospital was 6 (3.3–9) days.
Univariate logistic regression was applied for all the factors that could affect the outcome, and it was found that age group between 15 and 30 years had greater odds of poorer outcome [OR 12.6 (1.6–97.5), P = 0.015], males had poor outcome than females [OR 2.5 (1.4–4.4) P = 0.04], and those traveling for more than 30 km to reach our institute had poor outcome [OR 4.3 (1.5–12.1), P = 0.006]. On applying multivariate analysis, these factors were not found to be significant. But on applying multivariate regression of some significant co-variates derived from univariate analysis, it was found that organophosphate poisoning [OR 10.6 (2.9–37.8) P = 0.001], snakebite cases [14.4 (3.1–65.7) P = 0.001], and primary management received in other health care facilities [OR 2.8 (1.4–5.3) P = 0.001] were independent factors that had poor outcome [Table 3].
Table 3.
Logistic regression analysis of poisoned patients for outcomes
| Outcomes | P | OR (95%CI) Unadjusted | P | OR (95% CI) Adjusted | P | ||
|---|---|---|---|---|---|---|---|
| Poor | Good | ||||||
| Age group | |||||||
| <15 years | 1 (1.4) | 18 (14.3) | 0.005 | 1 | - | ||
| 15-30 years | 49 (66.2) | 70 (55.6) | 12.6 (1.6-97.5) | 0.015 | - | - | |
| >30 years | 24 (32.4) | 38 (30.1) | 11.3 (1.4-90.7) | 0.022 | - | - | |
| Sex | |||||||
| Female | 22 (29.7) | 64 (50.8) | 0.004 | 1 | - | - | - |
| Male | 52 (70,3) | 62 (49.2) | 2.4 (1.3-4.4) | 0.04 | - | - | |
| Distance to AIIMS | |||||||
| 0-10 km | 27 (36.5) | 68 (54.0) | 0.011 | 1 | - | - | - |
| 11-30 km | 35 (47.3) | 51 (40.5) | 1.7 (0.9-3.2) | 0.08 | - | - | |
| >30 km | 12 (16.2) | 7 (5.5) | 4.3 (1.5-12.1) | 0.006 | - | ||
| Agents | |||||||
| Organophosphate | |||||||
| No | 59 (79.7) | 121 (96.0) | 1 | ||||
| Yes | 15 (20.2) | 5 (4.0) | 6.1 (2.1-17.7) | 0.001 | 10.6 (2.9-37.8) | 0.001 | |
| Corrosive | |||||||
| No | 58 (78.4) | 89 (70.6) | 1 | ||||
| Yes | 16 (21.6) | 37 (29.4) | 0.6 (0.3-1.3) | 0.2 | |||
| snake | |||||||
| No | 60 (81.1) | 124 (98.4) | 1 | ||||
| yes | 14 (18.9) | 2 (1.6) | 0.001 | 14.4 (3.1-65.7) | 0.001 | 20.1 (4.2-85.7) | 0.001 |
| Alcohol | |||||||
| No | 67 (90.5) | 118 (93.7) | 1 | ||||
| Yes | 7 (9.5) | 8 (6.3) | 0.4 | 1.5 (0.5-4.4) | 0.4 | ||
| Drugs | |||||||
| No | 68 (91.9) | 110 (87.3) | 1 | ||||
| Yes | 6 (8.1) | 16 (12.7) | 0.3 | 0.6 (0.2-1.6) | 0.3 | ||
| Rodenticide | |||||||
| no | 64 (87.7) | 114 (90.5) | 1 | ||||
| Yes | 9 (12.3) | 12 (9.5) | 0.5 | 0.4 (0.2-1.8) | 0.4 | ||
| Other healthcare | |||||||
| No | 33 (44.6) | 87 (69.0) | 1 | - | |||
| Yes | 41 (55,4) | 39 (31.0) | 0.01 | 2.7 (1.5-5) | 0.001 | 2.8 (1.4-5.3) | 0.001 |
OR=odds ratio, CI=confidence interval, P value<0.05 is taken as statistically significant
Discussion
This study intended to look into the sociodemographic profile of the poisoning cases coming to emergency department and look into the factors which may affect the outcomes.
The findings of the study revealed that majority of the patients were in the age group of 15–30 years, with males being involved more than females, which has been the pattern in almost all the previous studies.[5,6,7] Suicidal cases were the major mode of poisoning, with 70% who tried committing suicide were in the age group of 15–30. Considering this age group being the most productive age group and men still being the sole breadwinner in the majority of the Indian families, such a trend seems worrying. As described by Kanchan et al.[8] in a study conducted from south India, we too found that increasing stress in jobs, lack of employment, peer pressure, and conflicts with the in-laws were few of the reasons of taking this extreme step. With increasing trends of deliberate self-harm, there is a need of a holistic approach to manage depression and other common mental health problems in primary care for preventing people from taking extreme steps.[9,10]
Three-wheelers were the main mode of transport used to reach hospital while ambulance being used less frequently, which highlights the lack of proper prehospital care in our city.
In our study, major agents implicated for toxic exposure were corrosives, which are common household agents used for cleaning. These were followed by pesticides and rodenticides. This finding was different from all the previous studies where pesticides were the most commonly used agents.[11,12,13] This could indicate a major shift in the trend of the agents used over the years. The reason for this could be relative ease of getting a corrosive agent like toilet cleaner at home rather than pesticides as most of our patient were from in and around Delhi, an urban setting. With proper packaging and warning signs, the incidence of accidental pesticide have been reduced, but still, the corrosive agents like sulfuric acid are being sold in normal plastic bottles having resemblance with the packaged drinking water often causing confusion.
We had included only those cases of snakebite who had features to suggest bites by poisonous snakes. Vasculotoxic snakebite cases were more than neurotoxic; this differentiation was based on the symptoms patient presented with and by blood tests, not by the species of snake that had bitten. The lack of information could be due to the fact that the patients were anxious and frightened, thus clouding their ability to identify the species, or poor visibility in darkness making the identification difficult and inability to spot the snake due to tall grass in the parks.[14]
The patient and their relatives panic after taking the agent or when they are bitten by a snake; hence, they try some traditional techniques to remove the toxin from the body.[15,16] In our study, we found that people still used age-old method of putting finger in the mouth to stimulate pharynx or using saline water in order to induce vomiting. The practice of applying tourniquet is still prevalent in cases of snakebite. The principle of “Do it R.I.G.H.T” for snakebite patient has to be advocated at primary care level.[17]
The median time for the point of first medical contact was 1 h, whether the patient came directly to our institute or received medical attention outside. This is better when compared to treatment-seeking time for other conditions, mainly because of the anxiety associated with intake of a toxic substance, in patients in the case of accidental intake and in relatives in the cases of suicidal ingestions. Majority of patients required only symptomatic treatment and were kept under observation for any delayed manifestations and then discharged. When the patient came under high-risk suicidal intent, a psychiatric consult was taken, and appropriate follow-up after discharge was ensured after 24 h of observation. Suicidal intent can be determined based on the degree of planning, the lethality of the method considered, and the existence (and content) of any suicide notes.[18]
We assessed the factors which could affect the disposition from emergency, males had 2.5 times greater chance of poor outcomes. Compared with the patients who came from nearby places, the patients who came from far off places (>30 km) were sicker and had a worse outcome; they had already received primary treatment somewhere else and then referred to our institute because of the insufficient capacity of the treating unit. On the agents used, patients taking organophosphate had a significant worse outcome with adjusted odds ratio of 10.6; although it was used by less number of people in our study, still the outcome was in sync with the previous studies.[8,19]
Limitations of the study
Our studies had certain limitations: not all patients admitted in the Emergency room for poisoning during the study period were taken. Therefore, further studies will be needed to validate the trend. The patients who absconded from the emergency were assumed to have recovered as they were stable during their stay in the emergency room. Another limitation of our study was that we included only poisonous snakebite cases. A larger multicentre study in an urban setting would help in better evaluation of the change in trend.
Conclusion
In our study, we found predominant use of corrosives as agents for poisoning, which demonstrated a change in trend from previous similar studies in which pesticides were commonly used. Although we could not find any significant factor that could lead the person to prefer corrosive over pesticide, the ease of access in urban households and more regulated sale of pesticides may be the reason for this change. There is a need for a regulation for proper distribution and storage of these common household corrosive agents. With increasing rates of suicidal ingestions because of depression and work-related stress, there is a need for early detection, creating more awareness, and help groups at the primary care level so that such incidents can be prevented.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflict of interest
There is no conflict of interest.
Acknowledgement
This manuscript was presented in the conference EMIndia2019, National level emergency medicine conference held at AIIMS, New Delhi, in August 2019.
References
- 1.Batra AK, Keoliya AN, Jadhav GU. Poisoning: An unnatural cause of morbidity and mortality in rural India. J Assoc Physicians India. 2003;51:955–9. [PubMed] [Google Scholar]
- 2.Pillay VV. MKR Krishnan's hand book of forensic medicine and toxicology. Hyderabad: Paras Publications; 2000. [Google Scholar]
- 3.Depression and other common mental disorders: Global health estimates. Geneva: World Health Organization; 2017. [Last accessed on 2017 Mar 25]. Available from: http://apps.who.int/iris/handle/10665/254610 . [Google Scholar]
- 4.WHO | Prevalence of snakebite envenoming [Internet] WHO; [cited 2018 Mar 19]. Available from: http://www.who.int/snakebites/epidemiology/en/ [Google Scholar]
- 5.Singh D, Jit I, Tyagi S. Changing trends in acute poisoning in Chandigarh zone: A 25-year autopsy experience from a tertiary care hospital in northern India. Am J Forensic Med Pathol. 1999;20:203–10. doi: 10.1097/00000433-199906000-00019. [DOI] [PubMed] [Google Scholar]
- 6.Srivastava A, Peshin SS, Kaleekal T, Gupta SK. An epidemiological study of poisoning cases reported to the National poisons information centre, all india institute of medical sciences, New Delhi. Hum Exp Toxicol. 2005;24:279–85. doi: 10.1191/0960327105ht527oa. [DOI] [PubMed] [Google Scholar]
- 7.Mishra PK, Kulkarni R, Sane MR, Deshpande A, Kushwah M. Prospects of poisoning-a multi facet study. Arch Med Sadowej Kryminol. 2016;66:235–43. doi: 10.5114/amsik.2016.68099. [DOI] [PubMed] [Google Scholar]
- 8.Kanchan T, Menezes RG, Kumar TSM, Bakkannavar SM, Bukelo MJ, Sharma PS, et al. Toxicoepidemiology of fatal poisonings in Southern India. J Forensic Leg Med. 2010;17:344–7. doi: 10.1016/j.jflm.2010.05.006. [DOI] [PubMed] [Google Scholar]
- 9.Park LT, Zarate CA. Depression in the primary care setting. N Engl J Med. 2019;380:559–68. doi: 10.1056/NEJMcp1712493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jegaraj MKA, Mitra S, Kumar S, Selva B, Pushparaj M, Yadav B, et al. Profile of deliberate self-harm patients presenting to emergency department: A retrospective study. J Fam Med Prim Care. 2016;5:73–6. doi: 10.4103/2249-4863.184627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sharma R, Neelanjana, Rawat N, Panwar N. Mortality and morbidity associated with acute poisoning cases in north-east India: A retrospective study. J Fam Med Prim Care. 2019;8:2068–72. doi: 10.4103/jfmpc.jfmpc_237_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thomas M, Anandan S, Kuruvilla PJ, Singh PR, David S. Profile of hospital admissions following acute poisoning--experiences from a major teaching hospital in south India. Adverse Drug React Toxicol Rev. 2000;19:313–7. [PubMed] [Google Scholar]
- 13.Mittal N, Shafiq N, Bhalla A, Pandhi P, Malhotra S. A prospective observational study on different poisoning cases and their outcomes in a tertiary care hospital. SAGE Open Med. 2013;1:205031211350421. doi: 10.1177/2050312113504213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Arvind V, Bedwal A, Rajarathna K, M NS. Pattern and pharmacotherapy of acute poisonings presenting to a tertiary care centre. Int J Basic Clin Pharmacol. 2017;6:879–86. [Google Scholar]
- 15.Dabbous IA, Bergman AB, Robertson WO. The ineffectiveness of mechanically induced vomiting. J Pediatr. 1965;66:952–4. doi: 10.1016/s0022-3476(65)80070-1. [DOI] [PubMed] [Google Scholar]
- 16.Roberts CJC, Noakes MJ. Fatal outcome from administration of a salt emetic. Postgrad Med J. 1974;50:513–5. doi: 10.1136/pgmj.50.586.513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mallik S, Singh SR, Sahoo S, Mohanty MK. Ornament induced complications in snake bites: Revisiting the “Do it RIGHT” approach. J Fam Med Prim Care. 2016;5:474–6. doi: 10.4103/2249-4863.192351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Patterson WM, Dohn HH, Bird J, Patterson GA. Evaluation of suicidal patients: The SAD PERSONS scale. Psychosomatics. 1983;24:343. doi: 10.1016/S0033-3182(83)73213-5. [DOI] [PubMed] [Google Scholar]
- 19.Gunnell D, Eddleston M, Phillips MR, Konradsen F. The global distribution of fatal pesticide self-poisoning: Systematic review. BMC Public Health. 2007;7:357. doi: 10.1186/1471-2458-7-357. [DOI] [PMC free article] [PubMed] [Google Scholar]


