Abstract
Objectives:
This study was aimed to measure the prevalence and associated risk factors of antenatal depression (AD) among women attending antenatal clinics at primary care centers in the Ministry of Health in Al-Ahsa, Saudi Arabia.
Materials and Methods:
A cross-sectional study was conducted on 357 pregnant women attending antenatal clinics at primary care centers, Ministry of Health, Al-Ahsa, Saudi Arabia between April 1, 2018 and July 1, 2019. A self-administered questionnaire was used for collection of information including questions relevant to sociodemographic variables and a screening tool Edinburgh Postnatal Depression Scale (EPDS) was used to assess the probable depression.
Results:
The prevalence of AD among pregnant women in Al-Ahsa is 31.9%. We found a significant association (P < 0.005) between AD and factors such as difficulty in sleeping, having a smoker husband, having one previous pregnancy, and having postabortion psychological complications.
Conclusion:
It was observed that depression prevails among pregnant ladies in Al-Ahsa city. Hence, in the present study, we tried to rule out the factors that led to depression in pregnant ladies during our antenatal care. In addition, we found that there is a need to train the physicians for asking questions (only two simple PHQ-2 questions) for the screening of depression during antenatal care visite.
Keywords: Antenatal, depression, prevalence, primary health care
Introduction
Antenatal depression (AD) is a depressive episode that arises during pregnancy. Approximately 10% of pregnant women worldwide experience depression during this phase. In developing countries, the rate is much higher (15%). The World Health Organization (WHO) estimated that by the year 2020, depressive disorders will be the second leading cause of global disease burden in women. Furthermore, antenatal depression can lead to postpartum depression if not treated properly. As per research conducted in the U.S., about 33% of postnatal depression cases begin during pregnancy.[1,2]
Antenatal depression can result in adverse effects on the mother, her baby, and her family as a whole. Adverse effects for mothers can be disturbed sleep, loss of follow up in antenatal clinics, clinical complications which include pre-eclampsia, postpartum bleeding, preterm labor, and even suicide. Adverse effects on their babies include low-birth weight, intrauterine growth retardation, preterm delivery, and failure to thrive. AD has been linked to risk-taking behaviors and unhealthy lifestyles including smoking and alcohol consumption, poor dietary habits leading to malnutrition.[3,4]
AD is a very serious depressive disorder and if untreated it may convert into more serious conditions such as postpartum psychosis. The early detection and treatment can be very useful in preventing those complications.[3,4]
Although there are many studies conducted on maternal depression in Saudi Arabia, most of them focus on postpartum depression. Moreover, there are no studies conducted on AD in Al-Ahsa city. Hence, our study aimed to identify the prevalence of AD and determine the associated risk factors among pregnant women attending antenatal clinics at the primary care centers, Ministry of Health in Al-Ahsa, Saudi Arabia.
Aim of the study
To measure the prevalence of AD among women attending primary health care centers in Al-Ahsa.
Objectives of the study
To estimate the prevalence of AD
To know which risk factors are present during the antenatal period
To determine the risk factors associated with AD in primary health care settings.
Literature Review
We found a total of 16 studies that underwent similar aims and objectives at national and international levels.
From America, we reviewed two studies; one study from United States (US) published on 2015 estimated the prevalence of AD in the US population, that was conducted with a sample (n = 3010) and the prevalence of minor depression among pregnant women was found to be 16.6% as compared to the nonpregnant women (11.4%; adjusted PR = 1.5, 95% CI 1.2–1.9).[5] Another study from Brazil published in 2015 aimed to determine the prevalence of AD among Brazilian sample (n = 148) in the second and third trimester and had found the prevalence of 13.5% and 10.1%, respectively, wherein major depression and intimate partner abuse were the main risk factors.[6]
From Africa, we have reviewed five studies with similar objectives; of which two were conducted in Ethiopia in 2015; a cross-sectional study research for the prevalence of AD and associated factors among pregnant women in Addis Ababa, in a sample (n = 393) and found that the prevalence was 24.94% and the risk factors were significant for; the previous history of depression, unplanned pregnancy, and lack of support from the baby's father.[7] Another study from Hawassa city, Ethiopia was institution based cross-sectional study published in 2019 which showed the prevalence to be 21.5% wherein the most contributed risk factors were age (20–30 years), complicated pregnancy, unplanned pregnancy, and health risks.[8]
A further cross-sectional study for AD and associated pregnancy-related anxiety, partner relations, and wealth in women, was conducted in North Tanzania in 2015 on sample (n = 134) wherein 33.8% had AD and the results were significant for pregnancy-related anxiety (odds ratio (OR) 1.36, 95% confidence interval (CI) 1.23 to 1.5). Poor relationship with the partner and low/moderate socioeconomic status had the highest OR for AD (82.34, 95% CI 4.47, 1516.60). Poor relationship with partner and high socio-economic status had an OR of 13.48 (95% CI 1.71, 106.31).[9] In Nigeria (2016), a cross-sectional study aimed to determine the prevalence of AD and associated risk factors among pregnant women attending antenatal clinics in Abeokuta on a sample (n = 314) and found that the prevalence of AD was 24.5% and the risk factors were significant for maternal young age (P = 0.012), not having formal education (P = 0.022), large family size (P = 0.029), coexisting medical conditions (P = 0.034), and a history of previous cesarian section (P = 0.032).[10] Another study in Nigeria which was a hospital-based cross-sectional study published in 2018, showed that the prevalence of depression and anxiety was 22% and the strongest factors were verbal abuse; 45% of women who were physically and/or sexually abused and 21% of those with verbal abuse had depression/anxiety compared to 43% of those who were not abused.[11]
In general, from Asia we reviewed a total of nine works of literature; from China, Malaysia, Bangalore, Jordon, Oman and four from Kingdom of Saudi Arabia (KSA).
The study from China published in 2015, a cross-sectional survey, aimed to determine the prevalence and predictors of antenatal depressive symptoms among Chinese women in their third trimester with sample (n = 292) and found that 28.5% of the participants had depressive symptoms. The risk factors were significant for history of miscarriage (OR = 1.86; 95% CI 1.30–2.66), irregular menstrual history (OR = 2.98; 95% CI 1.64–5.40), and financial worries (OR = 2.33; 95% CI 1.27–4.30).[3]
One study from Malaysia published in 2017aimed to search about poor social support as a risk factor for antenatal depressive symptoms among women attending public antennal clinics in Penang on the sample (n = 3000) and the prevalence of depressive symptoms was 20% and social support was found to be significantly associated with the depressive symptoms.[12] In Bangalore, a hospital-based cross-sectional study published in 2019, showed that the result of positive depression was 35.7% with pregnancy-related anxiety. A recent history of catastrophic events were also found to be a positive predictor of prenatal depression.[13]
From Arabian countries, we reviewed two studies from Jordon and Oman. The study from Jordon was published in 2011 with the aim to determine the prevalence and factors associated with the development of antenatal and postnatal depression among Jordanian women. On sample (n = 353) we found that the rate of antenatal depression was 19%. AD was significantly associated with stress, anxiety, financial problems, perceived lack of parenting knowledge, difficult relationship with the mother-in-law, unplanned pregnancy, and low self-efficacy.[14]
The study from Oman was published in 2016 and it was a cross-sectional study aimed to determine the prevalence and risk factors of AD among Omani women in a primary care setting on the sample (n = 986) which found that 24.3% have AD. That is significantly related to unplanned pregnancies (OR: 1.37; 95% [CI]: 1.02–1.86) and marital conflict (OR: 13.83; 95% CI: 2.99–63.93).[15]
Locally, four studies were conducted; one in Jeddah, two in Riyadh and one in Dammam. The study of Jeddah was published in 2017 and was conducted to determine the prevalence and determinants of AD among women attending primary health care centers in Western Saudi Arabia. The prevalence of antepartum depression among pregnant women in Jeddah is 57.5% and the greatest contributor is the thought of harming herself.[1]
Out of the two studies from Riyadh, a first study published in 2016 was conducted to determine the prevalence and risk factors for antenatal depression among pregnant women attending clinics in Riyadh, on the sample (n = 420), and found that the prevalence of AD was 54.50% which was significantly associated with employment history, educational background, unintended pregnancy, and lack of partner support.[16] The second study published in 2015 aimed to determine the prevalence of depression among Saudi pregnant women to find correlation between sociodemographic, medical, and psychological history and depression on sample (n = 316) and found that the prevalence rates of AD were mild-to-severe and extreme depression was 18.6%, 11.7%, and 6.6%, respectively (44.2% using Becks %). There is significant correlation between depression and marital status of mother, status of the pregnancy, and health complications of previous pregnancies.[17]
One prospective cohort study from Eastern province published in 2018 aimed to determine anxiety and depression during pregnancy in women attending clinics in a university hospital and assess the associated factors on the sample (n = 575), which found that the prevalence of depression was 26.8% and the risk is higher among unemployed women with history of miscarriage and unplanned pregnancy.[18]
Methodology
Study settings and time: The study was conducted at multiple primary health care centers belonging to the Public Health Department, Ministry of Health in Al-Ahsa, Saudi Arabia in between April 1, 2018 and July 1, 2019.
Study design: A descriptive cross-sectional study.
Study population: All registered pregnant women attending antenatal clinics at primary health care centers (PHCC) in Al-Ahsa, Saudi Arabia.
Inclusion criteria
Pregnant women from all age groups.
Pregnant women who can understand Arabic.
Pregnant women belonging to all nationalities.
Pregnant women who follow up at PHCCs Antenatal clinics (ANC) at Ministry of Health (MOH)
Exclusion criteria: Pregnant women with obstetrical complications.
Study variables:
- Dependent variables:
Prevalence and risk factors of antenatal depression.
- Independent variables:
Sociodemographic data included age, educational qualification of mother, educational qualification of husband, current marital status, occupation, monthly income, gestational age, first antenatal visit, number of previous pregnancies, mode of previous deliveries, complications of previous pregnancies in multiparous women, complications in the current pregnancy, and Edinburgh Postnatal Depression Scale (EPDS) scores.
Sample Size: The sample size was calculated by the Raosoft website with a margin of error 5%, confidence level 95%, and population size 24287. The calculation showed that the sample size should be 370.[19]
Sampling technique: A multistage sampling technique was used. There were 70 primary health care centers in Al-Ahsa area. The first stage of sampling was done by cluster sampling, for which 70 primary health care centers in Al-Ahsa were divided into three regions i.e. Al Omran, Al-Mubarraz, and Al-Hofuf. Each region had different number of PHC centers i.e., Al Omran-24 PHCs, Al-Mubarraz-23 PHCs, and Al-Hofuf-25 PHC centers. The cluster sampling was done for all three regions proportionately. Thirty-two patients from each clustered PHC centers of Al Omran and Al-Hofuf and 42 patients from each clustered PHC of Al-Mubarraz were included in the study by simple random sampling. The second stage was systematic random sampling of patients from the chosen primary health centers in clusters (every third patient).
All PHCCs were coded and then the code was entered in a computer and microsoft excel was used to cluster sample of coded PHC that were taken randomly. Each chosen PHC enrolled through cluster sampling was visited and a systematic sampling technique of every third patient visiting the ANC of that PHC was taken into consideration.
Data collection tool: Self-administered validated questionnaire was used in the research done in Jeddah.
The questionnaire consisted of sociodemographic characteristics with the translated Arabic version of the Edinburgh Postnatal Depression Scale (EPDS) questionnaire.[1]
Range of EPDS scores:
0–9: Scores in this range may indicate the presence of some symptoms of distress that may be short-lived and are less likely to interfere with day-to-day ability to function at home or at work. However, if these symptoms persist for more than a week or two, further enquiries are warranted.
10–12: Scores within this range indicate the presence of symptoms of distress that may be discomforting. Repeat the EDS in 2 weeks period and continue monitoring progress regularly. If the scores increase to above 12 assess further and consider referral as needed.
13+: Scores above 12 require further assessment and appropriate management as the likelihood of depression is high. Referral to a psychiatrist/psychologist may be necessary.
Data collection technique:
A self-administered questionnaire was distributed by the researcher to pregnant women who have visited the antenatal clinic. The researcher was available to clarify any issue and the response was collected on the same day.
Data management:
Data were entered by investigators into a personal computer, and Statistical Package for the Social Sciences (SPSS) software IBM version 21 was used for appropriate statistical analysis. All variables were coded before entry and checked for accuracy before analysis.
Data analysis:
Data analysis was managed with the assistance of a statistical advisor as follows:
All continuous data were presented in mean, and standard deviation. Categorical data were presented in percentage and frequency.
Chi-square test was applied to compare two or more qualitative variables.
Student's t-test was used to compare two independent quantitative variables
Significance was determined at P value < 0.05 and a confidence level of 95%.
Binary logistic regression analysis was performed to explain the relationship between dependent and independent variables.
Ethical considerations:
Written permission from the Joint Program of Family and Community Medicine was obtained before conducting the research.
Written permission from the Public Health Department, Ministry of Health was requested before implementing the study.
All information from the questionnaire were kept confidential and could not be accessed except by the researcher and the statistician involved in the study.
Informed consent was taken before the respondents' involvement in the study.
Written consent was placed on the first page of the questionnaire. (There are approval from ethical committee and the date of approval was 13/12/2017).
Study strengths: To our knowledge, this is going to be the first study in Al-Ahsa city that provides the prevalence of AD and associated risk factors among pregnant women attending antenatal clinics in PHCs.
Study limitations:
The Edinburgh Postnatal Depression Scale (EPDS) was considered as a screening tool and not a diagnostic tool. Therefore, any score equal to or above 12 is only suggestive of depression and needs to be confirmed by a psychiatric specialist.
This study is a cross-sectional study. As a result, it is not possible to determine the causal relationship between depression and risk factors.
Study reporting and implementation: A scientific paper will be submitted at the end of the study which could be published in national and international journals.
Results
SECTION 1: Sociodemographic characteristics
The study sample consisted of 357 participants with different sociodemographic characteristics.
Distribution by marital status
Four categories expressed the marital status of the study sample (separated, married, divorced, and widowed).
Figure 1 shows that the distribution of the study sample. By marital status the distribution of the sample was made as follows: (0.3%) for separated, (97.5%) for married, (1.1%) for divorce, and (1.1%) for widowed.
Figure 1.
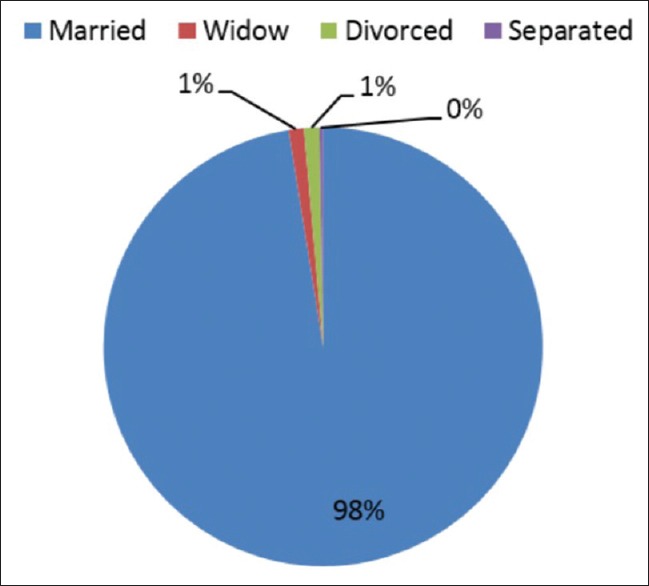
Distribution of the study sample by marital status
Distribution by age of the mother
The age of the mother was distributed in four categories: (<17 years, 18–27 years, 28–37 years, and > 37 years).
Figure 2 shows that the distribution of the study sample by age of the mother as follows: (1.7%) for < 17 years, (42.3%) for 18–27 years, (42.6%) for 28–37 years, and (13.4%) >37 years.
Figure 2.
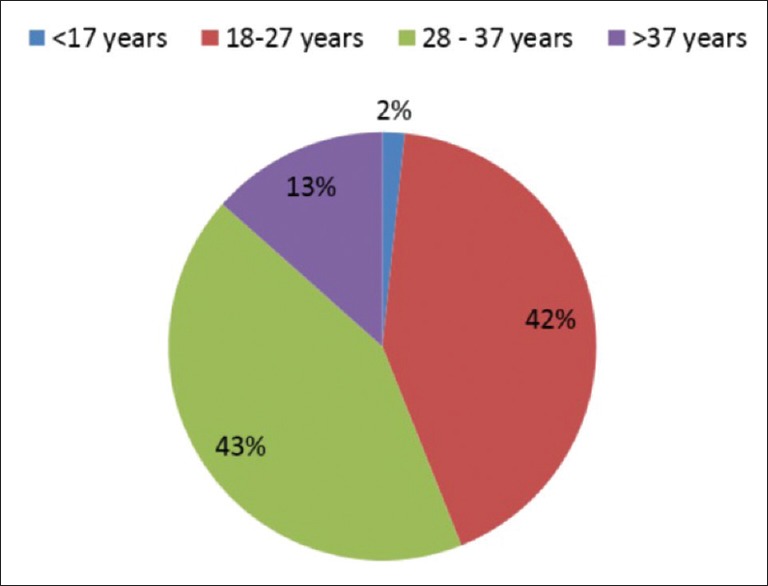
Distribution of the study sample by age of the mother
Distribution by Income
Income was distributed in four categories: (<2500 SR, 2500–5000 SR, 5000–10000 SR, and >10000 SR).
Figure 3 shows the distribution of the study sample by income as follows: (17%) for < 2500 SR, (31%) for 2500–5000 SR, (34%) for 5000–10000 SR, and (8%) for > 10000 SR.
Figure 3.
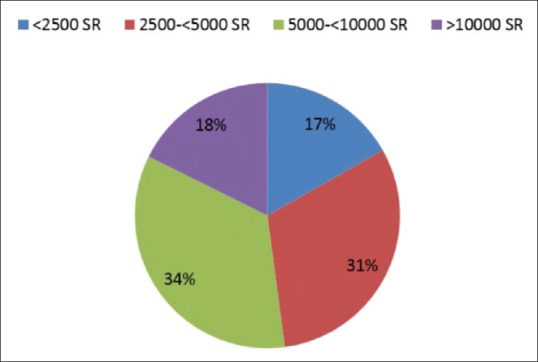
Distribution of the study sample by income
Distribution by Job
Job was distributed in eight categories: (housewife, teacher, physician, lawyer, engineer, administrative job, business, technical job, and others).
Table 1: Almost two-fifth of the interviewed pregnant women were 18–27 and two-fifth were 28–37, and almost 80% of the encountered women were high school educated or higher,
Table 1.
Frequencies, percentages for demographic and personal information (n=357)
| Demographic variables | n (%) |
|---|---|
| Mother’s Level of education | |
| Illiterate | 5 (1.4) |
| Read/Write | 12 (3.4) |
| Primary/Secondary | 56 (15.7) |
| High school or more | 284 (79.6) |
| Father’s level of education | |
| Read/Write | 7 (2) |
| Primary/Secondary | 77 (21.6) |
| High school or more | 264 (73.9) |
| Job | |
| Housewife | 251 (70.3) |
| Student | 12 (3.4) |
| Teacher | 25 (7) |
| Physician/Lawyer/Engineer | 20 (5.6) |
| Administrative job | 10 (2.8) |
| Business | 2 (0.6) |
| Technical job | 5 (1.4) |
| Other | 32 (9) |
15% were primary and secondary, and 70% of them housewives (jobless). Among the husbands' education level, almost three quarters had a high level of education. Most of the women were yet to be married and one-third of them reported monthly income 2500–5000 SAR and one-third reported 5000–1000 SAR.
SECTION 2: Risk factors
Table 2: Three-quarters of them had their first visit in the first trimester. And approximately they were distributed by third in each trimester (31%, 37%, and 31%, respectively) with more than half of pregnancy (60%) were planned and less than third accidental (28%), and half of them (50%) had more than 2 year separation between pregnancies and 80% of them did not have any complication in their current pregnancy. Most of the multiparty women had normal vaginal delivery, and 60% of them had no complications after the past delivery. Moreover, 65% of the interviewed woman did not experience abortion while 35% had at least once, with some psychological complications postabortion
Table 2.
Frequencies and percentages of the responses to the questions related to the risk factors (n=357)
| Obstetric history | |
|---|---|
| Characteristics | n (%) |
| First Antenatal Care visit | |
| 1st trimester | 290 (81.2) |
| 2nd trimester | 55 (15.4) |
| 3rd trimester | 12 (3.4) |
| Gestational age for current pregnancy | |
| 1st trimester | 111 (31.1) |
| 2nd trimester | 133 (37.3) |
| 3rd trimester | 113 (31.7) |
| Pregnancy mode | |
| Planned | 216 (60.5) |
| Accidental | 103 (28.9) |
| Unwanted | 38 (7.6) |
| Complications of previous pregnancies | |
| Medical | 36 (10.1) |
| Psychological | 16 (4.5) |
| Obstetric | 25 (7) |
| More than one complication | 13 (3.6) |
| No complications | 194 (54.3) |
| Complications of present pregnancies | |
| Medical problems | 40 (11.2) |
| Psychological problems | 12 (3.4) |
| More than one complication | 12 (3.4) |
| No complications | 293 (82.1) |
| Number of previous pregnancies plus abortions | |
| Nulliparous | 76 (21.3) |
| <5 | 218 (61.1) |
| ≤5 deliveries | 61 (17.1) |
| Mode of previous deliveries | |
| NVD | 210 (58.8) |
| LSCS | 37 (10.4) |
| both NVD and CS | 29 (8.1) |
| Complications after delivery | |
| Medical | 20 (5.6) |
| Psychological | 26 (7.3) |
| No complications | 220 (61.6) |
| Postabortion psychological complications | |
| Depression | 19 (5.3) |
| Anxiety | 10 (2.8) |
| Sadness | 42 (11.8) |
| None | 108 (30.3) |
Table 3: It shows the contribution of each item of the EPDS in the overall score and the most important parameter that contributed was blaming oneself when things went wrong (1.7 ± 0.99), or when things have been getting on top of her (1.5 ± 0.98), or when things have been getting on top of me (1.3 ± 0.92)
Table 3.
Edinburgh Postnatal Depression Scale (EPDS)
| Items of EPDS | Mean±SD |
|---|---|
| I have been able to laugh and see the funny side of things | 0.5±0.72 |
| I have looked forward with enjoyment to things: | 0.5±0.72 |
| I have blamed myself unnecessarily when things went wrong | 1.7±0.99 |
| I have been anxious or worried for no good reason | 1.3±0.92 |
| I have felt scared or panicky for no very good reason | 1.2±1.03 |
| Things have been getting on top of me | 1.5±0.98 |
| I have been so unhappy that I have had difficulty sleeping: | 1±0.99 |
| I have felt sad or miserable | 0.8±0.99 |
| I have been so unhappy that I have been crying | 0.7±0.96 |
| The thought of harming myself has occurred to me | 0.1±0.56 |
| Total average | 9.8 |
Table 4: It shows that about one third (31.9%) of the participants has risk to have depression, (5.6%) have high risk and (26.3%) have possible risk.
Table 4.
Mean scores for the response of the pregnant women on the EPDS items assessing depression (score 0-3 for each item)
| Categories of depression | n | % | Mean±SD |
|---|---|---|---|
| Low risk | 243 | 68.1% | 7±3.17 |
| Possible risk | 94 | 26.3% | 14.9±1.7 |
| High risk | 20 | 5.6% | 20.2±1.64 |
Table 5: It shows that there was a significant relationship between depression levels and high school or more education levels (P = 0.019).
Table 5.
Association between depression levels and socioeconomics variables
| Depression levels with | Chi-square | P | In favor of |
|---|---|---|---|
| Age of mother | 4.436 | 0.618 | |
| Level of education | 12.28 | 0.056 | |
| Level of education | 15.21 | 0.019 | High school or more |
| Job | 20.34 | 0.120 | |
| Marital Status | 8.07 | 0.233 | |
| Income | 10.64 | 0.100 | |
| Difficulties faced by the mother | 24.11 | 0.020 | Financial burden |
In addition, there was a significant relationship between depression levels and financial burden as a difficulty faced by the mother (P = 0.02).
Table 6: It shows the results of the logistic regression model for predictors of AD based on our participant group. Suffering problems or difficulty in sleeping, having a smoker husband, having one abortion, and having anxiety due to postabortion complications were significant predictors. Controlling factors such as suffering problems or difficulty in sleeping increases the likelihood for depression by almost six-fold (odds ratio, 6.572, 95% confidence interval [CI]: 1.321–32.692), having a smoker husband increases it by almost four-fold (odds ratio, 4.177, 95% CI: 1.178–14.813), having one previous pregnancy increases it by around 6-fold (odds ratio, 6.47, 95% CI: 1.574–26.58), having post-abortion psychological complications (anxiety) increases it by 3-fold (odds ratio, 3.611, 95% CI: 1.974–6.604), P value < 0.05.
Table 6.
Logistic regression of antenatal depression
| B | S.E. | Wald | P | Exp (B) | 95% C.I. for EXP (B) | ||
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| Have you ever suffered problems or difficulty sleeping | 1.883 | 0.819 | 5.291 | 0.021 | 6.572 | 1.321 | 32.692 |
| Is your husband smoker | 1.429 | 0.646 | 4.898 | 0.027 | 4.177 | 1.178 | 14.813 |
| Number of previous pregnancies plus abortions (one) | 1.867 | 0.721 | 4.597 | 0.032 | 6.47 | 1.574 | 26.58 |
| Postabortion psychological complications (anxiety) | 1.284 | 0.308 | 4.087 | 0.043 | 3.611 | 1.974 | 6.604 |
| Constant | 3.261 | 0.957 | 4.687 | 0.995 | 26.08 | ||
Discussion
In this study, AD prevalence was measured among 357 women attending the PHC centers in the Ministry of Health. The prevalence of antenatal depression was 31.9%, a prevalence which is slightly higher than that reported by Alqahtani et al.,[18] who found the prevalence was 26.8% among pregnant women in Eastern Province, Saudi Arabia. These differences might be attributed to the study design used. We used the cross-sectional method which is descriptive and takes a short duration of time rather than cohort study. In addition, our study setting was PHC centers rather than a university hospital. In addition, the prevalence was higher than reported from the US (16.6%),[5] Africa (24.9%),[9] Ethiopia (21.5%),[8] Nigeria (24.5%),[10] Nigeria (22%)[11] Asia (China 28.5%,[3] Malaysia 20%,[12] Oman 19%,[15] and Jordan 24.3%[14]). Our detected prevalence was lower than that found in Riyadh, Saudi Arabia,[16] the dissimilarity could be attributed to the sample size which is higher in Riyadh study consisting 420 pregnant women than our current study consisting of 357 pregnant women.
In this study the factors that showed greater association with antenatal depression included suffering problems or difficulty in sleeping, having a smoker husband, having one previous pregnancy, and having postabortion psychological complications. Our analysis revealed suffering problems or difficulty sleeping and having one previous pregnancy were the significant predictors of depression, suffering problems, or difficulty in sleeping.
In comparison to other research papers, our study did not find any direct relation between income and depression but it was associated with increase in anxiety (anxious or worried for no good reason P = 0.002), also we couldn't see direct relation between employment and depression but being unemployed correlated with blaming and being anxious or worried for no good reason (P = 0.007 and P = 0.021, respectively). Unplanned pregnancy and age of mother were not found to be risk factors in our research.
Conclusion and Recommendations
In conclusion, we found that the prevalence of depression among pregnant women in Al-Ahsa region was higher with largest contributors for blaming themselves for unnecessarily reasons when things went wrong, for being anxious or worried for no good reason, for things which have been getting on top of them along with several risk factors such as having problems or difficulty in sleeping, history of abortions and history of postabortion anxiety.
In fact, the physician in the primary care centers can screen mothers for their stressors, guide them to deal with the stress of pregnancy and even extend referral services, if needed. Furthermore, it has been recommended that family physicians should have a high index of suspicion, and assess the mother for the presence of depression during their health center visits. In addition, the most important intervention can be to design a comprehensive public health policy, to ensure that universal psychosocial assessment in perinatal women is undertaken within the primary health care system.
We recommend that pregnant women should be routinely screened for depression during her visits to PHC centers, especially those with the risk of depression. Moreover, women with risk factor who is planning to be pregnant should receive health education about measures they can take to avoid AD.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Bawahab JA, Alahmadi JR, Ibrahim AM. Prevalence and determinants of antenatal depression among women attending primary health care centers in Western Saudi Arabia. Saudi Med J. 2017;38:1237–42. doi: 10.15537/smj.2017.12.21262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Maternal Mental Health. Available from: www.who.int/reproductivehealth/publications/general/9789241563567/en .
- 3.Zeng Y, Cui Y, Li J. Prevalence and predictors of antenatal depressive symptoms among Chinese women in their third trimester: A cross-sectional survey. BMC Psychiatry. 2015;15:66. doi: 10.1186/s12888-015-0452-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mohamad Yusuff AS, Tang L, Binns CW, Lee AH. Prevalence of antenatal depressive symptoms among women in Sabah, Malaysia. J Matern Fetal Neonatal Med. 2016;29:1170–4. doi: 10.3109/14767058.2015.1039506. [DOI] [PubMed] [Google Scholar]
- 5.Ashley JM, Harper BD, Arms-Chavez CJ, LoBello SG. Estimated prevalence of antenatal depression in the US population. Arch Womens Ment Health. 2016;19:395–400. doi: 10.1007/s00737-015-0593-1. [DOI] [PubMed] [Google Scholar]
- 6.Castro E Couto T, Cardoso MN, Brancaglion MY, Faria GC, Garcia FD, Nicolato R, et al. Antenatal depression: Prevalence and risk factor patterns across the gestational period. J Affect Disord. 2016;192:70–5. doi: 10.1016/j.jad.2015.12.017. [DOI] [PubMed] [Google Scholar]
- 7.Biratu A, Haile D. Prevalence of antenatal depression and associated factors among pregnant women in Addis Ababa, Ethiopia: A cross-sectional study. Reprod Health. 2015;12:99. doi: 10.1186/s12978-015-0092-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Duko B, Ayano G, Bedaso A. Depression among pregnant women and associated factors in Hawassa city, Ethiopia: An institution-based cross-sectional study. Reprod Health. 2019;16:25. doi: 10.1186/s12978-019-0685-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rwakarema M, Premji SS, Nyanza EC, Riziki P, Palacios-Derflingher L. Antenatal depression is associated with pregnancy-related anxiety, partner relations, and wealth in women in Northern Tanzania: A cross-sectional study. BMC Womens Health. 2015;15:68. doi: 10.1186/s12905-015-0225-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thompson OK, Ajayi IK. Prevalence of antenatal depression and associated risk factors among pregnant women attending antenatal clinics in Abeokuta North Local Government Area, Nigeria. Depression Res Treatment. 2016:2016. doi: 10.1155/2016/4518979. doi: 10.1155/2016/4518979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Afusat OB. Prevalence and associated factors of anxiety and depression among pregnant women? Open Access J Neurol Neurosurg. 2018;9:555758. doi: 10.19080/OAJNN.2018.09. [Google Scholar]
- 12.Rashid A, Mohd R. Poor social support as a risk factor for antenatal depressive symptoms among women attending public antennal clinics in Penang, Malaysia. Reprod Health. 2017;14:144. doi: 10.1186/s12978-017-0404-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sheeba B, Nath A, Metgud CS, Krishna M, Venkatesh S, Vindhya J, et al. Prenatal depression and its associated risk factors among pregnant women in Bangalore: A hospital based prevalence study. Front Public Health. 2019;7:108. doi: 10.3389/fpubh.2019.00108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mohammad KI, Gamble J, Creedy DK. Prevalence and factors associated with the development of antenatal and postnatal depression among Jordanian women. Midwifery. 2011;27:e238–45. doi: 10.1016/j.midw.2010.10.008. [DOI] [PubMed] [Google Scholar]
- 15.Al-Azri M, Al-Lawati I, Al-Kamyani R, Al-Kiyumi M, Al-Rawahi A, Davidson R, et al. Prevalence and risk factors of antenatal depression among Omani women in a primary care setting: Cross-sectional study. Sultan Qaboos Univ Med J. 2016;16:e35–41. doi: 10.18295/squmj.2016.16.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alotaibe H, Elsaid T, Almomen R. The prevalence and risk factors for antenatal depression among pregnant women attending clinics in Riyadh, Saudi Arabia. Eur J Pharm Med Res. 2016;3:60–7. [Google Scholar]
- 17.Moawed SA, Gemaey EM, Al-Mutairi HA. Prevalence of depression among saudi pregnant women. IOSR J Nurs Health Sci. 2015;4:61–8. [Google Scholar]
- 18.Alqahtani AH, Al Khedair K, Al-Jeheiman R, Al-Turki HA, Al Qahtani NH. Anxiety and depression during pregnancy in women attending clinics in a University Hospital in Eastern province of Saudi Arabia: Prevalence and associated factors. Int J Womens Health. 2018;10:101–8. doi: 10.2147/IJWH.S153273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Raosoft.com . Sample Size Calculator by Raosoft, Inc. [online] [Last accessed on 2018 Mar 26]. Available from: http://www.raosoft.com/samplesize.html .


