Abstract
Background:
Breastfeeding plays an important role in both maternal and infant health and well-being. While researchers have examined the relationship between postpartum psychological distress and breastfeeding behaviors, few have investigated links between prenatal distress, postpartum distress, and breastfeeding behaviors over time.
Research Aim:
We aimed to determine if prenatal breastfeeding beliefs and psychological distress during and after pregnancy were associated with initiation and early cessation rates of breastfeeding.
Methods:
In our secondary data analysis, a nonexperimental longitudinal one-group design was used. We assessed pregnant women (N = 70) during four perinatal visits (early, mid, and late pregnancy and 7–10 weeks postpartum). Participants completed self-report surveys about psychological distress and depressive symptoms at each visit, breastfeeding beliefs during the third visit, and breastfeeding behaviors at the postpartum visit.
Results:
Participants who breastfed for ⩾8 weeks had more positive beliefs about breastfeeding prior to delivery than participants with early cessation, who in turn had more positive beliefs than those who never initiated. Participants with early cessation reported heightened levels of pregnancy-specific distress in early pregnancy compared to those who continued breastfeeding or never initiated. Participants who continued breastfeeding for ⩾8 weeks reported less general anxiety and depressive symptoms in postpartum than those who discontinued or never initiated.
Conclusions:
Prenatal beliefs about breastfeeding, pregnancy-specific distress in early pregnancy, and general anxiety and depressive symptoms in postpartum are associated with breastfeeding initiation and continuation. Of clinical relevance, addressing prenatal and postpartum distress in the implementation of breastfeeding practice interventions could improve breastfeeding rates.
Keywords: breastfeeding duration, breastfeeding initiation, breastfeeding practices, maternal psychology
Background
The World Health Organization (WHO, 2016) recommends exclusive breastfeeding for 6 months and continued breastfeeding for at least 1 year for optimal health benefits including decreased maternal postpartum depression and reduced likelihood of adult obesity for the offspring (Victora et al., 2016). Despite the important role breastfeeding plays in the health and well-being of mothers and infants, rates of breastfeeding initiation, duration, and exclusivity in the United States remain below U.S. Department of Health and Human Services national goals (Centers for Disease Control and Prevention [CDC], 2016, 2017). In 2016, the U.S. initiation rate of 81.1% approached the national goal of 81.9%, but only 51.8% of mothers continued to breastfeed for at least 6 months, which is below the national goal of 60.6% (CDC, 2016, 2017). Among women of lower socioeconomic status (SES), initiation and duration rates are even lower. Initiation rates range from 73.2% to 75.5% depending on the socioeconomic indicator, while 6-month duration rates range from 40.9% to 42.4% (CDC, 2015). For the U.S. population over-all, both initiation and duration rates have increased less than 10% between 2007 and 2016, suggesting that breastfeeding education, support, initiatives, and health care provider training may have impacted breastfeeding rates at a relatively slow pace, particularly for women with lower SES (Balogun et al., 2016; CDC, 2016, 2017; Lumbiganon et al., 2016).
Given the link between breastfeeding and maternal/infant health, researchers have examined sociodemographic characteristics and beliefs about breastfeeding associated with breastfeeding initiation, duration, and exclusivity. Several demographic and maternal factors (e.g., racial/ethnic minority status, higher prepregnancy body mass index [BMI], low SES, and younger age) reduce the likelihood that women will initiate breastfeeding, exclusively breastfeed for 6 months, or continuing breastfeeding through one year (Bartick et al., 2017; Gerd, Bergman, Dahlgren, Roswall, & Alm, 2012; Kitsantas, Gaffney, & Kornides, 2012; Mehta, Siega-Riz, Herring, Adair, & Bentley, 2012). In addition, less positive beliefs/attitudes about breastfeeding, particularly low self-efficacy, are associated with less intention to breastfeed as well as reduced likelihood of initiation and shorter breastfeeding duration (Brown, 2014). Many of these factors are interconnected resulting in particularly low breastfeeding rates among women of lower SES (Dozier, Nelson, & Brownell, 2012; Kitsantas et al., 2012).
Sociodemographic factors and breastfeeding beliefs/attitudes also correspond with psychological functioning (Brockway, Benzies, & Hayden, 2017; Chong, Biehle, Kooiman, & Mickelson, 2016; Dozier et al., 2012; Hinic, 2016). Researchers have observed a strong link between prenatal and/or postpartum depressive symptoms and breastfeeding practices (Dias & Figueiredo, 2015). Specifically, greater prenatal and/or postpartum depressive symptoms are associated with lack of intention, failure to initiate, and early cessation of breastfeeding (Dias & Figueiredo, 2015).
In contrast to the extensive literature on depression and breastfeeding, few researchers have examined how other forms of psychological distress during pregnancy (e.g., pregnancy-specific distress, anxiety, and perceived stress) relate to subsequent breastfeeding practices (Fallon, Bennett, & Harrold, 2016). In their review of the literature on prenatal anxiety and infant feeding outcomes, Fallon and colleagues (2016) found that the few researchers who investigated prenatal distress and breastfeeding behaviors used a variety of distress measures and produced mixed results. While none of these researchers reported an association between prenatal distress and breastfeeding initiation or duration, a few showed a relationship between high levels of prenatal distress and breastfeeding intention and exclusivity. Fallon and colleagues, however, determined that the low number of studies available provided insufficient evidence to make conclusions about the nature of relationships between these factors. In addition, researchers examining prenatal predictors have focused on distress at a single time point (Dozier et al., 2012; Fallon et al., 2016). Examining longitudinal data regarding different types of distress across pregnancy in relation to breastfeeding practices may inform the development of interventions to promote breastfeeding. Moreover, women who continue breastfeeding for at least 6 to 8 weeks are more likely to continue for 6 to 12 months because initial success is critical to establishing long-term continuation (Gerd et al., 2012). Thus, understanding predictors of early cessation is of clinical importance.
Building on the existing literature, we aimed to determine if prenatal breastfeeding beliefs and psychological distress during and after pregnancy were associated with initiation and early cessation rates of breastfeeding with the current study. In particular, our study addressed the following research questions:
Do women with more positive beliefs about breastfeeding have higher rates of initiation and lower rates of early cessation, defined as discontinuation at <8 weeks postpartum?
Do women reporting greater perceived stress, pregnancy-specific distress, general anxiety, and depressive symptoms during pregnancy and postpartum have lower rates of initiation and higher rates of early cessation?
Methods
Design
This investigation is a secondary analysis of data collected in a nonexperimental longitudinal one-group study of pregnant women focused on immune function. The larger study included self-report surveys, used in this study, and collection of blood samples (not used in the current analyses). As we were interested in the influence of women’s perceptions and beliefs on breastfeeding behaviors, self-report surveys allowed us to collect data on how women perceived their distress levels, depressive symptoms, and the act of breastfeeding. The longitudinal study design provided us with data on distress and depressive symptoms across pregnancy and postpartum to help fill a significant gap in the literature (Fallon et al., 2016). The Ohio State University Biomedical Institutional Review Board approved the study.
Setting
We conducted this study in Columbus, Ohio. Columbus is a city in the midwestern region of the United States with a population of 860,090 (U.S. Census Bureau, 2017). While Columbus has a predominantly white population (61%), the percentage of black or African American people living in Columbus (27%) is higher than the national percentage (13.3%; U.S. Census Bureau, 2017). Hispanic and Asian residents account for less than 10% of the remaining population. The percentage of people living below the poverty line (21.2%) is above the national percentage of 12.2% as well (U.S. Census Bureau, 2017). According to the CDC (2016), Ohio’s breastfeeding initiation rate of 77.7% did not meet the Healthy People 2020 goal in 2016. In addition, Ohio’s breastfeeding and duration rates are lower than national rates. Exploring additional factors that could influence women’s decisions about breastfeeding, therefore, is an essential step to improving breastfeeding rates in Ohio.
Sample
Women in early pregnancy were the target population to collect data across pregnancy and in the postpartum period. Thus, we recruited 84 women in early pregnancy from Ohio State University Wexner Medical Center and surrounding community of Columbus. As we focused on immune function in the larger study, we excluded women with diabetes, chronic conditions with implications for immune function (e.g., rheumatoid arthritis, multiple sclerosis, or human immunodeficiency virus), hypertension illicit drug use, drinking more than two alcoholic drinks per week during pregnancy (per self-report or via medical record review), or fetal anomaly. In addition, we excluded 14 participants from the larger sample from the current analyses because they did not complete the surveys about breastfeeding beliefs and breastfeeding behaviors. Within our final sample of 70 women, participants were rescheduled if they reported acute illness (e.g., cold or flu-like symptoms) or antibiotic use occurring within 10 days of a scheduled study visit. As this study was a secondary analysis, we did not conduct an a priori power analysis to show sample size adequacy. We performed post hoc power analyses for four psychosocial measures described in Table 1 (NUPDQ, STAI, CES-D, PSS). The two measures that produced significant results across time between groups, NUPDQ and STAI, had observed power of 0.870 and 0.593, respectively. The two measures for which we did not find significant differences between groups, CES-D and PSS, had observed power of 0.290 and 0.316, respectively. At the end of each study visit, participants received modest financial compensation.
Table 1.
Questionnaire Measures.
| Variable | Measure | # of questions | Types of questions | Reliabilitya |
|---|---|---|---|---|
| Breastfeeding beliefs | Breastfeeding Beliefs Scale (BBS)b | 18 | Knowledge, self-efficacy, embarrassment, time and social constraint, lack of social support | α = .783 |
| Depressive symptoms | Center for Epidemiological Studies Depression Scale (CES-D)c | 20 | Emotional, somatic, and cognitive symptoms of depression | α = .910 |
| Perceived stress | Perceived Stress Scale (PSS)d | 10 | Perceptions of stress levels | α = .870 |
| State anxiety | State-Trait Anxiety Inventory (STAI)e | 6 | Current emotional state | α = .934 |
| Pregnancy-specific distress | Revised Prenatal Distress Questionnaire (NUPDQ)f | 17 | Distress regarding financial resources, pain during delivery, and physical discomforts | α = .743 |
| Breastfeeding behaviors | Self-report of breastfeeding behaviors | 5 | Breastfeeding initiation and duration, daily frequency of formula | n/a |
Cronbach’s alphas were calculated for this study population.
Measurement
We collected demographic data about age, race/ethnicity, marital status, education, annual household income, self-reported socioeconomic class, postpartum employment status, total number of births (parity), and total number of pregnancies (gravidity) via self-report. The demographic variables did not connect directly to our research questions.
We determined parental attitudes about pregnancy by asking participants to rate their happiness and their perception of their partner’s happiness at the time pregnancy became known on a scale of 1 (unhappiness) to 10 (happiness). We assessed pregnancy intendedness by asking participants if their current pregnancy was planned or unplanned. We calculated prepregnancy BMI (kg/m2) utilizing self-reported prepregnancy weight and height (measured at the first visit). Finally, we collected information on mode of delivery (vaginal versus caesarean section) with medical record review. Again, these variables were not directly connected to our research questions.
As summarized in Table 1, to address our aims, we assessed perceived stress, anxiety, depressive symptoms, and breastfeeding beliefs using self-report questionnaires validated in pregnant women. We also administered questions regarding breastfeeding behaviors (initiation, duration), intention to breastfeed, and prior breastfeeding experience. While the CES-D has shown predictive validity for breastfeeding duration and beliefs, few researchers have investigated how our other measures connect to breastfeeding beliefs and behaviors (Chaudron et al., 2001; Pippins, Brawarsky, Jackson, Fuentes-Afflick, & Haas, 2006; Taveras et al., 2003).
Data Collection
Data collection occurred between July 2011 and January 2014. Women were assessed at three study visits during pregnancy and one at postpartum (Table 2). We collected all data in person at the Clinical Research Center at the Ohio State University Wexner Medical Center after obtaining written informed consent at the initial visit. We conducted study visits in a closed room and all study-related information was kept on password-protected computers and/or in a locked file cabinet to maintain confidentiality.
Table 2.
Data Collection Timeline.
| Study visit | ||||
|---|---|---|---|---|
| Data collection measure | Early pregnancy (12.9 ± 1.4 weeks) |
Midpregnancy (21.0 ± 1.3 weeks) |
Late pregnancy (29.8 ± 1.4 weeks) |
Postpartum (8.5 ± 0.7 weeks) |
| Demographics | X | |||
| Parental happiness | X | |||
| Pregnancy intendedness | X | |||
| CES-D | X | X | X | X |
| PSS | X | X | X | X |
| STAI | X | X | X | X |
| NUPDQ | X | X | X | |
| BBS | X | |||
| Breastfeeding behaviors | X | |||
Data Analysis
Based on breastfeeding initiation and duration, we categorized participants into the following groups: (a) participants who never initiated breastfeeding, (b) participants who discontinued prior to 8 weeks postpartum, and (c) participants who continued for ⩾8 weeks. We evaluated differences in demographic and descriptive characteristics between the three groups with chi-square tests and one-way ANOVAs, as appropriate. To address our first research question, we conducted one-way ANOVAs to assess differences in breastfeeding beliefs between the groups. To address our second research question, we used repeated measures ANOVAs to ascertain if the breastfeeding groups’ trajectories varied for perceived stress, pregnancy-specific distress, general anxiety, and depressive symptoms across pregnancy and postpartum (if applicable). We then conducted one-way ANOVAs for perceived stress, general anxiety, and depressive symptoms at each pregnancy time point and postpartum to further explore any effects that we observed in the repeated measures ANOVA results and evaluate any differences between the groups during or after pregnancy. We also used one-way ANOVAs to determine if groups differed in pregnancy-specific distress at any pregnancy time point. All analyses were conducted in SPSS version 22.0 (IBM Corporation, 2013).
Results
Differences in Demographic and Descriptive Characteristics
Tables 3 and 4 show demographic and descriptive characteristics for the three breastfeeding groups. Differences in these characteristics are described below as several of these characteristics impact distress, depressive symptoms, and breastfeeding beliefs and therefore affect how we interpreted the results in answering our research questions.
Table 3.
Demographic and Descriptive Characteristics by Breastfeeding Group (N = 70).
| Never initiated, 9 (12.9%) |
Early cessation (<8 weeks), 24 (34.3%) |
Continuing for ≥ 8 weeks, 37 (52.9%) |
||
|---|---|---|---|---|
| Race | ||||
| White or other | 4 (44.4) | 13 (52.0) | 20 (54.1) | χ2(2) = 0.3, p = .86 |
| Black | 5 (55.6) | 12 (48.0) | 17 (45.9) | |
| Employment | ||||
| Employed at V1 | 6 (66.7) | 18 (75.0) | 24 (64.9) | |
| Employed at V4 (includes maternity leave) | 6 (66.7) | 13 (54.2) | 23 (62.2) | χ2(2) = 0.6, p = .75 |
| Maternity leave | 0 (0.0) | 2 (8.3) | 5 (21.4) | |
| Family income | χ2(10) = 18.7, p = .04 | |||
| Less than $15,000 | 2 (22.2) | 8 (33.3) | 9 (24.3) | |
| $15,000-$29,999 | 6 (66.7) | 10 (41.7) | 5 (13.5) | |
| $30,000-$49,999 | 1 (11.1) | 3 (12.5) | 10 (27.0) | |
| $50,000-$74,999 | 0 (0.0) | 0 (0.0) | 7 (18.9) | |
| $75,000-$99,999 | 0 (0.0) | 2 (8.3) | 4 (10.8) | |
| $100,000 and above | 0 (0.0) | 1 (4.2) | 2 (5.4) | |
| Socioeconomic statusa | χ2(6) = 13.0, p = .04 | |||
| Lower | 0 (0.0) | 4 (16.7) | 6 (16.2) | |
| Working | 8 (88.9) | 15 (62.5) | 12 (32.4) | |
| Lower middle | 1 (11.1) | 3 (12.5) | 13 (35.1) | |
| Upper middle | 0 (0.0) | 2 (8.3) | 6 (16.2) | |
| Higher | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Unplanned pregnancy | 7 (77.8) | 18 (72.0) | 18 (48.6) | χ2(2) = 4.3, p = .11 |
| Delivery route | χ2(2) = 2.3, p = .32 | |||
| Vaginal delivery | 7 (13.5) | 17 (32.7) | 28 (53.8) | |
| C-section | 2 (15.4) | 8 (32.0) | 8 (21.6) | |
Table 4.
Breastfeeding Intention and Practices by Breastfeeding Group (N = 70).
| Never initiated, 9 (12.9%) |
Early cessation (<8 weeks), 24 (34.3%) |
Continuing for ≥8 weeks, 37 (52.9%) |
||
|---|---|---|---|---|
| Breastfeeding experience | Breastfed >6 months vs. no experience | |||
| First biological child | 1 (11.1) | 12 (48.0) | 10 (27.0) | χ2(8) = 41.7, p < .01 |
| Has child—never breastfed | 6 (66.7) | 4 (16.0) | 0 (0.0) | |
| Breastfed for at least 1 week | 1 (11.1) | 5 (20.0) | 3 (8.1) | |
| Breastfed for at least 3 months | 1 (11.1) | 1 (4.0) | 5 (13.5) | |
| Breastfed for at least 6 months | 0 (0.0) | 2 (8.0) | 19 (51.4) | |
| Intending to breastfeed | 3 (33.3) | 23 (92.0) | 36 (97.3) | Never initiated vs. early cessation, χ2(1) = 15.3, p < .01 |
| Never initiated vs. continuing, χ2(1) = 23.0, p < .01 | ||||
| Intending to use formula | Intending to use formula vs. not intending to use formula, χ2(2) = 2.9, p = .24 | |||
| No | 1 (11.1) | 13 (52.0) | 26 (70.3) | |
| Less than once per week | 0 (0.0) | 1 (4.0) | 5 (13.5) | |
| A few times per week | 0 (0.0) | 7 (28.0) | 5 (13.5) | |
| Once per day | 0 (0.0) | 2 (8.0) | 0 (0.0) | |
| More than once per day | 2 (22.2) | 0 (0.0) | 0 (0.0) | |
The three breastfeeding groups (never initiated, early cessation, continuing) did not differ significantly for several demographic factors, although there were significant differences in age, SES, and average household income (Table 3). Participants with early cessation were significantly younger than those who never initiated (p = .02) and those who continued breastfeeding (p < .01). In addition, participants who continued breastfeeding self-identified as having a higher socioeconomic class and reported higher average household incomes than those with early cessation or who never initiated. The groups did not differ significantly, however, in prepregnancy BMI, F(2, 67) = 2.5, p = .09, or parental happiness about current pregnancy as rated by the mother; mother: F(2, 67) = 0.2, p = .82; father: F(2, 67) = 0.1, p = .89.
Table 4 shows significant differences in breastfeeding intention and experience. Among participants who did intend to breastfeed, those who ultimately did not initiate planned to breastfeed for significantly fewer weeks than participants in the early cessation (p < .01) and continuing groups (p < .01). Last, participants who were still breastfeeding at the postpartum follow-up were more likely to have previously breastfed for ⩾6 months than those who never initiated or who had early cessation.
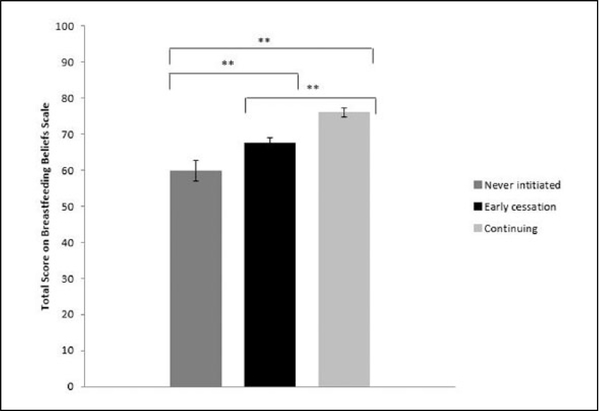
Research Question 1: Breastfeeding Beliefs and Behaviors
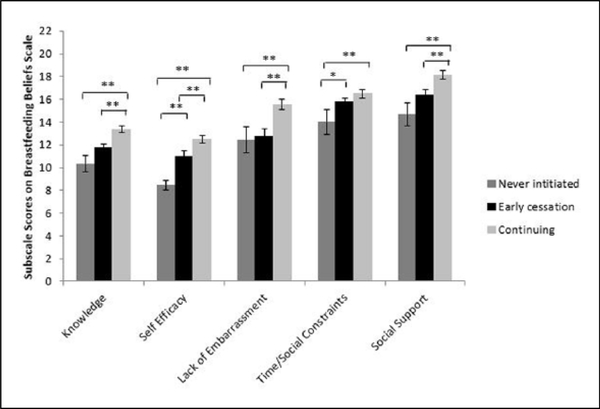
We observed significant differences between the three groups in beliefs about breastfeeding, F(2, 67) = 20.7, p < .01. Participants who continued breastfeeding had more positive beliefs about breastfeeding (per higher total score on the BBS) at the third trimester assessment than those with early cessation (p < .01), who in turn had more positive beliefs than those who never initiated (p = .01; Figure 1). As shown in Figure 2, significant differences between groups in the expected directions were observed for each subscale.
Figure 1.
Total scores on the BBS (M ± SE) from the third trimester visit (Visit 3) by breastfeeding group. Higher scores indicate more positive beliefs. **p ⩽ .01.
Figure 2.
Subscale scores on the BBS (M ± SE) from the third trimester visit (Visit 3) by breastfeeding group. Higher scores indicate more positive beliefs. *p ⩽ .05. **p ⩽ .01.
In the next section, we explore psychosocial factors that could affect breastfeeding beliefs as well as breastfeeding behaviors independent of beliefs. Unlike breastfeeding beliefs, however, the relationship between these psychosocial factors is not well understood. In particular, little is known about connections between prenatal distress, postnatal depression, anxiety, and breastfeeding behaviors (Fallon et al., 2016; Zhu, Hao, Jiang, Huang, & Tao, 2013).
Research Question 2: Psychosocial Functioning and Breastfeeding Behaviors
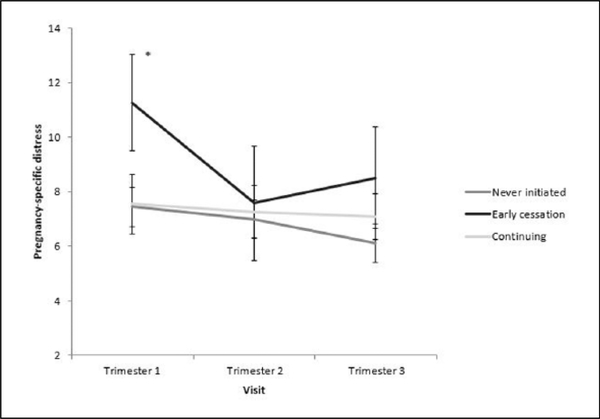
Regarding pregnancy-specific distress, a significant quadratic effect emerged over time by group, F(2, 67) = 6.0, p < .01. Post hoc comparisons demonstrated a significant difference in the first trimester, F(2, 67) = 4.7, p = .01, with participants with early cessation reporting significantly higher pregnancy-specific distress in the first trimester compared to the other two groups (ps ⩽ .05; Figure 3).
Figure 3.
Pregnancy-specific distress (per scores on the NUPDQ; mean ± SE) by breastfeeding group across pregnancy. * ps ⩽ .05.
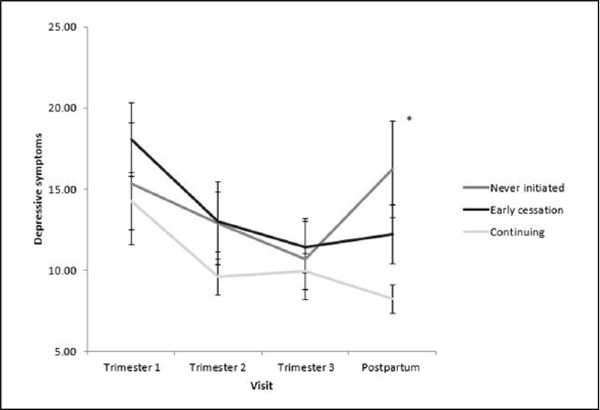
Depressive symptoms (per CES-D) showed a quadratic pattern of change over time, F(1, 67) = 10.7, p < .01. This pattern of change in depressive symptoms over time did not differ between groups, F(2, 67) = 1.3, p = .29 (Figure 4). However, we found a significant difference between groups at the postpartum time point in depressive symptoms, F(2, 67) = 5.3, p < .01. Participants who continued breastfeeding reported significantly fewer depressive symptoms than the other two groups (p ⩽ .04; Figure 5). In addition, groups differed in rates of clinically significant depressive symptoms (CES-D ⩾ 16) at postpartum, χ2(2) = 9.3, p < .01, with a rate of 55.6% (5/9) among participants who never initiated, 41.7% (10/24) among participants with early cessation, and 13.5% (5/37) among participants who continued.
Figure 4.
Depressive symptoms (per scores on the CES-D; M ± SE) by breastfeeding group across pregnancy and postpartum. *ps ⩽ .04.
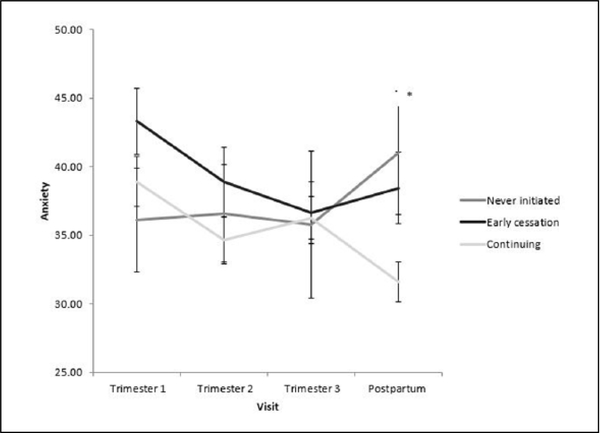
Figure 5.
Anxiety (per scores on the STAI; M ± SE) by breastfeeding group across pregnancy and postpartum. *ps ⩽ .04.
In relation to anxiety (per STAI), groups differed in their trajectory of change over time, F(2, 67) = 3.2, p = .05. Specifically, participants with early cessation exhibited steeper drops in anxiety across the course of pregnancy than did the other two groups, an effect driven by higher initial anxiety in the first trimester. In addition, we found a significant difference among groups in anxiety at the postpartum time point, F(2, 67) = 4.2, p = .02. At postpartum, both participants who never initiated (p < .01) and those with early cessation (p = .04) had significantly higher anxiety than those who continued to breastfeed (Figure 5).
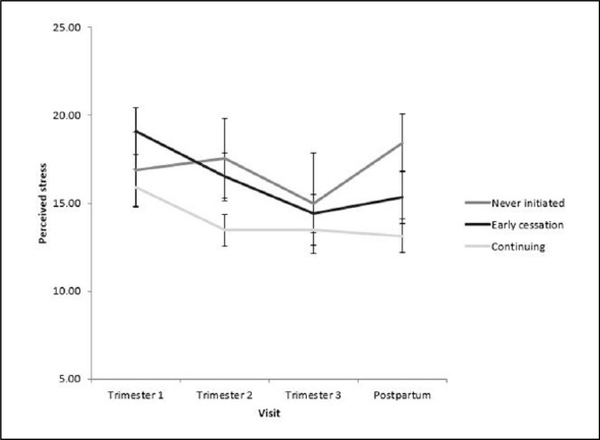
Perceived stress (per PSS), showed a quadratic pattern of change across time, F(1, 67) = 4.3, p = .04, but no significant differences were observed between groups, F(2, 67) = 2.4, p = .10, or over time by group, F(2, 67) = 1.5, p = .22 (Figure 6).
Figure 6.
Perceived stress (per scores on the PSS; M ± SE) by breastfeeding group across pregnancy and postpartum.
Discussion
We examined maternal beliefs about breastfeeding as well as prenatal and postpartum psychological distress in relation to breastfeeding initiation and early cessation. Our findings support the importance of fostering positive beliefs about breastfeeding to improve breastfeeding initiation and duration rates. In addition, our results highlight a distinctive relationship between pregnancy-specific distress and breastfeeding behaviors. We discuss how this unique relationship could manifest through impacts on women’s self-efficacy and confidence about breastfeeding leading to lower breastfeeding initiation rates and shorter duration. Finally, we examine how our longitudinal findings support and expand the extensive literature on the relationships between postpartum anxiety, depressive symptoms, and breastfeeding behaviors.
The association we identified between more positive breastfeeding beliefs (per total score and each subscale score) and breastfeeding initiation/longer duration mirror prior findings in the literature suggesting the importance of positive beliefs about breastfeeding in improving breastfeeding rates (Brockway et al., 2017; Brown, 2014). While breastfeeding educational campaigns have done much to create more positive breastfeeding beliefs, we still lack a complete understanding of how cultural factors influence breastfeeding beliefs (Kamoun & Spatz, 2018; Lutenbacher, Karp, & Moore, 2016; Savage, Neshteruk, Balantekin, & Birch, 2016). Connecting cultural expectations to breastfeeding beliefs will help educators and clinicians understand how to emphasize the positive aspects of breastfeeding without undermining cultural traditions in diverse populations.
The three groups (never initiated, early cessation, continuing) differ significantly in how pregnancy-specific distress changed over the course of pregnancy and postpartum. Pregnant women frequently have pregnancy-related concerns (e.g., fear of pain during labor and delivery, poor fetal health, and relationship changes) resulting in pregnancy-specific distress (Cole-Lewis et al., 2014; Dunkel Schetter, 2011; Guardino & Dunkel Schetter, 2014). Anxiety over these concerns often peak in early pregnancy as many women are encountering pregnancy-related concerns for the first time (Coussons-Read et al., 2012). Guardino and Dunkel Schetter (2014) argue that pregnancy-specific distress is a distinct construct from other forms of perceived distress and is highly correlated with birth outcomes (Alderdice, Lynn, & Lobel, 2012; Dunkel Schetter, 2011; Guardino & Dunkel Schetter, 2014). We support this concept by demonstrating the unique association between pregnancy-specific distress in early pregnancy with later breastfeeding practices. We did not observe a similar relationship for general perceived stress, state anxiety, or depressive symptoms during pregnancy (described below). In addition, while we cannot determine causality in the current study, addressing stressors with interventions early in pregnancy may help women gain self-efficacy to ultimately encourage continued breastfeeding practices. Our findings may be particularly relevant for first-time mothers, as they are overrepresented among the participants who never initiate breastfeeding or discontinue early in our sample and in the U.S. population as a whole (CDC, 2015).
Participants who never initiated and those with early cessation experienced more postpartum depressive symptoms and anxiety than those who continued breastfeeding. While we again cannot determine causal direction in the current study, other researchers have demonstrated bidirectional relationships between breastfeeding and postpartum depressive symptoms and anxiety (Ahn & Corwin, 2015; Chong et al., 2016; Wouk, Stuebe, & Meltzer-Brody, 2017), suggesting that the presence of depressive symptoms and anxiety may impede breastfeeding. Conversely, breastfeeding may improve maternal mood and reduce maternal anxiety through a suppression of the hypothalamic pituitary adrenal axis response (Ahn & Corwin, 2015; Chong et al., 2016; Wouk et al., 2017). With these data, we have provided evidence that the existence of depressive symptoms and anxiety prior to delivery may not be predictive of subsequent breastfeeding behavior.
National breastfeeding campaigns, initiatives, and health care provider training have affected breastfeeding initiation rates to a greater extent than breastfeeding duration (Balogun et al., 2016; Lumbiganon et al., 2016). Thus, understanding predictors of early cessation is of clinical importance. In our sample, most of the participants initiated breastfeeding, but discontinued prior to 8 weeks. Almost all of the participants showed a high interest in breastfeeding prior to giving birth, however. While directing resources toward increasing breastfeeding intentions is important, providing greater support to those with the intention to breastfeed is also necessary to increase duration. Examining longitudinal data from different types of distress across pregnancy in relation to breastfeeding practices may help in the development of early interventions to support women in their breastfeeding practices (Zhu et al., 2013). Intervention studies, though, are needed to determine if addressing psychosocial factors (e.g., pregnancy-specific distress) prior to delivery benefits breastfeeding behaviors.
Limitations
We recruited participants from a single geographic location. Our results, therefore, are not representative of the national population. Related to this, our sample size was relatively small, and as this was a secondary analysis, we were not able to perform an a priori power analysis. Finally, our observational study design does not permit determination of the causal versus correlational nature of observed associations.
Conclusion
In sum, we demonstrated that pregnancy-specific distress in early pregnancy was associated with early cessation of breastfeeding. In addition, beliefs about breastfeeding prior to delivery affected subsequent breastfeeding practices. Our study has relevance for identifying women who may particularly benefit from additional support and resources and addressing specific barriers to initiation and continuation. Interventions incorporating measures of pregnancy-specific distress in addition to breastfeeding beliefs may improve breastfeeding outcomes.
Key Messages.
In this longitudinal study, we examined beliefs about breastfeeding and prenatal and postpartum psychological distress in relation to breastfeeding initiation and early cessation.
Pregnancy-specific distress in early pregnancy was associated with early cessation of breastfeeding.
At postpartum, women with continued breastfeeding for ⩾8 weeks reported less general anxiety and fewer depressive symptoms compared to those who never initiated or had early cessation.
Our study underscores the importance of addressing prenatal as well as postpartum psychological distress in the implementation of breastfeeding practice interventions.
Acknowledgments
We appreciate the contributions of our clinical research assistants and students to data collection. We also thank the staff and study participants at the Ohio State University Wexner Medical Center Prenatal Clinic.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (HD067670, LMC) and the National Institute of Nursing Research (R01NR013661, LMC). The project described was supported by Grant UL1TR001070 from the National Center for Advancing Translational Sciences. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Advancing Translational Sciences or the National Institutes of Health. Funding sources had no involvement in the study design, collection, analysis, or interpretation of data, writing of the manuscript, nor the decision to submit the article for publication.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Ahn S, & Corwin EJ (2015). The association between breastfeeding, the stress response, inflammation, and postpartum depression during the postpartum period: Prospective cohort study. International Journal of Nursing Studies, 52(10), 1582–1590. doi: 10.1016/j.ijnurstu.2015.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alderdice F, Lynn F, & Lobel M (2012). A review and psychometric evaluation of pregnancy-specific stress measures. Journal of Psychosomatic Obstetrics and Gynecology, 33(2), 62–77. doi: 10.3109/0167482x.2012.673040 [DOI] [PubMed] [Google Scholar]
- Balogun OO, O’Sullivan EJ, McFadden A, Ota E, Gavine A, Garner CD, . . . MacGillivray S (2016). Interventions for promoting the initiation of breastfeeding. Cochrane Database of Systematic Reviews, 11. doi: 10.1002/14651858.CD001688.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartick MC, Jegier BJ, Green BD, Schwarz EB, Reinhold AG, & Stuebe AM (2017). Disparities in breastfeeding: Impact on maternal and child health outcomes and costs. Journal of Pediatrics, 181, 49–61. doi: 10.1016/j.jpeds.2016.10.028 [DOI] [PubMed] [Google Scholar]
- Brockway M, Benzies K, & Hayden KA (2017). Interventions to improve breastfeeding self-efficacy and resultant breastfeeding rates: A systematic review and meta-analysis. Journal of Human Lactation, 33(3), 486–499. doi: 10.1177/0890334417707957 [DOI] [PubMed] [Google Scholar]
- Brown A (2014). Maternal trait personality and breastfeeding duration: The importance of confidence and social support. Journal of Advanced Nursing, 70(3), 587–598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2015). Rates of any and exclusive breastfeeding by sociodemographics among children born in 2012 National Immunization Survey data. Retrieved from the Centers for Disease Control and Prevention; website: http://www.cdc.gov/breastfeeding/data/nis_data/rates-any-exclusive-bf-socio-dem-2012.htm [Google Scholar]
- Centers for Disease Control and Prevention. (2016). Breastfeeding report card: Progressing toward national breastfeeding goals. Retrieved from the Centers for Disease Control and Prevention; website: https://www.cdc.gov/breastfeeding/pdf/2016breastfeedingreportcard.pdf [Google Scholar]
- Centers for Disease Control and Prevention. (2017). Breastfeeding among US children born 2002–2014, CDC National Immunization Survey. Retrieved from the Centers for Disease Control and Prevention; website: https://www.cdc.gov/breastfeeding/data/nis_data/ [Google Scholar]
- Chaudron LH, Klein MH, Remington P, Palta M, Allen C, & Essex MJ (2001). Predictors, prodromes, and incidence of postpartum depression. Journal of Psychosomatic Obstetrics and Gynaecology, 22(2), 103–112. [DOI] [PubMed] [Google Scholar]
- Chong A, Biehle SN, Kooiman LY, & Mickelson KD (2016). Postnatal depression: The role of breastfeeding efficacy, breastfeeding duration, and family-work conflict. Psychology of Women Quarterly, 40(4), 518–531. doi: 10.1177/0361684316658263 [DOI] [Google Scholar]
- Cohen S, Kamarck T, & Mermelstein R (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24, 385–396. [PubMed] [Google Scholar]
- Cole-Lewis HJ, Kershaw TS, Earnshaw VA, Yonkers KA, Lin HQ, & Ickovics JR (2014). Pregnancy-specific stress, preterm birth, and gestational age among high-risk young women. Health Psychology, 33(9), 1033–1045. doi: 10.1037/a0034586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coussons-Read ME, Lobel M, Carey JC, Kreither MO, D’Anna K, Argys L, . . . Cole S (2012). The occurrence of preterm delivery is linked to pregnancy-specific distress and elevated inflammatory markers across gestation. Brain Behavior and Immunity, 26(4), 650–659. doi: 10.1016/j.bbi.2012.02.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dias CC, & Figueiredo B (2015). Breastfeeding and depression: A systematic review of the literature. Journal of Affective Disorders, 171, 142–154. [DOI] [PubMed] [Google Scholar]
- Dozier AM, Nelson A, & Brownell E (2012). The relationship between life stress and breastfeeding outcomes among low-income mothers. Advances in Preventative Medicine, 2012, 902487. doi: 10.1155/2012/902487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunkel Schetter C (2011). Psychological science on pregnancy: Stress processes, biopsychosocial models, and emerging research issues. Annual Review of Psychology, 62, 531–558. [DOI] [PubMed] [Google Scholar]
- Fallon V, Bennett KM, & Harrold JA (2016). Prenatal anxiety and infant feeding outcomes: A systematic review. Journal of Human Lactation, 32(1), 53–66. doi: 10.1177/0890334415604129 [DOI] [PubMed] [Google Scholar]
- Gerd AT, Bergman S, Dahlgren J, Roswall J, & Alm B (2012). Factors associated with discontinuation of breastfeeding before 1 month of age. Acta Paediatric, 101(1), 55–60. [DOI] [PubMed] [Google Scholar]
- Guardino CM, & Dunkel Schetter C (2014). Understanding pregnancy anxiety: Concepts, correlates, and consequences. Zero to Three, 34(4), 12–21. [Google Scholar]
- Hinic K (2016). Predictors of breastfeeding confidence in the early postpartum period. Journal of Obstetrics, Gynecology, and Neonatal Nursing, 45(5), 649–660. doi: 10.1016/j.jogn.2016.04.010 [DOI] [PubMed] [Google Scholar]
- IBM Corporation. (2013). IBM SPSS statistics for Windows (Version 22.0). Armonk, NY: Author. [Google Scholar]
- Kamoun C, & Spatz D (2018). Influence of Islamic traditions on breastfeeding beliefs and practices among African American Muslims in West Philadelphia: A mixed-methods study. Journal of Human Lactation, 34, 164–175. doi: 10.1177/0890334417705856 [DOI] [PubMed] [Google Scholar]
- Kitsantas P, Gaffney KF, & Kornides ML (2012). Prepregnancy body mass index, socioeconomic status, race/ethnicity and breastfeeding practices. Journal of Perinatal Medicine, 40(1), 77–83. doi: 10.1515/JPM.2011.106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lobel M (1996). The Revised Prenatal Distress Questionnaire (NUPDQ). Stony Brook: State University of New York. [Google Scholar]
- Lumbiganon P, Martis R, Laopaiboon M, Festin MR, Ho JJ, & Hakimi M (2016). Antenatal breastfeeding education for increasing breastfeeding duration. Cochrane Database of Systematic Reviews, 12. doi: 10.1002/14651858.CD006425.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lutenbacher M, Karp SM, & Moore ER (2016). Reflections of black women who choose to breastfeed: Influences, challenges, and supports. Maternal and Child Health Journal, 20, 231–239. [DOI] [PubMed] [Google Scholar]
- Marteau TM, & Bekker H (1992). The development of a six-item short-form of the state scale of the Spielberger State-Trait Anxiety Inventory (STAI). British Journal of Clinical Psychology, 31(3), 301–306. [DOI] [PubMed] [Google Scholar]
- Meades R, & Ayers S (2011). Anxiety measures validated in perinatal populations: A systematic review. Journal of Affective Disorders, 133, 1–15. [DOI] [PubMed] [Google Scholar]
- Mehta UJ, Siega-Riz AM, Herring AH, Adair LS, & Bentley ME (2012). Pregravid body mass index, psychological factors, and breastfeeding duration: Is there a link? Maternal and Child Nutrition, 8(4), 423–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitra AK, Khoury AJ, Hinton AW, & Carothers C (2004). Predictors of breastfeeding intention among low-income women. Maternal and Child Health Journal, 8(2), 65–70. [DOI] [PubMed] [Google Scholar]
- Pippins JR, Brawarsky P, Jackson RA, Fuentes-Afflick E, & Haas JS (2006). Association of breastfeeding with maternal depressive symptoms. Journal of Women’s Health, 15(6), 754–762. [DOI] [PubMed] [Google Scholar]
- Radloff LS (1977). The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401. [Google Scholar]
- Savage JS, Neshteruk CD, Balantekin KN, & Birch LL (2016). Low-income women’s feeding practices and perceptions of dietary guidance: A qualitative study. Maternal and Child Health Journal, 20, 2510–2517. [DOI] [PubMed] [Google Scholar]
- Spielberger CD (1983). State-Trait Anxiety Inventory for Adults: Manual, instrument and scoring guide. Menlo Park, CA: Consulting Psychologists Press. [Google Scholar]
- Taveras EM, Capra AM, Braveman PA, Jensvold NG, Escobar GJ, & Lieu TA (2003). Clinician support and psychosocial risk factors associated with breastfeeding discontinuation. Pediatrics, 112(1), 108–115. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. (2017). QuickFacts: United States; Columbus city, Ohio: Retrieved from the U.S. Census Bureau; website: https://www.census.gov/quickfacts/fact/table/US,columbuscityohio/PST045216 [Google Scholar]
- Veenstra G (2005). Social status and health: Absolute deprivation or relative comparison, or both? Health Sociology Review, 14(2), 121–134. [Google Scholar]
- Victora CG, Bahl R, Barros AJD, Franҫa GVA, Horton S, Krasevec J, . . . Rollins NC (2016). Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. Lancet, 387(10017), 475–490. [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2016, January). Infant and young child feeding. Fact Sheet No. 342. Retrieved from the World Health Organization; website: http://www.who.int/mediacentre/factsheets/fs342/en/ [Google Scholar]
- Wouk K, Stuebe AM, & Meltzer-Brody S (2017). Postpartum mental health and breastfeeding practices: An analysis using the 2010–2011 pregnancy risk assessment monitoring system. Maternal and Child Health Journal, 21(3), 636–647. doi: 10.1007/s10995-016-2150-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu P, Hao J, Jiang X, Huang K, & Tao F (2013). New insight into onset of lactation: Mediating the negative effect of multiple perinatal biopsychosocial stress on breastfeeding duration. Breastfeeding Medicine, 8(2), 151–158. doi: 10.1089/bfm.2012.0010 [DOI] [PMC free article] [PubMed] [Google Scholar]