Abstract
Background and Objectives:
The general surgery residency at the University of Illinois College of Medicine at Peoria has a long tradition of integrating robotic surgery into training since 2002. The purpose of this paper is to investigate our curriculum and evaluation system, which was designed to achieve a standardized format for education in general robotic surgery.
Methods:
The curriculum consists of two phases: phase 1 (PGY 1–2): Complete 4 robotic surgery training modules; read two assigned robotic surgery articles; and practice simulation modules on the robot. phase 2 (PGY 3–5): Refresh training modules, score >90% on the simulator modules every 6 months; bedside assist minimum of 4 robotic procedures; and act as console surgeon for a minimum of 10 procedures with 2 separate attending surgeons. The required simulator modules were specially selected to incorporate all of the skills categories documented in the simulator. The faculty evaluate the resident's operative performance using the Global Evaluative Assessment of Robotic Skills validated rubric.
Results:
Since the curriculum was instituted in June 2017, 73 evaluations from 8 surgeons have been collected. We examined data from 6 residents who had at least 5 Global Evaluative Assessment of Robotic Skills assessments completed. Correlation coefficient scores showed a positive correlation ranging from 0.476 to 0.862 for average skills and 0.334 to 0.866 for overall performance scores.
Discussion:
The preliminary results suggest an improvement of resident robotic surgical skills through tailored education. This curriculum is designed to enhance robotic general surgery education that could potentially produce general surgeons able to operate robotically without needing a robotic/MIS (Minimally Invasive Surgery) fellowship.
Keywords: Robotic surgery, Robotic surgical training, General surgery, Resident education, Curriculum
INTRODUCTION
The proliferation of robotic surgeries over the last decade has necessitated the development of training curricula to prepare residents for the 21st-century operating room. This need is perhaps most acutely felt in general surgery residency programs. While urology and gynecology led the robotics charge, utilization of the technology by the general surgery discipline evolved more slowly. However, general surgery has been the fastest growing user of the da Vinci Surgical System (Intuitive Surgical, Sunnyvale, California, USA) every year since 2012. In 2018, for the first time ever, there were more general surgery robotic procedures performed in the United States than any other specialty, representing a 32% increase in volume from 2017.1 While it is vital that academic medical centers keep pace with this rapidly developing technology, there currently exists no validated curriculum for robotic surgery education in general surgery residency programs.
Inconsistent approaches to robotic training across general surgery residency programs reveal the disparity between the use of robotic technology and the training for it. One survey from 2013 revealed that 60% of residents received no training or education before participating in their first robotic case.2 A more recent survey of general surgery residency program administrators showed that 92% of programs have residents participate in robotic cases, yet only 67% have instituted a formal robotic training curriculum. Of those with a curriculum, fewer than half track their residents' involvement with robotic cases.3
Of course, simply having a robotic training curriculum is no guarantee of learner proficiency and competency. Green, Chern, and O'Sullivan4 examined the robotic surgery curricula of 12 residency programs and found that participation in robotic procedures is often limited to an observational role. They warn that surgical trainees may not receive the necessary skills and knowledge to operate safely. Most recently, an article was published from Zhao et al5 confirming our assumptions and reasoning behind our format. Residents and attending surgeons alike believed that early robotic exposure is beneficial, should not be limited to bedside assisting for too long, dual consoles are greatly helpful, and simulations should be utilized.5 The above concerns and statements compelled our program to create a comprehensive and formalized robotic curriculum for general surgery residents to achieve certification through the progression of skill acquisition.
MATERIALS AND METHODS
This program was developed using the experience afforded the authors' academic medical center as an early adopter of robotic technology, which began training surgical residents in 2003 on foregut and colon procedures.6 Over the ensuing years, the program evolved along with the technology, aided in particular by the acquisition of the telestrator in 2009 and the dual surgeon's console in 2012.7 Yet, the need persisted for a more structured training program that could track participant performance over time, leading to the establishment of a formal curriculum in June 2017. Studying the residents' progress through this new curriculum has been approved and monitored by an Institutional Review Board.
The curriculum is divided into two phases based on stepwise progression. Phase 1 occurs during PGY 1–2 and is mandatory for all general surgery residents. Phase 2 occurs during the PGY 3–5 years.
Phase 1
Read two assigned articles: da Vinci Skills Simulator for Assessing Learning Curve and Criterion-Based Training of Robotic Basic Skills8 and Fundamental Skills of Robotic Surgery: A Multi-Institutional Randomized Controlled Trial for Validation of a Simulation-Based Curriculum.9 The first article, in summary, showed that robotic skills can be learned fairly quickly but trainees could not reach the designated “expert” level of a 90% score on the simulations within 10 attempts. The second article showed that urology participants who performed a Fundamentals of Robotic Surgery (FRS) curriculum were faster, more precise, had better camera control, better use of the fourth arm, and lost instruments less often than participants who did not complete the curriculum. Furthermore, that trial showed that participants in the controlled arm improved significantly when put through the FRS curriculum and tested again.
Complete the da Vinci Xi Online training modules for Vessel Sealer, Stapler, Single-Site, and assessment for robotic coordinators.
Attend a dry lab with an Intuitive representative. This is a training session where the group of junior residents meets with one of the Intuitive representatives in the operating suite and go over the intricacies of the robotic tower, the console, robotic arms, the history of the technology, and hands-on practicing with props in the room.
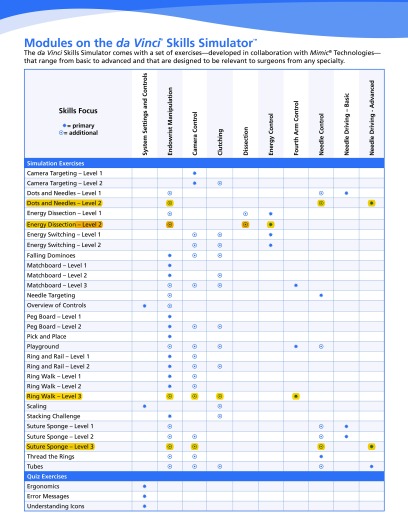
Practice the assigned da Vinci skills simulations: Energy Dissection level 2, Ring Walk level 3, and Suture Sponge level 3. These 3 modules were selected because they best capture the range of technical skills most fundamental to robotic surgery (Figure 1). Three simulators (2 in the operating suites on the actual robot and 1 Robotic Surgery Simulator (RoSS) in our simulation center) are available to our residents around the clock, allowing for flexibility to train as it best suits their schedules.
Figure 1.
The various simulations that one can complete and the respective skills each simulation exercises. For the curriculum, Energy Dissection level 2, Ring Walk level 3, and Suture sponge level 3 were chosen. Thus, all skills were included and evaluated.
Additionally, residents are encouraged to review da Vinci clinical videos online. These tutorials teach residents how to use and operate different components of the robotic system (such as basic setup, docking, and sterility). There are also videos that delineate how to approach robotic operative procedures to give learners exposure before they are scrubbed in on those particular cases. After completing phase 1 and with the consent from the Director of Robotics and the General Surgery Residency Program Director general surgery residents may elect to proceed to phase 2, where they gain hands-on clinical experience.
Phase 2
Residents first bedside assist on a minimum of four cases. This can actually be carried over from when the resident was a PGY-1 or −2. This allows trainees to learn the patient-side demands of robotic cases, such as patient positioning, port placement, and docking, instrument exchanges, as well as gaining an appreciation for the mechanics and physical restrictions of the robotic arms. The residents should bedside assist with at least two different faculty surgeons. Doing so will provide the trainees with feedback and constructive criticism from distinct perspectives.
Before being allowed to perform their first case, residents must retake the same 3 da Vinci Skills Simulator exercises that they did in phase 1 with a minimum score of 90. They must also complete these exercises every 6 months and show documented proof of their scores to the faculty surgeon. This provision helps counter skill decay as residents go through rotations where they may not have had the opportunity to use robotic technology.10,11 Since da Vinci Skills Simulator performance has been shown to be positively associated with intra-operative robotic performance, this refresher training is vital to maintaining skills and protecting patient safety.12
Residents operate from the surgeon's console for at least 10 procedures under the supervision of at least 2 different attending surgeons. Residents begin their console training in a limited role by performing the simplest operative tasks, increasing the level of complexity and involvement over time as abilities develop.
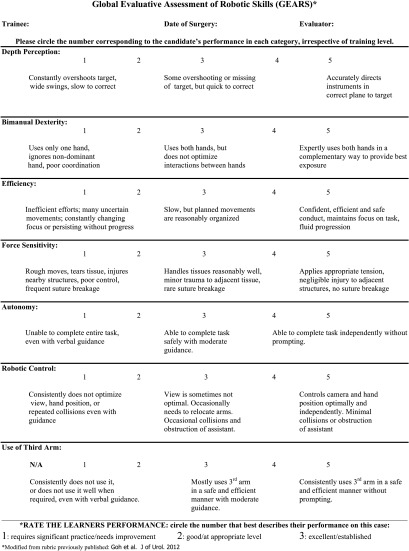
For every resident-led robotic operation, an attending surgeon will evaluate the performance using the Global Evaluative Assessment of Robotic Skills (GEARS) rubric (Figure 2). The GEARS assessment is available for faculty members to complete electronically, including on their mobile devices. The results of previous GEARS scores are available to all of the Faculty surgeons, so they are able to personalize their areas of critique during the operation. Nearing the end of residency, the participant's information is gathered and can be used for a Certificate of Completion showing their progress throughout residency. Only those residents who finish phase 2 will be eligible for a Certificate of Completion upon graduation.
Figure 2.
Global Evaluative Assessment of Robotic Skills validated rubric, created in 2012 by Aghazadeh et al.12
RESULTS
Since instituting this new curriculum in 2017, 18 residents have progressed to phase 2 and 1 Certificate of Completion has been awarded. More residents were eligible for this certificate, but only one has utilized it to get accelerated robotic privileges at their hospital thus far. Altogether, faculty surgeons have completed 101 GEARS assessments. For the purposes of this study, only the trainees who have 5 or more GEARS assessments completed to date are considered. There are 6 residents who fit these criteria for a total of 73 cases.
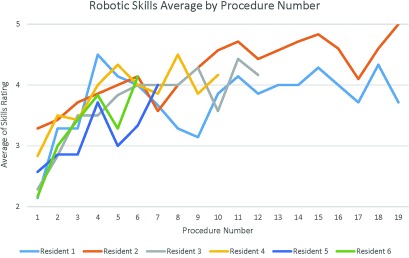
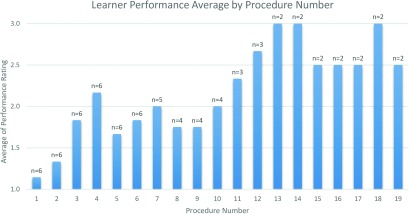
Overall, the results indicate an improvement of the residents' robotic abilities over time. When examining the average rating of the 7 skill categories measured by GEARS, there is a positive correlation between performance and experience for all residents (Figure 3). The overall performance score exhibits a positive association with the number of procedures performed (Figure 4). Table 1 lists the correlation coefficients for each of these measures.
Figure 3.
Graph showing improvement of residents' average skills rating over the time span of cases completed during phase 2.
Figure 4.
Graph showing improvement in the residents' Global Evaluative Assessment of Robotic Skills overall performance score over the time span of the cases completed in phase 2.
Table 1.
Correlation Coefficients for Average Skills Score and Overall Performance Scores
| Resident | Number of Gears Assessments | Average Skills Correlation Coefficient | Overall Performance Correlation Coefficient |
|---|---|---|---|
| 1 | 19 | 0.476 | 0.334 |
| 2 | 19 | 0.849 | 0.866 |
| 3 | 12 | 0.813 | 0.759 |
| 4 | 10 | 0.719 | 0.696 |
| 5 | 7 | 0.806 | 0.474 |
| 6 | 6 | 0.862 | 0.488 |
Residents 2–6 show a strong positive linear relationship on the average of their robotic skills assessments (>0.7). Resident 1 showed a weaker correlation (0.476). However, by examining their assessments on procedures 1–10 and 10–19 separately, the standard deviation decreased from 0.660 to 0.215, which demonstrates increased consistency with training. While GEARS uses a 1–5-point scale to rate robotic skills, the overall performance measure is measured on a scale of 1–3. Three residents showed a strong correlation between their overall performance and number of procedures and 3 showed a low correlation. While all correlation coefficients are positive and some show a strong linear relationship, given the small sample size of this study more data is needed to conclude that the residents' performance improvement is the result of the curriculum.
The skill that saw the largest improvement over time was depth perception, with an average increase of 2 points from the residents' first attempt to their last one. Their worst performance overall was in using the third arm, most likely due to it not being utilized for every procedure (use of the third arm occurred in 70% of cases).
DISCUSSION
Robotic surgery has quickly become a mainstay of US operating rooms and its application to general surgery appears to only be expanding. Academic institutions have the responsibility to establish a curriculum to educate upcoming residents to meet these dynamic surgical needs. A mixed-method curriculum using didactic lessons, simulation training, hands-on practice, and mentorship, designed as a stepwise progression with clear benchmarks, provides the training necessary to prepare residents to become robotic surgeons. Our hope is not that this will become a nationally standardized curriculum, but that programs that do not have an established curriculum can either adopt this curriculum or use it as a guide to create their own.
Residents face many demands during training and hour restrictions frequently can be an issue. The Accreditation Council for Graduate Medical Education (ACGME) duty hour restrictions underscore the need to maximize resident working hours by providing a quality learning environment that cultivates and optimizes their clinical abilities. Fortunately, it has been demonstrated that training general surgery residents in robotics does not amount to extra time in the operating room compared to standard laparoscopic procedures.13 In one program, 92% of general surgery residents reported that their robotics curriculum did not unduly stress their time or distract them from other duties.14 Moreover, most general surgery residents want to receive formal robotics training.2
Having a methodical, stepwise robotics curriculum is a responsible and efficient method of incorporating this critical training into residents' busy schedules. Residents who are not planning on pursuing robotic surgery careers are not required to proceed to phase 2 of the curriculum. However, exposing them to the fundamentals of robotic surgery during phase 1 helps ensure patient safety while observing robotic cases. Additionally, as robotic surgery becomes more ubiquitous and its clinical applications expand, the residents will carry with them a basic understanding of robotic equipment and skills.
One goal of this curriculum is for the Certificate of Completion, awarded to residents who complete the training, to be considered for hospital credentialing. Currently, as there is no national certification authority, requirements vary widely across hospitals for surgeons to gain robotic surgery privileges. Using the GEARS assessment to demonstrate crucial skill acquisition over time offers evidence of performance improvement using a validated assessment tool. This feature of the curriculum could be most meaningful to credentialing boards when granting robotic privileges. As most general surgery programs do not believe a fellowship in robotic surgery is necessary to gain the knowledge and skills to practice independently, providing residents with a standardized robotic training program that tracks progress is reasonable.15 Since there is no single operation that encompasses all the skills necessary to perform robotic general surgeries, Certificates of Completion are awarded at the discretion of faculty leaders. The Program Director, the Chair of Department of Surgery, and the Chair of Robotic General Surgery, all of whom reside at two large academic medical centers, assess demonstrated competency on the various procedures residents perform throughout their residency.
There are several limitations to this study. Since the curriculum was established in the summer of 2017, the sample size is limited. While the initial findings are promising, a larger data set is needed to substantiate these preliminary results. Currently this program does not record the resident's degree of participation at the console, just that >50% constitutes being “resident led.” This metric might be useful in determining rate of skill acquisition and can easily be added to the GEARS assessment. Further, this project did not look at operative times and complication rates in procedures over the span of an individual resident's training. Another limitation is that this robotic curriculum does not presently evaluate nontechnical skills (NTSs) such as communication, situational awareness, teamwork, leadership, and risk management. The high rate of adverse events caused by actions outside of the surgeon's console is becoming better understood.16–18 Integrating NTS assessment into the curriculum could help prepare the next generation of surgeons to confront the unique challenges of the robotic operating theatre. We initially incorporated the National Aeronautics and Space Administration Task Load Index to capture NTS metrics but due to low compliance, we were not able to show any correlating data. Perhaps better compliance rates could be achieved by adding relevant NTS categories onto the GEARS survey.
In terms of scalability, while our residents only use the da Vinci surgical system, the curriculum could be adjusted to include other surgical technologies provided that a simulation-based training module is available. The structured education methodology of this curriculum is the platform that produces the reproducible results rather than the brand of robotic system used through deliberate practice and just-in-time feedback.
For institutions that have limited resources, being able to purchase simulators and/or a dual console for enhanced proctoring can present a challenge. Our own experience has shown that this technology is not required to teach robotic surgery but it does greatly facilitate skill acquisition, real-time feedback, and learner participation in procedures. It can be understandably difficult for an attending surgeon to hand over the robotic console until he or she gains a certain level of trust with a particular resident. For institutions without a dual console system, having residents demonstrate their skills on a simulator can help attending surgeons feel more comfortable letting the learner take control of the console for portions of a procedure. Another option for limited resource residency programs is to partner with larger academic hospitals that share a collaborative patient base to enhance training in the region. We currently offer on-site and in situ robotic training programs for our region.
CONCLUSION
The need for robotic training in general surgery residency programs has grown in tandem with technological innovation. An effective curriculum will incorporate didactic elements, simulation training and practice, and expert mentorship in a systematic and stepwise process. Evaluating the residents' robotic skills in the operating room environment using this curriculum will not only track their caseload but also their progress. This provides a benchmark for faculty members to certify residents as capable of performing robot-assisted surgery safely and independently. This curriculum could be adopted or modified by programs across the country that are looking for a guide, and we encourage other programs to make adjustments as they feel necessary to further the progress of robotic surgery education nationwide.
Acknowledgments
We would like to thank our surgeons who help train residents in robotic operations: Dr. Richard Anderson, MD; Dr. J. Stephen Marshall, MD; Dr. Chadrick Evans, MD; Dr. Robin Alley, MD; Dr. Justin Fischer, MD; and Dr. Steven Tsoraides, MD. We also want to thank Professor Yolanda Rush for providing feedback on statistical methodology.
Contributor Information
Harley Moit, Department of Surgery, University of Illinois College of Medicine Peoria, Peoria, Illinois, USA..
Anthony Dwyer, Department of Surgery, University of Illinois College of Medicine Peoria, Peoria, Illinois, USA.; Graduate Medical Education, University of Illinois College of Medicine Peoria, Peoria, Illinois, USA.
Michelle De Sutter, Graduate Medical Education, University of Illinois College of Medicine Peoria, Peoria, Illinois, USA..
Sally Heinzel, Graduate Medical Education, University of Illinois College of Medicine Peoria, Peoria, Illinois, USA..
David Crawford, Department of Surgery, University of Illinois College of Medicine Peoria, Peoria, Illinois, USA..
References:
- 1. Intuitive Surgical, Inc. Annual report. Available from: http://www.annualreports.com/Company/intuitive-surgical-inc. Accessed June 7, 2019.
- 2. Farivar BS, Flannagan M, Leitman IM. General surgery residents' perception of robot-assisted procedures during surgical training. J Surg Educ. 2015;72:235–242. [DOI] [PubMed] [Google Scholar]
- 3. Tom CM, Maciel JD, Korn A, et al. A survey of robotic surgery training curricula in general surgery residency programs: how close are we to a standardized curriculum? Am J Surg. 2019;217:256–260. [DOI] [PubMed] [Google Scholar]
- 4. Green CA, Chern H, O'Sullivan PS. Current robotic curricula for surgery residents: a need for additional cognitive and psychomotor focus. Am J Surg. 2018;215:277–281. [DOI] [PubMed] [Google Scholar]
- 5. Zhao B, Lam J, Hollandsworth HM, et al. General surgery training in the era of robotic surgery: a qualitative analysis of perceptions from resident and attending surgeons. Surg Endosc. 2019; 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Huettner F, Dynda D, Ryan M, Doubet J, Crawford DL. Robotic-assisted minimally invasive surgery; a useful tool in resident training—the Peoria Experience, 2002–2009. Int J Med Robotics Comput Assist Surg. 2010;6:386–393. [DOI] [PubMed] [Google Scholar]
- 7. Crawford DL, Dwyer AM. Evolution and literature review of robotic general surgery resident training 2002–2018. Updates Surg. 2018;70:363–368. [DOI] [PubMed] [Google Scholar]
- 8. Brinkman WM, Luursema JM, Kengen B, et al. da Vinci skills simulator for assessing learning curve and criterion-based training of robotic basic skills. Urology. 2013;81:562–566. [DOI] [PubMed] [Google Scholar]
- 9. Stegemann AP, Ahmed K, Syed JR, et al. Fundamental skills of robotic surgery: a multi-institutional randomized controlled trial for validation of a simulation-based curriculum. Urology. 2013;81:767–774. [DOI] [PubMed] [Google Scholar]
- 10. Jenison EL, Gil KM, Lendvay TS, Guy MS. Robotic surgical skills: acquisition, maintenance, and degradation. JSLS. 2012;16:218–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Guseila LM, Saranathan A, Jenison EL, Gil KM, Elias JJ. Using virtual reality to maintain surgical skills during periods of robotic surgery inactivity. J Robot Surg. 2014;8:261–268. [DOI] [PubMed] [Google Scholar]
- 12. Aghazadeh MA, Mercado MA, Pan MM, Miles BJ, Goh AC. Performance of robotic simulated skills tasks is positively associated with clinical robotic surgical performance. BJU Int. 2016;118:475–481. [DOI] [PubMed] [Google Scholar]
- 13. Honaker MD, Paton BL, Stefanidis D, Schiffern L. Can robotic surgery be done efficiently while training residents? J Surg Educ. 2015;72:377–380. [DOI] [PubMed] [Google Scholar]
- 14. Krause W, Bird J. Training robotic community surgeons: our experience implementing a robotics curriculum at a rural community general surgery training program. J Robot Surg. 2019;13:385–389. [DOI] [PubMed] [Google Scholar]
- 15. George LC, O'Neill R, Merchant AM. Residency training in robotic general surgery: a survey of program directors. Minim Invasive Surg. 2018;2018:8464298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Vetter MH, Green I, Martino M, Fowler J, Salani R. Incorporating resident/fellow training into a robotic surgery program. J Surg Oncol. 2015;112:684–689. [DOI] [PubMed] [Google Scholar]
- 17. Sridhar AN, Briggs TP, Kelly JD, Nathan S. Training in robotic surgery—An overview. Curr Urol Rep. 2017;18:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ahmed K, Khan R, Mottrie A, et al. Development of a standardised training curriculum for robotic surgery: a consensus statement from an international multidisciplinary group of experts. BJU Int. 2015;116:93–101. [DOI] [PubMed] [Google Scholar]