Abstract
Objective
To determine whether women overactive bladder symptoms would report more frequent unhealthy toileting behaviors.
Methods:
A community-based sample of adult women were electronically recruited to complete the Toileting Behavior Scale and the International Consultation on Incontinence Questionnaire – Overactive Bladder module, as well as clinical and demographic questionnaires. The associations between overactive bladder and toileting behavior subscales were assessed as continuous variables using Spearman’s rank correlation and as dichotomous variables with multivariable logistic regression.
Results:
Of the 6,562 adult women included in the analytic sample, 1,059 (16.1%) were classified as having overactive bladder. Of the toileting behavior subscales, convenience voiding had the highest, positive association with overactive bladder score (r = 0.301, p < 0.0001). On multivariable logistic regression, women with OAB were more likely to report behaviors of convenience voiding (OR 1.13, CI 1.11-1.15), delayed voiding (OR 1.05, CI 1.02-1.08), straining to void (OR 1.05, CI 1.03-1.07), and position preference (OR 1.13, CI 1.08-1.18).
Conclusions:
OAB symptoms were associated with specific toileting behaviors of convenience voiding, delayed voiding, straining to void, and position preference. Further investigation is needed to determine if toileting behaviors are a risk factor for OAB or a compensatory adaptation to mitigate symptoms.
Keywords: lower urinary tract symptoms, overactive bladder, urinary incontinence, risk factors, women, bladder health
Introduction
Overactive bladder (OAB) is characterized by the symptom of urinary urgency, with or without urgency urinary incontinence, usually with frequency and nocturia, and is estimated to affect approximately 16.9% of adult women1-3. These symptoms can severely impact quality of life, making it important to identify modifiable risk factors4.
The underlying pathophysiology of OAB is complex and is thought to involve several proposed neuroanatomic and myogenic hypotheses5-7. Nevertheless, the impact that toileting behavior has on bladder function is commonly recognized and serves as the underpinning for why behavioral therapy is recommended in the management of lower urinary tract disorders, including OAB8. The American Urological Association’s OAB Guideline highlights the role of patient education regarding normal and abnormal bladder function and focuses on behavioral interventions for initial management.
While behavioral interventions for the symptomatic management of OAB are well supported in literature, the associations between women’s toileting behaviors and OAB are still being explored8. On the one hand, behavioral therapy, including strategies to decrease urgency, as well as biofeedback-assisted pelvic floor muscle identification and strengthening, can decrease urge incontinent episodes in women9. On the other hand, unhealthy bladder behaviors may contribute to bladder dysfunction, such as hovering over the toilet seat, which may prevent relaxation of the pelvic floor and increase urinary retention10. Is there a relationship between toileting behaviors and bladder symptoms? Prior studies have suggested that women who work at an academic medical center with urinary urgency were more likely to report unhealthy behaviors including straining and waiting too long to void11,12. However, there is a lack of population-based data regarding toileting behaviors in adult women. The aim of the present study was to investigate the associations between toileting behaviors and OAB symptoms in a large, community-based sample of women.
Materials and Methods
This is a secondary analysis of a prior, IRB-approved, cross-sectional questionnaire study, in which women aged 18 years or older were recruited by a single email advertisement between October - December 2017 from two study recruitment resources at our institution13. ResearchMatch is a national registry of volunteers created by several academic institutions and supported by the U.S. National Institutes of Health as part of the Clinical Translational Science Award program. ResearchMatch has 87,574 women who have consented to be contacted by researchers about health studies for which they may be eligible. The Research Notifications Distribution List is a recruitment tool available to our institution’s researchers consisting of approximately 18,500 regional volunteers and institutional staff with an unknown gender makeup. Women were incentivized to participate by entering two random drawings for Apple iPads.
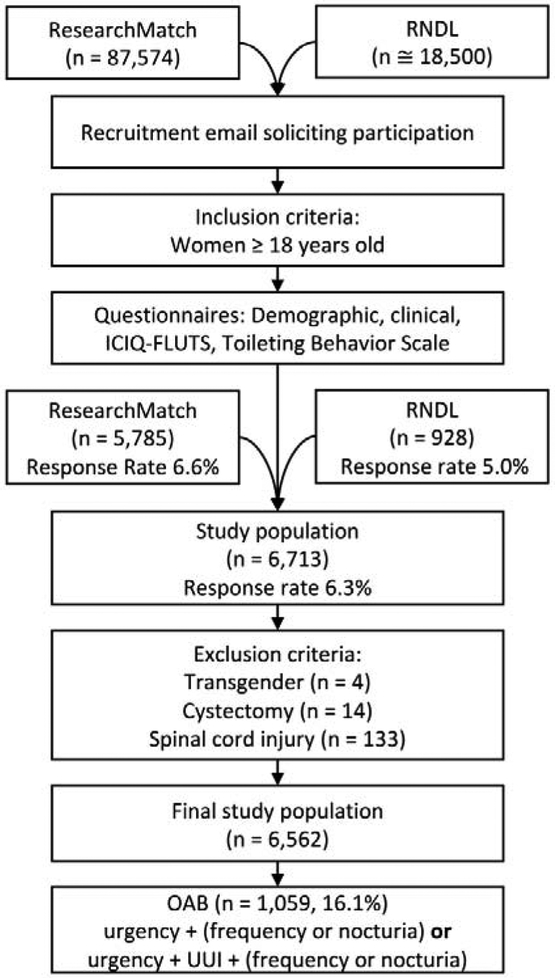
Study inclusion criteria were: 1) women age 18 or older, 2) ability to read English, and 3) ability to access the internet. Transgender women, individuals with a history of cystectomy, and those with a spinal cord injury were excluded from the final study population. Of the approximately 106,074 potential participants, 6,713 women responded to the invitation and completed the questionnaires, resulting in a response rate of 6.3%. After exclusion of women who were transgender (n = 4, < 0.1%), had a cystectomy (n = 14, 0.2%), or spinal cord injury, (n = 133, 2.0%), the final study sample included 6,562 women (Figure 1).
Figure 1.
Construction of study population. (RNDL, Research Notifications Distribution List; ICIQ-FLUTS, International Consultation on Incontinence Questionnaire- Female Lower Urinary Tract Symptoms; OAB, Overactive Bladder; UUI, Urgency Urinary Incontinence)
Following consent to participate, women completed anonymous validated questionnaires soliciting information on demographic and clinical data, and on toileting behaviors and LUTS. The Toileting Behavior Women’s Elimination Behavior Scale is a validated questionnaire that consists of 18 questions with five Likert scale responses: never (1), rarely (2), sometimes (3), often (4), and always (5)14. Behaviors were divided into 5 subscales: place preference (4 items, range 4-20), convenience voiding (5 items, range 5-25), delayed voiding (3 items, range 3-15), straining to void (4 items, range 4-20), and position preference (2 items, range 2-10), with higher scores representing more abnormal behavior. Place preference describes women’s actions regarding voiding at home or away. Convenience voiding is emptying the bladder in the absence of desire and delayed voiding is waiting to void despite an urge to do so. Straining to void describes the use of abdominal musculature to void. Voiding position refers to the posture used away from home, whether sitting, hovering over, or crouching on a toilet.
The International Consultation on Incontinence Questionnaire – Female Lower Urinary Tract Symptoms (ICIQ-FLUTS) is a validated instrument consisting of 12 questions, each with five responses scored from 0-4 with higher scores indicating more frequent occurrence of the symptom15. Within the ICIQ-FLUTS, an ICIQ-OAB score (range from 0-16) can be determined based on urgency, frequency, nocturia, and urgency urinary incontinence. Using a previously published algorithm for OAB consistent with the International Continence Society definition, OAB was defined as the presence of urgency at least sometimes (response of sometimes, often, or always), with or without urgency urinary incontinence, in combination with frequency and/or nocturia1.
The primary outcome measure was OAB while the primary exposure was toileting behavior. Continuous variables were reported as means with standard deviations. Spearman’s rank correlation coefficient was calculated for ICIQ-OAB scores and each toileting behavior subscale. To further investigate the relationship between OAB and convenience voiding, responses to each question were compared between those with and without OAB by Wilcoxon rank-sum test. Univariable and multivariable logistic regression analyses were performed to assess associations of toileting behaviors and covariates with OAB. Covariates were selected a priori from existing literature and included age, body mass index (BMI), diabetes, parity, mobility impairment, race, and education. Twenty-five women (0.4%) were excluded for one or more missing independent variables leaving 6,537 women for multivariable analysis. Statistical significance was set at a p value < 0.05. STATA® version 15 was used for all statistical analyses.
Results
Of the 6,562 subjects, 1,059 (16.1%) were classified as having OAB. These women were older (47.6 ± 15.1 vs. 40.1 ± 14.8) while the control group was more likely to be white (80.8% vs 74.4%) and college educated (74.1% vs 56.7%). Women with OAB had a higher rate of obesity, diabetes, and mobility impairments. They also had higher mean scores for each toileting behavior subscale (Table 1).
Table 1.
Demographic and clinical characteristics of women with and without overactive bladder
| Demographic | Control (n = 5,503) |
Overactive Bladder (n = 1,059) |
|---|---|---|
| Mean Age ± SD (Range 18-89) | 40.1 ± 14.8 | 47.6 ± 15.1 |
| Race/Ethnicity (%) | ||
| White | 4,446 (80.8%) | 788 (74.4%) |
| Black | 400 (7.3%) | 129 (12.2%) |
| Hispanic | 240 (4.4%) | 49 (4.6%) |
| Asian | 234 (4.3%) | 20 (1.9%) |
| Other/unknown | 183 (3.3%) | 73 (6.9%) |
| No. Highest Education (%) | ||
| High school graduate or less | 206 (3.7%) | 79 (7.5%) |
| Some college or associates degree | 1,219 (22.2%) | 380 (35.9%) |
| College graduate | 2,104 (38.2%) | 309 (29.2%) |
| Graduate or professional degree | 1,974 (35.9%) | 291 (27.5%) |
| Clinical | ||
| Mean ICIQ-OAB Score ± SD (Range 0-16) | 2.6 ± 1.8 | 7.2 ± 2.1 |
| Mean BMI ± SD (Range 14.5-94.2) | 27.2 ± 7.1 | 30.8 ± 9.0 |
| No. Obstetric History (%) | ||
| Nulliparous | 2,782 (50.6%) | 352 (32.2%) |
| One | 749 (13.6%) | 138 (13.0%) |
| Two | 894 (16.2%) | 226 (21.3%) |
| ≥ Three | 1,078 (19.6%) | 343 (32.4%) |
| No. Diagnosed with Diabetes (%) | 265 (4.8%) | 125 (11.8%) |
| No. with Mobility Impairment† (%) | 129 (2.3%) | 91 (8.6%) |
| Toileting behavior subscale scores | ||
| Mean place preference ± SD (Range 4-20) | 13.6 ± 3.4 | 14.5 ± 3.3 |
| Mean convenience voiding ± SD (Range 5-25) | 8.7 ± 3.5 | 11.0 ± 4.5 |
| Mean delayed voiding ± SD (Range 3-15) | 8.3 ± 2.6 | 8.8 ± 3.0 |
| Mean straining to void ± SD (Range 4-20) | 7.6 ± 3.7 | 8.8 ± 4.4 |
| Mean position preference ± SD (Range 2-10) | 3.9 ± 1.5 | 4.2 ± 1.8 |
Mobility impairment is requirement of cane, walker or wheelchair. (ICIQ-OAB, International Consultation on Incontinence Questionnaire- Overactive Bladder; BMI, Body Mass Index; SD, Standard Deviation)
All toileting behavior subscales had a statistically significant, positive Spearman’s correlation coefficient with increasing ICIQ-OAB scores, of which convenience voiding (r = 0.301, p < 0.0001) demonstrated the strongest association (Figure 2). For each individual convenience voiding question (i.e. voiding without desire at home, away from home, at someone else’s home, in public places, and “just in case”), there was a statistically significant increase in mean scores in those with OAB (Supplementary Table 1).
Figure 2.
Scatter plot and Spearman’s correlation of toileting behavior subscales with ICIQ-OAB score. (r = Spearman’s rank correlation coefficient; ICIQ-OAB, International Consultation on Incontinence Questionnaire- Overactive Bladder)
After adjusting for age, BMI, diabetes, parity, mobility impairment, race and education in a multivariable model, the behaviors of convenience voiding (OR 1.13, CI 1.11-1.15), delayed voiding (OR 1.05, CI 1.02-1.08), straining to void (OR 1.05, CI 1.03-1.07), and position preference (OR 1.13, CI 1.08-1.18), remained positively associated with OAB (Table 2). Place preference, i.e. preferring to void at home, was no longer statistically significant (OR 0.99, CI 0.96-1.01). Age, BMI, diabetes, and mobility impairment maintained a statistically significant association with OAB while parity no longer was significantly associated (OR 1.07, CI 1.00-1.14). Advanced education such as a graduate or professional degree had an inverse association with OAB (OR 0.47, CI 0.34-0.65).
Table 2.
Univariable and multivariable logistic regression analysis of variables associated with overactive bladder
| Toileting Behavior | Univariable OR (95% CI) |
Multivariable OR (95% CI) |
|---|---|---|
| Place preference | 1.08 (1.06-1.10) | 0.99 (0.96-1.01) |
| Convenience voiding | 1.16 (1.14-1.17) | 1.13 (1.11-1.15) |
| Delayed voiding | 1.07 (1.04-1.09) | 1.05 (1.02-1.08) |
| Straining to void | 1.08 (1.06-1.10) | 1.05 (1.03-1.07) |
| Position preference | 1.13 (1.09-1.18) | 1.13 (1.08-1.18) |
| Covariates | ||
| Age | 1.03 (1.03-1.04) | 1.03 (1.02-1.03) |
| BMI | 1.05 (1.05-1.06) | 1.04 (1.03-1.05) |
| Diabetes | 2.65 (2.11-3.31) | 1.41 (1.09-1.82) |
| Parity | 1.36 (1.29-1.44) | 1.07 (1.00-1.14) |
| Mobility impairment† | 3.92 (2.97-5.17) | 1.97 (1.44-2.70) |
| Race | ||
| White | Ref | Ref |
| Black | 1.82 (1.47-2.25) | 1.27 (0.99-1.62) |
| Asian | 0.48 (0.30-0.77) | 0.88 (0.54-1.45) |
| Hispanic | 1.15 (0.84-1.58) | 1.13 (0.79-1.61) |
| Other/unknown | 2.25 (1.70-2.98) | 1.58 (1.16-2.17) |
| Education | ||
| High school graduate or less | Ref | Ref |
| Some college or associates degree | 0.81 (0.61-1.08) | 0.83 (0.61-1.13) |
| College graduate | 0.38 (0.29-0.51) | 0.52 (0.38-0.72) |
| Graduate or professional degree | 0.38 (0.29-0.51) | 0.47 (0.34-0.65) |
Mobility impairment is requirement of cane, walker or wheelchair. Statistically significant values bolded. (OR, Odds Ratio; CI, Confidence Interval; Ref, Reference Category)
Discussion
In this large sample of women, convenience voiding, delayed voiding, straining to void, and position preference were found to have a significant positive association with OAB after adjusting for demographic and clinical comorbidities. Convenience voiding had the strongest correlation with ICIQ-OAB scores. Given the frequency of these behaviors within the population and their relation to OAB there may be substantial opportunity for behavior-based interventions.
While there is limited investigation into voiding behaviors and their consequences in adults, work in the pediatric population has demonstrated links between children’s voiding behavior and outcomes such as increased urinary tract infections and LUTS16,17. Of the few adult studies, one investigation of 209 adult patients treated in a urogynecology clinic demonstrated differences in toileting behaviors between women with and without urinary incontinence18. Women with urinary incontinence were more likely to strain, wait too long to urinate, void in the absence of an urge, and adopt alternative voiding positions. Sjogren and colleagues found most toileting behaviors, except position preference, positively correlated with LUTS in 173 young Swedish women aged 18-2519. Wan and associates found convenience voiding, delayed voiding, and straining to void scores positively associated with overall ICIQ-FLUTS score in 636 nurses in China20. A more recent study of 182 female medical center employees found only the specific behaviors of waiting too long to urinate at work and wearing panty liners for urinary leakage associated with urgency12. The present study documents similar findings, that toileting behaviors are related to lower urinary tract symptoms, in a large community-based sample of women. Across a broad range of ages, these findings suggest that toileting behaviors of convenience voiding, delayed voiding, straining to void, and position preference are related to symptoms of OAB.
The behavior of convenience voiding, with the strongest association among the behavior subscales, merits more investigation for its role in OAB. There are two plausible hypotheses for this finding. First, by routinely voiding in the absence of desire the individual sensitizes their bladder to smaller volumes, potentially increasing their OAB symptoms21. Alternatively, convenience voiding may be a compensatory behavior seeking to prevent urgency or urgency incontinence episodes14. These two concepts may together create a self-reinforcing spiral into worsening OAB symptoms. A separate study utilizing the Toileting Behavior Scale found 46.5% of women engaged in convenience voiding at home compared to 9.3% in a public place, perhaps supporting the idea that convenience voiding may originate from a desire to control where they void19. Straining to void was also associated with OAB symptoms in this cohort of women and may be a sign of underlying pathology, such as underactive bladder, or an adaptive measure to achieve bladder emptying faster.
Place preference was not statistically significant when adjusted for other covariates, likely due to the finding that nearly all women (98.8%) indicated at least some preference for home toilets. This highlights a pervasive negative view of public toilets that may influence other toileting behaviors as compensatory adaptations. For example, away from home women more frequently adopted alternative voiding positions, specifically hovering and squatting, that minimize contact with the toilet seat. This study was conducted in the United States where sitting to void is the most common position preference. Use of a squatting position may be more common in other populations in facilities designed for that position of voiding. Studies on the effect of voiding position indicate that hovering prevents complete bladder emptying due to incomplete pelvic floor relaxation10. Armed with more knowledge on the perception of public toilets it is possible that educational interventions, perhaps against myths (e.g. catching disease from a toilet seat), or targeted public health measures towards better sanitation or privacy may be able to reduce unhealthy toileting behaviors.
Bladder training, as a behavioral first-line therapy according to the American Urological Association OAB Guideline, may break this cycle through strategies such as timed voiding8. Regardless, this behavior encroaches upon every aspect of women’s lives as women with OAB were more likely to void without desire at home, where presumably access to a toilet is readily available, and in public places, where one may not be. Exactly how convenience voiding, as well as delayed voiding, straining to void, and position preference are related to OAB remains to be determined. Understanding how these behaviors affect the urothelium, detrusor activity, or bladder innervation may be important as all are postulated to be involved in the pathophysiology of OAB7.
The strengths of this work include its large, national sample of adult women and use of validated questionnaires. However, there are several limitations to these findings. First, this population consists of volunteers on research registries who are more highly educated and less diverse than the general population, thus the results may not be generalizable to the general population. Additionally, a low nominal response rate of 6.3% may have resulted in nonresponse bias. The exact response rate was unable to be determined due to an unknown gender make-up of the Research Notifications Distribution List; therefore, the rate was conservatively estimated at the lowest extreme. However, recent epidemiologic research suggests response rate is a poor proxy for study validity22. Fosnacht and colleagues found email administrations of a nationally used survey of university students to be reliable at a 5% response rate when they comprised a high number of responders23. This suggests that the strength in absolute number of respondents, rather than rate, makes these estimates more reliable. Any study using volunteer participation can have a selection bias, but while women with bladder symptoms may have been more likely to respond to this survey, the OAB prevalence was similar to previous studies1,2. Due to the large number of participants in this study statistically significant values need to be interpreted within a clinical context. It is possible that the smaller odds ratios, although statistically significant, reflect the heterogeneity of the underlying disease mechanisms involved in OAB and the variable role that toileting behaviors play in the natural history of OAB.
This study shows an association between toileting behaviors and OAB in a large community-based sample of women. As behavioral therapies are considered first-line management by the American Urological Association this suggests there may be an opportunity for instituting these low-cost, low-risk management options8. However, the conclusion that toileting behaviors are a risk factor for the development of OAB cannot be drawn from this cross-sectional study. Future work should focus on whether a causal relationship exists as it may be easier to prevent the development of unhealthy toileting behaviors with early education and behavioral changes rather than attempting to intervene after a diagnosis of OAB. In addition to the behaviors of convenience voiding, delayed voiding, straining to void, and position preference, several demographic variables and comorbid conditions were associated with OAB. OAB continues to be a complex syndrome with no clear driving etiology, but this study supports a hypothesis that behavioral factors, such as toileting habits, play a role.
Conclusion:
In conclusion, this work demonstrated an association of toileting behaviors with OAB symptoms. Further study is needed to investigate if these behaviors may be a risk factor for OAB or are a compensatory adaptation to mitigate symptoms. The wide prevalence of certain toileting behaviors in women and the mounting association with outcomes such as OAB suggests a need to further understand why women adopt these behaviors and what can be done to support healthy voiding habits.
Supplementary Material
Acknowledgments
Funding:
This work was supported by the Office of Medical Student Research at Vanderbilt University School of Medicine, the Vanderbilt Institute for Clinical and Translational Research by CTSA award number UL1 TR002243 from the National Center for Advancing Translational Sciences, and the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health under award number 1K23DK103910-01A1.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Temml C, Heidler S, Ponholzer A, Madersbacher S. Prevalence of the overactive bladder syndrome by applying the International Continence Society definition. Eur Urol. 2005;48(4):622–627. doi: 10.1016/j.eururo.2005.04.026. [DOI] [PubMed] [Google Scholar]
- 2.Stewart WF, Van Rooyen JB, Cundiff GW, et al. Prevalence and burden of overactive bladder in the United States. World J Urol. 2003;20(6):327–336. doi: 10.1007/s00345-002-0301-4. [DOI] [PubMed] [Google Scholar]
- 3.Abrams P, Cardozo L, Fall M, et al. The standardisation of terminology in lower urinary tract function: Report from the standardisation sub-committee of the International Continence Society. Urology. 2003;61(1):37–49. doi: 10.1016/S0090-4295(02)02243-4. [DOI] [PubMed] [Google Scholar]
- 4.Bartoli S, Aguzzi G, Tarricone R. Impact on Quality of Life of Urinary Incontinence and Overactive Bladder: A Systematic Literature Review. Urology. 2010;75(3):491–500. doi: 10.1016/j.urology.2009.07.1325. [DOI] [PubMed] [Google Scholar]
- 5.Banakhar MA, Al-Shaiji TF, Hassouna MM. Pathophysiology of overactive bladder. Int Urogynecol J. 2012;23(8):975–982. doi: 10.1007/s00192-012-1682-6. [DOI] [PubMed] [Google Scholar]
- 6.Chu FM, Dmochowski R. Pathophysiology of Overactive Bladder. Am J Med. 2006;119(3):3–8. doi: 10.1016/j.amjmed.2005.12.010. [DOI] [PubMed] [Google Scholar]
- 7.Roosen A, Chapple CR, Dmochowski RR, et al. A Refocus on the Bladder as the Originator of Storage Lower Urinary Tract Symptoms: A Systematic Review of the Latest Literature. Eur Urol. 2009;56(5):810–820. doi: 10.1016/j.eururo.2009.07.044. [DOI] [PubMed] [Google Scholar]
- 8.Gormley EA, Lightner DJ, Burgio L, et al. Diagnosis and treatment of overactive bladder (non-neurogenic) in adults: AUA/SUFU guideline. J Urol. 2014; 188(6):1–57. doi: 10.1016/j.juro.2012.09.079. [DOI] [PubMed] [Google Scholar]
- 9.Burgio KL, Locher JL, Goode PS, et al. Behavioral vs Drug Treatment for Urge Urinary Incontinence in Older Women. JAMA. 1998;280(23):1995. doi: 10.1001/jama.280.23.1995. [DOI] [PubMed] [Google Scholar]
- 10.Moore KH, Richmond DH, Sutherst JR, Imrie AH, Hutton JL. Crouching over the toilet seat: prevalence among British gynaecological outpatients and its effect upon micturition. BJOGAn Int J Obstet Gynaecol. 1991;98(6):569–572. doi: 10.1111/j.1471-0528.1991.tb10372.x. [DOI] [PubMed] [Google Scholar]
- 11.Zhou F, Newman DK, Palmer MH. Urinary Urgency in Working Women: What Factors Are Associated with Urinary Urgency Progression? J Women’s Heal. 2018;27(5):575–583. doi: 10.1089/jwh.2017.6555. [DOI] [PubMed] [Google Scholar]
- 12.Palmer MH, Willis-Gray MG, Zhou F, Newman DK, Wu JM. Self-reported toileting behaviors in employed women: Are they associated with lower urinary tract symptoms? Neurourology and Urodynamics. February 1, 2017:735–743. [DOI] [PubMed] [Google Scholar]
- 13.Kowalik CG, Daily A, Delpe S, et al. Toileting behaviors of adult women: What is healthy? J Urol. August 2018. doi: 10.1016/j.juro.2018.07.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang K, Palmer MH. Development and validation of an instrument to assess women’s toileting behavior related to urinary elimination: Preliminary results. Nurs Res. 2011;60(3): 158–164. doi: 10.1097/NNR.0b013e3182159cc7. [DOI] [PubMed] [Google Scholar]
- 15.Brookes ST, Donovan JL, Wright M, Jackson S, Abrams P. A scored form of the Bristol Female Lower Urinary Tract Symptoms questionnaire: Data from a randomized controlled trial of surgery for women with stress incontinence. Am J Obstet Gynecol. 2004;191(1):73–82. doi: 10.1016/j.ajog.2003.12.027. [DOI] [PubMed] [Google Scholar]
- 16.Snodgrass W Relationship of voiding dysfunction to urinary tract infection and vesicoureteral reflux in children. Urology. 1991;38(4):341–344. doi: 10.1016/0090-4295(91)80148-Z. [DOI] [PubMed] [Google Scholar]
- 17.Bower WF, Yip SK, Yeung CK, Nguyen D. Dysfunctional elimination symptoms in childhood and adulthood In: Journal of Urology. Vol 174 Elsevier; 2005:1623–1628. doi: 10.1097/01.ju.0000176599.91836.12. [DOI] [PubMed] [Google Scholar]
- 18.Willis-Gray MG, Wu JM, Sripad A, Newman D, Palmer MH. Toileting behaviors in women presenting to a urogynecology clinic. Urol Nurs. 2017;37(5):251–255. doi: 10.7257/1053-816X.2017.37.5.251. [DOI] [Google Scholar]
- 19.Sjögren J, Malmberg L, Stenzelius K. Toileting behavior and urinary tract symptoms among younger women. Int Urogynecol J. 2017;28(11):1677–1684. doi: 10.1007/s00192-017-3319-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wan X, Wu C, Xu D, Huang L, Wang K. Toileting behaviours and lower urinary tract symptoms among female nurses: A cross-sectional questionnaire survey. Int J Nurs Stud. 2017;65:1–7. doi: 10.1016/j.ijnurstu.2016.10.005. [DOI] [PubMed] [Google Scholar]
- 21.Reynolds WS, Dmochowski R, Wein A, Bruehl S. Does central sensitization help explain idiopathic overactive bladder? Nat Rev Urol. 2016;13(8):481–491. doi: 10.1038/nrurol.2016.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Morton SMB, Bandara DK, Robinson EM, Atatoa Carr PE. In the 21st Century, what is an acceptable response rate? Aust N Z J Public Health. 2012;36(2):106–108. doi: 10.1111/j.1753-6405.2012.00854.x. [DOI] [PubMed] [Google Scholar]
- 23.Fosnacht K, Sarraf S, Howe E, Peck LK. How Important are High Response Rates for College Surveys? Rev High Educ. 2017;40(2):245–265. doi: 10.1353/rhe.2017.0003. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.