Abstract
Objectives
To examine trends in smoking prevalence in key venues (workplaces, restaurants, bars) and in public support for comprehensive smoke-free laws, with comparisons between cities and rural areas in China.
Design
Data are from Waves 3–5 (2009–2015) of the International Tobacco Control (ITC) China Survey, a cohort survey of smokers and non-smokers. Logistic regression analyses employing generalised estimating equations assessed changes in smoking prevalence and support for smoke-free laws over time; specific tests assessed whether partial smoking bans implemented in three cities between Waves 3 and 4 had greater impact.
Setting
Face-to-face surveys were conducted in seven cities (Beijing, Changsha, Guangzhou, Kunming, Shanghai, Shenyang and Yinchuan) and five rural areas (Changzhi, Huzhou, Tongren, Yichun and Xining).
Participants
In each survey location at each wave, a representative sample of approximately 800 smokers and 200 non-smokers (aged 18+) were selected using a multistage cluster sampling design.
Main outcome measures
Prevalence of smoking (whether respondents noticed smoking inside restaurants, bars and workplaces); smoking rules inside these venues; and support for complete smoking bans in these venues.
Results
Although smoking prevalence decreased and support increased over time, neither trend was greater in cities that implemented partial smoke-free laws. Smoking was higher in rural than urban workplaces (62% vs 44%, p<0.01), but was equally high in all restaurants and bars. There were generally no differences in secondhand smoke (SHS) exposure between smokers and non-smokers except in rural workplaces (74% vs 58%, p<0.05). Support for comprehensive bans was equally high across locations.
Conclusions
Partial laws have had no effect on reducing SHS in China. There is an urgent need for comprehensive smoke-free laws to protect the public from exposure to deadly tobacco smoke in both urban and rural areas. The high support among Chinese smokers for such a law demonstrates that public support is not a barrier for action.
Keywords: public health, smoking, secondhand smoke, tobacco control, policy evaluation
Strengths and limitations of this study.
This is the first cohort study to estimate overall levels of smoking in public places and support for smoking bans in both cities and rural areas of China.
This study is not a national sample, but in each sampling location—seven major cities and five rural areas—there is a probability sampling design that led to fully representative samples of smokers and non-smokers in each location, including all of Beijing, Shanghai, Guangzhou and in each of the rural areas.
Analyses accounted for the complex sampling design through the use of analytical survey weights to represent the population, rescaled to ensure comparability over time.
Quasi-experimental tests (difference-in-difference analysis) examined differences between cities that implemented partial bans between survey waves and those where no new laws were implemented.
While the study relied on self-report measures, the results are unlikely to be explained by any possible reporting biases as we used consistent methods and measures at each time point to evaluate differences over time.
Introduction
As the world’s most populous country, China suffers the world’s greatest devastation from cigarette smoking and the world’s greatest toll from secondhand smoke (SHS).1 Approximately 100 000 non-smokers die every year from SHS exposure in China, with a disproportionate burden on women—whose smoking rate is low, but who experience the highest rate of SHS exposure in the world.2 3 Comprehensive smoke-free policies (ie, all indoor public places are 100% smoke free) that are well-enforced, as called for by the WHO Framework Convention on Tobacco Control (WHO FCTC), have been shown to reduce tobacco consumption and increase smoking cessation.4 5 China became a Party to the WHO FCTC in 2005, yet progress towards achieving universal protection from SHS exposure in public places has been slow and there is still no national smoke-free legislation. Regulations on smoking in public places have only been implemented at the city level, and up until 2015, none of these local laws were comprehensive, and many lacked strong enforcement.1 6 For example, some types of public venues have not been covered by smoking bans, or if they are, the law includes allowances for designated smoking areas (ie, partial bans). As a result, smoking and SHS exposure in public places has remained alarmingly high throughout China, and the number of deaths from tobacco will continue to rise substantially in the absence of strong measures to reduce SHS.7
Although studies have shown the weak impact of existing partial smoke-free laws across China and the need for stronger comprehensive laws,8–11 very little is known about the impact of current smoke-free policies in rural areas—where almost half (44%) of the Chinese population lives.12 Rural smoking rates have risen in recent years such that by 2015, male smokers in rural areas had a higher smoking prevalence, smoked more cigarettes per day and spent more of their income on cigarettes than urban smokers.13 14 The ever-widening urban-rural health disparity in China also means that rural areas have fewer resources to tackle the tobacco epidemic and the increase in non-communicable diseases, further intensifying the public health threat in these areas.15–17 Given the variation in tobacco control policies across the country and the growing health threat in rural areas, it is important to examine the impact of smoke-free policies across a wider range of both urban and rural locations in China.
This study uses cohort data from three survey waves (2009–2015) of the International Tobacco Control (ITC) China Survey to examine trends in self-reported exposure to SHS in public venues and level of support for smoke-free policies in five major cities and five rural areas across China. Results for the most recent survey waves were also compared between cities and rural areas, and between smokers and non-smokers.
Methods
Data source and sampling design
Data are from the ITC China Survey, a face-to-face cohort survey of adult smokers and non-smokers (≥18 years). The Wave 3 (2009) and 4 (2011–2012) Surveys were conducted in seven cities: Beijing, Changsha, Guangzhou, Kunming, Shanghai, Shenyang and Yinchuan. At the Wave 5 Survey (November 2013 to July 2015), Changsha and Yinchuan were dropped and five rural areas were added (Changzhi, Huzhou, Tongren, Yichun and Xining). Five waves of the ITC China Survey have been conducted since 2006; however, the present article reports results from Waves 3–5 because a more comprehensive set of key measures for evaluation of smoke-free policies was introduced at Wave 3.
In each survey location at each wave, a representative sample of approximately 800 smokers and 200 non-smokers were selected using a multistage cluster sampling design, following the initial sampling design from Wave 1. As in other ITC Project surveys, respondents who were lost to follow-up in subsequent survey waves were replenished with randomly selected respondents from the population, with the replenishment sample size based on retention rates.18 In this paper, smokers are those who have smoked more than 100 cigarettes in their lifetime and smoked at least weekly at recruitment.
Technical details of the ITC China Surveys including information on the survey locations, sampling methods and survey design are provided by Wu et al 18 19 and the ITC China technical reports at http://www.itcproject.org/technical-report/?country=China 20–24
Measures
Because individual public places may implement rules on smoking that are more strict than the local level laws, the rules in each venue were assessed at Wave 5 by asking smokers and non-smokers who had visited a bar or restaurant in their city what the no-smoking rule was the last time they visited, and by asking those who work inside a building what the no-smoking rule is in their workplace.
The prevalence of smoking in public places was measured at each survey wave by asking all respondents whether they noticed people smoking inside restaurants, bars and workplaces. For workplaces, those who worked indoors were asked whether people smoked in their workplace in the last 6 months. For restaurants and bars, those who said they had visited a restaurant/bar in their city in the last 6 months were asked whether people were smoking inside at their last visit. At Waves 4 and 5, those who had said ‘smoking was not allowed in any indoor area’ or ‘no rules or restrictions’ about the restaurant/bar they last visited were routed to the question differently than those who had said ‘smoking was allowed only in designated areas’. Responses from the two pools of respondents to these questions were combined for the estimates of prevalence at Waves 4 and 5.
Support for smoke-free policies was evaluated with the question ‘For each of the following public places—bars, restaurants, and workplaces—please tell me if you think smoking should not be allowed in any indoor areas; should be allowed only in some indoor areas; no rules or restrictions, or don’t know?’ For each venue, those who said smoking should not be allowed in any indoor areas were categorised as supporting a complete smoking ban.
Data analysis
Overview
All analyses were conducted in SAS V.9.4. with SUDAAN V.11.0.1. Results were calculated using both unadjusted and covariate-adjusted models, controlling for the following variables: smoking status, sex, age group and time in sample (number of waves completed by each respondent) except where noted. Results were very similar in both models, so only the adjusted results are presented. For most variables, responses of ‘do not know’, ‘refused’ or ‘not applicable’ were treated as missing; except for measures of support, where ‘do not know’ responses were treated as valid and included in the denominator.
Longitudinal analyses
To test changes in the outcome variables between waves, separate logistic regression models (PROC MULTILOG) were estimated using generalised estimating equations (GEE)25 assuming exchangeable correlation structure. The stratified multistage sampling design with strata and primary sampling units were also taken into consideration. In the GEE model, the variances were computed between clusters, whereas the intraclass correlations were computed within the individual respondent since the same questions were asked at each survey wave. Respondents with missing data on the outcome variables were excluded from the GEE model. Analyses were first conducted separately for smokers and non-smokers, and all respondents were then combined to estimate overall population prevalences over time. For the longitudinal trends, results are shown for the combined sample unless otherwise noted. The longitudinal trends were also conducted among respondents in the cities only (ie, rural areas were excluded from the Wave 5 sample).
Tests of differences between groups
Within the longitudinal design, a specific quasi-experimental (difference-in-difference) analysis was conducted to examine whether those cities that had implemented partial smoke-free laws between survey waves experienced significantly greater benefits (lower smoking rates, greater support for smoke-free laws) than did those cities where no new (partial) laws were implemented over that same period of time.
Differences between cities and rural locations and between smokers and non-smokers were also calculated for the Wave 5 results using the predicted marginal standardisation method in the SUDAAN GEE model to estimate prevalences, and general linear contrasts of the predicted marginals were specified to test for significance.26
Survey weights
Finally, analytical survey weights were used to account for the complex sampling design for all the analyses (see ref 24 for further information on the weights construction for the ITC China Wave 5 Survey). For the Wave 5 cross-sectional analyses, the Wave 5 inflation weights were applied to represent the actual population across the survey locations at that time. For the longitudinal analyses, the inflation weights from the time of recruitment were applied for each respondent and rescaled by cohort to ensure comparability between and within cohorts, assuming that conditioning on cohort does not affect the model unbiasedness of the individual’s term in the GEE estimating function. As a result, the longitudinal results are comparable between waves, but the Wave 5 only results are not necessarily comparable to the longitudinal results.
Patient and public involvement
No patients were involved in deciding the research question, study design, outcome measures or in the interpretation of results. This work uses data provided by survey participants which were securely accessed and stored. There are no plans to disseminate results of the research to study participants.
Results
Reported rules about smoking in public places at Wave 5
Overall at Wave 5 (2013–2015), workplaces were the most likely venue to completely ban indoor smoking (67.2%) compared with restaurants (41.8%) and bars (25.7%) (see table 1). Comparisons between the cities and rural areas showed that cities were significantly more likely to have a complete ban in workplaces than rural areas (68.8% vs 49.6%, p<0.05). Rural restaurants were more likely to have no rules (38.3% vs 21.1%, p<0.05), but rural bars were less likely to have no rules (16.6% vs 37.2%, p<0.01).
Table 1.
Prevalence of rules about smoking in workplaces, restaurants and bars
| Workplaces | Restaurants | Bars | ||||||||||
| Overall % |
Cities % |
Rural % |
P value (cities vs rural) | Overall % |
Cities % |
Rural % |
P value (cities vs rural) | Overall % |
Cities % |
Rural % |
P value (cities vs rural) | |
| Total n size | 2169 | 1598 | 571 | 4471 | 3385 | 1086 | 671 | 509 | 162 | |||
| Smoking is not allowed in any indoor area | 67.2 | 68.8 | 49.6 | 0.016* | 41.8 | 41.9 | 35.8 | 0.374 | 25.7 | 25.8 | 17.0 | 0.333 |
| Smoking is allowed in designated indoor areas | 18.1 | 17.8 | 21.9 | 0.478 | 31.9 | 33.2 | 11.6 | <0.001*** | 33.6 | 32.5 | 57.6 | 0.082 |
| No rules or restrictions | 14.6 | 13.4 | 25.8 | 0.064 | 22.1 | 21.1 | 38.3 | 0.019* | 36.0 | 37.2 | 16.6 | 0.003** |
| Don’t know | 0.1 | 0.0 | 2.7 | <0.001*** | 4.3 | 3.8 | 14.3 | 0.171 | 4.8 | 4.5 | 8.8 | 0.559 |
Bold numbers represent a significant difference between the percentages for cities and rural areas. Results are among smokers and non-smokers combined.
*p<0.05; **p<0.01; ***p<0.001.
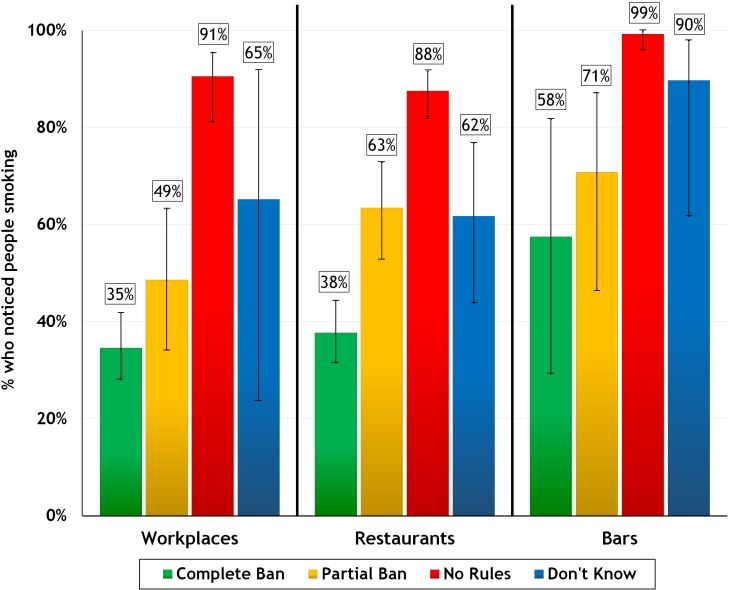
Association between rules about smoking and noticing smoking in public places
In all venues among those surveyed in 2013–2015, smoking was much more common in those places where there were no reported rules or restrictions (88%–99% across venues), compared with places that had a partial (49%–71%) or complete smoking ban (35%–58%) (see figure 1). However, even though smoking prevalence was lower in places that had a complete ban, the rates of smoking were still alarmingly high overall—especially in bars (58% in bars that reportedly did not allow smoking).
Figure 1.
Prevalence of smoking in public places with no rules, a partial smoking ban, or a complete ban across all survey locations at Wave 5 (2013–2015).
Prevalence of smoking in public places
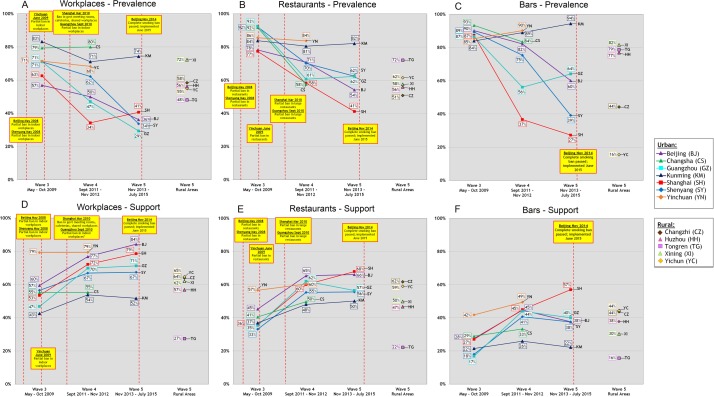
Longitudinal trends from Waves 3–5
Figure 2 shows the trends over Waves 3–5 (2009 to 2013–2015) in the adjusted prevalence of smoking in public places in each survey location, as reported by both smokers and non-smokers overall. As shown in figure 2A, the prevalence of smoking in workplaces in the last 6 months was high at Wave 3 (57%–83% across the five cities; 69% overall), but decreased over time (41% overall among cities at Wave 5). (The overall percentages for cities at Wave 5 in this section differ from the percentages presented in table 2 due to differences in the inflation weights that were used for longitudinal vs cross-sectional analyses (see the Methods section).)
Figure 2.
A- F Smoking prevalence and support for complete smoking bans in workplaces, restaurants and bars for each city and rural area over Waves 3–5 of the ITC China Survey, among the whole sample. ‘Large restaurants’ refers to those with 75+ seats or 150+ m2. The results for Wave 5 are separated by urban versus rural locations; however, all data for Wave 5 were collected over the same time period (2013–2015).
Table 2.
Difference between cities versus rural areas and smokers versus non-smokers in prevalence of smoking and support for smoking bans at Wave 5
| Cities | Rural | P value (cities vs rural) | |||||||
| Overall % (total n size) | Smokers % (total n size) |
Non-Smokers % (total n size) |
P value (smokers vs non-smokers) | Overall % (total n size) | Smokers % (total n size) |
Non-Smokers % (total n size) |
P value (smokers vs non-smokers) | ||
| Smoking in workplaces | 43.8 (1592) | 50.3 (1263) | 41.9 (329) | 0.104 | 61.8 (566) | 74.4 (457) | 57.6 (109) | 0.022* | 0.006** |
| Smoking in restaurants | 58.7 (3286) | 60.7 (2543) | 58.3 (743) | 0.578 | 56.1 (984) | 58.3 (788) | 55.5 (196) | 0.782 | 0.683 |
| Smoking in bars | 78.6 (497) | 83.2 (426) | 77.1 (71) | 0.552 | 67.9 (152) | 59.8 (134) | 76.3 (18) | 0.206 | 0.200 |
| Support for ban in workplaces | 73.2 (4470) | 63.2 (3423) | 75.4 (1047) | <0.001*** | 61.7 (4927) | 56.9 (3918) | 62.3 (1009) | 0.218 | 0.109 |
| Support for ban in restaurants | 61.1 (4469) | 54.2 (3424) | 62.6 (1045) | 0.032* | 55.8 (4924) | 49.5 (3915) | 57.4 (1009) | 0.059 | 0.445 |
| Support for ban in bars | 41.1 (4453) | 37.4 (3408) | 41.9 (1045) | 0.296 | 44.2 (4896) | 38.2 (3891) | 46.5 (1005) | 0.074 | 0.633 |
Bold numbers represent a significant difference between the percentages between groups (cities vs rural areas overall; and smokers vs non-smokers within cities or rural areas). Results were adjusted for gender, age group, smoking status and time in sample; however, time in sample was removed from the model for the noticing smoking in bars results due to its unexpected influence on the adjusted results.
*p<0.05; **p<0.01; ***p<0.001.
The quasi-experimental test of the impact of partial smoke-free laws showed a larger decrease in workplace smoking in the three cities that implemented a partial smoking ban between Waves 3 and 4 (Yinchuan, Shanghai and Guangzhou; average decrease of 25.1%) compared with the four cities that did not implement any laws between Waves 3 and 4 (Beijing, Changsha, Kunming and Shenyang; average decrease of 6.6%); however, the difference was not significant (p=0.06).
From Waves 3–5, the majority of respondents in almost all survey locations (cities and rural) who had visited a restaurant in the last 6 months reported that people were smoking inside the restaurant during their last visit—reflecting the fact that only 42% of these restaurants reportedly had a complete smoking ban (see table 1). The prevalence of smoking inside restaurants was highest at Wave 3 (77%–93% across the cities; 84% overall), but decreased over time in all cities (57% in cities at Wave 5) (see figure 2B). However, there was no significant difference (p=0.488) in the decrease in restaurant smoking in the three cities where partial laws were implemented between Waves 3 and 4 (average decrease of 21.3%) compared with the four cities where no new laws were implemented (16.0% decrease).
Smoking prevalence was highest overall in bars across the survey waves (84%–93% of cities at Wave 3; 86% overall) (see figure 2C). Results varied across survey locations at Wave 5 due to small sample sizes among non-smokers, but remained high overall (61% in cities), and actually increased over time in Kunming (94% at Wave 5). As there were no smoke-free laws covering bars implemented during the survey period, differences between cities were not analysed.
Cities versus rural areas at Wave 5
Table 2 compares overall smoking prevalence in the five cities and the five rural areas in 2013–2015. Smoking was significantly higher in workplaces in rural areas compared with cities (62% vs 44%, p<0.01), but there were no differences between cities and rural areas for restaurants or bars.
Smokers versus non-smokers at Wave 5
As shown in table 2, there were no significant differences in noticing smoking in restaurants, bars or workplaces between smokers and non-smokers in cities. In the rural areas, there were no differences for restaurants and bars, but smokers were more likely to report people smoking in their indoor workplace than non-smokers (74% vs 58%, p<0.05).
Support for smoke-free policies
Longitudinal trends from Waves 3–5
Support for smoking bans in public places was high overall among Chinese smokers and non-smokers and increased in most cities from Waves 3–5. Support was highest for total smoking bans in indoor workplaces (52%–84% across cities at Wave 5; 75% overall in cities; see figure 2D).
Support for total smoking bans in indoor areas of restaurants also increased across the cities from Waves 3–5 (50%–68% at Wave 5; 62% overall) (see figure 2E). Not surprisingly, support for smoking bans in bars was lower than support for smoking bans in other public places, ranging from only 22% in Kunming to 57% in Shanghai at Wave 5 and 42% of respondents in cities overall (figure 2F). However, support did increase slightly overall from Waves 3–5.
There were no significant differences in support for smoking bans between those cities that implemented a partial smoke-free law between Waves 3 and 4 and those that did not, for either workplaces (average increase of 14.4% vs 10.9%; p=0.553), restaurants (18.6% vs 16.1%, p=0.676) or bars (16.7% vs 13.5%, p=0.630).
Cities vs rural areas at Wave 5
As shown in table 2, there were no differences in support for complete smoking bans in restaurants, bars and workplaces between cities and rural areas at Wave 5.
Smokers vs non-smokers at Wave 5
Overall, support for smoke-free public places was high among all respondents but was higher among non-smokers compared with smokers at Wave 5 (see table 2). In the five cities, non-smokers were more likely than smokers to support complete smoking bans in restaurants (63% vs 54%, p<0.05) and workplaces (75% vs 63%, p<0.001), but there was no difference in support for smoke-free bars (42% vs 37%, p=0.296). Smokers and non-smokers in the rural areas did not differ in support.
Discussion
This study demonstrates that partial smoke-free laws in China have not led to significant reductions in SHS—a hazard that kills 100 000 people every year—and supports the urgent need for strong comprehensive smoke-free laws in China. During 2013–2015, fewer than half of all restaurants and one-quarter of bars that smokers and non-smokers last visited had complete smoking bans, and exposure to SHS in both urban and rural areas remains extremely high.
The finding that SHS in rural restaurants and bars is just as high as it is in cities and is significantly higher in rural workplaces is particularly alarming. The health and economic consequences of SHS exposure are thus likely to be greater in rural areas because of the higher prevalence and the lower level of healthcare resources available in rural China for preventing and treating smoking and SHS-related diseases.15 27
Comparison with other studies in China and other countries
It is well established that there is no safe level of exposure to tobacco smoke; thus, only 100% smoke-free laws have the potential to maximally protect the public from the harms of SHS.28 The findings from this study support previous research demonstrating that comprehensive smoking bans are more effective than partial bans or no ban.4 28 Across the ITC China cities, minor declines in smoking were observed in restaurants and workplaces, and to a lesser extent in bars, from 2009 to 2015. While smoking decreased in those cities that had implemented partial smoke-free laws between survey waves, there was no difference in the decrease in these cities compared with cities where no laws were implemented, demonstrating the failure of partial smoking bans to achieve even a partial reduction in SHS. These results are also consistent with previous research in China showing high levels of SHS exposure in public places—especially in rural areas—as well as no difference in SHS exposure in Chinese cities that had smoke-free restrictions in place compared with those without local smoke-free laws.10 13 29–31
The reductions in smoking across the ITC China cities from Waves 3–5 (ie, from 84% to 57% overall for restaurants) are also much lower than what has been achieved in other countries where comprehensive smoke-free laws have been implemented. For example, ITC research has shown that strong smoke-free laws implemented in Ireland in 2004 and in France in 2008 resulted in a near-total elimination of smoking in public places, including decreasing smoking in restaurants from over 70% to less than 5%.32 33
This study also highlights the high level of support for total smoking bans in China, even among smokers. Overall in 2013–2015, about two-thirds of all respondents (smokers and non-smokers combined) thought there should be a complete smoking ban in workplaces (62% in rural areas, 73% in cities), and over half of respondents supported a complete ban in restaurants (56% in rural areas, 61% in cities). Support was lower for complete smoking bans in bars (44% in rural areas, 41% in cities), but still increased among both smokers and non-smokers from 2009 to 2015. The levels of support for smoke-free public places among smokers in China (ie, from 37% for bars to 63% for workplaces among smokers in cities at Wave 5) are all higher than in every other ITC country prior to the implementation of comprehensive smoke-free laws, including Ireland, Scotland, England, France, Germany and the Netherlands—all of which experienced very substantial decreases in smoking after the ban, and most of which saw a significant increase in support among smokers after implementation.1 32 Support for smoke-free public places in China was even higher among non-smokers than smokers in 2013–2015, and there were no differences in support between urban and rural locations, demonstrating that comprehensive smoke-free laws would be very popular among all of the Chinese public.
Strengths and limitations of this study
Although previous studies in China using data from the 2010 Global Adult Tobacco Survey (GATS) and 2015 Tobacco Questions for Surveys (TQS) have examined rates of smoking in public places in urban and rural areas,31 34 the present study is the first cohort study of both smokers and non-smokers and in both cities and rural China to estimate overall population levels of smoking in public places and support for smoke-free laws, and to explicitly compare smokers and non-smokers in urban versus rural areas, where rates of smoking and smoking-related mortality are rising.
We relied on respondents’ self-reports to measure prevalence of smoking in public places and did not collect data on PM2.5 levels or use biomarkers to verify these reports, which may be subject to recall bias. However, the use of consistent measures in a cohort sample over time (which have been used in previous studies in China and other ITC countries31 33), the application of complex survey weights and the inclusion of both non-smokers and rural areas in the sample reduce any degree of bias and constitute a reasonably representative sample for estimates of smoking prevalence in each type of venue. Moreover, although there may be some degree of unreliability of reporting, there is no reason to believe that this would differ over time, and thus the analyses presented here on changes in reported smoking in these key venues from 2009 to 2015 would not be affected, including the key quasi-experimental test showing the lack of effectiveness of partial bans. Finally, while the longitudinal nature of the study means that some respondents were lost to attrition over time or did not provide responses at each time point, the use of GEE models that adjusted for within-subject correlation and the calibration of the rescaled cross-sectional survey weights means that the replenishment samples were comparable with the recontacted sample and can be used together to estimate population prevalences.24 25
Implications
The results showed that in both cities and rural locations, smoking was most likely to be observed in venues (workplaces, restaurants and bars) that had no rules about indoor smoking, and least likely to be observed in venues with a complete ban. These findings suggest that individual public venues can achieve success in reducing SHS exposure by implementing no-smoking rules that are stronger than what is required by local and national-level laws. It should be noted, however, that such bans in individual establishments are rare in China. In addition, despite the greater impact of complete smoking bans over partial bans on reducing smoking in public places, complete bans still did not eliminate smoking across all establishments. Smoking was still observed in 35% of workplaces, 38% of restaurants and 58% of bars that reportedly had a complete smoking ban in place at the time of the survey, demonstrating that enforcement of smoke-free laws was weak and remains a challenge in China. This is consistent with previous research showing that about 40% of public places where smoking was banned still had smoking in 2010–2011.29 35 The high smoking prevalence even in places where smoking is banned may also reflect the overall norms and expectations of the public that smoking is acceptable even in the presence of an official ban. It may be the case that if a comprehensive smoke-free law was implemented covering all venues, the norms would shift, and this would support and sustain compliance with that law.
Indeed, evidence from other countries has shown that public support does help to get smoke-free legislation adopted, and that implementation of smoke-free laws in turn increases support further through reduced visibility and social acceptability of smoking.36 This effect is greater with more comprehensive policies compared with partial laws. In China, cities may play an important role in changing the social norms of tobacco use from a bottom-up approach through efforts such as public education and media campaigns. By educating citizens, as well as taking the charge on implementing and enforcing smoke-free policies at the local level, cities have the opportunity and responsibility to increase acceptance and support for smoke-free laws, thus enhancing the likelihood of their success.37
Since China ratified the WHO FCTC, there has been little progress in its implementation, due to deep-rooted structural barriers and interference from the tobacco industry.38 Given the setback of the suspension of the draft national smoke-free law, there is now a shift towards smoke-free policy implementation at the local level. However, to date only four major cities—Beijing, Shanghai, Shenzhen and Xi’an—have implemented comprehensive smoke-free laws consistent with the Article 8 Guidelines of the WHO FCTC. Smoke-free progress is being further dampened by the State Tobacco Monopoly Agency’s recent strategy of building up a ‘civilized smoking environment’ where smokers coexist with non-smokers in ‘harmony’.39 40 This initiative has focused on building a network of indoor smoking rooms starting in four major cities in 2018 and is progressing rapidly across the country, despite strong evidence that designated smoking rooms do not protect against SHS exposure and only 100% smoke-free environments are effective.4 41
Comprehensive smoke-free laws with rigorous enforcement in China are ever more urgently needed in order to avert many millions of deaths. Doing so would put China on the path towards achieving its vision of a healthier future for its people.2 It is estimated that smoke-free policies alone could reduce the smoking rate in China by 2.7% by 2030, resulting in about 33 million fewer smokers.42 The positive impact of the 2015 Beijing smoke-free law confirms that such laws work in China: smoking prevalence in restaurants decreased from 40% before the law to 15% 1 month after the ban took effect, and reductions in smoking were observed across other public places and workplaces.43 44 However, while comprehensive smoke-free laws are an important step towards protecting the public from SHS, policymakers must also accelerate the implementation of stronger healthcare resources in addition to other key tobacco control measures needed to meet the country’s goal of reducing the smoking rate to 20% by 2030, especially for rural areas where disparities in healthcare services and accessibility remain.42
Supplementary Material
Acknowledgments
The authors acknowledge and thank all those who contributed to the ITC China Project, all study investigators, the project managers at University of Waterloo, China CDC team, and the local CDC staff at nine of the sampling locations, the Kunming Health Education Institute, and their field teams for their dedicated efforts in the data collection process.
Footnotes
Contributors: GTF, YJ and CW designed the sampling plan and the survey and led and oversaw the collection of data. MY and GM conducted the data analysis. GS and GTF designed the study and led the interpretation of results. GS led the writing of the manuscript and created the figures. LC, SSX, ACKQ, CW and GF reviewed the findings and contributed to the writing and interpretation of the findings. All authors approved the final version of the manuscript. All authors had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Funding: Waves 3–5 of the ITC China Survey were supported by grants from the US National Cancer Institute (R01 CA125116), the Canadian Institutes of Health Research (MOP 79551, MOP 115016) and the Chinese Center for Disease Control and Prevention. Additional support in preparing this paper was provided to University of Waterloo by the Canadian Institutes of Health Research (FDN-148477). GTF was supported by a Senior Investigator Grant from the Ontario Institute for Cancer Research and by a Senior Prevention Scientist Award from the Canadian Cancer Society Research Institute.
Disclaimer: The funders of the study had no role in study design, data collection, data analysis, data interpretation or writing of the report.
Competing interests: GTF has served as an expert witness on behalf of governments in litigation involving the tobacco industry.
Patient consent for publication: Not required.
Ethics approval: The ITC China Survey received ethics approval from the Chinese Center for Disease Control and Prevention (IRB 201114 and IRB 201325) and the Human Research Ethics Committee, University of Waterloo (ORE 15305 and ORE 17014). All respondents provided informed consent. Participation was voluntary and respondents received a token of appreciation for their time.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon reasonable request.
References
- 1. World Health Organization ITC project. Smoke-free policies in China, evidence of effectiveness and implications for action, October 2015. Geneva, 2015. [Google Scholar]
- 2. World Health Organization The Bill China Cannot Afford: Health, Economic and Social Costs of China’s Tobacco Epidemic. Manila, Philippines, 2017. [Google Scholar]
- 3. Drope J, Schluger N, Cahn Z, et al. . The tobacco atlas. 6th edn Atlanta: American Cancer Society and Vital Strategies, 2018. [Google Scholar]
- 4. International Agency for Research on Cancer (IARC) IARC handbooks of cancer prevention in tobacco control: evaluating the effectiveness of smoke-free policies. 13 Lyon, France: IARC, 2009. [Google Scholar]
- 5. Campaign for Tobacco Free Kids Smoke-free laws encourage smokers to quit and discourage youth from starting, 2017. [Google Scholar]
- 6. Lv J, Su M, Hong Z, et al. . Implementation of the WHO framework convention on tobacco control in mainland China. Tob Control 2011;20:309–14. 10.1136/tc.2010.040352 [DOI] [PubMed] [Google Scholar]
- 7. Ministry of Health China tobacco control report. Beijing, 2007. [Google Scholar]
- 8. Ye X, Yao Z, Gao Y, et al. . Second-hand smoke exposure in different types of venues: before and after the implementation of smoke-free legislation in Guangzhou, China. BMJ Open 2014;4:e004273 10.1136/bmjopen-2013-004273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gao J, Zheng P, Gao J, et al. . Workplace smoking policies and their association with male employees' smoking behaviours: a cross-sectional survey in one company in China. Tob Control 2011;20:131–6. 10.1136/tc.2010.036335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Fong GT, Sansone G, Yan M, et al. . Evaluation of smoke-free policies in seven cities in China, 2007-2012. Tob Control 2015;24 Suppl 4:iv14–20. 10.1136/tobaccocontrol-2015-052508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ye X, Chen S, Yao Z, et al. . Smoking behaviors before and after implementation of a smoke-free legislation in Guangzhou, China. BMC Public Health 2015;15:982 10.1186/s12889-015-2353-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Statistics China 2015 national population sampling survey main data Bulletin, 2016. Available: http://www.stats.gov.cn/tjsj/zxfb/201604/t20160420_1346151.html [Accessed 15 Aug 2017].
- 13. Liang X. China adult tobacco survey report. Beijing, China, 2015. [Google Scholar]
- 14. Chen Z, Peto R, Zhou M, et al. . Contrasting male and female trends in tobacco-attributed mortality in China: evidence from successive nationwide prospective cohort studies. Lancet 2015;386:1447–56. 10.1016/S0140-6736(15)00340-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ling RE, Liu F, Lu XQ, et al. . Emerging issues in public health: a perspective on China's healthcare system. Public Health 2011;125:9–14. 10.1016/j.puhe.2010.10.009 [DOI] [PubMed] [Google Scholar]
- 16. Wagstaff A, Lindelow M, Wang S, et al. . Reforming China’s rural health system. Washington, D.C.: World Bank, 2009. [Google Scholar]
- 17. Zimmer Z, Kaneda T, Spess L. An examination of urban versus rural mortality in China using community and individual data. J Gerontol B Psychol Sci Soc Sci 2007;62:S349–57. 10.1093/geronb/62.5.S349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wu C, Thompson ME, Fong GT, et al. . Methods of the International tobacco control (ITC) China survey: waves 1, 2 and 3. Tob Control 2015;24 Suppl 4:iv1–5. 10.1136/tobaccocontrol-2014-052025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Wu C, Thompson ME, Fong GT, et al. . Methods of the International tobacco control (ITC) China survey. Tob Control 2010;19 Suppl 2:i1–5. 10.1136/tc.2009.029900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. ITC Project ITC China wave 1 (2006) technical report. Waterloo, Ontario, Canada and Beijing, China, 2010. [Google Scholar]
- 21. ITC Project ITC China wave 2 (2007-2009) technical report. Waterloo, Ontario, Canada and Beijing, China, 2010. [Google Scholar]
- 22. ITC Project ITC China wave 3 (2009) technical report. Waterloo, Ontario, Canada and Beijing, China, 2011. [Google Scholar]
- 23. ITC Project ITC China wave 4 (2011-2012) technical report. Waterloo, Ontario, Canada and Beijing, China, 2015. [Google Scholar]
- 24. ITC Project ITC China wave 5 (2013-2015) technical report, 2017. [Google Scholar]
- 25. Liang K-YEE, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika 1986;73:13–22. 10.1093/biomet/73.1.13 [DOI] [Google Scholar]
- 26. Muller CJ, MacLehose RF. Estimating predicted probabilities from logistic regression: different methods correspond to different target populations. Int J Epidemiol 2014;43:962–70. 10.1093/ije/dyu029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hsiao W, Li M, Zhang S. China’s Universal Health Care Coverage : Towards universal health care in emerging economies. London: Palgrave Macmillan UK, 2017: 239–66. [Google Scholar]
- 28. World Health Organization WHO report on the global tobacco epidemic, 2009: implementing smoke-free environments. Geneva: World Health Organization, 2009. [Google Scholar]
- 29. Yang T, Jiang S, Barnett R, et al. . Who smokes in smoke-free public places in China? Findings from a 21 City survey. Health Educ Res 2015;21:cyv054 10.1093/her/cyv054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Yang T, Jiang S, Barnett R, et al. . Individual and city-level determinants of secondhand smoke exposure in China. Int J Health Geogr 2015;14:36 10.1186/s12942-015-0029-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Nan Y, Xi Z, Yang Y, et al. . [The 2015 China Adult Tobacco Survey: exposure to second-hand smoke among adults aged 15 and above and their support to policy on banning smoking in public places]. Zhonghua Liu Xing Bing Xue Za Zhi 2016;37:810–5. 10.3760/cma.j.issn.0254-6450.2016.06.014 [DOI] [PubMed] [Google Scholar]
- 32. Fong GT, Hyland A, Borland R, et al. . Reductions in tobacco smoke pollution and increases in support for smoke-free public places following the implementation of comprehensive smoke-free workplace legislation in the Republic of ireland: findings from the ITC Ireland/UK survey. Tob Control 2006;15 Suppl 3:iii51–8. 10.1136/tc.2005.013649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Fong GT, Craig LV, Guignard R, et al. . Evaluating the effectiveness of France's indoor smoke-free law 1 year and 5 years after implementation: findings from the ITC France survey. PLoS One 2013;8:e66692 10.1371/journal.pone.0066692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Jin Y, Wang L, Lu B, et al. . Secondhand smoke exposure, indoor smoking bans and smoking-related knowledge in China. Int J Environ Res Public Health 2014;11:12835–47. 10.3390/ijerph111212835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Liu R, Jiang Y, Travers MJ, et al. . Evaluating the efficacy of different smoking policies in restaurants and bars in Beijing, China: a four-year follow-up study. Int J Hyg Environ Health 2014;217:1–10. 10.1016/j.ijheh.2013.02.011 [DOI] [PubMed] [Google Scholar]
- 36. Mons U, Nagelhout GE, Guignard R, et al. . Comprehensive smoke-free policies attract more support from smokers in Europe than partial policies. Eur J Public Health 2012;22 Suppl 1:10–16. 10.1093/eurpub/ckr202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Redmon P, Koplan J, Eriksen M, et al. . The role of cities in reducing smoking in China. Int J Environ Res Public Health 2014;11:10062–75. 10.3390/ijerph111010062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Yang G, Wang Y, Wu Y, et al. . The road to effective tobacco control in China. Lancet 2015;385:1019–28. 10.1016/S0140-6736(15)60174-X [DOI] [PubMed] [Google Scholar]
- 39. Yu G. It is very necessary to build a civilized smoking environment, 2018. Available: http://www.tobaccochina.com/shidian/zaixianshidian/201812/20181217174257_777988.shtml [Accessed 14 Jan 2019].
- 40. STMA issued this guideline: building a civilized smoking environment and helping to build a beautiful China, 2018. Available: http://www.etmoc.com/gedi/Newslist?Id=104161 [Accessed 14 Jan 2019].
- 41. World Health Organization WHO report on the global tobacco epidemic, 2017: monitoring tobacco use and prevention policies. Geneva, 2017. [Google Scholar]
- 42. Goodchild M, Zheng R. Tobacco control and healthy China 2030. Tob Control 2019;28:409–13. 10.1136/tobaccocontrol-2018-054372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Xiao L, Jiang Y, Liu X, et al. . Smoking reduced in urban restaurants: the effect of Beijing smoking control regulation. Tob Control 2017;26:e75–8. 10.1136/tobaccocontrol-2016-053026 [DOI] [PubMed] [Google Scholar]
- 44. Hui SJ. Press release: 2016 Beijing adult tobacco survey results released, 2016. Available: http://www.bjjkjy.org/html/report/16120765-1.htm
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.