Abstract
Introduction:
This study sought to empirically evaluate whether the Medicaid expansion under the Affordable Care Act increased smoking cessation among low-income childless adult smokers.
Methods:
The effects of the Medicaid expansion on smoking quit attempts and the probability of 30- and 90-day smoking cessation were evaluated using logistic regression and data from the 2010–2011 and 2014–2015 waves Tobacco Use Supplement to the Current Population Survey. Using boosted logistic regression, the Tobacco Use Supplement was restricted to an analytic sample composed of childless adults with high probability of being <138% of the federal poverty level. Propensity score weighting was used to compare changes in smoking cessation among a sample of past smokers in states that expanded Medicaid with a control sample of past smokers in states that did not expand Medicaid with similar sociodemographic characteristics and smoking histories. This study additionally controlled for state socioeconomic trends, welfare policies, and tobacco control policies. Analysis was conducted between January 2018 and June 2019.
Results:
After weighting by propensity score and adjusting for state socioeconomic trends, welfare policies, and tobacco control policies, the Affordable Care Act Medicaid expansion was not associated with increases in quit attempts or smoking cessation.
Conclusions:
The Affordable Care Act Medicaid expansion did not appear to improve smoking cessation, despite extending health insurance eligibility to 2.3 million low-income smokers. Greater commitments to reducing barriers to cessation benefits and increasing smoking cessation in state Medicaid programs are needed to reduce smoking in low-income populations.
INTRODUCTION
Reducing smoking among people of low SES is an important goal for tobacco control in the U.S.1 Compared with people with high income or education, people with low income or education are more likely to smoke2,3 and smoke over longer periods of time.4 Consequently, they are at greater risk for lung cancer,5 respiratory and cardiovascular diseases,6 and premature mortality.3 Once initiated, low-SES smokers are far less likely to quit smoking than high-SES smokers,6 which contributes to the smoking disparities between these populations. For example, in 2012, only 34.5% of smokers living below the poverty line successfully quit smoking after quit attempts compared with 57.5% of those living at or above the poverty line.6 In part, low-SES smokers may be less likely to quit smoking because they have less access to cessation aids, which have been shown to be effective at increasing abstinence during quit attempts.7-13 Low-SES individuals are less likely to have health insurance,14 and cessation aids typically require prescriptions from healthcare providers and cost between $100 and $500 per prescription.15
In 2014, the Affordable Care Act (ACA) sought to expand Medicaid health insurance coverage to all individuals living <138% of the federal poverty level (FPL). However, the Supreme Court limited HHS’s authority to enforce the Medicaid expansion and left the Medicaid expansion up to states to decide.16 Since 2014, a total of 33 states have expanded Medicaid under the ACA.17 Most states expanded Medicaid on January 1, 2014, and all adults without dependent children <138% of the FPL became newly eligible. Some states expanded Medicaid after 2014 or already had coverage for some of the individuals included in the expansion before 2014. Appendix Table 1 provides information about each state’s Medicaid expansion status.
Among the newly Medicaid eligible populations were 2.3 million low-income smokers.18 In conjunction with an ACA mandate that state Medicaid programs cover all U.S. Food and Drug Administration-approved cessation aids, such as prescription medicines and nicotine-replacement therapies, this expansion increased access to smoking-cessation aids. Recent studies have found this expansion increased new prescriptions for smoking-cessation medications by 24%19 and decreased cigarette purchases while increasing the probability of purchasing smoking-cessation products.20
Despite the evidence that the Medicaid expansion decreased cigarette purchases and increased use of cessation aids, the relationship between Medicaid and smoking-cessation outcomes is unclear. Four studies have attempted to answer this question, three using Behavioral Risk Factor Surveillance System data and one using National Health Interview Survey data. All four studies used difference-in-differences study designs to compare smoking trends in states that did and did not expand Medicaid. Two studies found the Medicaid expansion reduced the probability of current smoking21,22 and another found that it increased 30-day cessation.23. However, one study that controlled for changes to Medicaid nationwide following the ACA found no effect of the Medicaid expansion on smoking.24
This study sought to build on this literature and examine the effect of the Medicaid expansion on smoking cessation using a different data set—the Tobacco Use Supplement to the Current Population Survey (TUS-CPS)—and propensity score weighting to compare smoking cessation across individuals in expansion and non-expansion states. The TUS-CPS permitted exploration of more detailed smoking-cessation outcomes than in previous studies, such as quit attempts and 90-day smoking cessation, as well as ability to adjust for previous smoking history and intensity.
METHODS
Study Sample
This analysis used data from the TUS-CPS and Annual Social and Economics Supplement of the Current Population Survey (ASEC), downloaded from the Integrated Public Use Microdata Series,25 for years 2010, 2011, 2014, and 2015. The TUS-CPS is a survey of non-institutionalized adults, with data about smoking behaviors and cessation, and is conducted alongside the U.S. Census Bureau’s CPS every 3–4 years. The ASEC is conducted alongside the CPS in March each year, measures individual income, and is the official source for estimates of health insurance coverage in each state. The CPS uses a panel-rotating design (described elsewhere)26 and only a subset of CPS respondents complete both the ASEC and TUS-CPS. Linking the two data sets would have limited sample size considerably, so the TUS-CPS and ASEC were analyzed separately. Analysis was conducted between January 2018 and June 2019.
Measures
Income in the TUS-CPS is reported as the total income of all related family members living in the same household. However, income used to determine health insurance eligibility is measured only among an individual, their spouse, and their dependent children (called a “health insurance unit”).27 To focus the analysis on respondents targeted by the ACA Medicaid expansion (childless adults <138% of the FPL), the TUS-CPS was restricted to respondents with high probability of being <138% of the FPL based on predictions from a boosted logistic regression trained in ASEC data where income at the health insurance unit was measured.
Variables used to fit boosted logistic regression predictions were sociodemographic characteristics available and collected in the same manner in both data sets. These included age, race/ethnicity, number of children, education, employment status, occupation classification, hours worked in the previous week, total family income, and up to second-order interaction terms for all variables. Diagnostics for the boosted logistic regression are described in the Appendix. These diagnostics include the rule used to determine the optimal cut off for inclusion in the analytic sample (Appendix Figure 1), plots demonstrating which variables were most influential in predictions (Appendix Figure 2), fivefold cross validation (Appendix Table 2), and descriptive statistics comparing respondents predicted <138% of the FPL in the TUS-CPS to respondents actually <138% of the FPL in the ASEC (Appendix Table 3).
To assess whether results were sensitive to the optimal cut off used for the sample restriction (described in Appendix Figure 1), sensitivity analyses were conducted using ten alternative cut offs. To assess whether results using boosted logistic regression for sample restriction were consistent with other possible sample restrictions, sensitivity analysis was also conducted restricting the sample to respondents with high school education or less following previous studies of the Medicaid expansion when income at the health insurance unit level has not been available.28
The analytic sample restricted the full TUS-CPS sample from 2010–2011 and 2014–2015 (N=438,618) to adults aged 25–64 years (n=309,671) without dependent children (n=155,713), who reported smoking 1 year ago (n=23,319), were predicted <138% of the FPL by the boosted logistic regression (n=10,408), lived in states without prior substantial state Medicaid expansions and that did not expand Medicaid after the second wave of data collection had already started (n=8,868), and did not have missing information regarding their smoking histories. The final analytic sample included 8,523 respondents. The main outcomes for this study consisted of binary events where respondents who reported smoking 1 year ago (1–year ago smokers) reported any attempts to quit smoking in the past year (quit attempts), reported having quit smoking >30 days ago (30-day cessation), and reported having quit smoking >90 days ago (90-day cessation).
Statistical Analysis
Changes in smoking cessation for childless adults predicted <138% of the FPL in states that expanded Medicaid between the 2010–2011 and 2014–2015 waves of the TUS-CPS were compared with changes in smoking cessation for a comparable sample of adults in states that did not expand Medicaid. The analysis used a propensity score weighting strategy that has been detailed closely in another paper,29 and has been shown to work well in difference-in-difference study designs with repeated cross-sectional data.29 Propensity score weights were estimated to balance the treatment and control groups before and after the Medicaid expansion with respect to age, sex, race/ethnicity, education, employment, number of years since started smoking regularly, and average number of cigarettes smoked per day 1 year ago.
Using the propensity score weights described above, weighted logistic regression was estimated for each cessation outcome using a binary indicator for whether each state expanded Medicaid, a binary indicator for the wave following the Medicaid expansion in 2014–2015, and an interaction term between whether each state expanded Medicaid and the 2014–2015 wave. In a second specification, the regression additionally controlled for state- and time-varying covariates that included state/year unemployment and poverty rates, maximum Temporary Assistance for Needy Families benefit for a family of two, minimum wage, earned income tax credits, state and federal taxes per pack on cigarettes, percentage of residents covered by smoke-free laws, and per-capita expenditures on tobacco control. This specification also included a variable for the number of cessation aids (prescription pills and nicotine-replacement therapies separately) that were covered by Medicaid in each state/year to control for the effects of the 2014 nationwide ACA mandate that state Medicaid programs cover all Food and Drug Administration–approved cessation products. Further description of these variables and their data sources is included in Appendix Table 4.
Average marginal effects (AMEs) and RRs associated with the interaction term between the binary indicators for Medicaid expansion states and the 2014–2015 survey waves were calculated and used for point estimates and hypothesis testing. In non-linear models, the magnitude and statistical significance of marginal effects varies across observations.30 Therefore, AMEs were reported and represent the average change in the predicted probability of quitting smoking associated with the Medicaid expansion. AMEs were reported instead of ORs to facilitate comparison to other studies.31,32 To assess whether results on the additive scale were consistent with results on the multiplicative scale, the RR associated with the interaction term was also reported.33 These estimates captured the unbiased policy effects of the ACA Medicaid expansion, provided that exposure to a state Medicaid expansion was independent of the trend in cessation outcomes that would have occurred without the Medicaid expansion, conditional on the covariates used to estimate propensity score weights.29
To account for complex survey design, the logistic regression was estimated with weights constructed by multiplying each individual’s self-respondent weight by their propensity score weight.26 All hypothesis testing accounted for weights and state-level clustering.
RESULTS
Table 1 provides descriptive statistics for each of the four groups of individuals in the analytic sample. The means within each group with respect to sociodemographic characteristics and smoking history are presented in Columns 2–5, and the unweighted standardized difference in means between each group and the group of individuals in Medicaid expansion states before the Medicaid expansion are presented in Columns 6–8. Before weighting by propensity score, several standardized differences in means between the groups were >0.1, including age, proportion that were black, proportion that were usually full-time employed, proportion that were not in the labor force, and the number of years smoking. This suggests that there were large differences between respondents in expansion and non-expansion states before and after the Medicaid expansion, and that propensity score weighting will account for bias in a more robust fashion than simply including the covariates in a regression.34 Columns 9–11 of Table 1 present the standardized difference in means between each group and the group of individuals living in expansion states, pre-expansion, after weighting by propensity score. After weighting, differences between groups were eliminated on all observed variables for sociodemographic characteristics and smoking history.
Table 1.
Characteristics of Respondents in Expansion and Non-expansion States Before and After Weighting by Propensity Score
| Covariate | Group 1: Expand pre |
Group 2: Expand post |
Group 3: No expand pre |
Group 4: No expand post |
Unweighted standardized difference in means |
Weighted standardized difference in means |
||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2 vs 1 | 3 vs 1 | 4 vs 1 |
2 vs 1 |
3 vs 1 |
4 vs 1 |
|||||
| Age, years | 45.6 | 47.9 | 46.9 | 48.3 | 0.19 | 0.11 | 0.23 | 0 | 0 | 0.02 |
| Female (p) | 0.41 | 0.42 | 0.40 | 0.43 | 0.03 | −0.01 | 0.06 | 0 | 0 | 0.04 |
| Black (p) | 0.14 | 0.15 | 0.22 | 0.26 | 0.02 | 0.24 | 0.33 | 0.01 | −0.01 | 0.01 |
| Hispanic (P) | 0.11 | 0.11 | 0.09 | 0.09 | 0.01 | −0.06 | −0.06 | −0.01 | 0 | −0.02 |
| High school graduate (P) | 0.43 | 0.40 | 0.44 | 0.42 | −0.05 | 0.02 | −0.02 | −0.01 | 0.01 | −0.01 |
| Some college (p) | 0.29 | 0.29 | 0.24 | 0.24 | 0.01 | −0.10 | −0.10 | 0 | −0.01 | 0 |
| College graduate (p) | 0.07 | 0.06 | 0.05 | 0.06 | −0.05 | −0.08 | −0.05 | 0.01 | −0.01 | 0 |
| Usual full-time (p) | 0.13 | 0.10 | 0.17 | 0.14 | −0.07 | 0.11 | 0.02 | 0 | 0 | −0.01 |
| Usual part-time (P) | 0.14 | 0.15 | 0.13 | 0.12 | 0.04 | −0.01 | −0.05 | 0 | −0.01 | 0.01 |
| Not in labor force (p) | 0.55 | 0.63 | 0.51 | 0.62 | 0.17 | −0.06 | 0.16 | 0 | 0.01 | 0.01 |
| Smoking Intensitya | 13.9 | 13.5 | 14.8 | 13.3 | −0.04 | 0.09 | −0.07 | 0.01 | 0.01 | 0.01 |
| Years smokingb | 27.9 | 30.5 | 29.0 | 30.1 | 0.20 | 0.09 | 0.21 | −0.01 | 0.01 | 0.02 |
| N | 2,234 | 1,758 | 2,373 | 2,158 | ||||||
Notes: Standardized difference in means are the difference in means between each group and Group 1 divided by Group 1’s SD. Variables with means that represent proportions are denoted by (p). Boldface indicate differences in standardized means that are greater than 0.1.
Smoking intensity was defined as the average number of cigarettes each respondent reported smoking 1 year ago. For the respondents in the analytic sample that reported smoking less than once per day (N=1,821), there was substantial missing information (N=1,492). For these respondents, a random Poisson variable with a mean of 4 was imputed which approximately matches the distribution of smoking intensity for non-daily 1 year ago smokers whose smoking intensity was observed. For comparison, the distribution of smoking intensity for daily 1 year ago smokers approximately resembled a Poisson random variable with a mean of 16.
Years smoking was calculated by subtracting the age each respondent reported starting smoking regularly from their current age.
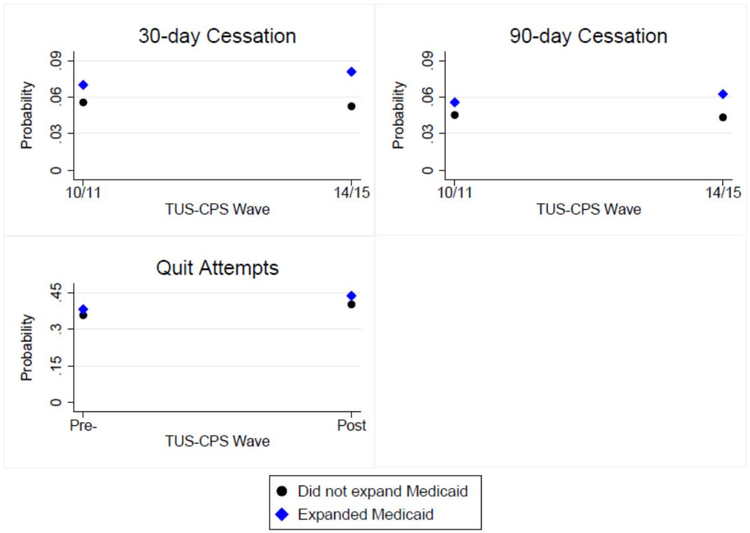
Figure 1 presents changes in each of the smoking-cessation outcomes between 2010–2011 and 2014–2015 in states that did and did not expand Medicaid under the ACA after propensity score weighting. In 2010–2011, the 30-day cessation, 90-day cessation, and quit attempts were higher in states that expanded Medicaid. Between 2010–2011 and 2014–2015, the 30- and 90- day cessation increased in expansion states and decreased in non-expansion states. Quit attempts increased between 2010–2011 and 2014–2015 in both expansion and non-expansion states.
Figure 1.
Changes in smoking cessation outcomes in expansion and non-expansion states following the Medicaid expansion.
TUS-CPS, Tobacco Use Supplement-Current Population Survey.
Prior to the Medicaid expansion, respondents in the analytic sample who lived in states that would later expand Medicaid had baseline probabilities of attempting to quit smoking of 0.383, quitting smoking for 30 days of 0.070, and quitting smoking for 90 days of 0.056 (Table 2). Based on the propensity score weighted logistic regression models, before adjusting for state-level variables, the effects of the Medicaid expansion were small, positive, and non-significant at the 5% level for quit attempts (AME=1.1 percentage points, 95% CI= −5 percentage points, 7 percentage points), 30-day cessation (AME=1.5 percentage points, 95% CI= −1 percentage points, 4 percentage points), and 90-day cessation (AME=1.0 percentage point, 95% CI= −2 percentage points, 4 percentage points) (Table 2, Column 3). However, after controlling for state-level covariates, point estimates changed; point estimates were negative and non-significant for quit attempts (AME= −1.9 percentage points, 95% CI= −9 percentage points, 5 percentage points), attenuated but still positive and non-significant for 30-day cessation (AME=0.3 percentage points, 95% CI= −3 percentage points, 3 percentage points), and negative and non-significant for 90-day cessation (AME= −0.1 percentage points, 95% CI= −3 percentage points, 3 percentage points) (Table 2, Column 5). Interaction effects on the risk scale matched marginal effects in terms of sign and significance across all specifications (Table 2, Columns 4 and 5).
Table 2.
Weighted Logistic Regression Analysis of the Effect of the Medicaid Expansion on Smoking Cessation (N=8,523)
| Unadjusted for state controlsa |
Adjusted for state controlsb | ||||
|---|---|---|---|---|---|
| Variable | Probability in expansion states pre- ACA |
Change in probability with expansion (95% CI) |
Change in relative risk with expansion (95% CI) |
Change in probability with expansion (95% CI) |
Change in relative risk with expansion (95% CI) |
| Quit attempts | 0.383 | 0.010 (−0.05,0.07) | 1.01 (0.87,1.17) | −0.019 (−0.09, 0.05) | 0.95 (0.79,1.11) |
| 30-day cessation | 0.070 | 0.014 (−0.01,0.04) | 1.22 (0.69,1.76) | 0.003 (−0.03,0.03) | 1.04 (0.56,1.53) |
| 90-day cessation | 0.056 | 0.010 (−0.02,0.04) | 1.17 (0.60,1.75) | −0.001 (−0.03, 0.03) | 0.98 (0.48,1.48) |
Notes: Column 2 provides a baseline estimate of the probability for each outcome in expansion states before the Medicaid expansion. Estimates were generated from a logistic regression, probability weighted by the product of each individual’s propensity score and TUS-CPS self-respondent weight. SEs used in CI estimation were clustered at the state level and calculated using the delta method. The authors estimate the effect of the Medicaid expansion as changes in probability (average marginal effects) and changes in RRs associated with the interaction term between Medicaid expansion states and the 2014/2015 TUS-CPS waves.
Columns 3 and 4 report estimates before adjusting for state-level controls.
Columns 5 and 6 report estimates after adjusting for state-level controls including state/year unemployment rates, poverty rates, earned income tax credit (EITC) as a percentage of federal EITC, maximum temporary assistance for needy families benefit for a family of two, minimum wage, cigarette taxes per pack, percentage of residents covered by comprehensive smoke-free laws, number of cessation aids covered by Medicaid, number of nicotine replacement therapies (NRTs) offered by Medicaid, and number of barriers to cessation aids and NRTs within Medicaid.
ACA, Affordable Care Act; TUS-CPS, Tobacco Use Supplement-Current Population Survey.
Results using alternative cut offs for restricting the sample to individuals with high probability of being <138% of the FPL were null and approximately the same as reported in Table 2 across all ten alternative specifications (Appendix Table 5) using the main propensity score weighted logistic regression with state-level controls. Alternative cut offs varied sensitivity (the probability that a respondent <138% of the FPL was included in the sample) from 60% to 90%, correspondingly increasing the sample size from 5,840 to 10,993 1-year ago smokers and false positive rate (the probability that a respondent >138% of the FPL was included in the sample) from 28% to 46%. Results restricting the sample to individuals with high school education or less, rather than using predictions from boosted logistic regression, were also null (Appendix Table 5).
DISCUSSION
The estimates reported in this study suggest that the effects of the Medicaid expansion on smoking cessation were close to zero. This contradicts the findings of previous papers that found expanding Medicaid was associated with decreased current smoking21,22 and increased smoking cessation.23 However, it supports the findings of another paper that found no effects of the Medicaid expansion on smoking after controlling for national effects of the ACA on Medicaid-eligible populations.24
The null results were surprising given evidence that cessation medication use increased following the Medicaid expansion.19,35 More work is needed to understand why increases in cessation medication use did not translate into meaningful changes in smoking-cessation outcomes. There may be other barriers to cessation that make cessation medications less effective in low-income and Medicaid-eligible populations. Collecting data on Medicaid enrollees about smoking behaviors, quit attempts, and cessation benefit use would help researchers better understand this important question and could result in meaningful improvements to cessation support programs in Medicaid.
Future work should identify barriers to smoking cessation among Medicaid enrollees and support reforms to Medicaid that evidence suggests would increase smoking cessation. For example, combined coverage of cessation aids and counseling therapy has been shown to increase probability of successful smoking cessation in Medicaid programs,36,37 but fewer than 33 states cover both of these services for all enrollees38 and few Medicaid smokers who try to quit use counseling services.22 Furthermore, several recent papers have pointed out that most Medicaid enrollees do not receive smoking-cessation services or know that Medicaid will pay for these services39 and that coverage for cessation services and barriers to their use vary widely across states and plans despite federal requirements.18,38 Variation in Medicaid cessation benefits exists even in states that expanded Medicaid, limiting the potential effectiveness of the Medicaid expansion for reducing smoking among newly eligible populations.39
Limitations
There were several limitations to this analysis, which might have led to underestimating the effect of the Medicaid expansion on smoking cessation. First, predicting whether respondents were <138% of the FPL means that the analysis was subject to measurement and misclassification error. As this threshold was not an exposure variable but rather an assessment of eligibility for the effect of Medicaid exposure, it was unclear what the effect of these errors would be on the analysis. To assess the impact of this measurement error, a separate multiple imputation analysis (reported in Appendix Table 4) was conducted. For the multiple imputation analysis, the entire analyses outlined in this paper was repeated 20 times using different random samples of ASEC respondents to train the boosted logistic regression that predicted whether TUS-CPS respondents were <138% of the FPL. Combined estimates of treatment effects and variance were then computed using Rubin’s combining rules.40 The results using this approach closely matched those reported in Table 2 (Appendix Table 4). Second, though this analysis indicated a lack of large effects of the Medicaid expansion on smoking cessation, smoking cessation is a rare outcome, the statistical tests used were moderately powered, and the CIs included negative, null, as well as small meaningful and positive effect sizes. In particular, the CIs included the effects identified in the one study that identified a positive effect of Medicaid expansion on smoking cessation using Behavioral Risk Factor Surveillance System data.23 Finally, this study reported on the effects of the Medicaid expansion during its first 2 years. The Medicaid expansion may have effects on smoking cessation as new enrollees experience improved access to medical professionals and cessation services over a longer time.
CONCLUSIONS
Although the Medicaid expansion extended new health insurance eligibility to millions of low-income smokers, this study did not find evidence that it increased smoking cessation in the first 2 years. Less than 20% of the newly Medicaid eligible smokers in the sample who attempted to quit smoking in 2014 and 2015 successfully quit for more than 30 days. Decreasing smoking among new Medicaid enrollees will require addressing the well-known barriers to cessation benefits in Medicaid programs.
Supplementary Material
ACKNOWLEDGMENTS
Research reported in this publication was supported by the National Cancer Institute of NIH (grant number R37CA214787). The content is solely the responsibility of the authors and does not necessarily represent the official views of NIH.
Footnotes
No financial disclosures or conflicts of interest were reported by the authors of this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.U. S. National Cancer Institute. A Socioecological Approach to Addressing Tobacco-Related Health Disparities. Bethesda, MD: HHS, NIH, National Cancer Institute; 2017. [Google Scholar]
- 2.Warren GW, Alberg AJ, Kraft AS, Cummings KM. The 2014 Surgeon General’s report: “The Health Consequences of Smoking–50 Years of Progress”: a paradigm shift in cancer care. Cancer. 2014;120(13): 1914–1916. 10.1002/cncr.28695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jamal A, Homa DM, O’Connor E, et al. Current cigarette smoking among adults—United States, 2005–2014. MMWRMorb Mortal Wkly Rep. 2015;64(44): 1233–1240. 10.15585/mmwr.mm6444a2. [DOI] [PubMed] [Google Scholar]
- 4.Siahpush M, Singh G, Jones P, Timsina L. Racial/ethnic and socioeconomic variations in duration of smoking: results from 2003, 2006 and 2007 Tobacco Use Supplement of the Current Population Survey. J Public Health (Oxf). 2010;32(2):210–218. 10.1093/pubmed/fdp104. [DOI] [PubMed] [Google Scholar]
- 5.Clegg LX, Reichman ME, Miller BA, et al. Impact of socioeconomic status on cancer incidence and stage at diagnosis: selected findings from the surveillance, epidemiology, and end results: National Longitudinal Mortality Study. Cancer Causes Control. 2009;20(4):417–435. https://doi.org/10,1007/s10552-008-9256-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.HHS. The health consequences of smoking—50 years of progress: a report of the Surgeon General. Atlanta, GA: HHS, CDC, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014. [Google Scholar]
- 7.Aubin H-J, Bobak A, Britton JR, et al. Varenicline versus transdermal nicotine patch for smoking cessation: results from a randomised open-label trial. Thorax. 2008;63(8):717–724. https://doi.org/10,1136/thx.2007.090647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Biazzo LL, Froshaug DB, Harwell TS, et al. Characteristics and abstinence outcomes among tobacco quitline enrollees using varenicline or nicotine replacement therapy. Nicotine Tob Res. 2010;12(6):567–573. 10.1093/ntr/ntq045. [DOI] [PubMed] [Google Scholar]
- 9.Cahill K, Lancaster T, Perera R. Pharmacological interventions for smoking cessation: an overview of reviews. Cochrane Database Syst Rev. 2011;9:CD009329 10.1002/14651858.cd009329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cummings KM, Hyland A. Impact of nicotine replacement therapy on smoking behavior. Anna Rev Public Health. 2005;26:583–599. 10.1146/annurev.publhealth.26.021304.144501. [DOI] [PubMed] [Google Scholar]
- 11.Ruger JP, Lazar CM. Economic evaluation of pharmaco-and behavioral therapies for smoking cessation: a critical and systematic review of empirical research. Annu Rev Public Health. 2012;33:279–305. 10.1146/annurev-publhealth-031811-124553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stead LF, Perera R, Bullen C, et al. Nicotine replacement therapy for smoking cessation. Cochrane Database Syst Rev. 2012;11:CD000146 10.1002/14651858.CD000146.pub4. [DOI] [PubMed] [Google Scholar]
- 13.Zhu S-H, Melcer T, Sun J, Rosbrook B, Pierce JP. Smoking cessation with and without assistance: a population-based analysis. Am J Prev Med. 2000; 18(4):305–311. 10.1016/s0749-3797(00)00124-0. [DOI] [PubMed] [Google Scholar]
- 14.Garfield R, Damico A, Stephens J, Rouhani S. The coverage gap: uninsured poor adults in states that do not expand Medicaid-an update. Menlo Park, CA: Kaiser Family Foundation; 2016. [Google Scholar]
- 15.Maclean JC, Pesko MF, Hill SC. The effect of insurance expansions on smoking cessation medication prescriptions: evidence from ACA Medicaid expansions. NBER Work Pap Ser. 2017;23450 10.3386/w23450. [DOI] [Google Scholar]
- 16.Musumeci M A Guide to the Supreme Court’s Decision on the ACA’s Medicaid Expansion. Menlo Park, CA: Kaiser Family Foundation; 2012. [Google Scholar]
- 17.The Kaiser Family Foundation State Health Facts. Status of State Action on the Medicaid Expansion Decision. Published 2018.
- 18.DiGiulio A, Haddix M, Jump Z, et al. State Medicaid expansion tobacco cessation coverage and number of adult smokers enrolled in expansion coverage—United States, 2016. MMWRMorb Mortal WklyRep. 2016;65(48):1364–1369. 10.15585/mmwr.mm6548a2. [DOI] [PubMed] [Google Scholar]
- 19.Maclean JC, Pesko MF, Hill SC. Public insurance expansions and smoking cessation medications. Econ Inq. In press. Online May 7, 2019. 10.1111/ecin.12794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cotti CD, Nesson E, Tefft N. Impacts of the ACA Medicaid expansion on health behaviors: evidence from household panel data. Health Econ. 2019;28(2):219–244. 10.1002/hec.3838. [DOI] [PubMed] [Google Scholar]
- 21.Simon K, Soni A, Cawley J. The impact of health insurance on preventive care and health behaviors: evidence from the first two years of the ACA Medicaid expansions. J Policy Anal Manage. 2017;36(2): 390–417. 10.1002/pam.21972. [DOI] [PubMed] [Google Scholar]
- 22.Brantley E, Greene J, Bruen B, Steinmetz E, Ku L. Policies affecting Medicaid beneficiaries’ smoking cessation behaviors. Nicotine Tob Res. 2019;21(2): 197–204. 10.1093/ntr/nty040. [DOI] [PubMed] [Google Scholar]
- 23.Koma JW, Donohue JM, Barry CL, Huskamp HA, Jarlenski M. Medicaid coverage expansions and cigarette smoking cessation among low-income adults. Med Care. 2017;55(12): 1023–1029. 10.1097/mlr.0000000000000821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Courtemanche C, Marton J, Ukert B, Yelowitz A, Zapata D. Early impacts of the Affordable Care Act on health insurance coverage in Medicaid expansion and non-expansion states. J Policy Anal Manage. 2017;36(1):178–210. 10.1002/pam.21961. [DOI] [PubMed] [Google Scholar]
- 25.Flood S, King M, Ruggles S, Warren R. Integrated Public Use Microdata Series, Current Population Survey: Version 5.0 [dataset]. Minneapolis, MN: University of Minnesota, 2017. 10.18128/D030.V5.0. [DOI] [Google Scholar]
- 26.Ridgeway G, Kovalchik SA, Griffin BA, Kabeto MU. Propensity score analysis with survey weighted data. J Causal Inference. 2015;3(2):237–249. 10.1515/jci-2014-0039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.State Health Access Data Assistance Center. Defining Family for Studies of Health Insurance Coverage. Minneapolis, MN: University of Minnesota; 2012. [Google Scholar]
- 28.Wehby GL, Lyu W. The impact of the ACA Medicaid expansions on health insurance coverage through 2015 and coverage disparities by age, race/ethnicity, and gender. Health Serv Res. 2018;53(2): 1248–1271. 10.1111/1475-6773.12711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stuart EA, Huskamp HA, Duckworth K, et al. Using propensity scores in difference-in-differences models to estimate the effects of a policy change. Health Sen’ Outcomes Res Methodol. 2014;14(4): 166–182. 10.1007/s10742-014-0123-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ai C, Norton EC. Interaction terms in logit and probit models. Econ Lett. 2003;80(1):123–129. 10.1016/s0165-1765(03)00032-6. [DOI] [Google Scholar]
- 31.Norton EC, Dowd BE, Maciejewski ML. Odds ratios—current best practice and use. JAMA. 2018;320(1):84–85. 10.1001/jama.2018.6971. [DOI] [PubMed] [Google Scholar]
- 32.Norton EC, Dowd BE. Log odds and the interpretation of logit models. Health Serv Res. 2018;53(2):859–878. 10.1111/1475-6773.12712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dow WH, Norton EC, Donahoe JT. Stata tip 131: multiplicative and marginal interaction effects in nonlinear models. Stata J. In press. [Google Scholar]
- 34.Harder VS, Stuart EA, Anthony JC. Propensity score techniques and the assessment of measured covariate balance to test causal associations in psychological research. Psychol Methods. 2010;15(3):234–239. 10.1037/a0019623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Richards MR, Marti J, Maclean JC, Fletcher J, Kenkel D. Tobacco control, Medicaid coverage, and the demand for smoking cessation drugs. Am J Health Econ. 2017;3(4):528–549. 10.1162/aihe_a_00087. [DOI] [Google Scholar]
- 36.Greene J, Sacks RM, McMenamin SB. The impact of tobacco dependence treatment coverage and copayments in Medicaid. Am J Prev Med. 2014;46(4):331–336. 10.1016/j.amepre.2013.11.019. [DOI] [PubMed] [Google Scholar]
- 37.Kostova D, Xu X, Babb S, McMenamin SB, King BA. Does state Medicaid coverage of smoking cessation treatments affect quitting? Health Serv Res. 2018;53(6):4725–4746. 10.1111/1475-6773.12979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.DiGiulio A, Jump Z, Yu A, et al. State Medicaid coverage for tobacco cessation treatments and barriers to accessing treatments—United States, 2015–2017. MMWR Morb Mortal Wkly Rep. 2018;67(13):390–395. 10.15585/mmwr.mm6713a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ku L, Bruen BK, Steinmetz E, Bysshe T. Medicaid tobacco cessation: big gaps remain in efforts to get smokers to quit. Health Aff (Millwood). 2016;35(l):62–70. 10.1377/hlthaff.2015.0756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Little RJ, Rubin DB. Statistical analysis with missing data. 2nd ed. Hoboken, NJ: John Wiley & Sons; 2002. 10.1002/9781119013563. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.