http://aasldpubs.onlinelibrary.wiley.com/hub/journal/10.1002/(ISSN)2046-2484/video/14-5-reading-moore a video presentation of this article
http://aasldpubs.onlinelibrary.wiley.com/hub/journal/10.1002/(ISSN)2046-2484/video/14-5-interview-moore the interview with the author
https://www.wileyhealthlearning.com/Activity/6952108/disclaimerspopup.aspx questions and earn CME
Abbreviations
- FDA
US Food and Drug Administration
- HCV
hepatitis C virus
- ITP
idiopathic thrombocytopenic purpura
- TIPS
transjugular intrahepatic portosystemic shunt
- TPO
thrombopoietin
Background
Thrombocytopenia is one of the most common hematological abnormalities and is often the first abnormality seen in patients with chronic liver disease. Thrombocytopenia affects approximately 6% of patients without cirrhosis and 70% of patients with cirrhosis. It is defined as a platelet count of less than 150,000/μL, with 100,000 to 150,000/μL considered as mild thrombocytopenia, 50,000 to 100,000/μL labeled as moderate thrombocytopenia, and less than 50,000/μL defined as severe thrombocytopenia.1 Thrombocytopenia can often be used as a marker of advanced liver disease, and some studies have shown moderate‐to‐severe thrombocytopenia to be a strong independent predictor of mortality.2, 3 Mild‐to‐moderate thrombocytopenia rarely has any clinical significance because spontaneous bleeding is unlikely to occur at these levels. However, moderate‐to‐severe thrombocytopenia can prevent patients from receiving vital interventions such as medications and invasive procedures. Delayed procedures and correction of platelet abnormalities for these procedures can increase hospitalization time and increase overall health care costs.4
The pathophysiology of thrombocytopenia in chronic liver disease is a rapidly evolving field. Previously, thrombocytopenia was thought to be solely a result of splenic sequestration caused by congestive splenomegaly as a result of portal hypertension. Now, however, there are several other proposed mechanisms regarding platelet production and destruction in cirrhosis (Fig. 1).
Figure 1.
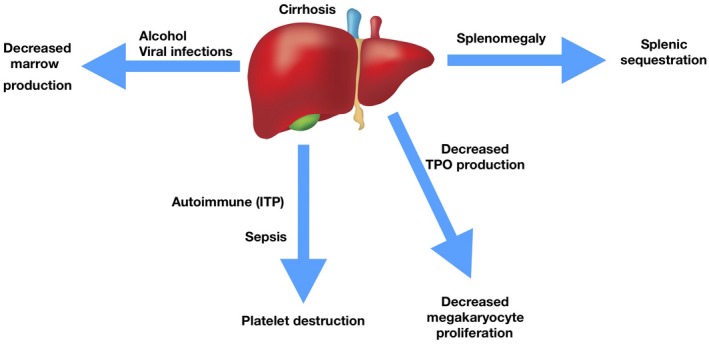
Common mechanisms of thrombocytopenia in cirrhosis.
Platelet production is largely associated with thrombopoietin (TPO). TPO is predominantly synthesized in the liver in parenchymal and sinusoidal endothelial cells and in the kidneys. Small amounts are also made in bone marrow stromal cells. TPO binds to the c‐mpl receptor on megakaryocytes, which, in turn, regulates the differentiation into platelets.5 There appears to be a direct correlation with stages of cirrhosis, levels of circulating TPO, and degree of thrombocytopenia. Increasing stages of fibrosis have been shown to lead to decreasing levels of circulating TPO, and thus a worsening degree of thrombocytopenia.6 In a study by Koruk et al.,7 comparing serum TPO levels in patients with chronic hepatitis and liver cirrhosis, TPO levels were normal in control and chronic hepatitis groups. However, TPO levels decreased as the degree of cirrhosis increased. Another cause of decreased platelet production includes reduced bone marrow production that can be a result of numerous causative factors but is commonly seen with alcohol abuse and with viral infections.
Mechanisms of platelet destruction can also contribute to thrombocytopenia in patients with cirrhosis. Immune‐mediated destruction plays a large role in platelet destruction, specifically in patients with autoimmune liver diseases and chronic hepatitis C virus (HCV), both of which have been shown to have an increased association with autoimmune thrombocytopenia purpura. Sepsis is another important contributor to platelet destruction. Patients with cirrhosis are at an increased risk for sepsis compared with the general population, and multiple mechanisms such as tumor necrosis factor‐α release during inflammatory states have been shown to contribute to platelet destruction.6
Another cause of thrombocytopenia, which is associated with platelet sequestration but not directly related to the mechanisms listed earlier, is pseudothrombocytopenia. This is a falsely low platelet count because of platelet clumping after some samples are exposed to the anticoagulant ethylene diamine tetraacetic acid. It is always important to exclude pseudothrombocytopenia by reviewing the peripheral smear for clumping or by repeating the complete blood count using a heparin or sodium citrate anticoagulant. Pulmonary hypertension and pulmonary emboli are also associated with platelet consumption and can often be seen in patients with cirrhosis.
Management of Thrombocytopenia in Cirrhosis
Thrombocytopenia plays an important role in the management of liver cirrhosis because a number of procedures have significant bleeding risks associated with them. Bedside and routine procedures such as paracentesis and esophagogastroduodenoscopy are generally considered a lower bleeding risk; however, liver biopsies, chemoembolizations, transjugular intrahepatic portosystemic shunts (TIPSs), and biliary procedures are considered higher risk, and thus could be deferred or could place the patient at significant risk for bleeding.8 In an analysis of bleeding complications after liver biopsy in patients with HCV with cirrhosis, 11% of biopsies were missed at the 24‐month mark because of thrombocytopenia, and there was a significantly increased risk for bleeding in patients with a platelet count of less than 60,000/μL.9
There have been several advances in the management of thrombocytopenia in chronic liver disease over the past decade. Standard treatments of thrombocytopenia include transfusions, splenectomy, or splenic artery embolization. Aside from an inability to correct platelet function, there are several problems associated with platelet transfusions. First, no clear cutoffs exist to guide platelet transfusions, specifically with regard to safe thresholds for different procedures. Second, platelet transfusions carry an increased risk for infection in all patients with cirrhosis and an increased risk for graft‐versus‐host disease in transplant patients. Lastly, multiple platelet transfusions can lead to platelet refractoriness, an inability to achieve the desired platelet count after a transfusion.10 Laparoscopic splenectomy and splenic artery embolization have been extensively studied and have been shown to have effective improvement in thrombocytopenia. However, both are associated with significant morbidity and mortality rates. TIPS has been effective in some patients, specifically those with severe thrombocytopenia; however, it is not a proven intervention. Few studies exist on the effectiveness of TIPS, and it is unclear which patients will respond because of the unknown mechanism of correction of thrombocytopenia.11
Recent advances in the management of thrombocytopenia include the use of TPO receptor agonists, especially in patients who are considered poor surgical candidates. These medications act on the human TPO receptor (c‐mpl), thereby promoting the proliferation of megakaryocytes and increasing platelet count. The first of these medications, eltrombopag, was approved by the US Food and Drug Administration (FDA) in 2008 for the treatment of idiopathic thrombocytopenic purpura (ITP). In a study by Afdhal et al.,12 eltrombopag reduced the need for transfusions in patients with chronic liver disease who underwent elective invasive procedures, but it was also associated with an increased risk for portal vein thrombosis. As a result, eltrombopag is not recommended for patients with chronic liver disease who are undergoing elective procedures.12 Two newer medications, avatrombopag and lusutrombopag, were FDA approved in 2018; they were approved specifically for patients with liver disease who are scheduled for a procedure. Both have been shown to have a lower incidence of platelet transfusions prior to procedures and lower associated bleeding risks postprocedure.13, 14 In addition, TPO receptor agonists have been shown to reduce costs by approximately $500 when compared with the costs of multiple platelet transfusions.15
In conclusion, thrombocytopenia plays an important role in the management of patients with chronic liver disease and cirrhosis. Multiple mechanisms can contribute to the development of thrombocytopenia, and a number of management options are available for its treatment, with early promising results noted among the newly approved TPO receptor agonists. Further studies are needed to investigate the association of morbidity and mortality with thrombocytopenia and the role that TPO receptor agonists play in increasing survival in patients with chronic liver disease and cirrhosis.
Potential conflict of interest: Nothing to report.
References
- 1. Peck‐Radosavljevic M. Thrombocytopenia in chronic liver disease. Can J Gastroenterology 2000;14(suppl D):60D‐66D. [DOI] [PubMed] [Google Scholar]
- 2. Bleibel W, Caldwell S, Curry M, et al. Peripheral platelet count correlates with liver atrophy and predicts long‐term mortality on the liver transplant waiting list. Transplant Int 2013;26:435‐442. [DOI] [PubMed] [Google Scholar]
- 3. Qamar A, Grace N, Groszmann RJ, et al. Incidence, prevalence, and clinical significance of abnormal hematologic indices in compensated cirrhosis. Clin Gastroenterol Hepatol 2009;7:689‐695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Poordad F. Thrombocytopenia in chronic liver disease. Aliment Pharmacol Ther 2007;26(suppl 1):5‐11. [DOI] [PubMed] [Google Scholar]
- 5. Kaushansky K. Lineage‐specific hematopoietic growth factors. N Engl J Med 2006;354:2034‐2045. [DOI] [PubMed] [Google Scholar]
- 6. Mitchell O, Feldman D, Diakow M, et al. The pathophysiology of thrombocytopenia in chronic liver disease. Hepat Med 2016;8:39‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Koruk M, Onuk MD, Akçay F, et al. Serum thrombopoietin levels in patients with chronic hepatitis and liver cirrhosis, and its relationship with circulating thrombocyte counts. Hepatogastroenterology 2002;49:1645‐1648. [PubMed] [Google Scholar]
- 8. Terrault N, Bibbiani F, Chen Y‐C, et al. Superiority of avatrombopag (AVA) to placebo (PBO) for the treatment of chronic liver disease (CLD)‐associated thrombocytopenia (TCP) in patients undergoing scheduled procedures: results of 2 randomized, PBO‐controlled phase 3 studies. Hepatology 2017;66(suppl S1):124A‐125A (abstract 217).28295475 [Google Scholar]
- 9. Seeff LB, Everson GT, Morgan TR, et al. Complication rate of percutaneous liver biopsies among persons with advanced chronic liver disease in the HALT‐C trial. Clin Gastroenterol Hepatol 2010;8:877‐883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Maan R, Knegt RJ, Veldt BJ. Management of thrombocytopenia in chronic liver disease: focus on pharmacotherapeutic strategies. Drugs 2015;75:1981‐1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Massoud OI, Zein NN. The effect of transjugular intrahepatic portosystemic shunt on platelet counts in patients with liver cirrhosis. Gastroenterol Hepatol 2017;13:286‐291. [PMC free article] [PubMed] [Google Scholar]
- 12. Afdhal NH, Giannini EG, Tayyab G, et al. Eltrombopag before procedures in patients with cirrhosis and thrombocytopenia. N Engl J Med 2012;367:716‐724. [DOI] [PubMed] [Google Scholar]
- 13. Hidaka H, Kurosaki M, Tanaka H, et al. Lusutrombopag reduces need for platelet transfusion in patients with thrombocytopenia undergoing invasive procedures. Clin Gastroenterol Hepatol 2019;17:1192‐1200. [DOI] [PubMed] [Google Scholar]
- 14. Tateishi R, Seike M, Kudo M, et al. A randomized controlled trial of lusutrombopag in Japanese patients with chronic liver disease undergoing radiofrequency ablation. J Gastroenterol 2019;54:171‐181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Moussa MM, Mowafy N. Preoperative use of romiplostim in thrombocytopenic patients with chronic hepatitis C and liver cirrhosis. J Gastroenterol Hepatol 2013;28:335‐341. [DOI] [PubMed] [Google Scholar]


