Abstract
The aim of this study was to evaluate the effectiveness of preventing mother to child syphilis transmission to improve pregnancy outcomes. We performed a retrospective analysis of municipal databases of mother-to-child syphilis transmission. Pregnant women with syphilis were included. Group specific pregnancy outcomes were analyzed according to treatment. A total of 28 pregnant women were diagnosed with syphilis in 2012; 321 were diagnosed with syphilis in 2018. A prevalence of 0.14% was observed amongst pregnant women in Suzhou city from 2012–2018. Primary treatments included benzathine penicillin, ceftriaxone sodium or erythromycin when patients were allergic to Benzathine penicillin. The treatment coverage was 81.57%, and only 52.86% of pregnant women were adequately treated. Adverse pregnant outcomes were higher amongst untreated women. Expanding early screening coverage and promoting treatment were key to improving pregnancy outcomes amongst women with syphilis.
Subject terms: Bacterial infection, Health policy
Introduction
Syphilis is a systemic, sexually transmitted disease caused by the bacterium Treponema pallidum that can be transmitted via sexual exposure or from infected mothers to children. Most maternal syphilis infections are latent, and untreated infections can lead to adverse pregnancy outcomes1,2. Syphilis remains a public health problem. There were an estimated 988,000 pregnant women infected with syphilis of which 52% experienced adverse pregnancy outcomes in 2016, including spontaneous abortions, stillbirths, preterm or low weight births, and clinical disease in infants3,4. Early diagnosis and immediate treatment with penicillin during antenatal care are highly effective in to the prevention of mother-to-child-transmission (PMTCT)5–7. The World Health Organization (WHO) launched the global initiative for the elimination of MTCT of syphilis and developed global guidance to reduce congenital syphilis incidence to ≤50 or fewer per 100,000 live births3. This included population-level antenatal care coverage for women ≥95%; coverage of syphilis testing of pregnant women ≥95%; and treatment coverage of syphilis-seropositive pregnant women ≥95%8. The implementation of PMTCT aims to control and eliminate the MTCT of syphilis. The ultimate goal is to minimize the proportion of untested, untreated or inadequately treated pregnant women to prevent adverse pregnancy outcomes in infants9.
Suzhou city is located in central Yangtze River Delta and is famous for its national high-tech industrial base. The population of Suzhou is 10.72 million. 50% of which are migrants. In 2018, the total number of pregnant women and live births in Suzhou were 111488 and 112523 respectively. According to Jiangsu provincial sexual disease surveillance data, adult syphilis increased from 23594 in 2015 to 27256 in 2018, with the incidence of congenital syphilis showing an upward trend during this period. The incidence of syphilis amongst pregnant women has significantly increased with the lack of diagnosis leading to underreported maternal and congenital syphilis cases10. The national program of integrated PMTCT of syphilis, HIV and hepatitis B were initiated in Suzhou city from 2011. A clearer understanding of the epidemiology of maternal syphilis and the effects of treatment were necessary for policy decisions and interventional guidance. This study was the first to evaluate the prevalence of maternal syphilis, the effectiveness of treatment, and syphilis-associated pregnancy outcomes in Suzhou city.
Results
From 2012 to 2018, a total of 1247 pregnant women diagnosed with syphilis in Suzhou according to the PMTCT system were assessed. The increase in annually diagnosed syphilis cases is shown in Table 1. The incidence of pregnant women with syphilis infections increased (χ2 = 873176, p < 0.001). A total of 368 (29.51%) infected pregnant women were local residents, and 879 (70.49%) were migrants. Amongst the 10 reported districts, the incidence was highest in Kunshan city and lowest in the Suzhou industrial park. The number of hospitalized live births decreased from 120,343 to 116,399, but the number of pregnant women diagnosed with syphilis increased from 28 to 321 from 2012 to 2018. Approximately 86.45% of pregnant women were diagnosed during prenatal examinations. In total, 12.27% were diagnosed during delivery. The demographic information of the pregnant women with syphilis infection was showed in Table 2.
Table 1.
Numbers of live births and syphilis infected women from 2012 to 2018.
| Year | Number of live births | Number of syphilis-infected pregnant women | Diagnose time | Number of congenital syphilis | ||
|---|---|---|---|---|---|---|
| prenatal examination | delivery | postpartum | ||||
| 2012 | 120343 | 28 | 23 | 5 | 0 | 0 |
| 2013 | 112947 | 98 | 85 | 12 | 1 | 2 |
| 2014 | 135181 | 155 | 135 | 20 | 0 | 2 |
| 2015 | 113714 | 203 | 174 | 27 | 2 | 1 |
| 2016 | 144437 | 206 | 172 | 29 | 5 | 2 |
| 2017 | 130155 | 236 | 207 | 24 | 5 | 1 |
| 2018 | 116399 | 321 | 282 | 36 | 3 | 0 |
| Total number | 873176 | 1247 | 1078 | 153 | 16 | 8 |
Table 2.
Demographic information of the 1247 pregnant women with syphilis infection.
| Number of infected pregnant women | ||
|---|---|---|
| Age | ≤20 years | 35 |
| 20–35 years | 1051 | |
| 35–48 years | 161 | |
| Education background | primary school and below | 88 |
| junior school | 538 | |
| junior high school | 332 | |
| bachelor degree and above | 238 | |
| no detailed information | 51 | |
| Transmission route | MTCT | 1 |
| needle stabbing | 1 | |
| Occupational exposure | 1 | |
| history of drug use | 1 | |
| sexual transmission | 508 | |
| blood transmission | 4 | |
| no detailed information | 731 | |
| Stage | latent stage | 1052 |
| primary stage | 25 | |
| secondary stage | 7 | |
| tertiary stage | 1 | |
| no detailed information | 162 | |
| Whether previously infected or not | yes | 489 |
| no | 758 | |
| Infection status of sexual partner | syphilis infected | 181 |
| not infected with syphilis | 532 | |
| not tested | 248 | |
| no detailed information | 286 | |
| Total number of pregnant women with syphilis infection | 1247 |
The number of puerpera with syphilis infections and live births increased from 2012 to 2018. The treatment of pregnant women with syphilis decreased (χ2 = 18.29, p = 0.006), but standardized treatment rates remained unchanged (χ2 = 10.22, p = 0.116), Table 3, Fig. 1.
Table 3.
Treatment rates of pregnant women and their newborns.
| Year | Number of puerpera with syphilis infection | Number of live births | Number of puerperae with treatment (n,%) | Number of puerperae with standardized treatment (n,%) | Number of newborns needed to be treated | Number of newborns with preventive Treatment (n,%) |
|---|---|---|---|---|---|---|
| 2012 | 30 | 29 | 29 (96.67) | 19 (63.33) | 10 | 8 (80.00) |
| 2013 | 112 | 112 | 100 (89.29) | 71 (63.39) | 41 | 15 (36.59) |
| 2014 | 157 | 152 | 124 (78.98) | 76 (48.41) | 76 | 35 (46.05) |
| 2015 | 178 | 174 | 151 (84.83) | 89 (50.00) | 85 | 39 (45.88) |
| 2016 | 202 | 207 | 150 (74.26) | 107 (52.97) | 98 | 34 (34.69) |
| 2017 | 193 | 196 | 159 (82.38) | 108 (55.96) | 86 | 34 (39.53) |
| 2018 | 246 | 247 | 199 (80.89) | 121 (49.19) | 126 | 67 (53.17) |
Figure 1.
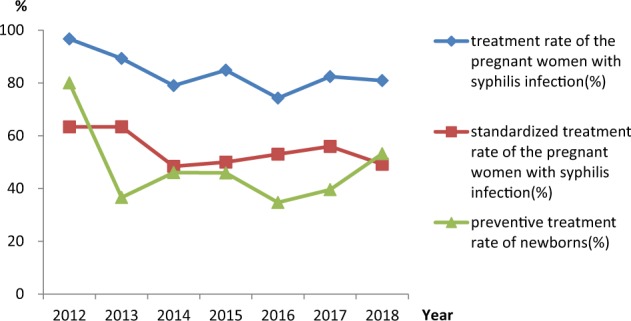
Treatment rates of pregnant women and newborns. (p ≤ 0.05 was considered statistically significant.
A total of 106 spontaneous abortions occurred, of which 11 died within 7 days of birth and 17 stillbirths occurred. Adverse pregnancy outcomes were higher amongst untreated women (χ2 = 213.96, p < 0.001). Detailed information is shown in Table 4.
Table 4.
Comparison of pregnancy outcomes according to treatment groups.
| Treatment group | Abortion (n,%) | Live births (n,%) | Died within seven days after birth (n,%) | Stillbirth (n,%) | Total |
|---|---|---|---|---|---|
| Untreated | 78 (73.59) | 193 (17.11) | 5 (45.45) | 10 (58.82) | 286 |
| Treated | 27 (25.47) | 323 (28.63) | 5 (45.45) | 3 (17.65) | 358 |
| Standardized treatment | 1 (0.94) | 612 (54.26) | 1 (9.10) | 4 (23.53) | 618 |
| Total | 106 | 1128 | 11 | 17 | 1262 |
(p ≤ 0.05 was considered statistically significant).
Discussion
According to the National Statutory Infectious diseases reports, the prevalence of adult syphilis and maternal syphilis infections have increased in China since 2011. The prevention of syphilis transmission from mother to children is therefore of high priority. In this study, the average prevalence of syphilis in pregnant women was 0.14%, which was similar to the reported prevalence of Europe (0.16%)11. The rate of maternal syphilis in Suzhou was 0.28% in 2018, which was higher than China (0.24%)12 and the Mediterranean (0.06%), but lower than Latin America (1.1%) and India (0.57–0.78%)11,13,14. The increased prevalence of maternal syphilis was partly due to the accumulation of the previously infected women and the inflow of the migrant pregnant women with syphilis infections. According to the requirement of PMTCT of syphilis program, free syphilis screening should be provided to all pregnant women during initial prenatal care examinations, but full coverage was not achieved. Based on our studies, most syphilis cases in infected pregnant women occur in migrants and the unemployed, in which educational background are junior school or below. These women do not value prenatal care and lack access to effective treatment. In addition, women with syphilis infections suffer from the stigma and sociological discrimination that occur for other sexually transmitted diseases (STDs). This physiological status restricts the awareness of pregnant women seeking professional medical healthcare.
Vertical transmission is dependent on the stages of maternal infection, for which the risk is highest during the primary and secondary stages of infection, followed by asymptomatic syphilis during pregnancy1,15. Adverse outcomes in pregnant women with syphilis infections are common, particularly for those who are inadequately treated16–18. A single dose of penicillin is the first-line treatment and most cost-effective treatment for women with syphilis during pregnancy19,20. Since the launch of the global initiative of eliminating the MTCT of syphilis, the Chinese government has integrated the PMTCT of HIV and syphilis with maternal healthcare management. The screening and surveillance of prenatal syphilis has improved in Suzhou city. From 2012 to 2018, the number of infants diagnosed with congenital syphilis has decreased. However, due to deliberate concealment and avoidance of syphilis detection, delayed diagnosis leads to delayed treatment. Consistent with previous studies21–23, to improve patient compliance, a efforts to promote the importance of pregnant syphilis screening and the benefits of standardized treatment have been employed. The syphilis screening rates at the first trimester have improved from 82.14% to 87.85% during the past 7 years in Suzhou. However, treatment rates of 16.32% were recorded in 2018 which were lower than those of 2012. The adverse pregnancy outcomes amongst women lacking treatment were higher than those treated with standard care.
Despite the prevalence of syphilis in Suzhou city being lower than high-epidemic cities in China, the Jiangsu province was highly afflicted due to the large migrant population. Migrants are attracted by economic development. These relationships should be assessed in more detail in future studies.
This was the first study investigating the prevalence of syphilis and its characteristics amongst pregnant women in Suzhou, There were several limitations. Firstly, we could not compare pregnancy outcomes between healthy women and women with syphilis due to the lack of data availability. Secondly, the influence of a partner’s infection status on infant health was not assessed due to limited information. Finally, only selected adverse pregnancy outcomes were recorded in the PMTCT system, meaning the effectiveness of PMTCT was not fully evaluated.
In summary, we demonstrate that full-course and adequate treatment improves pregnancy outcomes and infant health. The priority of PMTCT of syphilis is to improve early screening coverage and the compliance of pregnant women with medication in Suzhou city, particularly in the migrant population.
Methods
Data collection
Data were extracted from the municipal PMTCT system from 2012 to 2018. According to the requirements of the PMTCT program, syphilis counseling and testing were combined with routine prenatal healthcare. All pregnant women underwent syphilis counseling and testing upon their initial prenatal healthcare appointment. Positive results in syphilis rapid plasma regain (RPR)/toluidine red unheated serum test (TRUST) and treponemal pallidum particle agglutination (TPPA)/enzyme linked immunosorbent assay (ELISA) tests led to a diagnosis of maternal syphilis infection. Syphilis infected women were provided free penicillin in the first and the third trimester, respectively. All pregnant women were screened prior to delivery. For children born to syphilis infected women, syphilis screening and preventive treatment were performed if the mothers failed to receive two courses of full-time penicillin during the first and third trimester of pregnancy, or if their mothers received full-time penicillin treatment during pregnancy. Newborns maintained reactive TRUST or RPR serum titers that were 4-times lower than the mothers prior to delivery. Exposed children were followed up every three months until a syphilis diagnosis was excluded. Information on infected pregnant women, pregnancy outcomes and follow ups of exposed children were recorded in the PMTCT system.
Statistical analysis
The database was exported in Excel and analyzed using SPSS 17.0 software (Chicago Illinois, USA). Demographic characteristics of syphilis infected women were described. Categorical variables are presented as numbers and frequencies. Statistically significant differences between the groups were evaluated using the χ2-test or Fisher’s exact test as appropriate. P < 0.05 was considered statistically significant.
Ethical considerations
This study was approved by the Ethics committee of Suzhou Municipal Hospital. All infected mothers were required to complete a routine questionnaire upon receiving syphilis screening and testing at their first antenatal care or delivery. Informed consent was obtained from syphilis infected mothers. Prenatal syphilis screening and testing processes followed the guidelines and regulations of the integrated National Preventing Mother to Child Transmission Program of HIV, Syphilis and Hepatitis B. In the final database, only mothers and infant numbers were listed. All personal information was kept confidential.
Author contributions
Tian Gong: collecting data, data analysis, paper writing and quality control; Yan Shao: collecting data; Juning Liu: collecting data; Qianlan Wu: collecting data; Rong Xu: data analysis; Li Sun: data analysis; Xiaoju Peng: data analysis.
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gomez GB, et al. Untreated maternal syphilis and adverse outcomes of pregnancy: a systematic review and meta-analysis. Bull World Health Organ. 2013;91:217. doi: 10.2471/BLT.12.107623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Woods CR. Congenital syphilis-persisting pestilence. Pediatr Infect Dis J. 2009;28:536. doi: 10.1097/INF.0b013e3181ac8a69. [DOI] [PubMed] [Google Scholar]
- 3.Korenromp EL, et al. Global burden of maternal and congenital syphilis and associated adverse birth outcomes-Estimates for 2016 and progress since 2012. Plos One. 2019;14:e211720. doi: 10.1371/journal.pone.0211720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Saweri OP, et al. Cost and cost-effectiveness of point-of-care testing and treatment for sexually transmitted and genital infections in pregnancy in low-income and middle-income countries: a systematic review protocol. BMJ Open. 2019;9:e29945. doi: 10.1136/bmjopen-2019-029945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Milanez H. Syphilis in Pregnancy and Congenital Syphilis: Why Can We not yet Face This Problem? Rev Bras Ginecol Obstet. 2016;38:425. doi: 10.1055/s-0036-1593603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Organization, W. H., (World Health Organization, Geneva, 2016).
- 7.Kahn JG, et al. The cost and cost-effectiveness of scaling up screening and treatment of syphilis in pregnancy: a model. Plos One. 2014;9:e87510. doi: 10.1371/journal.pone.0087510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Organization, W. H., Elimination of mother-to-child transmission of HIV and syphilis (second edition) (2017).
- 9.Zhang XH, Xu J, Chen DQ, Guo LF, Qiu LQ. Effectiveness of treatment to improve pregnancy outcomes among women with syphilis in Zhejiang Province, China. Sex Transm Infect. 2016;92:537. doi: 10.1136/sextrans-2015-052363. [DOI] [PubMed] [Google Scholar]
- 10.Matteelli A, et al. Congenital syphilis in Italy. Sex Transm Infect. 2007;83:590. doi: 10.1136/sti.2007.025338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Newman L, et al. Global estimates of syphilis in pregnancy and associated adverse outcomes: analysis of multinational antenatal surveillance data. Plos Med. 2013;10:e1001396. doi: 10.1371/journal.pmed.1001396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jiang N, Gong X, Yue X. Estimation of syphilis epidemic through application of workbook method among populations aged from 15 to 49 years old in China in 2011. Zhonghua Yu Fang Yi Xue Za Zhi. 2014;48:693. [PubMed] [Google Scholar]
- 13.Arnesen L, Martinez G, Mainero L, Serruya S, Duran P. Gestational syphilis and stillbirth in Latin America and the Caribbean. Int J Gynaecol Obstet. 2015;128:241. doi: 10.1016/j.ijgo.2014.09.017. [DOI] [PubMed] [Google Scholar]
- 14.Archana BR, et al. Maternal and congenital syphilis in Karnataka, India. Southeast Asian J Trop Med Public Health. 2014;45:430. [PubMed] [Google Scholar]
- 15.Peeling RW, et al. Syphilis. Nat Rev Dis Primers. 2017;3:17073. doi: 10.1038/nrdp.2017.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fiumara NJ. Congenital syphilis in Massachusetts. N Engl J Med. 1951;245:634. doi: 10.1056/NEJM195110252451702. [DOI] [PubMed] [Google Scholar]
- 17.Watson-Jones D, et al. Syphilis in pregnancy in Tanzania. I. Impact of maternal syphilis on outcome of pregnancy. J Infect Dis. 2002;186:940. doi: 10.1086/342952. [DOI] [PubMed] [Google Scholar]
- 18.Qin J, et al. Reported estimates of adverse pregnancy outcomes among women with and without syphilis: a systematic review and meta-analysis. Plos One. 2014;9:e102203. doi: 10.1371/journal.pone.0102203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Watson-Jones D, et al. Syphilis in pregnancy in Tanzania. II. The effectiveness of antenatal syphilis screening and single-dose benzathine penicillin treatment for the prevention of adverse pregnancy outcomes. J Infect Dis. 2002;186:948. doi: 10.1086/342951. [DOI] [PubMed] [Google Scholar]
- 20.Terris-Prestholt F, et al. Is antenatal syphilis screening still cost effective in sub-Saharan Africa. SEX TRANSM INFECT. 2003;79:375. doi: 10.1136/sti.79.5.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wallace HE, Isitt CE, Broomhall HM, Perry AE, Wilson JD. Adverse pregnancy outcomes following syphilis treatment in pregnancy in the UK. Int J Std Aids. 2016;27:1108. doi: 10.1177/0956462415609862. [DOI] [PubMed] [Google Scholar]
- 22.Oliveira LR, et al. Evaluation of preventative and control measures for congenital syphilis in State of Mato Grosso. Rev Soc Bras Med Trop. 2014;47:334. doi: 10.1590/0037-8682-0030-2014. [DOI] [PubMed] [Google Scholar]
- 23.Arnesen L, Serruya S, Duran P. Gestational syphilis and stillbirth in the Americas: a systematic review and meta-analysis. Rev Panam Salud Publica. 2015;37:422. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.


