Abstract
OBJECTIVE
Improving neighborhood walkability has been proposed as a policy intervention to reduce obesity. The objective of this study was to evaluate longitudinal relationships between neighborhood walkability and body weight among adults living in large urban areas.
METHODS
In this retrospective longitudinal study of United States (U.S.) military veterans using Department of Veterans Affairs (VA) healthcare, we linked VA clinical and administrative data (2007-2014) to environmental measures constructed from public (2006-2014) and proprietary (2008-2014) sources and used linear regression models with person fixed effects to estimate associations between walkability and body mass index (BMI) among 758,434 men and 70,319 women aged 20-80 years in 2009-2014.
RESULTS
Neighborhood walkability was associated with small reductions in BMI. Effects were most pronounced among men ages 30-49 and 50-64. For women, differences were largest in the two youngest age groups, 20-29 and 30-49, though only estimates for all women combined were statistically significant. For women 30-49 years effect sizes grew when we limited the sample to those who remained in the same neighborhood during the entire follow-up period.
CONCLUSIONS
Investments in the built environment to improve walkability may be a useful strategy for weight maintenance in some segments of the adult population.
Keywords: Databases, Environmental Factors, Physical Activity, Weight Control
INTRODUCTION
Overweight and obesity affect more than 70% of U.S. adults and together are a leading cause of death in the U.S. and worldwide.1 Reducing the prevalence of overweight and obesity would have substantial public health benefits. Unfortunately, there are very few interventions or policy instruments that seem to reliably reduce population levels of overweight and obesity. Many jurisdictions are pursuing initiatives designed to reduce obesity by encouraging physical activity. One idea is to improve neighborhood walkability, that is, features of the built environment that influence residents’ transportation choices or propensity to walk including density (people, housing), destinations that people want to access in their daily lives (e.g., shopping, jobs), and a street network design (e.g., intersections) that provides potential pedestrian travel paths between destinations.2 To increase walkability, cities might build well-connected street networks and/or adopt mixed-use zoning policies that help bring shopping, dining, and entertainment destinations close to where people live. These strategies are fueled partly by research showing that people living in more walkable communities tend to be more physically active and weigh less.3–11 But the results in the literature are inconsistent.12–16 The correlation between neighborhood walkability and body weight seems to be different for men and women, and for older and younger people.3,5,6,17,18 And some studies have found no relationship between neighborhood walkability and body weight.19–21
The limitations in the existing literature make it hard to draw conclusions about the likely effects of policies aimed at improving walkability. Most studies have been conducted at local or regional scales such as within a single metropolitan area.3,5,6,11 This limits the generalizability of the findings. Few studies include healthcare data, such as clinical measurements, diagnoses, and healthcare use and so are subject to confounding related to those factors. Most studies rely on a cross-sectional study design, which further limits causal inference. Residential self-selection bias, in which people choose where to live in part based on lifestyle preferences that are correlated with overweight status, is an important threat to the validity of the cross-sectional study designs that are common in the literature.15,22–24
The Weight and Veterans’ Environments Study (WAVES) is a retrospective longitudinal study of over 3.2 million U.S. military veterans.25 WAVES leverages rich Department of Veterans Affairs (VA) healthcare data, linked to repeated measures of individual residential environments. The veterans in the WAVES database can be followed for up to 6 years (2009-2014), and they live in diverse geographic areas across the country. In this study, we exploit the longitudinal WAVES data to estimate the effects of changes in neighborhood walkability on body weight among adults living in counties classified as large central metropolitan areas.
METHODS
Sample
The study sample was derived from the larger WAVES cohort of veterans aged 20-80 years living in the continental U.S. and receiving VA primary healthcare services between 2009 and 2014. Details regarding eligibility and exclusion criteria are available elsewhere.25 The male (N=758,434) and female (N=70,319) samples for this analysis were limited to those who lived in counties classified by the National Center for Health Statistics Urban-Rural Classification Scheme as large central metropolitan (the most highly urban counties) in at least one year during the study period.26
Measures
We linked VA clinical and administrative data (2007-2014) to environmental measures constructed from public (American Community Survey (ACS), 2006-2014) and proprietary sources (NAVTEQ and TeleAtlas, 2010 and 2014, and InfoUSA and Dun and Bradstreet, 2008-2014). The VA Corporate Data Warehouse and the VA/CMS data repository (Medicare inpatient and outpatient claims data) provided subjects’ demographic, residential location, healthcare utilization, and diagnosis information. We constructed a neighborhood walkability index using NAVTEQ (street intersections) and the US Census Bureau (population, housing units, land area, jobs in certain business types) data. We measured other environmental factors using NAVTEQ (food and parks, sociodemographics), TeleAtlas (parks), InfoUSA (commercial fitness facilities, supermarkets, grocery stores, convenience stores), Dun and Bradstreet (fast-food restaurants); and the American Community Survey (5-year estimates; census tract populations and housing characteristics). To assign environmental information to each individual, we partitioned the continental U.S. into 30 × 30 meter cells, computed environmental measures within various distances of each cell, and then assigned the environmental measurements to each person based on the cell in which their geocoded home address was located (recorded in VA data as of October 1 each year).25,27
Study outcome.
Body mass index (BMI, weight in kilograms/height in meters2) was calculated using height and weight measurements taken during patient encounters, as previously described.25,27
Neighborhood walkability.
We use a person-specific index of the level of walkability within a 1-mile buffer around the person’s home address. The index comprises five items that summarize four environmental features that have been associated with walking in previous research: population density, housing unit density, walking destinations, and street connectivity.28,29 Thus, the index reflects three “Ds” recognized as influences on walking or transportation choice: density, design, and destination accessibility.30 We measured population and housing unit density (number of people and housing units per square mile) using ACS 5-year block group estimates. We used the number of jobs in business sectors whose community locations present walking destinations as a walking destinations proxy measure: retail (NAICS sector 44-45); accommodation and food service (NAICS sector 72); and arts, entertainment, and recreation (NAICS sector 71).29 These data, from the Local Employer-Household Dynamics (LEHD) Origin-Destination Employment Statistics databases, have the distinct advantage of being available for locations nationwide and, while not a direct measure of the number of businesses or their land area, job numbers within a defined area at least reflect the amount of activity in relevant business sectors. We counted the jobs for businesses located within the 1-mile buffer. We measured street connectivity as the number of intersections in the buffer, and the percentage of intersections that were at least 4-way. We calculated z-scores for each of the index components, normalizing the values over the study sample and all observations, 2009-2014. Each person’s walkability index value was the average of the five z-scores. We calculated walkability index scores for each year and created a 4-category variable, representing quartiles of the distribution with the least walkable areas (lowest walkability index scores) in Quartile 1 and the most walkable areas (highest walkability index scores) in Quartile 4. Table S1 shows means and standard deviations for index components in Quartiles 1-4 for each year, 2009-2014. Table S2 shows summary statistics for within-person changes over time in walkability index components. Individuals experienced appreciable changes over time in all components of the built environment that comprise the walkability index. For example, on average, highest and lowest intersection density within individuals’ 1-mile buffers differed over time by over 19%. And highest and lowest numbers of jobs differed by over 32%, on average.
Covariates.
Individual-level covariates included age at baseline; race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, Other, Unknown); marital status (married, separated/divorced, widowed, single, unknown); healthcare use (number of primary and specialty care outpatient visits and inpatient days in the calendar year), and VA priority group.25,31 Priority group designations reflect the factors on which VA enrollment eligibility is based (e.g., service connected disability, income) and determine copayment obligations. We collapsed the eight groups to three groups reflecting services for which the veteran pays a copayment: all, some, or none. Marital status and healthcare utilization variables were treated as time-varying variables. Area-level time-varying covariates included the number of parks, commercial fitness facilities, supermarkets, grocery stores, fast food restaurants, and convenience stores within 1 mile of home; census division; census tract poverty rate; and census tract median household income.25
Statistical Analysis
To estimate the effect of walkability on BMI, we fit linear regression models of BMI on the walkability measures, covariates, year fixed effects, and person fixed effects. The walkability measure is entered as a set of dummy variables for Quartiles 2-4. The reference group is people living in Quartile 1 areas, the least walkable. In the person fixed-effects model, the effects of walkability are identified using only variation that comes from within-person changes in neighborhood walkability. Within-person variation in walkability may arise because the person’s neighborhood becomes more or less walkable or because a person migrates to a new neighborhood with different walkability. Estimates from fixed-effects models resolve concerns about omitted variable bias for a large class of time-invariant unmeasured characteristics that might differentiate people who live in more vs less walkable neighborhoods. However, the fixed-effects models could still be biased if there are unmeasured covariates that change over time, affect a person’s BMI, and are correlated with within-person changes in neighborhood walkability. For example, a person might retire from the workforce and decide to focus more on living a healthy life. She might move to a more walkable neighborhood, increase her physical activity, and lose some weight. Our fixed-effects model would attribute the effects of her lifestyle change on BMI to the walkability of the new neighborhood. To address this problem, we estimated the fixed-effects models in a sample limited to people who lived in the same residential location during the entire study period. In these non-migrant models, within-person variation in walkability comes from neighborhood changes that people have little control over, strengthening inferences about the causal effects of walkability on BMI. Note that the interpretation of the coefficients resulting from the within-person identification strategy is unchanged; it is the effect of living in a specific walkability category on BMI relative to the reference category.
We estimated separate models for men and women mainly because the male and female veteran populations using VA healthcare differ considerably in their demographic and health characteristics with little overlap in some of those characteristics. To better understand the BMI-walkability relationship within age as well as gender cohorts, we estimated separate models for age-group subsamples: 20-29 years, 30-49 years, 50-64 years, and 65 years and older, with the latter group split into 65-74 years and 75 years and older for men. Results of studies in gender- and age-specific subpopulations (e.g., young adults, elderly) suggest that sensitivity to walkability may not be constant across cohorts or the life course, though findings have been inconsistent.32–36 Plausibly, older populations may suffer from a range of health conditions that make walking difficult and that may make their BMI less responsive to neighborhood conditions. Therefore, we might expect larger effects in younger and middle aged groups than in older groups.
To assess the sensitivity of our results to the scale at which we measured walkability, we also estimated models with walkability measured within a 1/4-mile buffer rather than a 1-mile buffer. We computed standard errors using a cluster robust variance matrix that allowed for dependence among observations on people who lived in the same county at baseline. We analyzed the data in 2017 and 2018 using Stata version 14. This study was approved by the institutional review boards of the University of Illinois at Chicago and Edward Hines, Jr. VA Hospital.
RESULTS
Table 1 shows the characteristics of the study sample and their residential environments (see Table S3 for age group breakdown). Among men, mean age is 58.1 years (SD 13.8), 28.3% are non-Hispanic Black, 52.9% are non-Hispanic White, and 7.4% are Hispanic. Among women, mean age is 44.8 years (SD 13.4), 36.2% are non-Hispanic Black, 43.8% are non-Hispanic White and 8.0% are Hispanic.
Table 1.
Cohort Characteristics at Baseline: U.S. Urban Areas, 2009 – 2014
| Variable | Men | Women | |||
|---|---|---|---|---|---|
| N | % | N | % | ||
| Age | mean(SD) | 58.1 | (13.8) | 44.8 | (13.4) |
| Age group | 20-29 | 40,846 | 5.4 | 11,640 | 16.6 |
| 30-49 | 131,693 | 17.4 | 31,169 | 44.3 | |
| 50-64 | 331,216 | 43.7 | 22,520 | 32.0 | |
| 65-74 | 165,176 | 21.8 | 4,990 | 7.1 | |
| 75+ | 89,503 | 11.8 | |||
| Race/ethnicity | Non-Hispanic white | 401,115 | 52.9 | 30,792 | 43.8 |
| Non-Hispanic black | 214,697 | 28.3 | 25,471 | 36.2 | |
| Hispanic | 56,356 | 7.4 | 5,619 | 8.0 | |
| Other | 22,935 | 3.0 | 2,755 | 3.9 | |
| Unknown | 63,331 | 8.4 | 5,682 | 8.1 | |
| Marital status | Married | 338,650 | 44.7 | 18,531 | 26.4 |
| Separated/divorced | 208,814 | 27.5 | 23,372 | 33.2 | |
| Widowed | 29,387 | 3.9 | 2,269 | 3.2 | |
| Single | 174,572 | 23.0 | 25,095 | 35.7 | |
| Unknown | 7,011 | 0.9 | 1,052 | 1.5 | |
| Census division | New England | 19,850 | 2.6 | 1,024 | 1.5 |
| Middle Atlantic | 81,523 | 10.8 | 5,695 | 8.1 | |
| East North Central | 108,781 | 14.3 | 7,970 | 11.3 | |
| West North Central | 25,875 | 3.4 | 1,779 | 2.5 | |
| South Atlantic | 127,123 | 16.8 | 15,789 | 22.5 | |
| East South Central | 38,359 | 5.1 | 3,803 | 5.4 | |
| West South Central | 116,352 | 15.3 | 13,246 | 18.8 | |
| Mountain | 77,233 | 10.2 | 7,159 | 10.2 | |
| Pacific | 163,338 | 21.5 | 13,854 | 19.7 | |
| Census tract median household income (thousands) | 2.5 - 29.5 | 94,248 | 12.4 | 7,256 | 10.3 |
| 29.5 - 36.0 | 82,788 | 10.9 | 7,401 | 10.5 | |
| 36.0 - 41.2 | 74,747 | 9.9 | 7,151 | 10.2 | |
| 41.3 - 45.9 | 69,550 | 9.2 | 7,025 | 10.0 | |
| 45.9 - 50.8 | 72,503 | 9.6 | 7,355 | 10.5 | |
| 50.8 - 55.8 | 74,967 | 9.9 | 7,376 | 10.5 | |
| 55.8 - 62.2 | 76,612 | 10.1 | 7,753 | 11.0 | |
| 62.2 - 70.4 | 81,732 | 10.8 | 7,846 | 11.2 | |
| 70.4 - 83.8 | 78,756 | 10.4 | 7,194 | 10.2 | |
| 83.8 - 250 | 52,531 | 6.9 | 3,962 | 5.6 | |
| Census tract percent below federal poverty threshold | 0.0 - 3.7 | 63,935 | 8.4 | 5,104 | 7.3 |
| 3.7 - 5.7 | 82,600 | 10.9 | 7,055 | 10.0 | |
| 5.7 - 7.6 | 77,326 | 10.2 | 6,974 | 9.9 | |
| 7.6 - 9.6 | 76,535 | 10.1 | 7,434 | 10.6 | |
| 9.6 - 11.9 | 71,162 | 9.4 | 7,163 | 10.2 | |
| 11.9 - 14.5 | 68,919 | 9.1 | 7,374 | 10.5 | |
| 14.5 - 18.0 | 72,199 | 9.5 | 7,153 | 10.2 | |
| 18.0 - 22.8 | 76,919 | 10.1 | 7,579 | 10.8 | |
| 22.8 - 30.9 | 84,043 | 11.1 | 7,673 | 10.9 | |
| 30.9 - 100 | 84,796 | 11.2 | 6,810 | 9.7 | |
| Health conditions | Diabetes | 184,113 | 24.3 | 6,644 | 9.5 |
| Hypertension | 393,853 | 51.9 | 18,105 | 25.8 | |
| Stroke/CVD | 39,884 | 5.3 | 1,290 | 1.8 | |
| Breast cancer | 209 | 0.0 | 1,233 | 1.8 | |
| Colon cancer | 6,303 | 0.8 | 160 | 0.2 | |
| Hyperlipidemia | 292,877 | 38.6 | 13,387 | 19.0 | |
| Osteoarthritis | 94,374 | 12.4 | 6,387 | 9.1 | |
| CHF | 42,459 | 5.6 | 958 | 1.4 | |
| MI | 21,098 | 2.8 | 408 | 0.6 | |
| Depression | 141,178 | 18.6 | 21,150 | 30.1 | |
| VA priority groupa | No copayments | 204,624 | 27.0 | 24,595 | 35.0 |
| Some copayments | 420,160 | 55.4 | 38,779 | 55.1 | |
| All copayments | 133,650 | 17.6 | 6,945 | 9.9 | |
| Primary care encounters | mean(SD) | 3.19 | 2.8 | 3.459 | 2.9 |
| Specialty care encounters | mean(SD) | 6.14 | 9.3 | 6.837 | 9.8 |
| Days in hospital | mean(SD) | 1.75 | 8.2 | 1.043 | 6.2 |
| Parks | 0 | 106,236 | 14.0 | 12,232 | 17.4 |
| 1-2 | 224,879 | 29.7 | 22,462 | 31.9 | |
| 3-4 | 191,438 | 25.2 | 16,841 | 23.9 | |
| 5+ | 235,881 | 31.1 | 18,784 | 26.7 | |
| Commercial fitness facilities | 0 | 99,311 | 13.1 | 9,876 | 14.0 |
| 1-2 | 191,386 | 25.2 | 18,277 | 25.9 | |
| 3-6 | 258,866 | 34.1 | 23,882 | 33.9 | |
| 7+ | 208,871 | 27.5 | 18,284 | 26.0 | |
| Supermarkets | 0 | 217,133 | 28.6 | 21,647 | 30.8 |
| 1 | 199,530 | 26.3 | 18,858 | 26.8 | |
| 2 | 143,546 | 18.9 | 13,128 | 18.7 | |
| 3+ | 198,225 | 26.1 | 16,686 | 23.7 | |
| Convenience stores | 0-2 | 198,983 | 26.2 | 19,493 | 27.7 |
| 3-5 | 188,655 | 24.9 | 18,551 | 26.4 | |
| 6-9 | 185,672 | 24.5 | 17,099 | 24.3 | |
| 10+ | 185,124 | 24.4 | 15,176 | 21.6 | |
| Grocery stores | 0 | 239,204 | 31.5 | 23,788 | 33.8 |
| 1 | 129,582 | 17.1 | 12,764 | 18.2 | |
| 2-5 | 202,555 | 26.7 | 18,990 | 27.0 | |
| 6+ | 187,093 | 24.7 | 14,777 | 21.0 | |
| Fast food restaurants | 0-4 | 192,688 | 25.4 | 18,762 | 26.7 |
| 5-10 | 188,391 | 24.8 | 17,777 | 25.3 | |
| 11-18 | 181,939 | 23.9 | 17,059 | 24.3 | |
| 19+ | 195,416 | 25.8 | 16,721 | 23.8 | |
| Walkability | Quartile 1 | 195,543 | 25.8 | 19,685 | 27.9 |
| Quartile 2 | 187,975 | 24.8 | 19,267 | 27.4 | |
| Quartile 3 | 184,948 | 24.4 | 16,647 | 23.7 | |
| Quartile 4 | 189,968 | 25.0 | 14,720 | 20.9 | |
Priority groups: no copayments, 1, 4; some copayments 2, 3, 5, 6; all copayments 7, 831
Table 2 shows results from the regression models. Men living in the most walkable (Quartile-4) areas had lower BMI than those in the least walkable (Quartile-1) areas (all ages combined, −0.059 [CI95 −0.087,−0.031] kg/m2). The BMI differences associated with Quartile-4 areas were driven by the 30-49 and 50-64 year age groups; men in those age groups who lived in Quartile-4 areas weighed, on average, 0.067 [CI95 −0.117,−0.016] and 0.067 [CI95 −0.106,−0.028] kg/m2 less, respectively, than men living in Quartile-1 areas. There were no statistically significant differences in BMI associated with area walkability among men 20-29 years, 65-74 years, or 75 years and older.
Table 2.
Estimated BMI Differences between Individuals Living in Walkability Quartile−2, −3, and −4 Areas and those Living in Quartile-1 Areas: U.S. Large Urban Areas, 2009-2014
| MEN | WOMEN | ||||||
|---|---|---|---|---|---|---|---|
| Quartile 2 | Quartile 3 | Quartile 4 | Quartile 2 | Quartile 3 | Quartile 4 | ||
| b [95% CI] | b [95% CI] | b [95% CI] | b [95% CI] | b [95% CI] | b [95% CI] | ||
| All | −0.001 [−0.017, 0.015] | −0.017 [−0.038, 0.003] | −0.059*** [−0.087, −0.031] | All | 0.017 [−0.029, 0.063] | −0.041 [−0.100, 0.018] | −0.097* [−0.171, −0.022] |
| 20-29 Years | −0.020 [−0.080, 0.041] | −0.040 [−0.112, 0.031] | −0.085 [−0.179, 0.010] | 20-29 Years | 0.031 [−0.081,0.143] | −0.000 [−0.123, 0.124] | −0.190 [−0.403, 0.022] |
| 30-49 Years | −0.013 [−0.048, 0.021] | −0.017 [−0.063, 0.030] | −0.067** [−0.117, −0.016] | 30-49 Years | −0.049 [−0.121, 0.024] | −0.104* [−0.195, −0.014] | −0.087 [−0.215, 0.041] |
| 50-64 Years | −0.001 [−0.023, 0.022] | −0.024 [−0.053, 0.005] | −0.067** [−0.106, −0.028] | 50-64 Years | 0.101* [0.021, 0.181] | 0.006 [−0.113, 0.126] | −0.064 [−0.198, 0.070] |
| 65-74 Years | 0.003 [−0.020, 0.026] | 0.000 [−0.036, 0.036] | −0.018 [−0.069, 0.033] | >=65 Years | 0.108 [−0.098, 0.313] | 0.117 [−0.140, 0.374] | 0.019 [−0.353, 0.391] |
| >=75 Years | 0.032 [−0.015, 0.080] | 0.015 [−0.042, 0.071] | −0.031 [−0.103, 0.041] | ||||
Note: Boldface indicates p-value < 0.05.
p<0.05,
p<0.01,
p<0.001.
Covariates included age, race/ethnicity, marital status, census division, census tract percent of the population living below the federal poverty threshold, census tract median household income, VA priority group, number of primary care encounters, number of specialty care encounters, number of inpatient days, food outlets within 1 mile (supermarkets, grocery stores, convenience stores, fast-food restaurants), parks within 1 mile, commercial fitness facilities within 1 mile. Models included year and person fixed effects. Area walkability was measured within 1 mile of home.
CI, Confidence Interval
Figure 1 shows differences in average predicted BMI among subgroups of men defined by area walkability and age, based on the regression model estimates. In men younger than 65 years, average BMI tends to decrease with area walkability, though only the Quartile-4 coefficients (for men 30-49 years and 50-64 years) reach statistical significance. Further, the differences are very small and not clinically meaningful. For example, the model implies that a man 30-49 years old who is 70 inches tall (average height) would weigh about 0.47 pounds less if he lived in an area with the highest rather than the lowest levels of walkability, a weight difference of about 0.2%. In models with samples limited to non-migrants (Table S4), none of the walkability quartile coefficient estimates reached statistical significance. Results of models with samples limited to migrants showed results substantively identical to those for the full sample.
Figure 1.
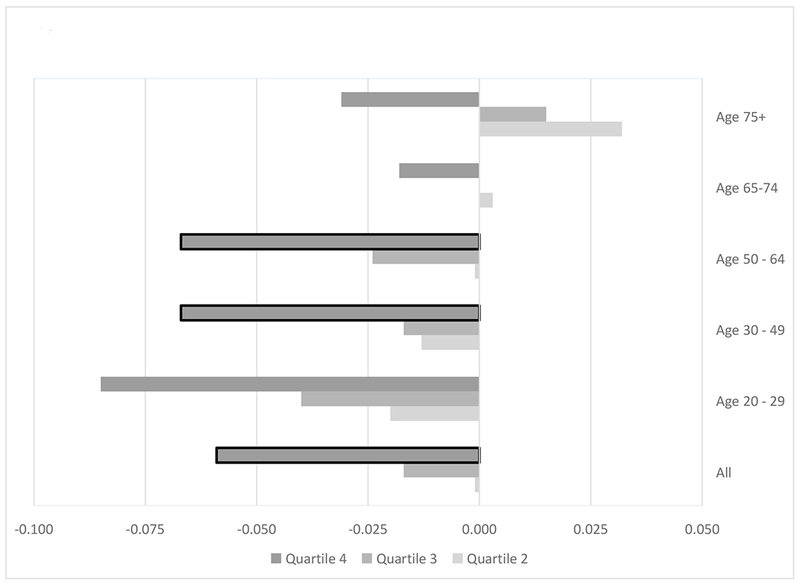
Differences in Predicted BMI According to Area Walkability, Men: U.S. Urban Areas, 2009-2014
Regression model results for women (Table 2, right panel) show that women living in Quartile-4 areas had lower BMI than those in Quartile-1 areas (all ages combined: −0.097, [CI95 −0.171,−0.022] kg/m2). Women age 30-49 years living in Quartile-3 areas had a lower estimated BMI [−0.104, CI95 −0.195,−0.014] kg/m2 and women age 50-64 in Quartile-2 areas had higher estimated BMI [0.101, CI95 0.021, 0.181] kg/m2 than their counterparts living in Quartile-1 areas. There were no statistically significant differences in BMI associated with area walkability among women 20-29 or 65+ years.
Figure 2 shows differences in average predicted BMI among subgroups of women defined by area walkability and age, based on regression model estimates. The graph illustrates that average BMI tends to decrease with area walkability among younger women. Among women 50 years and older, results are different. For women 50-64 years, average predicted BMI among those in Quartile-2 areas was higher than their counterparts in the lowest walkability areas. But there were no differences in predicted BMI among those in Quartile-3 and Quartile-4 compared to those in Quartile-1 areas. For women 65 years and older, average predicted BMI was higher among those in Quartile-2, Quartile-3, and Quartile-4 areas compared to women in Quartile-1 areas but none of those differences were statistically significant. Overall, even when statistically significant, differences in predicted BMI are small in magnitude. The model implies that a 30-49 year old woman who is 65 inches tall (average height in our sample), would weigh about 0.52 pounds less if she lived in a Quartile-4 rather than a Quartile-1 area, a weight difference of about 0.3%. In models with samples limited to non-migrants (Table S4), there were no statistically significant BMI differences associated with area walkability among all women combined. Among 30-49 year old women, however, average BMI was 0.136 kg/m2 lower [CI95 −0.243,−0.029] and 0.156 kg/m2 lower [CI95 −0.292,−0.020] in Quartile-2 and Quartile-3 compared to Quartile-1 areas, respectively. Among women 50-64 years and 65 years and older, results were in the opposite direction, though only one of the estimated BMI differences reached statistical significance (>=65 years, Quartile-3 compared to Quartile-1 areas: 0.322 [CI95 0.023, 0.620] kg/m2). Results of models with samples limited to migrants showed results very similar to those for the full sample, though with fewer statistically significant coefficients.
Figure 2.
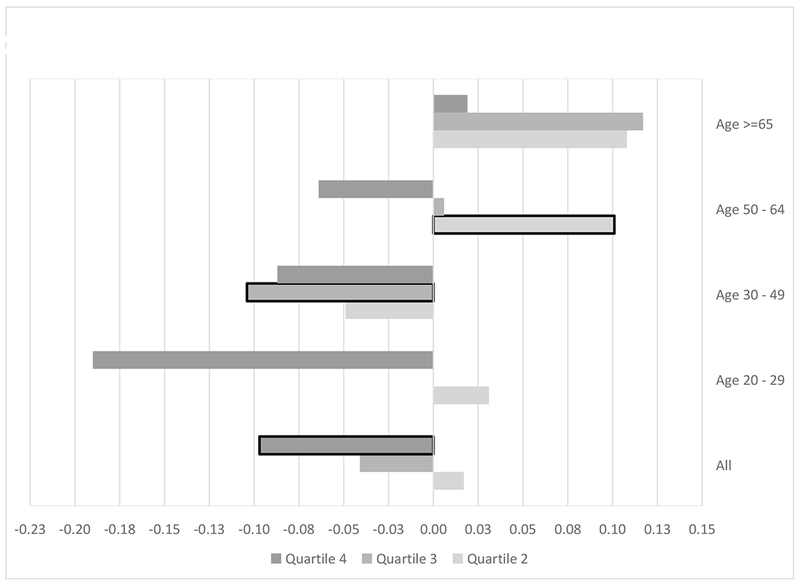
Differences in Predicted BMI According to Area Walkability, Women: U.S. Urban Areas, 2009-2014
For both men and women, results from models using walkability measured within 1/4-mile of home were substantively identical to those described above (Table S5). We also estimated models that excluded food outlets as covariates; patterns in estimated walkability associations were very similar to those presented here.
DISCUSSION
We found that neighborhood walkability was associated with small reductions in BMI, among men and women living in large urban areas, after adjusting for a large set of observed and time-invariant unmeasured factors. The effects of walkability on BMI were most pronounced among men ages 30-49 and 50-64. For women, differences were largest in the two youngest age groups, 20-29 and 30-49, though only estimates for all women combined were statistically significant. The magnitude of the walkability effects was small and in most cases we were unable to reject the hypothesis of no BMI difference. For women 30-49 years the effects grew when we limited the sample to non-migrants, suggesting that models based on changes that arise from migration may suffer from negative selection bias. Altogether, under the assumption that any time-varying unobserved factors associated with walkability group were unrelated to changes in body weight, our results provide evidence that supports a small causal effect of neighborhood walkability on BMI among men and women, at least in some age groups. We found little or no evidence of salutary effects of walkability on BMI among men 65 years and older or women 50 years and older.
While the BMI advantage of living in a more walkable neighborhood appears small in magnitude, it may be important from the perspective of curbing weight gain. On average, men and women gained weight during the 6-year study period. Given recent evidence demonstrating that risk for mortality and disability associated with cardiovascular disease and diabetes increases incrementally with BMI,37,38 even small reductions in weight gain, particularly if they accumulate over time, may have public health significance.
This study adds to a limited body of research using longitudinal data and more robust research designs to study relationships between neighborhood walkability and BMI.18,19,22,39‘41 Results of those studies have been mixed with few demonstrating relationships in the hypothesized direction. For example, Wasfi et al. (2016) used biannual survey data from Canada’s National Population Health Survey to study relationships between neighborhood Walk Score and BMI among 2,943 urban-dwelling adults age 18-55 years (up to 7 cycles and 12 years of follow-up).18,42,43 They found relationships in the expected direction for men (a decrease in BMI trajectory of 1 kg/m2 for men who moved to a more walkable neighborhood compared to those who did not move) and no effects for women, consistent with our study. Hirsch and colleagues (2014) also used fixed-effects models to study relationships between Street Smart Walk Score and BMI among 701 participants age 48-87 years in the Multi-Ethnic Study of Atherosclerosis (MESA) who moved between two waves (2004-2012).39 They found a 10-point increase in Walk Score was associated with 0.06 kg/m2 decrease in body mass. The authors did not report on gender differences.
Our study has several limitations. The walkability measure we use is not able to capture differences in other factors that might affect the desire or ability to walk: two areas with equal walkability index values may differ in terms of quality of walking areas, safety, or aesthetics. Availability of public transport or car ownership may be associated with walkability and BMI, and our study is not able to control for such factors. Also, while we controlled for area income, including changes over time, we were unable to account for differences in individual income changes over time. Given that income is strongly associated with physical activity and body weight, the absence of individual income information could have biased our results if individuals in different walkability areas differed in amount or direction of income change over time. We used successive ACS 5-year estimates of census tract median household income and poverty rate and of population and housing unit density in the walkability index. Because successive 5-year estimates (e.g., 2009-2013 and 2010-2014) are constructed from data that overlap, our use of these measures underestimates year-to-year change in walkability in areas undergoing rapid sociodemographic change. We think this would likely have the effect of biasing our estimates of walkability-BMI relationships toward the null since the precision of our estimates is dependent on change in the “exposure”, walkability. The strength of the 5-year estimates is they provide statistically precise measures for small areas. 1-year estimates are available only for areas with populations of at least 65,000 people and so were not feasible for use in this study. Generalizability may be affected by differences between the population of veterans using VA health care and the general U.S. adult population. In particular, some health conditions such as ambulatory difficulty that may affect the walkability-BMI relationship are more prevalent in the VA population. Recent data from the Behavioral Risk Factor Surveillance Survey found 13.4% and 13.1% mobility disability prevalence among veterans and non-veterans, respectively, though comparisons are difficult to make since veterans’ age distribution is skewed older than that of the general population.44,45 We might expect BMI among individuals with mobility disability to be less sensitive to area walkability. In that case, our estimates of walkability effects might be considered conservative.
The study also has several strengths. The data allow us to analyze repeated measures of both BMI and neighborhood walkability for the same individuals over time, which makes it possible to distinguish temporal shifts in walkability due to neighborhood change from those due to moves to new neighborhoods. Those advantages facilitated our use of statistical models that were robust to multiple sources of threat to internal validity. Our study also includes clinical measures of BMI (rather than self-reports) and objective measures of exposure to walkable neighborhoods. Our exposure measure (walkability) was precisely calculated for each individual rather than assigned based on pre-existing administrative units. Finally, our study controls for access to care and time-invariant health status and the population we study covers a diverse set of urban areas across the country.
CONCLUSIONS
This study found some evidence supporting a small causal effect of neighborhood walkability on BMI in both men and women in some age groups. Thus, investments in the built environment to improve walkability may be a useful strategy for weight maintenance in some segments of the adult population. There may be other (social, economic, and/or health) gains realized from improving neighborhood walkability, possibly with broader population impact. These are areas for future research.
Supplementary Material
STUDY IMPORTANCE QUESTIONS.
What is already known about this subject?
Some studies have found that people living in more walkable communities tend to be more physically active and weigh less.
Results suggest those relationships may vary depending on age group and gender.
Methodological limitations in the existing literature make it hard to draw conclusions about the likely effects of policies aimed at improving walkability.
What does this study add?
This study found evidence supporting a causal effect of neighborhood walkability on BMI in both men and women in some age groups but the expected BMI change associated with improving walkability is small.
ACKNOWLEDGMENTS
We acknowledge the invaluable contributions of Brian Bartle, Lishan Cao, Cezary Gwarnicki, and Hao Tong, who constructed analytic data files and performed data analyses, and Alexandrina Balanean who assisted with document editing.
FUNDING: This research was funded by the National Cancer Institute (R01CA172726) with substantial resources provided by the US Department of Veterans Affairs.
The views expressed in this article are those of the authors and do not necessarily represent the views of the National Institute of Health or the Department of Veterans Affairs.
Footnotes
DISCLOSURE: The authors declared no conflict of interest
REFERENCES
- 1.Health, United States, 2016: With Chartbook on Long-term Trends in Health. Hyattsville, MD: 2017. [PubMed] [Google Scholar]
- 2.Cervero R, Duncan M. Walking, bicycling, and urban landscapes: evidence from the San Francisco Bay Area . American journal of public health. 2003;93(9):1478–1483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berke EM, Koepsell TD, Moudon AV, Hoskins RE, Larson EB. Association of the built environment with physical activity and obesity in older persons. Am J Public Health. 2007;97(3):486–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Creatore MI, Glazier RH, Moineddin R, et al. Association of Neighborhood Walkability With Change in Overweight, Obesity, and Diabetes. JAMA. 2016;315(20):2211–2220. [DOI] [PubMed] [Google Scholar]
- 5.Frank LD, Schmid TL, Sallis JF, Chapman J, Saelens BE. Linking objectively measured physical activity with objectively measured urban form: findings from SMARTRAQ. Am J Prev Med. 2005;28(2 Suppl 2):117–125. [DOI] [PubMed] [Google Scholar]
- 6.Hoehner CM, Handy SL, Yan Y, Blair SN, Berrigan D. Association between neighborhood walkability, cardiorespiratory fitness and body-mass index. Soc Sci Med. 2011;73(12):1707–1716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li F, Harmer PA, Cardinal BJ, et al. Built environment, adiposity, and physical activity in adults aged 50-75. Am J Prev Med. 2008;35(1):38–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mayne DJ, Morgan GG, Jalaludin BB, Bauman AE. The contribution of area-level walkability to geographic variation in physical activity: a spatial analysis of 95,837 participants from the 45 and Up Study living in Sydney, Australia. Popul Health Metr. 2017;15(1):38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McCormack GR, McLaren L, Salvo G, Blackstaffe A. Changes in Objectively-Determined Walkability and Physical Activity in Adults: A Quasi-Longitudinal Residential Relocation Study. International journal of environmental research and public health. 2017;14(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rodriguez DA, Evenson KR, Diez Roux AV, Brines SJ. Land use, residential density, and walking. The multi-ethnic study of atherosclerosis. Am J Prev Med. 2009;37(5):397–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rundle A, Roux AV, Free LM, Miller D, Neckerman KM, Weiss CC. The urban built environment and obesity in New York City: a multilevel analysis. Am J Health Promot. 2007;21(4 Suppl):326–334. [DOI] [PubMed] [Google Scholar]
- 12.Chudyk AM, McKay HA, Winters M, Sims-Gould J, Ashe MC. Neighborhood walkability, physical activity, and walking for transportation: A cross-sectional study of older adults living on low income. BMC Geriatr. 2017;17(1):82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grasser G, Van Dyck D, Titze S, Stronegger W. Objectively measured walkability and active transport and weight-related outcomes in adults: a systematic review. Int J Public Health. 2013;58(4):615–625. [DOI] [PubMed] [Google Scholar]
- 14.Koohsari MJ, Oka K, Shibata A, et al. Associations of neighbourhood walkability indices with weight gain. Int J Behav Nutr Phys Act. 2018; 15(1):33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mackenbach JD, Rutter H, Compernolle S, et al. Obesogenic environments: a systematic review of the association between the physical environment and adult weight status, the SPOTLIGHT project. BMC public health. 2014;14:233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sugiyama T, Niyonsenga T, Howard NJ, et al. Residential proximity to urban centres, local-area walkability and change in waist circumference among Australian adults. Prev Med. 2016;93:39–45. [DOI] [PubMed] [Google Scholar]
- 17.Frank LD, Andresen MA, Schmid TL. Obesity relationships with community design, physical activity, and time spent in cars. Am J Prev Med. 2004;27(2):87–96. [DOI] [PubMed] [Google Scholar]
- 18.Wasfi RA, Dasgupta K, Orpana H, Ross NA. Neighborhood Walkability and Body Mass Index Trajectories: Longitudinal Study of Canadians. Am J Public Health. 2016;106(5):934–940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Berry TR, Spence JC, Blanchard C, Cutumisu N, Edwards J, Nykiforuk C. Changes in BMI over 6 years: the role of demographic and neighborhood characteristics. Int J Obes (Lond). 2010;34(8):1275–1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Michael YL, Gold R, Perrin N, Hillier TA. Built environment and change in body mass index in older women. Health Place. 2013;22:7–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sriram U, LaCroix AZ, Barrington WE, et al. Neighborhood Walkability and Adiposity in the Women’s Health Initiative Cohort. Am J Prev Med. 2016;51(5):722–730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Eid J, Overman HG, Puga D, Turner MA. Fat city: Questioning the relationship between urban sprawl and obesity. Journal of Urban Economics. 2008;63(2):385–404. [Google Scholar]
- 23.Garfinkel-Castro A, Kim K, Hamidi S, Ewing R. Obesity and the built environment at different urban scales: examining the literature*. Nutrition Reviews. 2017;75(suppl_1):51–61. [DOI] [PubMed] [Google Scholar]
- 24.Van Dyck D, Cardon G, Deforche B, Owen N, De Bourdeaudhuij I. Relationships between neighborhood walkability and adults’ physical activity: How important is residential self-selection? Health Place. 2011;17(4):1011–1014. [DOI] [PubMed] [Google Scholar]
- 25.Zenk SN, Tarlov E, Powell LM, et al. Weight and Veterans’ Environments Study (WAVES) I and II: Rationale, Methods, and Cohort Characteristics. Am J Health Promot. 2018;32(3):779–794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ingram DD, Franco SJ. 2013 NCHS urban-rural classification scheme for counties. In. Vital and Health Statistics 2014:1–73. [PubMed] [Google Scholar]
- 27.Zenk SN, Tarlov E, Wing C, et al. Geographic Accessibility of Food Outlets not Associated with Body Mass Index Change Among Veterans, 2009-14. Health Aff (Millwood). 2017;36(8):1433–1442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ewing R, Hamidi S. Measuring urban sprawl and validating sprawl measures. Washington, DC: National Institutes of Health and Smart Growth America; 2014. [Google Scholar]
- 29.U.S. Census Bureau. LEHD Origin-Destination Employment Statistics (2002-2014) In: Longitudinal-Employer Household Dynamics Program [distributor], ed. 20160303. Washington, DC: 2017. [Google Scholar]
- 30.Cervero R, Kockelman K. Travel demand and the 3Ds: density, diversity, and design. Transport Res Part D: Transport Environ. 1997;2(3):199–219. [Google Scholar]
- 31.U.S. Department of Veterans Affairs. Health Care Benefits Overview, 2014. Edition. http://www.adopt-a-va.com/assets/ib10-185_health_care_overview_2014_eng_v6_web.pdf. Accessed 5/12/2019 2014. [Google Scholar]
- 32.Barnett DW, Barnett A, Nathan A, Van Cauwenberg J, Cerin E. Built environmental correlates of older adults’ total physical activity and walking: a systematic review and meta-analysis. Int J Behav Nutr Phys Act. 2017; 14(1):103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Carlson JA, Bracy NL, Sallis JF, et al. Sociodemographic moderators of relations of neighborhood safety to physical activity. Med Sci Sports Exerc. 2014;46(8):1554–1563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Carlson JA, Remigio-Baker RA, Anderson CA, et al. Walking mediates associations between neighborhood activity supportiveness and BMI in the Women’s Health Initiative San Diego cohort. Health Place. 2016;38:48–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cerin E, Nathan A, van Cauwenberg J, Barnett DW, Barnett A. The neighbourhood physical environment and active travel in older adults: a systematic review and metaanalysis. Int J Behav Nutr Phys Act. 2017; 14(1): 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pollard TM, Wagnild JM. Gender differences in walking (for leisure, transport and in total) across adult life: a systematic review. BMC public health. 2017; 17(1):341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Aune D, Sen A, Prasad M, et al. BMI and all cause mortality: systematic review and non-linear dose-response meta-analysis of 230 cohort studies with 3.74 million deaths among 30.3 million participants. BMJ. 2016;353:i2156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Global Burden of Disease 2015 Obesity Collaborators, Afshin A, Forouzanfar MH, et al. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N Engl J Med. 2017;377(1):13–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hirsch JA, Diez Roux AV, Moore KA, Evenson KR, Rodriguez DA. Change in walking and body mass index following residential relocation: the multi-ethnic study of atherosclerosis. Am J Public Health. 2014;104(3):e49–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hirsch JA, Moore KA, Barrientos-Gutierrez T, et al. Built environment change and change in BMI and waist circumference: Multi-ethnic Study of Atherosclerosis. Obesity. 2014;22(11):2450–2457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lee IM, Ewing R, Sesso HD. The Built Environment and Physical Activity Levels: The Harvard Alumni Health Study. American Journal of Preventive Medicine. 2009;37(4):293–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Carr LJ, Dunsiger SI, Marcus BH. Validation of Walk Score for estimating access to walkable amenities. Br J Sports Med. 2011;45(14):1144–1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Duncan DT, Aldstadt J, Whalen J, Melly SJ, Gortmaker SL. Validation of walk score for estimating neighborhood walkability: an analysis of four US metropolitan areas. International journal of environmental research and public health. 2011;8(11):4160–4179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Courtney-Long EA, Carroll DD, Zhang QC, et al. Prevalence of disability and disability type among adults—United States, 2013. MMWR Morb Mortal Wkly Rep. 2015;64(29):777–783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Holder KA. The Disability of Veterans. Washington, DC: U.S. Census Bureau Social, Economic, and Housing Statistics Division;2016. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


