Abstract
Background
Telemedicine use is increasing in many specialties, but its impact on clinical outcomes in infectious diseases has not been systematically reviewed. We reviewed the current evidence for clinical effectiveness of telemedicine infectious diseases consultations, including outcomes of mortality, hospital readmission, antimicrobial use, cost, length of stay, adherence, and patient satisfaction.
Methods
We queried Ovid MEDLINE 1946-, Embase.com 1947-, Scopus 1823-, Cochrane Database of Systematic Reviews (CDSR), Cochrane Central Register of Controlled Trials (CENTRAL), and ClinicalTrials.gov 1997- through August 5, 2019, for studies looking at clinical outcomes of infectious diseases in the setting of telemedicine use. We did not restrict by language or year of publication. Clinical outcomes searched included 30-day all-cause mortality, 30-day readmissions, patient compliance/adherence, patient satisfaction, cost or cost-effectiveness, length of hospital stay, antimicrobial use, and antimicrobial stewardship. Bias was assessed using standard methodologies. PROSPERO CRD42018105225.
Results
From a search pool of 1154 studies, only 18 involved telemedicine infectious diseases consultation and our selected clinical outcomes. The outcomes tracked were heterogeneous, precluding meta-analysis, and the majority of studies were of poor quality. Overall, clinical outcomes with telemedicine infectious diseases consultation seem comparable to in-person infectious diseases consultation.
Conclusions
Although in widespread use, the clinical effectiveness of telemedicine infectious diseases consultations has yet to be sufficiently studied. Further studies, or publication of previously collected and available data, are warranted to verify the cost-effectiveness of this widespread practice.
Systematic review registration
PROSPERO CRD42018105225.
Keywords: clinical outcomes, infectious diseases consultation, mortality, systematic review, telemedicine
According to recent estimates, infectious diseases may be the third leading cause of death in the United States [1]. However, underserved and/or economically disadvantaged areas may not have access to infectious diseases (ID) physicians (up to 45% of US hospitals) to help treat these infections [2]. This is problematic because consultation with ID physicians significantly reduces mortality for numerous infections [3, 4]. Providing access to ID expertise in underserved/rural areas could substantially reduce mortality and improve clinical outcomes. As 51% of ID fellowship programs did not fill in 2015 [5, 6], access to ID expertise may be limited. With a shortage of ID physicians, it may not be possible for remote locations to employ an ID physician, that is, what is seen in current practice. Telemedicine could potentially expand ID expertise to underserved areas.
Telemedicine is widely used in many subspecialties. Studies show that telemedicine reduces mortality in progressive and intensive care units and in very low birth weight infants [7–9], but its effectiveness for important clinical outcomes in infectious diseases is lacking. To date, there has been no synthesis of evidence for the use of telemedicine for infectious diseases consultation. Our systematic review addresses this deficiency by answering the following question: In patients with infectious diseases, do telemedicine ID consultations improve the clinical outcomes of mortality, readmission, patient adherence/compliance, patient satisfaction, cost, cost-effectiveness, length of stay, antibiotic use, or antibiotic stewardship?
METHODS
Data Sources and Searches
A medical librarian (L.H.Y.) searched the literature for records including the concepts of infectious diseases, infection, antimicrobial stewardship, antibiotic stewardship, antifungal stewardship, antiviral stewardship, telemedicine and videoconferencing, and consultation/consult. The librarian created search strategies using a combination of keywords and controlled vocabulary in Ovid Medline 1946-, Embase 1947-, Scopus 1823-, Cochrane Database of Systematic Reviews (CDSR), Cochrane Central Register of Controlled Trials (CENTRAL), and Clinicaltrials.gov 1997-. All search strategies were completed in November 2018, then updated in August 2019. The protocol was registered with the international prospective register of systematic reviews (PROSPERO), in accordance with PRISMA-P guidelines (PROSPERO CRD42018105225) [10]. The protocol for this systematic review has been previously described [11].
Aim
Our goal was to assess the effectiveness of telemedicine ID consultation for a range of clinical outcomes (enumerated below) as compared with either (1) no ID consultation or (2) other modalities of ID consultation (eg, in person). Clinical outcomes considered included 30-day all-cause mortality, readmission within 30 days of discharge from an initial hospitalization with an infection, patient compliance/adherence, patient satisfaction, cost or cost-effectiveness, length of hospital stay, antimicrobial use, and/or antimicrobial stewardship.
There were no language or year of publication restrictions. Translation of non-English-language abstracts was undertaken, as required, though ultimately all full-text articles were in English. Conference abstracts were excluded if sufficient outcome and bias data could not be extracted. REDCap was used for data entry.
Study Selection
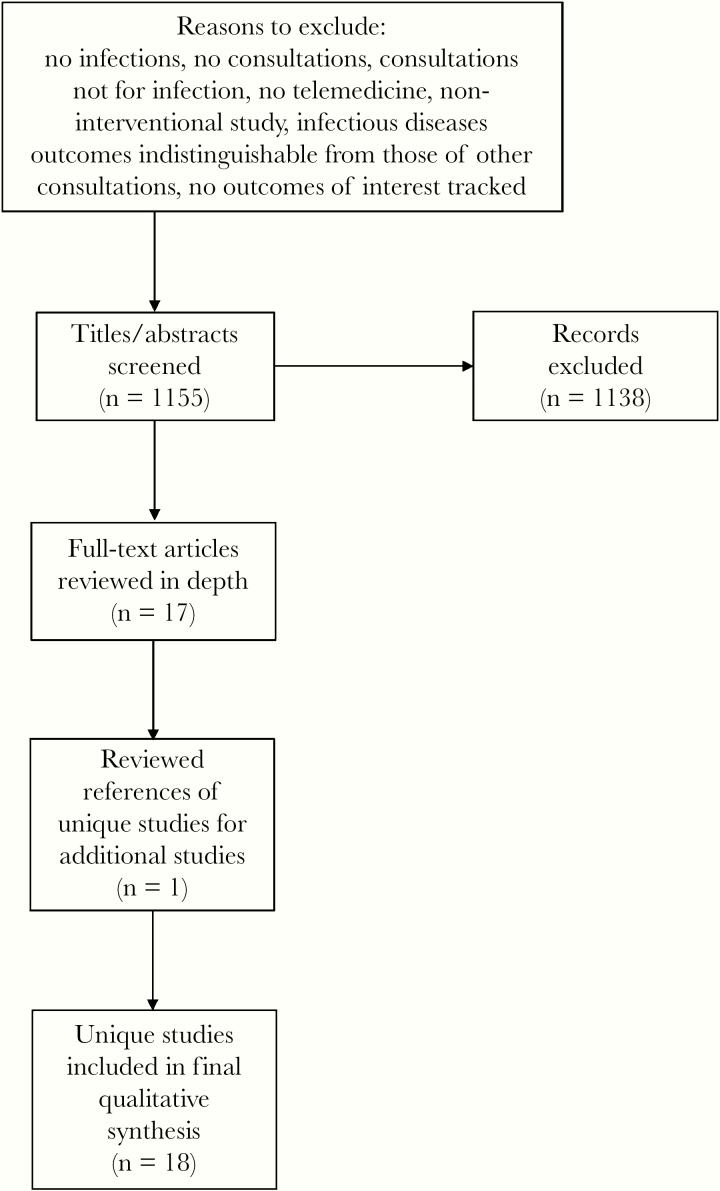
After removal of duplicate results, titles and abstracts were reviewed for relevance to the research question by J.P.B. See Figure 1 for the study flowchart from title/abstract review to final inclusion. Articles were excluded if any of the following conditions was met: (1) infections not studied, (2) no consultations, (3) consultations not performed for infection, (4) no telemedicine, (5) noninterventional (eg, viewpoint articles, commentaries, etc.), (6) infectious diseases outcomes indistinguishable from other consultations, (7) no prespecified outcomes of interest tracked, or (8) abstract only with insufficient methodological or results reporting. Studies that were not excluded underwent independent, blinded, full-text review by J.P.B. and G.A.C.
Figure 1.
Flowchart for systematic review.
Definitions
Telemedicine was defined as remote clinical services administered using a technological medium. This included face-to-face video chat (physician-to-physician or physician-to-patient), voice chat after review of electronic health records, or electronic health record documentation after remote chart review without direct voice or video contact with physician or patient. Antibiotic stewardship was quantified as either antibiotic costs or antibiotic appropriateness, as judged by the authors of the individual studies.
Data Extraction
In a blinded fashion, 2 authors (J.P.B. and G.A.C.) independently extracted data from full-text articles. Data extracted included study quality, clinical or system-level outcome tracked, percent change or proportion experiencing each clinical outcome, numbers of patients, age group, consultant specialty, type of telemedicine, study location, whether infection was confirmed by laboratory results, and type and risk of bias.
Data extraction disputes were settled by a third reviewer (S.A.F.—also blinded), and in cases requiring further adjudication, a group session of all 3 reviewers was convened.
Quality Assessment
Risk of bias was independently reviewed by 2 reviewers (J.P.B. and G.A.C.) in a blinded fashion. Disputes were resolved by a third reviewer (S.A.F.—also blinded), and in cases of continued disagreement, the 3 reviewers met for adjudication. Bias determination was guided by the Cochrane Consumers and Communication Review Group Study Quality Guide or Newcastle-Ottawa scale [12, 13]. Using the Newcastle-Ottawa Scale, the case–control and cohort studies were given star ratings in 3 categories —Selection (maximum 4 stars), Comparability (maximum 2 stars), and Outcome (maximum 3 stars)—with a maximum score of 9 stars [13]. The quality of case–control and cohort studies was adjudicated based on previously published guidance [14]: good quality: Selection ≥3 stars AND Comparability ≥1 stars AND Outcome ≥2 stars; fair quality: Selection 2 stars AND Comparability ≥1 stars AND Outcome ≥2 stars; poor quality: Selection ≤1 Star OR Comparability 0 stars OR ≤1 stars.
Analysis
Per protocol [11], prespecified subgroup analyses included outcomes by age (children <18 years vs adult ≥18 years), telemedicine consultant being ID trained or not, infection type, type of telehealth/telemedicine intervention (eg, face-to-face, asynchronous, etc.), study location (US vs non-US), number of ID consultations (ie, days physician interacted with patient/provider), and culture- or laboratory-confirmed infection vs presumed infection. Due to the limited number of studies, qualitative/narrative synthesis was performed.
RESULTS
A total of 1328 results were found using our initial search strategy, which was completed in November 2018. A total of 284 duplicate records were identified using Endnote’s automatic duplication finder, and another 31 duplicates were removed by manual review, leaving 1013 unique citations in the project library. One additional study was identified after reviewing references of full-text article reviews, for a total of 1014 search results. We updated our search on August 5, 2019. With this update, an additional 140 results were found, leaving a total of 1154 results to be reviewed. Fully reportable searches can be found in Appendix 1.
Of the 1154, none of the clinical trials identified only from ClinicalTrials.gov (n = 21) had available results. Of the remaining excluded articles, the reasons for exclusion are listed in Figure 1 and Supplementary Table 1. A total of 18 articles were relevant to the research question and underwent full-text review. From these articles, clinical outcomes tracked included 30-day mortality after an infection (16.7%, n = 3), readmission within 30 days after discharge from the initial hospitalization with an infection (5.6%, n = 1), patient compliance/adherence (11.1%, n = 2), patient satisfaction (50.0%, n = 9), cost or cost-effectiveness (22.2%, n = 4), length of stay (27.8%, n = 5), and antimicrobial use (27.8%, n = 5). Meta-analysis was not performed due to the low number of studies with any 1 outcome.
Biases/Quality Assessment
There were 2 (11.1%) randomized clinical trials, 2 case–control studies (11.1%), and 14 (77.8%) cohort studies. Both randomized controlled trials had high risk of bias in 3 categories and unclear risk in 2 others [15, 16]. Using the Newcastle-Ottawa Scale, both the case–control studies and 8 cohort studies were rated as poor quality. The remaining 6 cohort studies were rated as good quality (Supplementary Table 2).
Study Characteristics
Most studies were performed only in adults (n = 13, 72.2%). Consultant specialty was infectious diseases in only 38.9% (n = 7). Infections studied included pneumonia (n = 4), urinary tract infection (n = 5), sepsis (n = 3), bacteremia (n = 3), endocarditis (n = 2), skin and soft tissue infections (n = 3), upper respiratory infections (n = 4), and other (n = 12). More than 1 infection type could be studied in each article.
The most common type of telemedicine was face-to-face videoconferencing with the patient in 72.2% (n = 13), followed by telephone only (16.7%, n = 3), physician-to-physician only (5.6%, n = 1), and 1 study in which the telemedicine type could not definitively be determined.
Just over half (n = 10) were based in the United States, and 8 in other countries (Europe = 4, Australia = 2, Asia = 1, Canada = 1). Infections were confirmed by culture in 61.1% (n = 11) of studies.
Clinical Outcomes
Patient satisfaction with telemedicine was the most commonly reported outcome, and the percentage of patients satisfied with telemedicine was above 97% in 6/7 studies [17–22], with 1 study reporting patient satisfaction of 69% (Table 1) [16]. Two additional studies reported patient satisfaction but provided a mean satisfaction score without a numerator and denominator for the number of patients reporting the outcome, though the mean score in both studies was indicative of high satisfaction [23, 24].
Table 1.
Clinical Outcomes of Telemedicine Infectious Diseases Consultation as Compared With Control for Individual Studies From Systematic Review
| Study (First Author, Reference Number) | Control | Intervention | Group Size (Control, Intervention) | Telehealth Type |
|---|---|---|---|---|
| Mortality, % | ||||
| Assimacopoulos [35] | 5 | 1 | 59, 48 | Face-to-face video |
| Chen [15] | 1 | 0 | 150, 148 | Telephone only |
| Saunderson [26] | 12 | 22 | 294, 183 | Telephone only |
| Monkowski [27] | 10 | 5 | 73, 171 | Face-to-face video |
| Readmission, % | ||||
| Monkowski [27] | 17 | 11 | 73, 171 | Face-to-face video |
| Patient satisfaction, % | ||||
| Cuadrado [23] | n/a | Unable to determine | 0, 63 | Face-to-face video |
| Garrett [17] | n/a | 100 | 0, 28 | Telephone only |
| Leόn [16] | n/a | 69 | 41, 42 | Face-to-face video |
| Mashru [21] | n/a | 98 | 0, 76 | Face-to-face video |
| Nazareth [18] | n/a | 100 | 559, 50 | Face-to-face video |
| Saifu [19] | n/a | 97 | 0, 43 | Face-to-face video |
| You [20] | n/a | 100 | 0, 96 | Face-to-face video |
| Eron [24] | n/a | Unable to determine | 25, 25 | Face-to-face video |
| Staicu [22] | n/a | 98 | 0, 50 | Face-to-face video |
| Antimicrobial use, % | ||||
| Mehrotra [30] | 77 | 99 | 7545, 574 | Face-to-face video |
| Rincon [31] | n/a | 74 | 0, 5437 | Other |
| Shi [32] | 53 | 52 | 1128629, 38839 | Face-to-face video |
| Patient adherence/compliance, % | ||||
| Chen [15] | 88 | 95 | 150, 148 | Telephone only |
| Saifu [19] | n/a | 76 | 0, 43 | Face-to-face video |
| Length of hospital stay, d | ||||
| Assimacopoulos [35] | 10.7 | 6.5 | 59, 48 | Face-to-face video |
| Ceradini [28] | 8.4 | 8.4 | 683, 531 | Physician-to-physician |
| Saunderson [26] | 29 | 30 | 294, 183 | Telephone only |
| Eron [24] | 8 | 2.6 | 25, 25 | Face-to-face video |
| Monkowski [27] | 14 | 9 | 73, 171 | Face-to-face video |
| Antimicrobial use, d | ||||
| Assimacopoulos [35] | 13.4 | 6.9 | 59, 48 | Face-to-face video |
| Monkowski [27] | 19 | 15 | 73, 171 | Face-to-face video |
Mortality was higher in the telemedicine group in 2 studies and lower in the other 2 studies reporting this outcome (range for all studies, 0%–22%) [15, 25–27], with 1 study reporting 90-day instead of 30-day mortality (higher mortality in the control group) (Table 1) [27]. Only 1 of these studies was statistically significant, with lower mortality in patients receiving in-person rather than telephone-only ID consults [26]. Length of stay was shorter in the telemedicine group in 4/5 studies [24–27] and equivalent in 1 study (range, 2.6–30 days) (Table 1) [28].
Readmission and adherence/compliance were similar between telemedicine and nontelemedicine groups (Table 1) [15, 19, 27]. Costs were lower in the telemedicine groups, but based on projections that may not be generalizable [15, 24, 28, 29]. Antibiotic use was similar between telemedicine groups and controls [25, 27, 30–32].
Discussion
Based on the available, albeit limited, evidence, telemedicine ID consultation seems comparable to standard of care for the clinical outcomes of mortality, length of stay, readmission, adherence, cost, and antimicrobial use. However, there were few relevant studies tracking our prespecified clinical outcomes, and the majority were of poor quality. Without more robust data quality and availability, it is difficult to draw any firm conclusions.
Few studies have been published demonstrating effectiveness of telemedicine for infectious diseases consultation. Infection types that have been studied, as well as the settings in which telemedicine has been used, have been varied. As telemedicine continues to expand, clinicians and researchers should consider publication of their already existing data to document the clinical effectiveness needed to validate this model of care and costs. In addition, researchers must report their processes of telemedicine ID implementation so that what works in 1 study can be applied more broadly, understanding that adaptations will likely be required. In this rapidly blossoming field, we must publish best practices using standardized reporting for effective and implementable telemedicine ID consults so that our patients reap maximum benefits.
Our review is limited in scope by our chosen clinical outcomes. Among the excluded studies (data not shown) were studies looking at the use of telemedicine to care for patients with hepatitis C or HIV (among others). These studies are important and relevant to the telemedicine ID consultation landscape, but did not track our prespecified clinical outcomes. The clinical outcomes we chose are of interest to inpatient settings (mortality, readmission, length of stay) and administrators (cost, patient satisfaction, readmission, antimicrobial use, mortality). A summary of the currently available data may help in the adoption of inpatient telemedicine ID services by inpatient physicians and administrators, should the data become more robust.
Infectious diseases consultation can save lives, and with almost half of US hospitals without ID physician access [2], telemedicine has great potential to fill this gap. Before its wide adoption, it should be robustly evidence-based. Important questions in this arena are related to which type of telemedicine is required, how frequently telemedicine visits must be performed (eg, daily, 1-time), and what level of infectious diseases physician involvement is optimal to achieve the best clinical outcomes. For example, a recent study showed that an algorithm-based care model for Staphylococcus aureus bacteremia achieved noninferior outcomes to usual care [33]. With this in mind, one must ask what the minimum unit of efficacy is for infection management. Whether that is in-person consultation, telemedicine consultation, Extension for Community Healthcare Outcomes (ECHO)–like models, algorithm-based care, or another care model has yet to be determined. In addition, it is unknown whether certain infections will require different levels of ID input for optimal outcomes. Notably, curbside consultations are often inaccurate and potentially harmful [34], which may have implications for care delivery methods (eg, telephone consultation only). Further studies are required.
Many questions remain to be answered for telemedicine ID consultation, including reimbursement, as state-to-state differences in telemedicine coverage remain a barrier to implementation. As the field of telemedicine continues to grow, these questions must be addressed to provide the best and most efficient care for patients. Societal and technological barriers such as access to high-speed Internet and video quality have limited telemedicine’s usefulness in the past. Although Internet access issues persist in some rural areas, progress has been made and video quality has improved. High-priority areas of telemedicine research include publishing data that are already being collected as part of routine clinical care, understanding the use of telemedicine in rural/underserved settings and how it reduces barriers to care and reduces the health care disparities therein, and determining how to most efficiently deliver care (eg, face-to-face vs e-consult, etc.). Telemedicine ID consultation may be a way to reduce inequities and treatment disparities for rural/economically disadvantaged patients, and from the perspective of primum non nocere, we must be sure that what we are doing is what is best.
Supplementary Data
Supplementary materials are available at Open Forum Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Acknowledgments
Financial support. This work was supported by grant number UL1 TR002345, sub-award KL2 TR002346, from the National Institutes of Health (NIH)–National Center for Advancing Translational Sciences (NCATS), components of the NIH, and the NIH Roadmap for Medical Research. This publication, in whole or in part, was supported by The Foundation for Barnes-Jewish Hospital and their generous donors and the Washington University Institute of Clinical and Translational Sciences, which is, in part, supported by the NIH/NCATS, CTSA grant UL1TR002345. This work was also supported by the Agency for Healthcare Research and Quality (AHRQ; grant number R01-HS024269 to S.A.F.).
Disclaimer. This article’s contents are solely the responsibility of the authors and do not necessarily represent the official view of NCATS or the NIH.
Potential conflicts of interest. All authors: no reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Burnham JP, Olsen MA, Kollef MH. Re-estimating annual deaths due to multidrug-resistant organism infections. Infect Control Hosp Epidemiol 2019; 40(1):112–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. McQuillen DP, MacIntyre AT. The value that infectious diseases physicians bring to the healthcare system. J Infect Dis 2017; 216:588–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Vogel M, Schmitz RP, Hagel S, et al. Infectious disease consultation for Staphylococcus aureus bacteremia - a systematic review and meta-analysis. J Infect 2016; 72:19–28. [DOI] [PubMed] [Google Scholar]
- 4. Burnham JP, Olsen MA, Stwalley D, et al. Infectious diseases consultation reduces 30-day and 1-year all-cause mortality for multidrug-resistant organism infections. Open Forum Infect Dis 2018; 5(X):XXX–XX. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chandrasekar PH. Bad news to worse news: 2015 infectious diseases fellowship match results. Clin Infect Dis 2015; 60:1438. [DOI] [PubMed] [Google Scholar]
- 6. Chandrasekar P, Havlichek D, Johnson LB. Infectious diseases subspecialty: declining demand challenges and opportunities. Clin Infect Dis 2014; 59:1593–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Armaignac DL, Saxena A, Rubens M, et al. Impact of telemedicine on mortality, length of stay, and cost among patients in progressive care units: experience from a large healthcare system. Crit Care Med 2018; 46:728–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kahn JM, Le TQ, Barnato AE, et al. ICU telemedicine and critical care mortality: a national effectiveness study. Med Care 2016; 54:319–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kim EW, Teague-Ross TJ, Greenfield WW, et al. Telemedicine collaboration improves perinatal regionalization and lowers statewide infant mortality. J Perinatol 2013; 33:725–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Moher D, Shamseer L, Clarke M, et al. ; PRISMA-P Group Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) 2015 statement. Syst Rev 2015; 4:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Burnham JP, Fritz SA, Yaeger LH, Colditz GA. Telemedicine infectious diseases consultations and clinical outcomes: a systematic review and meta-analysis protocol. Syst Rev 2019; 8:135–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ryan R, Hill S, Prictor M, McKenzie J.Cochrane Consumers and Communication Review Group. Study Quality Guide 2013. Available at: http://cccrg.cochrane.org/author-resources. Accessed 12 December 2018. [Google Scholar]
- 13.Wells GA, Shea B, O'Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analysis Available at: www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 3 January 2019.
- 14. Likis FE, Andrews JA, Collins MR, et al. Nitrous Oxide for the Management of Labor Pain. Comparative Effectiveness Review No. 67 (Prepared by the Vanderbilt Evidence-based Practice Center under Contract No. 290-2007-10065-I). Rockville, MD: Agency for Healthcare Research and Quality; 2012. [PubMed] [Google Scholar]
- 15. Chen WL, Chiu WT, Wu MS, et al. Translational research of telecare for the treatment of hepatitis C. Biomed Res Int 2014; 2014:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. León A, Cáceres C, Fernández E, et al. A new multidisciplinary home care telemedicine system to monitor stable chronic human immunodeficiency virus-infected patients: a randomized study. PLoS One 2011; 6: 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Garrett CC, Kirkman M, Chen MY, et al. Clients’ views on a piloted telemedicine sexual health service for rural youth. Sex Health 2012; 9:192–3. [DOI] [PubMed] [Google Scholar]
- 18. Nazareth S, Kontorinis N, Muwanwella N, et al. Successful treatment of patients with hepatitis C in rural and remote Western Australia via telehealth. J Telemed Telecare 2013; 19:101–6. [DOI] [PubMed] [Google Scholar]
- 19. Saifu HN, Asch SM, Goetz MB, et al. Evaluation of human immunodeficiency virus and hepatitis C telemedicine clinics. Am J Manag Care 2012; 18:207–12. [PubMed] [Google Scholar]
- 20. You A, Kawamoto J, Smith JP. A pharmacist-managed telemedicine clinic for hepatitis C care: a descriptive analysis. J Telemed Telecare 2014; 20:99–101. [DOI] [PubMed] [Google Scholar]
- 21. Mashru J, Kirlew M, Saginur R, Schreiber YS. Management of infectious diseases in remote northwestern Ontario with telemedicine videoconference consultations. J Telemed Telecare 2017; 23:83–7. [DOI] [PubMed] [Google Scholar]
- 22. Staicu ML, Holly AM, Conn KM, Ramsey A. The use of telemedicine for penicillin allergy skin testing. J Allergy Clin Immunol Pract 2018; 6:2033–40. [DOI] [PubMed] [Google Scholar]
- 23. Cuadrado A, Llerena S, Cobo C, et al. Microenvironment eradication of hepatitis C: a novel treatment paradigm. Am J Gastroenterol 2018; 113:1639–48. [DOI] [PubMed] [Google Scholar]
- 24. Eron L, King P, Marineau M, Yonehara C. Treating acute infections by telemedicine in the home. Clin Infect Dis 2004; 39:1175–81. [DOI] [PubMed] [Google Scholar]
- 25. Assimacopoulos A, Alam R, Arbo M, et al. A brief retrospective review of medical records comparing outcomes for inpatients treated via telehealth versus in-person protocols: is telehealth equally effective as in-person visits for treating neutropenic fever, bacterial pneumonia, and infected bacterial wounds? Telemed J E Health 2008; 14:762–8. [DOI] [PubMed] [Google Scholar]
- 26. Saunderson RB, Gouliouris T, Nickerson EK, et al. Impact of routine bedside infectious disease consultation on clinical management and outcome of Staphylococcus aureus bacteraemia in adults. Clin Microbiol Infect 2015; 21:779–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Monkowski D, Rhodes LV, Templer S, et al. A retrospective cohort study to assess the impact of an inpatient infectious disease telemedicine consultation service on hospital and patient outcomes. Clin Infect Dis. In press. [DOI] [PubMed] [Google Scholar]
- 28. Ceradini J, Tozzi AE, D'Argenio P, et al. Telemedicine as an effective intervention to improve antibiotic appropriateness prescription and to reduce costs in pediatrics. Ital J Pediatr 2017; 43:1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Gordon AS, Adamson WC, DeVries AR. Virtual visits for acute, nonurgent care: a claims analysis of episode-level utilization. J Med Internet Res 2017; 19:e35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Mehrotra A, Paone S, Martich GD, et al. A comparison of care at e-visits and physician office visits for sinusitis and urinary tract infection. JAMA Intern Med 2013; 173:72–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Rincon TA, Bourke G, Seiver A. Standardizing sepsis screening and management via a tele-ICU program improves patient care. Telemed J E Health 2011; 17:560–4. [DOI] [PubMed] [Google Scholar]
- 32. Shi Z, Mehrotra A, Gidengil CA, et al. Quality of care for acute respiratory infections during direct-to-consumer telemedicine visits for adults. Health Aff (Millwood) 2018; 37:2014–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Holland TL, Raad I, Boucher HW, et al. ; Staphylococcal Bacteremia Investigators Effect of algorithm-based therapy vs usual care on clinical success and serious adverse events in patients with staphylococcal bacteremia: a randomized clinical trial. JAMA 2018; 320:1249–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Burden M, Sarcone E, Keniston A, et al. Prospective comparison of curbside versus formal consultations. J Hosp Med 2013; 8:31–5. [DOI] [PubMed] [Google Scholar]
- 35. Assimacopoulos A, Alam R, Arbo M, et al. A brief retrospective review of medical records comparing outcomes for inpatients treated via telehealth versus in-person protocols: is telehealth equally effective as in-person visits for treating neutropenic fever, bacterial pneumonia, and infected bacterial wounds? Telemed J E Health 2008; 14:762–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.