Abstract
Present-day drug therapies provide clear beneficial effects as many diseases can be driven into remission and the symptoms of others can be efficiently managed; however, the success of many drugs is limited due to both patient non-compliance and adverse off-target or toxicity-induced effects. There is emerging evidence that many of these side effects are caused by drug-induced impairment of mitochondrial function and eventual mitochondrial dysfunction. It is imperative to understand how and why drug-induced side effects occur and how mitochondrial function is affected. In an aging population, age-associated drug toxicity is another key area of focus as the majority of patients on medication are older. Therefore, with an aging population possessing subtle or even more dramatic individual differences in mitochondrial function, there is a growing necessity to identify and understand early on potentially significant drug-associated off-target effects and toxicity issues. This will not only reduce the number of unwanted side effects linked to mitochondrial toxicity but also identify useful mitochondrial-modulating agents. Mechanistically, many successful drug classes including diabetic treatments, antibiotics, chemotherapies and antiviral agents have been linked to mitochondrial targeted effects. This is a growing area, with research to repurpose current medications affecting mitochondrial function being assessed in cancer, the immune system and neurodegenerative disorders including Parkinson's disease. Here, we review the effects that pharmacological agents have on mitochondrial function and explore the opportunities from these effects as potential disease treatments. Our focus will be on cancer treatment and immune modulation.
Introduction
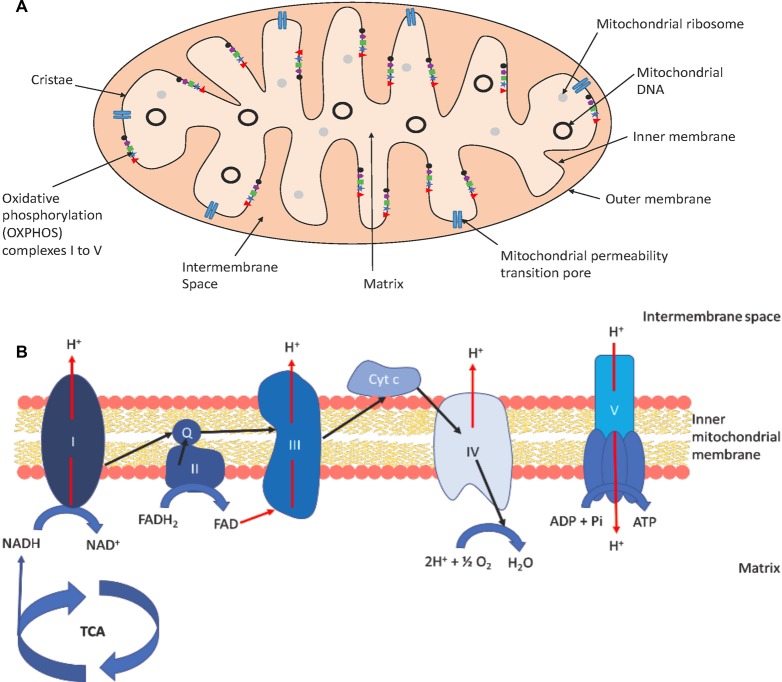
Mitochondria are intracellular membrane-bound organelles that act as the cells ‘powerhouse’ due to their principal function in synthesizing adenosine triphosphate (ATP) required for a multitude of processes and reactions. This is achieved through the coupling of electron transport and the creation of an electrochemical gradient to the synthesis of ATP. The gradient is created by the translocation of protons across the inner membrane to the intermembrane space by three unique oxidoreductases [1]. As protons pass back into the mitochondrial matrix via ATP synthase/complex V, this drives the ATP synthase to combine ADP and inorganic phosphate generating the cellular energy fuel ATP (Figure 1).
Figure 1. Key features of mitochondrial structure and function of the ETC.
Key structures of the mitochondrion are represented in (A), while (B) depicts the structure of the OXPHOS system and its functioning. Oxidative phosphorylation complexes represent reduced nicotinamide adenine dinucleotide (NADH) dehydrogenase (I), succinate dehydrogenase (II), cytochrome c reductase (III), cytochrome c oxidase (IV) and ATP synthase (V) where Q represents coenzyme Q and cyt c represents cytochrome c. In (B), black arrows show the transfer of electrons between complexes while red arrows show the transfer of protons throughout the chain for the eventual production of ATP and H2O. Features are not to scale.
Mitochondria possess their own genome, mitochondrial DNA (mtDNA), which is a 16.6 kbp closed, circular, double-stranded DNA genome. Most cells contain hundreds to thousands of copies of mtDNA, which encodes two ribosomal ribonucleic acid (RNA) and 22 transfer RNAs which are necessary for translation of the 13 mtDNA-encoded mRNAs that comprise key subunits of the oxidative phosphorylation (OXPHOS) complexes [2]. Despite the ability of the mitochondria to carry out DNA replication, mtDNA transcription and protein translation independently of the nucleus, these functions are, in fact, semiautonomous in nature [3]. Mitochondria require nuclear DNA-encoded genes for function, and indeed, all of the DNA replication, transcription, ribosomal protein machinery and most of the OXPHOS subunits are nuclear encoded [4]. Furthermore, anterograde and retrograde signalling between the mtDNA and the nucleus allows mitochondria to change bioenergetics and biosynthetic output to match cellular needs or respond to cellular stress [5]. MtDNA contains no introns and histones, and only low levels of repair mechanisms such as mtDNA damage, depletion or mutation may have a very large impact on mitochondrial function. The mtDNA copy number per cell varies greatly with over 150 000 in an oocyte to only several hundred in cells found in lung tissue [6]. Generally, cells with the highest energy demand have the highest number of mitochondria [7] and mtDNA copy number [8]. The cellular distribution of mitochondria varies between cell types. Large cells such as motor neurones, being over 1 m long, reposition their mitochondria to the site of the neuromuscular junction where the most ATP is required [9]. This provides a further complication of moving mitochondria (dynamics) from the cell body along the axon to the synaptic terminals. An inability to maintain mitochondrial function at the synapse potentially leads to neuronal dysfunction and neurodegeneration [10] with a disruption in mitochondrial distribution at synaptic/neuromuscular junctions associated with motor neurone diseases such as amyotrophic lateral sclerosis and Huntingdon's disease [11,12].
A diverse range of mitochondrial functions have been identified in addition to their crucial role in aerobic respiration and ATP production. Mitochondria dictate cell survival and death via opening of the mitochondrial permeability transition pore [13] and play a crucial role in calcium homeostasis and buffering [14]. Furthermore, mitochondria have been found to be key players in steroid and hormone signalling, energy sensing, production of reactive oxygen species (ROS) and cofactor synthesis [5]. The biosynthesis of critical cofactors is an important role of the organelle including the highly eukaryotic-conserved, formation of iron–sulfur clusters and the biosynthesis of haeme, biotin and lipoic acid [15]. More recently, it has emerged that mitochondria serve as key immune regulators, shaping both beneficial and detrimental immune responses during pathogen infection, inflammatory diseases, cancer and aging [16–18]. This pivotal role in cell biology explains the severe and multisystem clinical symptoms which occur as a result of mitochondrial dysfunction and highlights the need for increased research on the role of mitochondria in health and disease. To maintain integrity, mitochondria are under strict quality control measures involving fission/fusion [19], mitophagy and proteasomal degradation, which can selectively remove both damaged proteins and dysfunctional mitochondria [20]. Mitophagy is particularly important in differentiated cells where attempts at modulating it are being explored in order to enhance removal or turnover of damaged mitochondria associated with disease or aging [21–24].
Toxic effects of pharmacological agents on mitochondrial function
Drug therapy has clear beneficial effects by causing remission of many diseases and improvement in symptom management; however, as patient life expectancy increases, long-term side effects of treatments have emerged. Mitochondrial dysfunction can result from different drug types through a variety of mechanisms, summarized in Table 1. Antiviral therapy using nucleoside reverse transcriptase inhibitors (NRTIs) can successfully control virus levels, and the development of this antiviral therapy approach proved to be a major cornerstone in reducing the morbidity and mortality of various viral infections such as human immunodeficiency virus (HIV). However, there is a risk of NRTI-induced inhibition of human DNA polymerases due to structural conservation between human and viral polymerases and the disruption of dNTP pools [25]. Polymerase inhibition has led to the well-supported ‘DNA pol-γ hypothesis’ of mitochondrial dysfunction, where NRTI treatment inhibits DNA pol-γ in mitochondria and results in mtDNA depletion [26]. It was found that early HIV treatments had substantial levels of toxicity, such that 25% of patients discontinued their antiviral regime due to the toxicity or from non-compliance [27]. Other HIV treatments have been withdrawn completely due to associated mitochondrial toxicity, the antiretroviral drug zalcitibine being a key example [28]. The clinical development of new antiviral agents to treat viral infection produced compounds such as tenofovir, which has minimal mitochondrial toxicity compared with zalcitabine and didanosine [29]. Tenofovir is used in combination with other NRTI antivirals such as abacavir and lamivudine in modern HIV therapy, all of which report lower mitochondrial toxicity than previous NRTIs [30].
Table 1. Summary of drugs with associated mitochondrial toxicity.
| Drug type | Examples | Mechanism | Mitochondrial effects | Clinical symptoms |
|---|---|---|---|---|
| Antiviral-nuceloside reverse transcriptase inhibitor (NRTI) | Zidovudine (AZT) (black box warning) Acyclovir (ACV) Ganciclovir (GCV) Zalcitabine (ddC) |
Analogues to endogenous dNTPs therefore inhibit mtDNA polymerase-γ and prevent chain elongation of nascent mtDNA chain [131,132] | MtDNA depletion [26,132] Decreased synthesis of OXPHOS proteins, increased superoxide levels [133] DNA breaks in mtDNA with ACV and GCV [134] Abnormally structured mitochondria [135,136] Inhibition of cytochrome c oxidase and citrate synthase [137] Interference with the phosphoregulation of ETC subunits [26] |
Lactic acidosis, altered lipid metabolism and altered carbohydrate metabolism [26] Red-ragged fibers in muscle, myopathy [138,139] Neuropathy, liver steacidosis, pancreatitis [29] |
| Antiviral-protease inhibitor (PI) | Saquinavir (black box warning) | Inhibits cleavage of host cell polyprotiens into functional proteins [140] | Inability to assemble functional ETC [26] Interference with lipid metabolism and retinoid signalling [141] |
Lipodystrophy, hyperlipidaemia, insulin resistance [141] |
| Antibiotic | Tetracycline | Inhibition of protein synthesis | Decreased mitochondrial membrane potential, down-regulation of ETC function and protein synthesis [67,142] | |
| Ciprofloxacin (black box warning) | Inhibition of Top2 (topoisomerase) which prevents the relaxation of mtDNA for replication [143] | Inhibition of mtDNA replication, mtDNA depletion and dysregulation of ETC complexes [143] dsDNA breaks [144] Increased ROS levels and oxidative stress [145] Respiration decreased 40% in vitro, accompanied by reduced cytochrome c oxidase (COX) activity and lactate accumulation [146] Suppression of ETC complexes I and II [147] |
Tendinopathies, neuropathies, myopathy and psychological symptoms [143] | |
| Chemotherapy agent | Cisplatin (black box warning) Cyclophosphamide |
Bind to the purine residues in the mtDNA of cells to cause damage in the DNA, inhibition of cell division and apoptotic cell death [148,149] | Increased ROS production [36,129] mtDNA damage in lung and prostate cancer cells [150] Decreased exercise capacity, decreased maximum mitochondrial ATP production [151] |
Nephrotoxicity, ototoxicity [152] Peripheral neuropathy [129] Cardiac myopathy [36] Hepatotoxicity [78] |
| Anti-psychotic | Clozapine (black box warning) | Binds serotonin and dopamine receptors with off-target effects on mitochondria [153] | Mitochondrial membrane depolarization, increased inflammatory response, mitochondrial swelling and changes in structure, all which resulted in ATP depletion [49] Oxidation of mitochondrial proteins including malate dehydrogenase and pyruvate kinase [50,154] |
Obesity, metabolic disturbances and increased diabetes risk [50,154] Tardive dyskinesia [155] |
| Antiepileptic | Sodium valporate (black box warning) | Acts to increase the concentration of synaptic GABA with off-target effects on mitochondria [156] | Decreased membrane potential, ATP depletion, increased cell death and reduction in cell number [51] Inhibition of the PDH complex [52] Sequestration of free acetyls CoA [157] |
Hepatotoxicity [51,52,157] Metabolic disturbances [52] Foetal anticonvulsant syndrome [53] |
| Antidepressant-selective serotonin reuptake inhibitor (SSRI) | Sertraline Fluoxetine (black box warning) |
Acts to increase the concentration of serotonin by blocking reabsorption with off-target effects on mitochondria [158] | OXPHOS inhibited in isolated rat brain and liver mitochondria [159,160] Reduced mitochondrial biogenesis [161] Ion compartmentalization [162] Change in morphology to more rounded and shrivelled, indicative of increased caspase 3 activity [163] Decreased respiratory activity [164] Inhibition of complexes I, III and IV in the ETC [163] Down-regulation of ETC proteins [165] |
Hyponatremia, weight gain [166] |
Mitochondrial toxicity is also associated with other drug classes with responses being significantly influenced by patient–patient variability in mitochondrial function. Mitochondrial toxicity is also associated with other drug classes, with the effects being significantly influenced by differences in mitochondrial function caused by patient–patient variability. Patients with diagnosed mitochondrial disorders, in particular those carrying A1555G and C1494T mutations in human mitochondrial 12S rRNA, are acutely sensitive to aminoglycoside antibiotics, which can result in deafness [31]. Age-related deafness (presbyacusis) is extremely common in western societies affecting half of all people over 75 years of age. An impact on mitochondrial function by many common medications on age-related deafness cannot be ruled out [32]. Since the 1920s, cardiovascular diseases have been the leading cause of death globally (World Health Organization). Statins which lower lipid levels, illness and mortality for individuals at high risk have become the most commonly prescribed drug class in the world. However, like other drugs, these are also associated with mitochondrial toxicity [33]. Recent studies have shown the presence of mitochondrial-induced myopathies brought on through reduced respiratory enzyme activity, calcium leakage and ROS-induced oxidative stress in patients being treated with statins [34,35]. The reported incidence varies between 5% and 30% with the milder disease being more common than the very rare rhabdomyolysis reported at 1 in 10 000 patients. Chemotherapeutic agents are renowned for adverse side effects. Drugs must be potent in order to combat the highly resistant cancer cells; however, many chemotherapy agents cause the generation of excessive ROS, which results in oxidative stress and mitochondrial damage [36]. Although this affect limits the efficacious potential of these agents, mitochondrial signalling pathways associated with ROS are essential for cellular function and are linked to various processes including the activity of phosphatases [37], mitochondria perinuclear clustering [38] and longevity at the level of the whole organism in Caenorhabditis elegans [39]. In C. elegans, reduced glucose availability leads to increase mitochondrial respiration and mitochondrial ROS (mtROS) production that actually delays worm aging [40]. Control over mtROS signalling is an exciting new area of research which presents opportunities to regulate appetite and food intake by the actions of uncoupling protein 2 (UCP2) in the brain (reviewed in [41]). UCP2 likely controls mtROS indirectly via alteration of mitochondrial fuel utilization [42,43]. Pharmacological regulation of mtROS will be an important area in the future with opportunities to regulate many cellular pathways including wound healing [44], survival under hypoxia [45], intracellular pH homeostasis [46], innate immunity [47] and cell differentiation [48].
Mitochondrial off-target effects are also observed with anti-psychotic drugs. Anti-psychotic drugs became the standard of care for psychiatric disorders such as schizophrenia and mood disorders in the 1950s with the development of chlorpromazine, the first anti-psychotic. However, adverse effects originating from the mitochondria soon became apparent as metabolic disturbances caused by mitochondrial membrane depolarization and swelling were observed [49,50]. The epileptic drug sodium valproate has well documented mitochondrial toxicity showing respiratory dysfunction in vitro in HEPG2 cells [51] and in vivo where valproate-induced mitochondrial dysfunction has been associated with hepatotoxicity [52] and foetal anticonvulsant syndrome [53]. Mitochondrial linked organ toxicities are the commonest reason for licensed medicines to be given black warnings [54].
Patient-to-patient variation in treatment benefits and adverse toxicity is potentially linked to the variation in mitochondrial function found between individuals and declines with aging as it is also influenced by cell type, gender, state of immunity, and number and severity of pathogenic infections [55,56]. Mitochondria become larger, less numerous and less efficient with age as continuous ROS-associated protein, lipid and nucleic acid damage result in an increase in mitochondrial dysfunction over time [5]. Furthermore, mitochondrial quality control also deteriorates with aging as is observed in the decline of mitophagy in age-related pathologies such as Alzheimer's disease and Parkinson's disease (PD) [57]. The result of this decline is a decreased ability to remove damaged mitochondria and ultimately leads to the accumulation of dysfunctional mitochondria [58].
Genetics also influences susceptibility to mitochondrial and metabolic dysfunction. For example, the mtDNA genetic variant at 16 189 from T to C has been associated with increased oxidative damage, altered antioxidant status and onset of type two diabetes [59–61]. Furthermore, different mtDNA haplogroups have been increasingly associated with individual susceptibility to toxic side effects observed in some patients [62–66]. Haplogroups, distinct patterns in single-nucleotide polymorphisms (SNPs) in mtDNA, naturally arise from human evolution and have been shown to result in different bioenergetic capacities, ROS production and apoptotic capabilities [64]. With these different haplogroups influencing mitochondrial function, it has since been shown that specific haplogroups increase susceptibility to toxic side effects of drug use; for example, the 4917G allele in patients with haplogroup T and the subhaplo group L02a are associated with NRTI-induced peripheral neuropathy [64,65]. The accumulation of SNPs in mtDNA, combined with the use of drugs that affect mitochondrial function, is therefore a major determinant in the development of idiosyncratic drug-induced adverse effects [63].
Opportunities in disease treatment using mitochondrial drug-induced effects
As suggested above, screening drugs for adverse toxicity against mitochondria is vital for their safe use. However, many drugs have been discovered with interesting modulating properties that potentially could prove useful in the clinic or as research tools. The concern in the pharmaceutical industry to screen out drugs with dangerous adverse side effects may have led to the rejection of many beneficial drugs. Research has revealed over the past decade a dependency of many cancer types on mitochondrial function. These dependencies can be shown to be a liability in some cases as selective targeting of the mitochondria has proved efficacious in these studies. Potentially useful new therapeutic cancer agents such as the common antibiotic doxycycline with only mild mitochondrial effects [67,68] might have been discarded at the initial drug-screening phase if put through these. The benefit of drug-targeting mitochondria is particularly relevant to the treatment of cancer. Recent research has demonstrated that cancer cells have a strong reliance on mitochondrial function particularly in the area of metastatic disease [69–72]. The new cancer drug ONC201 [73], which has demonstrated efficacy in cell culture and animal models, is currently being tested against multiple cancer types and could have been discarded if put through a mitochondrial toxicity screen. ONC201 was identified from a screen for compounds that induced the transcription of tumour necrosis-related apoptosis-inducing ligand (TRAIL), an inducer of apoptosis [74]. Follow-up studies discovered that ONC201 did not directly activate TRAIL in all of the cancer cells in which it was effective but was impairing mitochondrial function [75]. Recent data from two studies identified the target of ONC201 as being the mitochondrial CLPP protease which is activated by ONC201 and results in increased cancer cell killing [76,77].
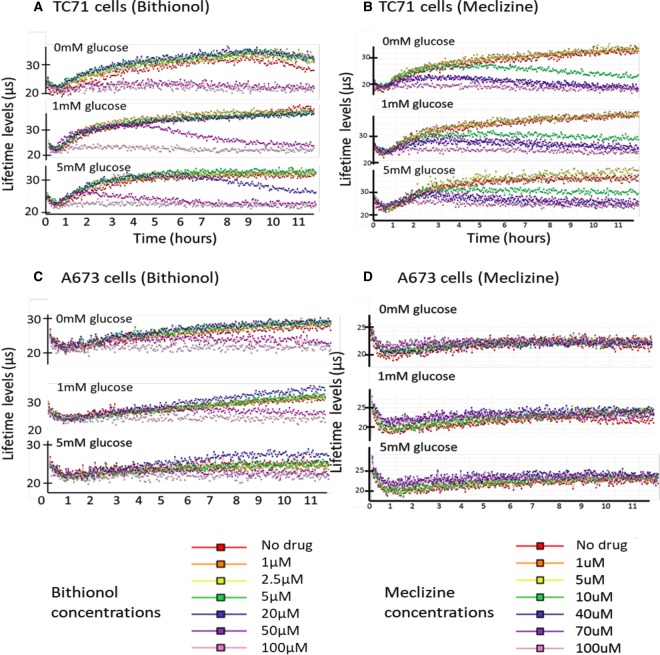
There exists a range of disorders which could potentially benefit from (i) therapeutic-targeting of dysfunctional mitochondria, (ii) modulation of mitochondrial metabolism or (iii) the delivery of antioxidants to reduce oxidative stress-induced damage [78]. The treatments of epilepsy and pyruvate dehydrogenase (PDH) deficiency are good examples of the therapeutic benefits of modulating mitochondrial metabolism, where dietary alterations to a ketogenic diet cause increased fatty acid utilization and alleviation of symptoms [79,80]. Metabolic hormesis is another growing area of interest and is defined by mitochondrial inhibitory agents causing a positive effect on mitochondria when in a low dose range [81]. The general concept related to mitochondrial function is that a little of what is bad for you does you good, analogous to red wine in small doses being beneficial [82]. The idea of metabolic hormesis is demonstrated in Figure 2 where two drugs bithionol and meclizine are added to Ewings sarcoma cancer cell lines. This is an effect we observed with many drugs emphasizing the potential of increasing mitochondrial function at low drug doses. At each glucose condition tested, bithionol and meclizine at higher doses inhibit oxygen consumption (i.e. little change in fluorescence lifetime over time). However, at low drug doses, respiration can be enhanced and the response is shown to vary with both glucose level and cell type. This is an effect we observed with many drugs emphasizing the potential of increasing mitochondrial function at low drug doses. In agreement with this data, meclizine inhibits mitochondrial respiration in vitro but has also shown to provide neuroprotective effects against PD and Huntingdon's models [83–85].
Figure 2. Oxygen consumption of Ewing sarcoma in the presence of Bithionol or Meclizine.
Ewing sarcoma cell lines TC71 and A673 were seeded at 50k cells/well (with and without treatment) in an oil-layered sealed system under varying glucose levels. Fluorescence lifetime was monitored using an oxygen sensing probe (MitoXpress Xtra, Agilent [73]). Vertical axis indicates fluorescent lifetime levels in microseconds with increases, indicating higher oxygen consumption (lower media levels). Horizontal axis indicates time in hours.
Mitochondrial targeting to treat cancer
In 2018, 17 million new cases of cancer were reported worldwide with 9.6 million deaths from the disease [86]. Targeting malignancy and therapy resistance are the major obstacles limiting current treatment strategies. Otto Warburg was the first to suggest mitochondrial involvement in the disease upon the observation that malignant cells have elevated uptake of glucose, which undergoes fermentation to lactate even in the presence of oxygen. This indicates a metabolic switch from OXPHOS to aerobic glycolysis, later named the ‘Warburg effect’ [87], and fuelled the hypothesis that mitochondrial dysfunction was the cause of tumour progression. Positron-emission tomography imaging, which monitors tumour glucose utilization, is the main clinical approach to determine in a non-invasive manner, treatment effectiveness and tumour recurrence [88]. The glucose signature was believed to reflect the glycolytic nature of the tumour; however, recent evidence suggests that this may not be the case, as functional mitochondria are essential for malignant cell survival and oncogenesis [89]. This was highlighted by reduced tumour growth and progression in mice when cancer cells are made mtDNA deficient (ρ0) or when the mtDNA transcription factor A is knocked out causing mtDNA depletion [90]. Other data suggest that mtDNA mutations in cancer are not linked to the development or spread and that cancer cells require the presence of active mitochondria to survive [91]. Targeting cancer mitochondrial function is an exciting area with new drugs identified and several drugs (Metformin; IM156 Immuniomet; IACS10759 MD Anderson CC; AG-636 Agios; CPI-839; CB-839 Calithera) currently being tested in clinical trials across a wide range of tumour types [92–94]. Mitochondrial targeted drugs are presently being explored in combination with chemotherapy [95,96] and radiotherapy [97]. These combinatorial studies will most likely extend to immunomodulatory agents in the near future.
An increasing number of studies addressing the phenomenon of cancer cell and metabolic-reprogramming conclude the essential nature of the switching for both cell survival and resistance to anticancer therapies [70,98,99]. Metabolic switching between OXPHOS, glycolysis, fatty acid oxidation and other carbon sources for energy and biosynthetic needs allows adaptation to drastic changes in the tumour microenvironment [100]. These bioenergetic adaptations depend greatly on mitochondrial function. Complex I's role in the glycolytic switch is one example as it has been found to be essential in several tumour types [101,102]. The anticancer BRAF inhibitor vemurafenib switches cellular metabolism from glycolysis to OXPHOS. This drug, coupled with an electron transport chain (ETC) inhibitor such as honokiol, decreases drug resistance and has activity in vivo against vemurafenib-resistant melanoma [103]. Therefore, combinatorial treatments utilizing both OXPHOS and glycolytic inhibitors provide exciting new therapeutic opportunities [70].
Mitochondrial reprogramming in tumour progression extends beyond changes in mitochondrial bioenergetics. Tumour metastasis, a process implicated in 90% of cancer deaths, is also dictated by changes in mitochondrial function and distribution [104]. Agarwal et al. [105] demonstrated that the exploitation of mitochondrial trafficking is a key hallmark of myc-driven tumour progression, where subcellular mitochondrial trafficking to the cortical cytoskeleton is vital for tumour cell invasion and metastasis. Myc proteins are products of oncogenes, often amplified in human cancers, which promote tumour growth and progression. They have been associated with the control of the gene network of mitochondrial trafficking and changes in the expression of OXPHOS genes and bioenergetics pathways [105]. Mitochondrial trafficking and redistribution is a vital and standard process in healthy neurones, where mitochondria are repositioned to axon terminals to fuel highly energy-intensive processes such as synaptic functions and active growth cones [106]; however, the same protein network is exploited by tumour cells to propel metastasis [107]. The importance of mitochondrial trafficking in myc-driven tumours is further highlighted by the up-regulation of RHOT2, a mitochondrial atypical GTPase [107], and the down-regulation of syntaphilin (SNPH), an inhibitor of mitochondrial trafficking [108] in tumour progression. This recent evidence demonstrates the involvement of mitochondrial dynamics in tumour progression; therefore, the inhibition of myc proteins through doxycycline use, or drug-induced modulation of mitochondrial dynamics may have therapeutic benefit.
Oxidative stress is a hallmark of cancer cells as elevated ROS activates signalling pathways such as the epidermal growth factor receptor and mitogen-activated protein kinase which promote cell growth and proliferation [100,109]. Antioxidant systems in cells, such as the thioredoxin and glutathione system, allow cells to cope with excessive ROS production in both malignant and healthy cells [96]. Elevated ROS in cancer cells is what differentiates malignant cells from healthy cells. Thus, it is thought that the inhibition of antioxidant systems in cancer cells would cause an overload of ROS-induced damage leading to apoptosis in cancer cells only. NSC130362, a small molecule glutathione inhibitor, is one such treatment developed to test this hypothesis. NSC130362 suppressed growth of cancer cell lines and hindered tumour growth in vivo, but did not affect the viability of primary human hepatocytes [110]. Furthermore, the molecule sensitized ex vivo leukaemia cells to other anticancer drugs and potentiated their cytotoxic effects [96]. These results suggest that the induction of additional oxidative stress in tumour cells may provide a therapeutic benefit. Furthermore, using potent antivirals or antibiotics which possess off-target ROS-producing effects in the mitochondria, for example doxorubicin, may cause the accumulation of ROS beyond the antioxidant capacity of malignant cells and result in apoptosis [111–113]. These drugs will induce oxidative stress in healthy cells also; however, the malignant cells already have elevated ROS such that the additional levels will exceed a critical threshold, while healthy cells will survive as oxidative stress is low.
Epigenetic dysregulation is a feature of almost all human cancers [114], and while ROS is a well-known genotoxin at excess levels, other mitochondrial metabolites have also proved to be oncogenic [100]. The tricarboxylic acid cycle metabolites such as succinate, fumarate and 2-hydroxyglutarate all inhibit α-ketoglutarate-dependent enzymes and interfere with their control over epigenetic regulation. Importantly, the result of this interference leads to post-translational protein modifications and the activation of oncogenic transcription factors. These include Jumonji domain histone lysine demethylases, stabilization of hypoxia-inducible factor A and succination of kelch-like ECH-associated protein 1 activating the oncogenic nuclear factor erythroid 2-related protein 2 [100]. Efficient mitochondrial function is dependent on optimal mitochondrial ribosomal translation and assembly of the oxidative phosphorylation complexes. Topoisomerases, which are required for efficient DNA replication and RNA transcription, also play a crucial role in the tumorigenic process. Mitochondrial topoisomerase IB (TOP1MT) is a nuclear encoded, exclusively mitochondrial localized enzyme which is found overexpressed in some tumour types. Baechler et al. [115] showed that HCT116 colon cancer cells had decreased tumour growth and cell proliferation in TOP1MT knockout models, therefore providing further proof of the importance of mitochondrial function in cancer progression.
In summary, many mitochondrial-specific, drug-induced adverse effects have proved useful in reducing tumour growth and sensitizing tumour cells to standard of care therapies. This is due to modulation of mitochondrial metabolism, induction of ROS-mediated apoptosis and regulation of the mitochondrial-induced cell death pathways through mitochondrial outer membrane permeabilization (MOMP) and mitochondrial permeability transition. Therapeutic selectivity remains a main concern when using drugs with mitochondrial toxicity as they have the potential to induce severe and unpleasant clinical symptoms if healthy cells are affected.
Modulation of the innate immune system by mitochondrial manipulation
Mitochondria also play an important role in the immune response such as during activation of the innate response and through direct stimulation of specific pathways. Pathogen clearance relies heavily on various signalling cascades involved in the maturation, expansion and functioning of immune cells. As these processes require significant amounts of energy, it is not surprising that mitochondria are involved in the innate immune system through their role in cellular bioenergetics and signalling. An important signalling role of mitochondria has already been well established, for example during key steps of apoptosis and autophagy mediated through the generation of ROS and the regulation of calcium [116]. Mitochondria exert their modulatory effects on the innate immune system primarily through various cell-signalling events, usually activated on the entry of pathogenic RNA, dsDNA and dsRNA into the cell. In addition, a recent paper by Dhir et al. [117] showed that mitochondrial derived dsRNA can induce antiviral signalling by triggering a type I interferon response. In both the innate and adaptive immune systems, rewiring of mitochondrial function is required for optimal function of both phagocytic cells and lymphocytes. Indeed, naive T-cells must switch from a metabolically quiescent to a metabolically active state in order to become fully activated. This increased metabolic activity is achieved through enhanced mitochondrial metabolism and indicates that the important role the organelle plays in the immune response [118].
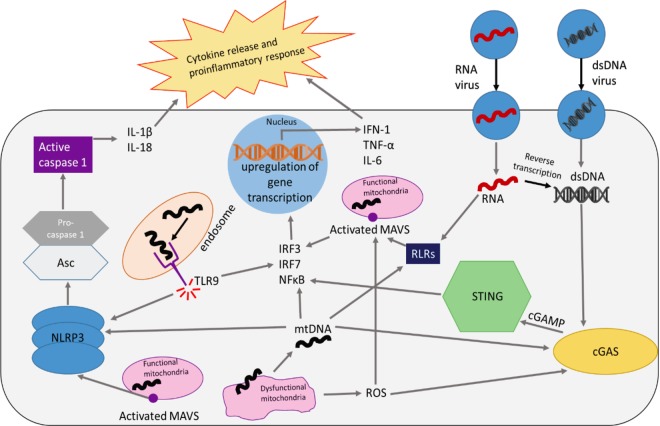
Furthermore, defective mitochondria can activate immune responses through a variety of different mechanisms (Figure 3). The cytosolic release of mtDNA can exert potent immunostimulatory effects. Mitochondrial dysfunction or MOMP caused by pathogenic infection or toxic drugs can result in the release of mtDNA [106,107], which acts as a damage-associated molecular pattern and engages with pattern recognition receptors (PRRs) [108] to activate immune responses. The predominant immunomodulatory action of cytosolic mtDNA is through the activation of the STING pathway, a critical antiviral regulatory system activated by viral dsDNA during infection [118]. During an infection, viral pathogens can cause mitochondrial dysfunction within infected cells. This is achieved by viral interference with mitochondrial signalling pathways and dynamics to favour viral proliferation and commonly occurs through the inhibition of apoptosis or the innate immune response [119]. The pathogen-induced dysfunction increases the production of ROS or the release of mtDNA, where both may act as mediators for the STING pathway [120]. The activation of the STING pathway leads to increased expression of IRF3, IRF7 and nuclear factor kappa-light-chain-enhancer of activated B cells (NFκB) transcription factors that control the expression of type I interferons (IFN-I) and interferon-stimulated genes, which directly restrict viral replication [16,57,121]. Drugs which induce mtDNA release or enhance ROS may therefore mimic this effect and lead to up-regulation of antiviral pathways independent of infection, making them useful for both priming the innate immune system or for increasing the efficiency of viral clearance. mtDNA also contains a regulatory D-loop which allows it to act as a ligand for PRRs causing the activation of immune responses [57,118,122]. In endosomal vesicles, this orchestrates signalling through Toll-like receptor 9 (TLR9) for the activation of both pro-inflammatory and antiviral effector responses in a variety of human immune cells [123]. TLR9 is also expressed on the outer surface of cells, allowing free mtDNA present in extracellular fluid to also activate the pathway. Similar to the STING pathway, TLR9 signalling can also activate IRF7 and NFκB transcription factors. Among the inflammatory cytokine proteins up-regulated are TNF-α (tumour necrosis factor alpha) and IFN-I (interferon type I) which increase both pro-inflammatory and antiviral responses.
Figure 3. Cellular signalling pathways in response to pathogenic viral infection or mtDNA release.
Antiviral pathways can be stimulated by both RNA and dsDNA from receptor-mediated fusion events or endocytosis. These foreign nucleic acids interact with pattern recognition receptors, such as RIG-I like receptors (RLRs), or with cGAS (cyclic GMP-AMP synthase) which initiates the STING (Stimulator of Interferon Genes) antiviral response pathway. mtDNA acts as a ligand for many immune receptors so is capable of activating both cGAS and RLRs as well as the NLRP3 (nod-like receptor family pyrin domain containing 3) inflammasome for the up-regulation of cytokine release and a pro-inflammatory response.
The activation of the NLRP3 inflammasome is also a key pathway in mtDNA-dependent immune responses. Oxidized mtDNA is able to directly bind to the inflammasome to induce IL-1β production [124]. Furthermore, ROS from dysfunctional mitochondria are also potent activators of the inflammasome. This was demonstrated in vitro as rotenone and antimycin A treatments produced both increased mtROS levels and NLRP3 inflammasome activity [125–127]. The activation of the inflammasome causes cleavage-mediated release of caspase-1 from procaspase-1 resulting in the activation of IL-1B and IL-18, which contribute to an increased pro-inflammatory response. Induction of mild-to-moderate mitochondrial dysfunction through drug therapy could increase cytosolic mtDNA and ROS production from impaired ETC function. These changes could potentially enhance the activation of TLR9, STING and NLRP3 inflammasome-regulated pathways causing increased inflammatory responses and potentially more efficient pathogen and infection clearance. However, care must be taken if using drug therapy to enhance an immune response as there exist a chance of initiating a pro-inflammatory state.
As just described, recent studies have revealed an important role for mitochondria in the immune response. There is much to understand in this emerging field as the specific functional role that mitochondria assume is immune cell specific. Because these roles manifest themselves through different forms such as enhanced/reduced ROS or altered mtDNA copy number-modulation of mitochondrial morphology, a variety of opportunities are thus presented for drug manipulation of mitochondria. Manipulating mtROS production, for example, has the potential to drive an increased immune response through both increased innate immune signalling and increased release of mtDNA for PRR stimulation. Up-regulating immune activation via altering bioenergetics or increasing mtDNA release/sensing could be beneficial not only in clearing both viral and bacterial infections, but also be effective tools in engaging the immune system to destroy cancer cells. Indeed, several drugs that increase STING activation are being developed or are in clinical trials for cancer therapy. These drugs perhaps may be paired with other chemotherapeutics that cause mitochondrial dysfunction, leading to the increased sensing of mtDNA and other mitochondrial ligands to augment anti-tumour immunity at both the innate and adaptive levels. On the contrary, long-term drug-induced mtDNA depletion has been shown to inhibit interferon and PRR-mediated signalling and therefore can blunt innate immune responses [128]. Therapeutics that down modulate mitochondrial function in immune cells may be beneficial in diseases where hyper-activation of the immune system causes life-threatening symptoms, such as autoimmunity and sepsis. Thus, future research into compounds that dampen mitochondrial function or improve mitochondrial quality control may yield new therapies for a wide array of immunological and inflammatory disorders.
Conclusions
Much of the evidence to date indicates that a variety of drugs, particularly antivirals and chemotherapy agents, are capable of inducing mitochondrial dysfunction through mtDNA depletion, increased ROS production and uncoupled OXPHOS [26,129,130]. Mitochondrial dysfunction results from off-target effects from these drugs rather than being the main mode of action; however, we have shown that modulating mitochondrial function could be beneficial in the treatment of a variety of diseases such as cancer, diabetes and chronic viral infection. This can be achieved through alterations in mtDNA biogenesis, metabolic rewiring and up-regulation of the immune system. The great challenge to achieve beneficial effects will selectivity and how to maintain mitochondrial outputs in normal healthy tissue while modulating mitochondrial function, or pathogen levels in target tissues.
Perspectives
Importance of the field: Understanding the mechanisms of drug-induced mitochondrial toxicity is a highly important field for the development of new therapeutic agents with lower toxicity, as this is vital for patient safety and the development of successful therapeutics. Exploring opportunities of the off-target effects of current drugs is just as vital. Advancements in disease treatment in the last century have left few new drug targets available; therefore, rethinking new uses for the current drugs available is crucial.
Current thinking: Overall, we believe that there is considerable evidence that current drugs carrying black box warnings of mitochondrial toxicity are a growing opportunity. Drugs indirectly affecting mitochondria have been recently used as a main mode of action to treat diseases such as type 2 diabetes and cancer, as well as up-regulating the immune system to clear infection with promising success; however, considerable caution must be taken when inducing mitochondrial dysfunction for disease treatment because of the vital dependency normal cells have on mitochondrial function.
Future direction: Presently, most drug therapy literature rightfully keys in on adverse side effects and the avoidance of mitochondrial toxicity. It is important going forward that we better understand the role and function of mitochondria in both health and the disease states in order to better take advantage of opportunities and potential therapeutic benefits of mitochondrial and metabolic manipulation
Abbreviations
- ATP
adenosine triphosphate
- ETC
electron transport chain
- HIV
human immunodeficiency virus
- IFN-I
type I interferons
- MOMP
mitochondrial outer membrane permeabilization
- mtDNA
mitochondrial DNA
- mtROS
mitochondrial ROS
- NRTIs
nucleoside reverse transcriptase inhibitors
- OXPHOS
oxidative phosphorylation
- PD
Parkinson's disease
- PDH
pyruvate dehydrogenase
- PRRs
pattern recognition receptors
- RNA
ribonucleic acid
- ROS
reactive oxygen species
- SNPs
single-nucleotide polymorphisms
- TLR9
Toll-like receptor 9
- TOP1MT
topoisomerase IB
- TRAIL
tumour necrosis-related apoptosis-inducing ligand
- UCP2
uncoupling protein 2.
Author Contribution
All authors contributed to, read and approved the final version of the manuscript.
Funding
M.S. was supported by the ME Association
Competing Interests
The Authors declare that there are no competing interests associated with the manuscript.
References
- 1.Dudkina N., Kouřil R., Peters K., Braun H. and Boekema E. (2010) Structure and function of mitochondrial supercomplexes. Biochim. Biophys. Acta 1797, 664–670 10.1016/j.bbabio.2009.12.013 [DOI] [PubMed] [Google Scholar]
- 2.Taanman J. (1999) The mitochondrial genome: structure, transcription, translation and replication. Biochim. Biophys. Acta 1410, 103–123 10.1016/S0005-2728(98)00161-3 [DOI] [PubMed] [Google Scholar]
- 3.D'Erchia A., Atlante A., Gadaleta G., Pavesi G., Chiara M., De Virgilio C. et al. (2015) Tissue-specific mtDNA abundance from exome data and its correlation with mitochondrial transcription, mass and respiratory activity. Mitochondrion 20, 13–21 10.1016/j.mito.2014.10.005 [DOI] [PubMed] [Google Scholar]
- 4.Brinkman K., ter Hofstede H., Burger D., Smeitink J. and Koopmans P. (1998) Adverse effects of reverse transcriptase inhibitors. AIDS 12, 1735–1744 10.1097/00002030-199814000-00004 [DOI] [PubMed] [Google Scholar]
- 5.Rose G., Santoro A. and Salvioli S. (2017) Mitochondria and mitochondria-induced signalling molecules as longevity determinants. Mech. Ageing Dev. 165, 115–128 10.1016/j.mad.2016.12.002 [DOI] [PubMed] [Google Scholar]
- 6.Wai T., Ao A., Zhang X., Cyr D., Dufort D. and Shoubridge E. (2010) The role of mitochondrial DNA copy number in mammalian fertility. Biol. Reprod. 83, 52–62 10.1095/biolreprod.109.080887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Benard G., Faustin B., Passerieux E., Galinier A., Rocher C., Bellance N. et al. (2006) Physiological diversity of mitochondrial oxidative phosphorylation. Am. J. Physiol. Cell Physiol. 291, 1172–1182 10.1152/ajpcell.00195.2006 [DOI] [PubMed] [Google Scholar]
- 8.Samuels D.C., Wonnapinij P. and Chinnery P.F. (2013) Preventing the transmission of pathogenic mitochondrial DNA mutations: can we achieve long-term benefits from germ-line gene transfer? Hum. Reprod. 28, 554–559 10.1093/humrep/des439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Course M.W.X. (2016) Transporting mitochondria in neurons. F1000Research 5, 1735 10.12688/f1000research.7864.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sheng Z.H. and Cai Q. (2012) Mitochondrial transport in neurons: impact on synaptic homeostasis and neurodegeneration. Nat. Rev. Neurosci. 13, 77–93 10.1038/nrn3156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Magrané J. and Manfredi G. (2009) Mitochondrial function, morphology, and axonal transport in amyotrophic lateral sclerosis. Antioxid. Redox. Signal. 11, 1615–1626 10.1089/ars.2009.2604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Reddy P.H. and Shirendeb U.P. (2012) Mutant huntingtin, abnormal mitochondrial dynamics, defective axonal transport of mitochondria, and selective synaptic degeneration in Huntington's disease. Biochim. Biophys. Acta 1822, 101–110 10.1016/j.bbadis.2011.10.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lemasters J., Theruvath T., Zhong Z. and Nieminen A. (2009) Mitochondrial calcium and the permeability transition in cell death. Biochim. Biophys. Acta 1787, 1395–1401 10.1016/j.bbabio.2009.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Celsi F., Pizzo P., Brini M., Leo S., Fotino C., Pinton P. et al. (2009) Mitochondria, calcium and cell death: a deadly triad in neurodegeneration. Biochim. Biophys. Acta 1787, 335–344 10.1016/j.bbabio.2009.02.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stehling O. and Lill R. (2013) The role of mitochondria in cellular iron-sulfur protein biogenesis: mechanisms, connected processes, and diseases. Cold Spring Harb. Perspect. Biol. 5, a011312 10.1101/cshperspect.a011312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.West A.P. and Shadel G. (2017) Mitochondrial DNA in innate immune responses and inflammatory pathology. Nat. Rev. Immunol. 17, 363–375 10.1038/nri.2017.21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Youle R. (2019) Mitochondria — striking a balance between host and endosymbiont. Science 365, 655–662 10.1126/science.aaw9855 [DOI] [PubMed] [Google Scholar]
- 18.Kapnick S.M., Pacheco S.E. and McGuire P.J. (2018) The emerging role of immune dysfunction in mitochondrial diseases as a paradigm for understanding immunometabolism. Metabolism 81, 97–112 10.1016/j.metabol.2017.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pernas L. and Scorrano L. (2016) Mito-morphosis: mitochondrial fusion, fission, and cristae remodeling as key mediators of cellular function. Annu. Rev. Physiol. 78, 505–531 10.1146/annurev-physiol-021115-105011 [DOI] [PubMed] [Google Scholar]
- 20.Williams J.A. and Ding W.X. (2018) Mechanisms, pathophysiological roles and methods for analyzing mitophagy — recent insights. Biol. Chem. 399, 147–178 10.1515/hsz-2017-0228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Diot A., Morten K. and Poulton J. (2016) Mitophagy plays a central role in mitochondrial ageing. Mamm. Genome 27, 381–395 10.1007/s00335-016-9651-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brown E., Lewin A. and Ash J. (2018) Mitochondria: potential targets for protection in age-related macular degeneration. Adv. Exp. Med. Biol. 1074, 11–17 10.1007/978-3-319-75402-4_2 [DOI] [PubMed] [Google Scholar]
- 23.Guan R., Zou W., Dai X., Yu X., Liu H., Chen Q. et al. (2018) Mitophagy, a potential therapeutic target for stroke. J. Biomed. Sci. 25, article no. 87 10.1186/s12929-018-0487-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dombi E., Mortiboys H. and Poulton J. (2019) Modulating mitophagy in mitochondrial disease. Curr. Med. Chem. 25, 5597–5612 10.2174/0929867324666170616101741 [DOI] [PubMed] [Google Scholar]
- 25.Berdis A. (2018) DNA polymerases as therapeutic targets. Biochemistry 47, 8253–8260 10.1021/bi801179f [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wallace K. (2008) Mitochondrial off targets of drug therapy. Trends Pharmacol. Sci. 29, 361–366 10.1016/j.tips.2008.04.001 [DOI] [PubMed] [Google Scholar]
- 27.Montessori V., Press N., Harris M., Akagi L. and Montaner J.S.G. (2004) Adverse effects of antiretroviral therapy for HIV infection. CMAJ 170, 229–238 [PMC free article] [PubMed] [Google Scholar]
- 28.Lee H., Hanes J. and Johnson K. (2003) Toxicity of nucleoside analogues used to treat AIDS and the selectivity of the mitochondrial DNA polymerase. Biochemistry 42, 14711–14719 10.1021/bi035596s [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Birkus G., Hitchcock M. and Cihlar T. (2002) Assessment of mitochondrial toxicity in human cells treated with tenofovir: comparison with other nucleoside reverse transcriptase inhibitors. Antimicrob. Agents Chemother. 46, 716–723 10.1128/AAC.46.3.716-723.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.U.S.F.A.D. Administration (2019) Antiretroviral drugs used in the treatment of HIV infection, https://www.fda.gov/patients/hiv-treatment/antiretroviral-drugs-used-treatment-hiv-infection [cited 18 June 2019].
- 31.Qian Y. and Guan M.X. (2009) Interaction of aminoglycosides with human mitochondrial 12S rRNA carrying the deafness-associated mutation. Antimicrob. Agents Chemother. 53, 4612–4618 10.1128/AAC.00965-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.NIDCD (2019) Age-related hearing loss , https://www.nidcd.nih.gov/health/age-related-hearing-loss [cited 4 July 2019].
- 33.Golomb B.A. and Evans M.A. (2018) Statin adverse effects. Am. J. Cardiovasc. Drugs 8, 373–418 10.2165/0129784-200808060-00004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.du Souich P., Roederer G. and Dufour R. (2019) Myotoxicity of statins: mechanism of action. Pharmacol. Ther. 175, 1–16 10.1016/j.pharmthera.2017.02.029 [DOI] [PubMed] [Google Scholar]
- 35.Ramachandran R. and Wierzbicki A.S. (2017) Statins, muscle disease and mitochondria. J. Clin. Med. 6, 75 10.3390/jcm6080075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nicolson G. and Conklin K. (2007) Reversing mitochondrial dysfunction, fatigue and the adverse effects of chemotherapy of metastatic disease by molecular replacement therapy. Clin. Exp. Metastasis 25, 161–169 10.1007/s10585-007-9129-z [DOI] [PubMed] [Google Scholar]
- 37.Finkel T. (2012) Signal transduction by mitochondrial oxidants. J. Biol. Chem. 287, 4434–4440 10.1074/jbc.R111.271999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Al-Mehdi A.B., Pastukh V.M., Swiger B.M., Reed D.J., Patel M.R., Bardwell G.C. et al. (2012) Perinuclear mitochondrial clustering creates an oxidant-rich nuclear domain required for hypoxia-induced transcription. Sci. Signal. 5, ra47 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ristow M. and Zarse K. (2010) How increased oxidative stress promotes longevity and metabolic health: the concept of mitochondrial hormesis (mitohormesis). Exp. Gerontol. 45, 410–418 10.1016/j.exger.2010.03.014 [DOI] [PubMed] [Google Scholar]
- 40.Schulz T.J., Zarse K., Voigt A., Urban N., Birringer M. and Ristow M. (2007) Glucose restriction extends Caenorhabditis elegans life span by inducing mitochondrial respiration and increasing oxidative stress. Cell Metab. 6, 280–293 10.1016/j.cmet.2007.08.011 [DOI] [PubMed] [Google Scholar]
- 41.Diano S. and Horvath T.L. (2012) Mitochondrial uncoupling protein 2 (UCP2) in glucose and lipid metabolism. Trends Mol. Med. 18, 52–58 10.1016/j.molmed.2011.08.003 [DOI] [PubMed] [Google Scholar]
- 42.Pecqueur C., Alves-Guerra C., Ricquier D. and Bouillaud F. (2009) UCP2, a metabolic sensor coupling glucose oxidation to mitochondrial metabolism? IUBMB Life 61, 762–767 10.1002/iub.188 [DOI] [PubMed] [Google Scholar]
- 43.Vozza A., Parisi G., De Leonardis F., Lasorsa F.M., Castegna A., Amorese D. et al. (2014) UCP2 transports C4 metabolites out of mitochondria, regulating glucose and glutamine oxidation. Proc. Natl Acad. Sci. U.S.A. 111, 960–965 10.1073/pnas.1317400111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Xu S. and Chisholm A.D. (2014) C. elegans epidermal wounding induces a mitochondrial ROS burst that promotes wound repair. Dev. Cell 31, 48–60 10.1016/j.devcel.2014.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Schieber M. and Chandel N.S. (2014) TOR signaling couples oxygen sensing to lifespan in C. elegans. Cell Rep. 9, 9–15 10.1016/j.celrep.2014.08.075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Johnson D., Allman E. and Nehrke K. (2012) Regulation of acid-base transporters by reactive oxygen species following mitochondrial fragmentation. Am. J. Physiol. Cell Physiol. 302, C1045–C1054 10.1152/ajpcell.00411.2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.West A.P., Shadel G.S. and Ghosh S. (2011) Mitochondria in innate immune responses. Nat. Rev. Immunol. 11, 389–402 10.1038/nri2975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hamanaka R.B., Glasauer A., Hoover P., Yang S., Blatt H., Mullen A.R. et al. (2013) Mitochondrial reactive oxygen species promote epidermal differentiation and hair follicle development. Sci. Signal. 6, ra8 10.1126/scisignal.2003638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Contreras-Shannon V., Heart D., Paredes R., Navaira E., Catano G., Maffi S. et al. (2013) Clozapine-induced mitochondria alterations and inflammation in brain and insulin-responsive cells. PLoS ONE 8, e59012 10.1371/journal.pone.0059012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Baig M., Navaira E., Escamilla M., Raventos H. and Walss-Bass C. (2010) Clozapine treatment causes oxidation of proteins involved in energy metabolism in lymphoblastoid cells: a possible mechanism for antipsychotic-induced metabolic alterations. J. Psychiatr. Pract. 16, 325–333 10.1097/01.pra.0000388627.36781.6a [DOI] [PubMed] [Google Scholar]
- 51.Komulainen T., Lodge T., Hinttala R., Bolszak M., Pietilä M., Koivunen P. et al. (2015) Sodium valproate induces mitochondrial respiration dysfunction in HepG2 in vitro cell model. Toxicol. Appl. Pharmacol. 331, 47–56 PMID: [DOI] [PubMed] [Google Scholar]
- 52.Silva M., Ruiter J., IJlst L., Jakobs C., Duran M., de Almeida I. et al. (1997) Valproate inhibits the mitochondrial pyruvate-driven oxidative phosphorylation in vitro. J. Inherit. Metab. Dis. 20, 397–400 10.1023/A:1005398516208 [DOI] [PubMed] [Google Scholar]
- 53.Kulkarni M., Zaheeruddin M., Shenoy N. and Vani H. (2006) Fetal valproate syndrome. Indian J. Pediatr. 73 [DOI] [PubMed] [Google Scholar]
- 54.Will Y. and Dykens J. (2014) Mitochondrial toxicity assessment in industry — a decade of technology development and insight. Expert. Opin. Drug. Metab. Toxicol. 10, 1061–1067 10.1517/17425255.2014.939628 [DOI] [PubMed] [Google Scholar]
- 55.Matthews T. and Boehme R. (1988) Antiviral activity and mechanism of action of ganciclovir. Clin. Infect. Dis. 10, 490–494 10.1093/clinids/10.Supplement_3.S490 [DOI] [PubMed] [Google Scholar]
- 56.Margolis A., Heverling H., Pham P. and Stolbach A. (2013) A review of the toxicity of HIV medications. J. Med. Toxicol. 10, 26–39 10.1007/s13181-013-0325-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Fang C., Wei X. and Wei Y. (2015) Mitochondrial DNA in the regulation of innate immune responses. Protein Cell 7, 11–16 10.1007/s13238-015-0222-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Srivastava S. (2017) The mitochondrial basis of aging and age-related disorders. Genes 8, 398 10.3390/genes8120398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lin T., Chen S., Wang P., Wei Y., Lee C., Chen T. et al. (2005) Increased oxidative damage with altered antioxidative status in type 2 diabetic patients harboring the 16189T to C variant of mitochondrial DNA. Ann. N. Y. Acad. Sci. 1042, 64–69 10.1196/annals.1338.007 [DOI] [PubMed] [Google Scholar]
- 60.Pinti M., Fink G., Hathaway Q., Durr A., Kunovac A. and Hollander J. (2019) Mitochondrial dysfunction in type 2 diabetes mellitus: an organ-based analysis. Am. J. Physiol.-Endocrinol. Metab. 316, E268–E285 10.1152/ajpendo.00314.2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Park K. (2016) Role of mitochondrial DNA variation in the pathogenesis of diabetes mellitus. Front. Biosci. 21, 1151–1167 10.2741/4447 [DOI] [PubMed] [Google Scholar]
- 62.Pacheu-Grau D., Gomez-Duran A., Iglesias E., Lopez-Gallardo E., Montoya J. and Ruiz-Pesini E. (2012) Mitochondrial antibiograms in personalized medicine. Hum. Mol. Genet. 22, 1132–1139 10.1093/hmg/dds517 [DOI] [PubMed] [Google Scholar]
- 63.Pereira C., Oliveira P., Will Y. and Nadanaciva S. (2012) Mitochondrial bioenergetics and drug-induced toxicity in a panel of mouse embryonic fibroblasts with mitochondrial DNA single nucleotide polymorphisms. Toxicol. Appl. Pharmacol. 264, 167–181 10.1016/j.taap.2012.07.030 [DOI] [PubMed] [Google Scholar]
- 64.Canter J., Haas D., Kallianpur A., Ritchie M., Robbins G., Shafer R. et al. (2007) The mitochondrial pharmacogenomics of haplogroup T: MTND2*LHON4917G and antiretroviral therapy-associated peripheral neuropathy. Pharmacogenomics J. 8, 71–77 10.1038/sj.tpj.6500470 [DOI] [PubMed] [Google Scholar]
- 65.Kampira E., Kumwenda J., van Oosterhout J. and Dandara C. (2013) Mitochondrial DNA subhaplogroups L0a2 and L2a modify susceptibility to peripheral neuropathy in Malawian adults on stavudine containing highly active antiretroviral therapy. J. Acquir. Immune Defic. Syndr. 63, 647–652 10.1097/QAI.0b013e3182968ea5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Garrabou G., Soriano À., Pinós T., Casanova-Mollà J., Pacheu-Grau D., Morén C. et al. (2017) Influence of mitochondrial genetics on the mitochondrial toxicity of linezolid in blood cells and skin nerve fibers. Antimicrob. Agents Chemother. 61, e00542–e00517 10.1128/AAC.00542-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ahler E., Sullivan W., Cass A., Braas D., York A., Bensinger S. et al. (2013) Doxycycline alters metabolism and proliferation of human cell lines. PLoS ONE 8, e64561 10.1371/journal.pone.0064561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Son K F.S., Iida T., Furukawa K., Fujita T., Yamada H., Chiao P.J. et al. (2009) Doxycycline induces apoptosis in PANC-1 pancreatic cancer cells. Anticancer Res. 29, 3995–4003 [PubMed] [Google Scholar]
- 69.Potter M., Newport E. and Morten K. (2016) The Warburg effect: 80 years on. Biochem. Soc. Trans. 44, 1499–1505 10.1042/BST20160094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hirpara J., Eu J., Tan J., Wong A., Clement M., Kong L. et al. (2018) Metabolic reprogramming of oncogene-addicted cancer cells to OXPHOS as a mechanism of drug resistance. Redox Biol. 101076 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Tan A.S., Baty J.W., Dong L.F., Bezawork-Geleta A., Endaya B., Goodwin J. et al. (2015) Mitochondrial genome acquisition restores respiratory function and tumorigenic potential of cancer cells without mitochondrial DNA. Cell Metab. 6, 81–94 10.1016/j.cmet.2014.12.003 [DOI] [PubMed] [Google Scholar]
- 72.Kelley L.C., Chi Q., Cáceres R., Hastie E., Schindler A.J., Jiang Y. et al. (2019) Adaptive F-actin polymerization and localized ATP production drive basement membrane invasion in the absence of MMPs. Dev. Cell 48, 313–328 10.1016/j.devcel.2018.12.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Oncoceutics ONC201 clinical trials 2019, https://oncoceutics.com [cited 9 July 2019]
- 74.Allen J., Krigsfeld G., Mayes P., Patel L., Dicker D., Patel A. et al. (2013) Dual inactivation of Akt and ERK by TIC10 signals Foxo3a nuclear translocation, TRAIL gene induction, and potent antitumor effects. Sci. Transl. Med. 5, 171ra17 10.1126/scitranslmed.3004828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Greer Y., Porat-Shliom N., Nagashima K., Stuelten C., Crooks D., Koparde V. et al. (2018) ONC201 kills breast cancer cells in vitro by targeting mitochondria. Oncotarget 9 10.18632/oncotarget.24862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Graves P., Aponte-Collazo L., Fennell E., Graves A., Hale A., Dicheva N. et al. (2019) Mitochondrial protease ClpP is a target for the anticancer compounds ONC201 and related analogues. ACS Chem. Biol. 14, 1020–1029 10.1021/acschembio.9b00222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ishizawa J., Zarabi S., Davis R., Halgas O., Nii T., Jitkova Y. et al. (2019) Mitochondrial ClpP-mediated proteolysis induces selective cancer cell lethality. Cancer Cell 35, 721–737 10.1016/j.ccell.2019.03.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ribeiro M., Castro e Santos A. and Custódio J., (2015) Mitochondrial dysfunction on the toxic effects of anticancer agents — from lab bench to bedside In Toxicology Studies — Cells, Drugs and Environment (Andreazza, A.C. and Scola, G. eds), pp. 23-59, IntechOpen [Google Scholar]
- 79.Liu H., Yang Y., Wang Y., Tang H., Zhang F., Zhang Y. et al. (2018) Ketogenic diet for treatment of intractable epilepsy in adults: a meta-analysis of observational studies. Epilepsia Open 3, 9–17 10.1002/epi4.12098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Sofou K., Dahlin M., Hallböök T., Lindefeldt M., Viggedal G. and Darin N. (2017) Ketogenic diet in pyruvate dehydrogenase complex deficiency: short- and long-term outcomes. J. Inherit. Metab. Dis. 40, 237–245 10.1007/s10545-016-0011-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Nunn A., Guy G. and Bell J. (2016) The quantum mitochondrion and optimal health. Biochem. Soc. Trans. 44, 1101–1110 10.1042/BST20160096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Artero A., Artero A., Tarín J.J. and Cano A. (2015) The impact of moderate wine consumption on health. Maturitas 80, 3–13 10.1016/j.maturitas.2014.09.007 [DOI] [PubMed] [Google Scholar]
- 83.Gohil V., Offner N., Walker J., Sheth S., Fossale E., Gusella J. et al. (2010) Meclizine is neuroprotective in models of Huntington's disease. Hum. Mol. Genet. 20, 294–300 10.1093/hmg/ddq464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Gohil V., Zhu L., Baker C., Cracan V., Yaseen A., Jain M. et al. (2013) Meclizine inhibits mitochondrial respiration through direct targeting of cytosolic phosphoethanolamine metabolism. J. Biol. Chem. 288, 35387–35395 10.1074/jbc.M113.489237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Hong C., Chau K. and Schapira A. (2016) Meclizine-induced enhanced glycolysis is neuroprotective in Parkinson disease cell models. Sci. Rep. 6, 25344 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Cancer Research UK. (2019) Worldwide cancer statistics, https://www.cancerresearchuk.org/health-professional/cancer-statistics/worldwide-cancer [cited 13 March 2019]. [Google Scholar]
- 87.Warburg O. (1927) The metabolism of tumors in the body. J. Gen. Physiol. 8, 519–530 10.1085/jgp.8.6.519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Malviya G. and Nayak T. (2014) PET imaging to monitor cancer therapy. Curr. Pharm. Biotechnol. 14, 669–682 10.2174/1389201014666131226104750 [DOI] [PubMed] [Google Scholar]
- 89.Pustylnikov S., Costabile F., Beghi S. and Facciabene A. (2018) Targeting mitochondria in cancer: current concepts and immunotherapy approaches. Transl. Res. 202, 35–51 10.1016/j.trsl.2018.07.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Wallace D. (2012) Mitochondria and cancer. Nat. Rev. Cancer 12, 685–698 10.1038/nrc3365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Ju Y., Alexandrov L., Gerstung M., Martincorena I., Nik-Zainal S., Ramakrishna M. et al. (2014) Origins and functional consequences of somatic mitochondrial DNA mutations in human cancer. eLife 3, e02935 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Shi Y., Lim S., Liang Q., Iyer S., Wang H., Wang Z. et al. (2019) Gboxin is an oxidative phosphorylation inhibitor that targets glioblastoma. Nature 567, 341–346 10.1038/s41586-019-0993-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Molina J., Sun Y., Protopopova M., Gera S., Bandi M., Bristow C. et al. (2018) An inhibitor of oxidative phosphorylation exploits cancer vulnerability. Nat. Med. 24, 1036–1046 10.1038/s41591-018-0052-4 [DOI] [PubMed] [Google Scholar]
- 94.Zhang L., Yao Y., Zhang S., Liu Y., Guo H., Ahmed M. et al. (2019) Metabolic reprogramming toward oxidative phosphorylation identifies a therapeutic target for mantle cell lymphoma. Sci. Transl. Med. 11, eaau1167 10.1126/scitranslmed.aau1167 [DOI] [PubMed] [Google Scholar]
- 95.Liu Y Z.X., Zhou M., Nan X., Chen X. and Zhang X. (2017) Mitochondrial-targeting lonidamine-doxorubicin nanoparticles for synergistic chemotherapy to conquer drug resistance. ACS Appl. Mater Interfaces 9, 43498–43507 10.1021/acsami.7b14577 [DOI] [PubMed] [Google Scholar]
- 96.Rozanov D., Cheltsov A., Nilsen A., Boniface C., Forquer I., Korkola J. et al. (2019) Targeting mitochondria in cancer therapy could provide a basis for the selective anti-cancer activity. PLoS ONE 14, e0205623 10.1371/journal.pone.0205623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ashton T., Fokas E., Kunz-Schughart L., Folkes L., Anbalagan S., Huether M. et al. (2016) The anti-malarial atovaquone increases radiosensitivity by alleviating tumour hypoxia. Nat. Commun. 7 10.1038/ncomms12308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Andrzejewski S., Siegel P. and St-Pierre J. (2018) Metabolic profiles associated with metformin efficacy in cancer. Front. Endocrinol. 9, 372 10.3389/fendo.2018.00372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Lee M., Hirpara J., Eu J., Sethi G., Wang L., Goh B. et al. (2018) Targeting STAT3 and oxidative phosphorylation in oncogene-addicted tumors. Redox Biol. 101073 10.1016/j.redox.2018.101073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Porporato P., Filigheddu N., Pedro J., Kroemer G. and Galluzzi L. (2017) Mitochondrial metabolism and cancer. Cell Res. 28, 265–280 10.1038/cr.2017.155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Chavez A., Miranda L., Pichiule P. and Chavez J. (2008) Mitochondria and hypoxia-induced gene expression mediated by hypoxia-inducible factors. Ann. N. Y. Acad. Sci. 1147, 312–320 10.1196/annals.1427.021 [DOI] [PubMed] [Google Scholar]
- 102.Calabrese C., Iommarini L., Kurelac I., Calvaruso M., Capristo M., Lollini P. et al. (2013) Respiratory complex I is essential to induce a Warburg profile in mitochondria-defective tumor cells. Cancer Metab. 1, 11 10.1186/2049-3002-1-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Bonner M., Karlsson I., Rodolfo M., Arnold R., Vergani E. and Arbiser J. (2016) Honokiol bis-dichloroacetate (Honokiol DCA) demonstrates activity in vemurafenib-resistant melanoma in vivo. Oncotarget 7 10.18632/oncotarget.7289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Altieri D.C. (2019) Mitochondrial dynamics and metastasis. Cell. Mol. Life Sci. 76, 827–835 10.1007/s00018-018-2961-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Agarwal E., Altman B.J., Ho Seo J., Bertolini I., Ghosh J.C., Kaur A. et al. (2019) Myc regulation of a mitochondrial trafficking network mediates tumor cell invasion and metastasis. Mol. Cell. Biol. 39, e00109–e00119 10.1128/MCB.00109-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Sheng Z. (2014) Mitochondrial trafficking and anchoring in neurons: new insight and implications. J. Cell Biol. 204, 1087–1098 10.1083/jcb.201312123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Caino M., Seo J., Aguinaldo A., Wait E., Bryant K., Kossenkov A. et al. (2016) A neuronal network of mitochondrial dynamics regulates metastasis. Nat. Commun. 7, 13730 10.1038/ncomms13730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Caino M., Seo J., Wang Y., Rivadeneira D., Gabrilovich D., Kim E. et al. (2017) Syntaphilin controls a mitochondrial rheostat for proliferation-motility decisions in cancer. J. Clin. Invest. 127, 3755–3769 10.1172/JCI93172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Schieber M. and Chandel N. (2014) ROS function in redox signaling and oxidative stress. Curr. Biol. 24, R453–R462 10.1016/j.cub.2014.03.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Rozanov D., Cheltsov A., Sergienko E., Vasile S., Golubkov V., Aleshin A. et al. (2015) TRAIL-based high throughput screening reveals a link between TRAIL-mediated apoptosis and glutathione reductase, a key component of oxidative stress response. PLoS ONE 10, e0129566 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Wen S., Zhu D. and Huang P. (2013) Targeting cancer cell mitochondria as a therapeutic approach. Future Med. Chem. 5, 53–67 10.4155/fmc.12.190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Gilliam L., Fisher-Wellman K., Lin C., Maples J., Cathey B. and Neufer P. (2013) The anticancer agent doxorubicin disrupts mitochondrial energy metabolism and redox balance in skeletal muscle. Free Radic. Biol. Med. 65, 988–996 10.1016/j.freeradbiomed.2013.08.191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Shieh J., Huang T., Hung C., Chou K., Tsai Y. and Wu W. (2010) Activation of c-Jun N-terminal kinase is essential for mitochondrial membrane potential change and apoptosis induced by doxycycline in melanoma cells. Br. J. Pharmacol. 160, 1171–1184 10.1111/j.1476-5381.2010.00746.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Mohammad H., Barbash O. and Creasy C. (2019) Targeting epigenetic modifications in cancer therapy: erasing the roadmap to cancer. Nat. Med. 25, 403–418 10.1038/s41591-019-0376-8 [DOI] [PubMed] [Google Scholar]
- 115.Baechler S., Factor V., Dalla Rosa I., Ravji A., Becker D., Khiati S. et al. (2019) The mitochondrial type IB topoisomerase drives mitochondrial translation and carcinogenesis. Nat. Commun. 10 10.1038/s41467-018-07922-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Tait S. and Green D. (2012) Mitochondria and cell signalling. J. Cell Sci. 125, 807–815 10.1242/jcs.099234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Dhir A., Dhir S., Borowski L.S., Jimenez L., Teitell M., Rötig A. et al. (2018) Mitochondrial double-stranded RNA triggers antiviral signalling in humans. Nature 560, 238–242 10.1038/s41586-018-0363-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Mohanty A., Tiwari-Pandey R. and Pandey N. (2019) Mitochondria: the indispensable players in innate immunity and guardians of the inflammatory response. J. Cell Commun. Signal. 13, 303–318 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Khan M., Syed G.H., Kim S. and Siddiqui A. (2015) Mitochondrial dynamics and viral infections: a close nexus. Biochim. Biophys. Acta 1853, 2822–2833 10.1016/j.bbamcr.2014.12.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Côté H., Brumme Z., Craib K., Alexander C., Wynhoven B., Ting L. et al. (2002) Changes in mitochondrial DNA as a marker of nucleoside toxicity in HIV-infected patients. N. Engl. J. Med. 346, 811–820 10.1056/NEJMoa012035 [DOI] [PubMed] [Google Scholar]
- 121.West A., Khoury-Hanold W., Staron M., Tal M., Pineda C., Lang S. et al. (2015) Mitochondrial DNA stress primes the antiviral innate immune response. Nature 520, 553–557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Walker M., Volpi S., Sims K., Walter J. and Traggiai E. (2019) Powering the immune system: mitochondria in immune function and deficiency. J. Immunol. Res. 14, 164309 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Zhang Q., Raoof M., Chen Y., Sumi Y., Sursal T., Junger W. et al. (2010) Circulating mitochondrial DAMPs cause inflammatory responses to injury. Nature 464, 104–107 10.1038/nature08780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Shimada K., Crother T.R., Karlin J., Dagvadorj J., Chiba N., Chen S. et al. (2012) Oxidized mitochondrial DNA activates the NLRP3 inflammasome during apoptosis. Immunity 36, 401–414 10.1016/j.immuni.2012.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Jo E.K., Kim J.K., Shin D.M. and Sasakawa C. (2016) Molecular mechanisms regulating NLRP3 inflammasome activation. Cell. Mol. Immunol. 132, 148–159 10.1038/cmi.2015.95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Chen Q., Vazquez E.J., Moghaddas S., Hoppel C.L. and Lesnefsky E.J. (2003) Production of reactive oxygen species by mitochondria: central role of complex III. J. Biol. Chem. 278, 36027–36031 10.1074/jbc.M304854200 [DOI] [PubMed] [Google Scholar]
- 127.Won J.H., Park S., Hong S., Son S. and Yu J.W. (2015) Rotenone-induced impairment of mitochondrial electron transport chain confers a selective priming signal for NLRP3 inflammasome activation. J. Biol. Chem. 290, 27425–27437 10.1074/jbc.M115.667063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Widdrington J., Gomez-Duran A., Steyn J., Pyle A., Ruchaud-Sparagano M., Scott J. et al. (2017) Mitochondrial DNA depletion induces innate immune dysfunction rescued by IFN-γ. J. Allergy Clin. Immunol. 140, 1461–1464 10.1016/j.jaci.2017.04.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Canta A., Pozzi E. and Carozzi V. (2015) Mitochondrial dysfunction in chemotherapy-induced peripheral neuropathy. Toxics 3, 198–223 10.3390/toxics3020198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Li Y., Couch L., Higuchi M., Fang J. and Guo L. (2012) Mitochondrial dysfunction induced by sertraline, an antidepressant agent. Toxicol. Sci. 127, 582–591 10.1093/toxsci/kfs100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.De Clercq E. and Neyts J. (2009) Antiviral agents acting as DNA or RNA chain terminators In Handbook of Experimental Pharmacology (Kräusslich H. and Bartenschlager R. eds), pp. 53-84, Springer-Verlag, Berlin: [DOI] [PubMed] [Google Scholar]
- 132.Martin J., Brown C., Matthews-Davis N. and Reardon J. (1994) Effects of antiviral nucleoside analogs on human DNA polymerases and mitochondrial DNA synthesis. Antimicrob. Agents Chemother. 38, 2743–2749 10.1128/AAC.38.12.2743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Lewis W., Day B. and Copeland W. (2003) Mitochondrial toxicity of NRTI antiviral drugs: an integrated cellular perspective. Nat. Rev. Drug Discov. 2, 812–822 10.1038/nrd1201 [DOI] [PubMed] [Google Scholar]
- 134.Laberge R., Adler D., DeMaria M., Mechtouf N., Teachenor R., Cardin G. et al. (2013) Mitochondrial DNA damage induces apoptosis in senescent cells. Cell Death Dis. 4, e727–e727 10.1038/cddis.2013.199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Benbrik E., Chariot P., Bonavaud S., Ammi-Saı¨d M., Frisdal E., Rey C. et al. (1997) Cellular and mitochondrial toxicity of zidovudine (AZT), didanosine (ddI) and zalcitabine (ddC) on cultured human muscle cells. J. Neurol. Sci. 149, 19–25 10.1016/S0022-510X(97)05376-8 [DOI] [PubMed] [Google Scholar]
- 136.Lewis W., Papoian T., Gonzalez B., Louie H., Kelly D.P., Payne R.M. et al. (1991) Mitochondrial ultrastructural and molecular changes induced by zidovudine in rat hearts. Lab. Invest. 65, 228–236 [PubMed] [Google Scholar]
- 137.Pan-Zhou X., Cui L., Zhou X., Sommadossi J. and Darley-Usmar V. (2000) Differential effects of antiretroviral nucleoside analogs on mitochondrial function in HepG2 cells. Antimicrob. Agents Chemother. 44, 496–503 10.1128/AAC.44.3.496-503.2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Chabi B., Adhihetty P., Ljubicic V. and Hood H. (2005) How is mitochondrial biogenesis affected in mitochondrial disease? Med. Sci. Sports Exerc. 37, 2102–2110 10.1249/01.mss.0000177426.68149.83 [DOI] [PubMed] [Google Scholar]
- 139.Arnaudo E., Shanske S., DiMauro S., Schon E., Moraes C., Schon E. et al. (1991) Depletion of muscle mitochondrial DNA in AIDS patients with zidovudine-induced myopathy. Lancet 3377, 508–510 10.1016/0140-6736(91)91294-5 [DOI] [PubMed] [Google Scholar]
- 140.Müller B. and Kräusslic H.G. (2009) Antiviral strategies In Handbook of Experimental Pharmacology (Kräusslich H.G. and Bartenschlager R. eds), pp. 1–24, Springer-Verlag, Berlin, Heidelberg [Google Scholar]
- 141.Brinkman K., Smeitink J., Romijn J. and Reiss P. (1999) Mitochondrial toxicity induced by nucleoside-analogue reverse-transcriptase inhibitors is a key factor in the pathogenesis of antiretroviral-therapy-related lipodystrophy. Lancet 354, 1112–1115 10.1016/S0140-6736(99)06102-4 [DOI] [PubMed] [Google Scholar]
- 142.Lleonart M., Grodzicki R., Graifer D. and Lyakhovich A. (2017) Mitochondrial dysfunction and potential anticancer therapy. Med. Res. Rev. 37, 1275–1298 10.1002/med.21459 [DOI] [PubMed] [Google Scholar]
- 143.Hangas A., Aasumets K., Kekäläinen N., Paloheinä M., Pohjoismäki J., Gerhold J. et al. (2018) Ciprofloxacin impairs mitochondrial DNA replication initiation through inhibition of topoisomerase 2. Nucleic Acids Res. 46, 9625–9636 10.1093/nar/gky793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Lawrence J.W., Claire D.C., Weissig V. and Rowe T.C. (1996) Delayed cytotoxicity and cleavage of mitochondrial DNA in ciprofloxacin-treated mammalian cells. Mol. Pharmacol. 50, 1178–1188 [PubMed] [Google Scholar]
- 145.Kalghatgi S., Spina C., Costello J., Liesa M., Morones-Ramirez J., Slomovic S. et al. (2013) Bactericidal antibiotics induce mitochondrial dysfunction and oxidative damage in mammalian cells. Sci. Transl. Med. 5, 192ra85 10.1126/scitranslmed.3006055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Lawrence J., Darkin-Rattray S., Xie F., Neims A. and Rowe T. (1993) 4-Quinolones cause a selective loss of mitochondrial DNA from mouse L1210 leukemia cells. J. Cell. Biochem. 51, 165–174 10.1002/jcb.240510208 [DOI] [PubMed] [Google Scholar]
- 147.Wang D., Liu Y., Zhang R., Zhang F., Sui W., Chen L. et al. (2016) Apoptotic transition of senescent cells accompanied with mitochondrial hyper-function. Oncotarget 7, 28286–28300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Dasari S. and Tchounwou P.B. (2014) Cisplatin in cancer therapy: molecular mechanisms of action. Eur. J. Pharmacol. 740, 364–378 10.1016/j.ejphar.2014.07.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Ta L., Espeset L., Podratz J. and Windebank A. (2006) Neurotoxicity of oxaliplatin and cisplatin for dorsal root ganglion neurons correlates with platinum-DNA binding. Neurotoxicology 27, 992–1002 10.1016/j.neuro.2006.04.010 [DOI] [PubMed] [Google Scholar]
- 150.Marullo R., Werner E., Degtyareva N., Moore B., Altavilla G., Ramalingam S. et al. (2013) Cisplatin induces a mitochondrial-ROS response that contributes to cytotoxicity depending on mitochondrial redox status and bioenergetic functions. PLoS ONE 8, e81162 10.1371/journal.pone.0081162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Crouch M., Knowels G., Stuppard R., Ericson N., Bielas J., Marcinek D. et al. (2017) Cyclophosphamide leads to persistent deficits in physical performance and in vivo mitochondria function in a mouse model of chemotherapy late effects. PLoS ONE 12, e0181086 10.1371/journal.pone.0181086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Astolfi L., Ghiselli S., Guaran V., Chicca M., Simoni E., Olivetto E. et al. (2013) Correlation of adverse effects of cisplatin administration in patients affected by solid tumours: a retrospective evaluation. Oncol. Rep. 29, 1285–1292 10.3892/or.2013.2279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Meltzer H.Y. (1994) An overview of the mechanism of action of clozapine. J. Clin. Psychiatry 55, 47–52 PMID: [PubMed] [Google Scholar]
- 154.Walss-Bass C., Weintraub S., Hatch J., Mintz J. and Chaudhuri A. (2008) Clozapine causes oxidation of proteins involved in energy metabolism: a possible mechanism for antipsychotic-induced metabolic alterations. Int. J. Neuropsychopharmacol. 11, 1097 10.1017/S1461145708008882 [DOI] [PubMed] [Google Scholar]
- 155.Streck E., Rezin G., Barbosa L., Assis L., Grandi E. and Quevedo J. (2007) Effect of antipsychotics on succinate dehydrogenase and cytochrome oxidase activities in rat brain. Naunyn Schmiedebergs Arch. Pharmacol. 376, 127–133 10.1007/s00210-007-0178-2 [DOI] [PubMed] [Google Scholar]
- 156.Chapman A., Keane P., Meldrum B., Simiand J. and Vernieres J. (1982) Mechanism of anticonvulsant action of valproate. Prog. Neurobiol. 19, 315–359 10.1016/0301-0082(82)90010-7 [DOI] [PubMed] [Google Scholar]
- 157.Ponchaut S., Van Hoof F. and Veitch K. (1992) In vitro effects of valproate and valproate metabolites on mitochondrial oxidations. Biochem. Pharmacol. 43, 2435–2442 10.1016/0006-2952(92)90324-C [DOI] [PubMed] [Google Scholar]
- 158.Sangkuhl K., Klein T. and Altman R. (2009) Selective serotonin reuptake inhibitors pathway. Pharmacogenet. Genomics 19, 907–909 10.1097/FPC.0b013e32833132cb [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Souza M., Polizello A., Uyemura S., Castro-Silva O. and Curti C. (1994) Effect of fluoxetine on rat liver mitochondria. Biochem. Pharmacol. 48, 535–541 10.1016/0006-2952(94)90283-6 [DOI] [PubMed] [Google Scholar]
- 160.Curti C., Mingatto F.E., Polizello A.C., Galastri L.O., Uyemura S.A. and Santos A.C. (1999) Fluoxetine interacts with the lipid bilayer of the inner membrane in isolated rat brain mitochondria, inhibiting electron transport and F1F0-ATPase activity. Mol. Cell Biochem. 199, 103–109 10.1023/A:1006912010550 [DOI] [PubMed] [Google Scholar]
- 161.Klinedinst N.J. and Regenold W.T. (2014) A mitochondrial bioenergetic basis of depression. J. Bioenerg. Biomembr. 47, 155–171 10.1007/s10863-014-9584-6 [DOI] [PubMed] [Google Scholar]
- 162.Eto K., Inoue B., Ogata M., Fukuda T. and Araki Y. (1985) Effect of tricyclic drugs on mitochondrial membrane. Acta Med. Okayama 39, 289–295 [DOI] [PubMed] [Google Scholar]
- 163.Abdel-Razaq W., Kendall D. and Bates T. (2010) The effects of antidepressants on mitochondrial function in a model cell system and isolated mitochondria. Neurochem. Res. 36, 327–338 10.1007/s11064-010-0331-z [DOI] [PubMed] [Google Scholar]
- 164.Katyare S. and Rajan R.R. (1995) Effect of long-term in vivo treatment with imipramine on the oxidative energy metabolism in rat brain mitochondria. Comp. Biochem. Physiol. Part C: Pharmacol. Toxicol. Endocrinol. 112, 353–357 10.1016/0742-8413(95)02031-4 [DOI] [PubMed] [Google Scholar]
- 165.Ji B., La Y., Gao L., Zhu H., Tian N., Zhang M. et al. (2009) A comparative proteomics analysis of Rat mitochondria from the cerebral cortex and hippocampus in response to antipsychotic medications. J. Proteome Res. 8, 3633–3641 10.1021/pr800876z [DOI] [PubMed] [Google Scholar]
- 166.Ferguson J. (2001) SSRI antidepressant medications. Prim. Care Companion J. Clin. Psychiatry 3, 22–27 10.4088/PCC.v03n0105 [DOI] [PMC free article] [PubMed] [Google Scholar]