Abstract
Objective:
This exploratory study is the first to examine FBT adherence and association to treatment outcome in the context of a large-scale, multi-centre study for the treatment of adolescents with Anorexia Nervosa.
Method:
190 recorded FBT sessions from 68 adolescents with AN and their families were recruited across multiple sites (N=6). Each site provided 1-4 tapes per family over four treatment time points and each were independently rated for therapist adherence.
Results:
There were differences in adherence scores within and between sites. ANOVA produced a main effect for site (F(5,46)=8.6, p<0.001), and phase (F(3,42)=12.7, p<0.001), with adherence decreasing in later phases. Adherence was not associated to end of treatment percent ideal body weight after controlling for baseline percent ideal body weight (r=0.088, p=0.48).
Conclusions:
Results suggest that FBT can be delivered with adherence in phase one of treatment. Adherence was not associated with treatment outcome as determined using percent ideal body weight.
Keywords: Fidelity, Family Based Treatment, Adolescents, Anorexia Nervosa
Family Based Treatment (FBT) has the largest evidence base supporting it as an effective treatment of Anorexia Nervosa (AN) in adolescents (Agras et al., 2014; Lock, Agras, Bryson & Kraemer, 2005; Lock et al., 2010; Madden et al., 2015). FBT targets disordered eating by empowering parents to re-nourish their child (Lock & Le Grange, 2015) and is most efficacious in facilitating weight restoration in adolescents with a shorter duration of illness (Agras et al., 2014; Gusella, Campbell & Lalji, 2017; Lock et al., 2005; Lock et al., 2010; Madden et al., 2015). Thus, FBT is helpful for treating adolescents with AN, but therapist adherence to the treatment manual designed to train and guide this therapy has received minimal attention in studies. Adherence to a manualized therapy is one aspect of treatment fidelity; treatment fidelity has been conceptualized as a method for evaluating the degree to which clinicians closely follow a model as intended by the developers and includes both competence and adherence. Competence encompasses how well therapists apply their skill in the provision of the treatment (Hogue et al., 2008), whereas adherence captures the degree to which a skill or technique matches what is recommended in the model. Being able to demonstrate fidelity (in terms of both competence and adherence) would increase confidence in the results of RCTs of psychological treatments (Borrelli, 2011; Southam-Gerow & McLeod, 2013) and thereby also enhance reliability and validity of such treatments (Carroll et al., 2007; Borelli et al., 2005). To ensure competence, study investigators carefully select and educate therapists then monitor competence throughout a supervision process. Treatment adherence can be more easily quantified by comparing and contrasting a therapists’ use of interventions to a manual.
Treatment fidelity measuring adherence to adolescent family therapy across a range of mental health issues such as psychosis and addictions has been investigated (Baer et al., 2007; Marvin, Miklowitz, O’brien, & Cannon, 2016; Hogue et al., 2014; Marvin, Miklowitz, O’Brien & Cannon, 2016; Perepletchikova, Treat & Kazdin, 2007; Robbins et al., 2011; Weisz et al., 2009). The influence of treatment adherence on outcomes in psychotherapy research has resulted in mixed findings with some research demonstrating that higher adherence was associated with improved treatment outcomes (Campost-Melady et al., 2017; Holder, Holliday, Williams, Mullen & Suris, 2018) while other studies have found no association (Baldwin & Imel, 2013; Farmer, Mitchell, Parker-Guilbert & Galovski, 2017; Tschuschke et al., 2015; Webb, Derubeis & Barber, 2010).
In contrast to the research on treatments for adolescents with other mental health issues (Teague, Mueser & Rapp, 2014) and their families, the examination of treatment fidelity and adherence in eating disorders has received relatively little attention from researchers (Andony et al., 2015; Frosberg et al., 2015; Loeb et al., 2005; Couturier, Isserlin & Lock, 2010; Peterson, Becker, Treasure, Shafran & Bryant-Waugh, 2016; Wilfley et al., 2002). The small number of available studies only focused on adherence rather than competence of the therapist delivering FBT. A study of therapist adherence to manualized FBT was conducted by Couturier et al. (2010). The study was an open trial of 14 adolescent outpatients with AN and it measured adherence using a standardized scale to assess session recordings. The study found that adherence to manualized FBT decreased over time and that therapists had higher rates of adherence to behaviorally oriented interventions focused on eating and meals. Lower rates of adherence were related to the role of siblings in FBT, the modifications of parental and sibling criticism and general family process issues. Deviations from FBT may be common as approximately one third of clinicians who responded to an online survey reported significant deviations from the protocol when conducting FBT for adolescent with eating disorders (Kosmerly, Waller & Lafrance Robinson, 2015). A better understanding of the role of treatment adherence is important to shape training and enhance the quality of manuals for clinical interventions. In the case of FBT, increased understanding of adherence to the manual can facilitate focused training, identify key points for supervision, and potentially increase fidelity in adherence and competence as well as efficiency in dissemination by honing in on salient ingredients of treatment. Components of FBT that have a positive association with treatment outcomes include: empowering parents to re-nourish their child back to health, externalization and alignment of the family against the eating disorder, and increased warmth and low parental criticism (Ellison et al., 2012) and early weight gain. To date, there is no empirical research to support the influence of therapist adherence on outcomes in adolescents (weight restoration and eating rehabilitation) participating in FBT.
Thus, the current exploratory study examines therapist fidelity, with a specific focus on adherence to FBT in the context of a large-scale, multi-site study in adolescents with AN. While this is a secondary analysis for which the original study was not powered, it is nonetheless, the first to examine the associations between therapist adherence to FBT and outcomes. Our exploratory hypotheses were that adherence would be highest early in the course of FBT and then decline over time, consistent with previous findings (Couturier et al., 2010). Given the mixed findings regarding the relationship between therapist adherence and adolescent outcomes, in our second exploratory hypothesis we predicted that adherence would not be associated with treatment outcome as measured by Percent Ideal Body Weight (IBW). Building on earlier findings by Couturier et al., our third exploratory hypothesis is that therapists will have higher adherence to behavioural interventions focused on eating, food and meals and lower adherence ratings on interventions related to process issues.
Methods
Family therapy sessions rated for fidelity with a specific focus only on adherence were derived from a randomized sample consisting of 68 adolescent participants from the following six sites: Weill Medical College Cornell University; University of California at San Diego (UCSD), School of Medicine; Stanford University School of Medicine; Sheppard-Pratt Health System; University of Toronto School of Medicine (UofT); and, Washington University School of Medicine, St. Louis (WASH U). Each clinical site approved study procedures through their internal research ethics review boards. Full details of the study design can be found in Agras et al., 2014. Briefly, all 68 participants provided informed consent. Inclusion criteria were as follows: 1) age 12–18 years, 2) DSM IVTR criteria met for AN, 3) below 87% Expected Body Weight at entry, 4) residing with family, and 5) medically stable for outpatient treatment. Exclusion criteria were as follows: associated physical illnesses or mental illnesses that required hospitalization; current misuse of drugs or alcohol; physical conditions (e.g. diabetes mellitus, pregnancy) known to influence eating or weight; and, previous participation in FBT for AN. Each therapy session was recorded. For this study the primary outcome variable (% IBW) was assessed at baseline and end-of-treatment.
FBT, which focuses on helping families make behavioral changes in adolescents with AN to promote weight restoration and taking up adolescent roles, was delivered using a manualized approach (Lock & Le Grange, 2013). FBT consists of three sequential phases. Treatment begins with parents obtaining symptom control to assist their child to achieve weight restoration. In the second phase, parents incrementally return control of eating back to the adolescent in order for them to practice eating meals with greater independence. In the final phase of FBT, the family explores adolescent developmental issues and ways to sustain recovery. All study therapists had PhD, MD, or postgraduate level qualifications in family therapy, psychology, psychiatry or social work. Given the large number of therapists (N=26) involved in the study, it was assumed that non-specific therapist variables would be equally distributed, thereby minimizing the influence of these confounding factors on outcomes (see Brown et al., 2013). Training began with a two-day intensive training event, delivered by clinicians highly experienced in FBT. Each study therapist completed two pilot cases that were reviewed by the overall supervisor for that treatment as well as by a site supervisor. Therapists received weekly face to face supervision from their local site supervisor. Site supervisors were chosen by the site PI based on their perceived ability to provide supervision in FBT. In addition to supervision provided at each site, a monthly supervisory session of paired sites (site pairs were rotated quarterly) was conducted using teleconferencing to limit site drift. These monthly site supervision sessions were led by the overall supervisors and investigators for the study.
Fidelity Measure
The fidelity measure was developed by Drs. Lock and Le Grange for use in studies of FBT (Forsberg et al., 2015; 2018; LeGrange & Lock, 2015). The measure only assesses the therapist’s adherence to key interventions of FBT across all three phases of the treatment. The FBT fidelity measure contains 25 items rated using a 7-point Likert Scale, distributed across three sections that correspond with the phases of the model as described in the FBT manual1 (see Table 2 for examples of specific items). The FBT instrument had not been psychometrically evaluated at the time of this study but has since been modified and found to demonstrate strong consistency and reliability for sessions 1 and 2 of FBT (Forsberg et al., 2015) and was re-named the FBT-FACT (Family Therapy Fidelity and Adherence Check).
Table 2:
Treatment Fidelity Scores (Scale of 1 to 7) for Each Item of Family-Based Treatment by phase
| Phase 1 (Session 1) | N of 22 | Mean | SD |
|---|---|---|---|
| Greet Family in sincere but grave manner | 22 | 4.1 | .75 |
| Take a history that engages family | 22 | 4.8 | .74 |
| Separate the patient from the illness | 22 | 4.5 | 1.1 |
| Orchestrate an intense scene around seriousness | 22 | 4.6 | .95 |
| Charge the parents with task of re-feeding | 22 | 4.4 | 1.3 |
| Session 2 (Meal) | 10 | ||
| Take history and observe family patterns around food | 10 | 4.7 | .82 |
| Help parents convince patient to eat one more bite | 10 | 5.3 | .95 |
| Align patient with siblings | 8 | 4.0 | 1.1 |
| Rest of Phase 1 | 70 | ||
| Focus Therapeutic discussion on food and eating | 69 | 4.9 | 1.1 |
| Help parental dyad’s efforts at re-feeding | 70 | 4.8 | 1.0 |
| Discuss and evaluate siblings efforts | 41 | 3.3 | 1.5 |
| Continue to modify parental and sibling criticism | 54 | 3.9 | 1.2 |
| Continue to distinguish patient’s interests from those of AN | 70 | 3.9 | 1.4 |
| Phase 2 | 68 | ||
| Continue to support parents in management of eating disorder symptoms | 68 | 4.8 | 1.1 |
| Assist parents in negotiating return of control to adolescent | 66 | 4.0 | 1.2 |
| Encourage family to examine relationships between adolescent issues and the development of Anorexia | 67 | 3.6 | 1.2 |
| Continue to modify parental and sibling criticisms | 45 | 3.6 | 1.3 |
| Continue to assist siblings in supporting their ill sibling | 28 | 3.2 | 1.3 |
| Continue to highlight difference between adolescent’s own ideas and those of Anorexia | 68 | 3.7 | 1.4 |
| Phase 3 | 20 | ||
| Review adolescent issues with family to model problem solving | 20 | 4.2 | 1.4 |
| Involve the family to review of issues | 20 | 4.6 | 1.2 |
| Check with parents how much they are doing as a couple | 15 | 1.9 | 1.2 |
| Explore adolescent themes | 20 | 3.6 | 1.6 |
| Plan for future issues | 20 | 3.9 | 1.4 |
| Manage termination | 19 | 3.5 | 1.8 |
Fidelity Assessment Procedures to determine adherence
Each rater (n=6) had a graduate degree in social work, psychology or a related field and extensive clinical experience with eating disorders. Raters were not “experts” in FBT but were trained by reading the manual and viewing tapes of the training workshop for clinicians and trained in the application of the fidelity instrument to assess adherence. Raters were trained to observe a session in its entirety before ranking the extent to which a study therapist adhered to each item on the fidelity instrument. A randomly selected sample of 20% of ratings from each assessor was audited by the lead assessor (GD) to check for drift. This was done by the lead assessor rating all of the items on the fidelity instrument again herself. When a rater scored consistently higher (range of 6 or higher) or lower (2 or lower) in all the domains, the rater and lead assessor met to discuss the discrepancies and worked together until consensus was reached. Each site provided 4 tapes per family. Within families, 4 sessions were randomly selected in advance from each of the following blocks: Block #1: sessions 1–4; Block #2 sessions 5–8, Block #3: 9–12, and Block #4 Session 13–16. However due to inaudibility of some tapes and missed tapes due to attrition, not all subjects contributed 1 tape per block. Overall fidelity was calculated by averaging the scores of the four blocks. FBT Inter rater reliability was calculated using an intraclass correlation based on 21 tapes (2 raters). These tapes were randomly selected based on the completed tapes per rater. The resulting ICC=0.73 which is considered good according to commonly-cited cutoffs (Cicchetti, 1994).
Data Analysis
Descriptive statistics were used to describe the sample of therapists analyzed in the study. Because not every subject had an adherence measurement from each of the 4 blocks, a mixed models approach was used to analyze the adherence data. Mixed models can adjust for missing data by imputing from the non-missing data for a subject as well as from the non-missing data from other similar subjects; thus, it is an ideal approach to use in this analysis. Mixed effects modelling assumes data is missing at random and employs Maximum Likelihood method for handling missing data (Jo, 2008; Little & Rubin, 2002). Blocks and Site and the interaction were entered as fixed effects. Post hoc Bonferroni tests were used to determine specific differences between blocks. The relationship of fidelity (specifically therapists’ adherence to the model) to outcome was assessed using Spearman correlations, controlling for baseline measurement.
Results
Therapist characteristics
A total of 26 therapists participated in the multi-site study, with data missing from one therapist. The degrees of the study therapists were as follows: three with a Master of Social Work; thirteen with a PhD in clinical psychology; eight with a master’s degree in counseling; and, two MD psychiatrists. With respect to ethnicity, 22 therapists identified as Caucasian, two as Asian and two as Hispanic. The types of activities engaged in during supervision included: 69% of therapists endorsed time spent listening to audio and video tapes; 85% spent time discussing treatment planning; 42% discussed administrative issues; 23.1% engaged in behavioral rehearsal and role playing; and 15% reviewed journal articles. Across all sites, 65% of therapists reported weekly supervision on average, and 30.8% reported having on average of bi-weekly sessions. On a scale of 1–10, therapists ranked themselves as having a lot of confidence (mean = 8±1.5) that they were adhering to manualized FBT. To protect the confidentiality of the clinicians, we only gathered descriptive information on all the therapists without linking the data to the results of the fidelity measure and therapy type in the larger study.
Table 1 presents a description of the therapists across the six sites. Sites differed on the average number of years the staff had worked in their position (F (5,19) = 5.02, p = 0.004). Therapists at site 1 had worked in their position significantly longer than therapists at Site 2, Site 5 and Site 6. Sites differed on the age of the therapists. The therapists at site 1 were older than the therapists at Site 2, 5 and 6.
Table 1:
Descriptive data on therapists across all six sites (Means and Frequencies)
| Site | N | Mean Age* (SD) |
Minority Status (%) |
Years working with eating disorders (SD) |
Years working with Anorexia Nervosa (SD) |
Years using family therapy (SD) |
Years in Position (SD)** |
Weekly Supervision |
|---|---|---|---|---|---|---|---|---|
| Site 1 | 5 | 43.6 (9.7) |
0% | 14.2 (4.7) |
8.4 (6.7) |
12.4 (4.8) |
13.2 (4.8) |
40% |
| Site 2 | 5 | 35.8 (7.5) |
20% | 7.8 (1.8) |
3.4 (3.1) |
3.6 (5.0) |
4.4 (3.4) |
100% |
| Site 3 | 2 | 38.5 (10.6) |
0% | 10.5 (7.8) |
11.7 (4.2 |
7.5 (3.5) |
10.5 (9.2) |
100% |
| Site 4 | 3 | 39.3 (4.2) |
33% | 11.7 (4.2) |
11.7 (4.2) |
12.0 (4.4) |
10.0 (4.4) |
67% |
| Site 5 | 7 | 36.1 (8.2) |
29% | 7.2 (6.7) |
4..2 (7.8) |
5.3 (8.1) |
3.5 (1.5) |
29% |
| Site 6 | 4 | 34.7 (4.6) |
0% | 7.17 (6.7) |
3.0 (3.4) |
5.2 (5.9) |
3.5 (3.3) |
100% |
Site differences <.05
Site differences <.01
One hundred and ninety tapes (Block 1– 56, Block 2– 45, Block 3–48, Block 4–41) from 68 participants were assessed for fidelity. Figure 1 presents the estimated means by site and block. There were significant site (F(5,46)=8.6, p<0.001) and block (F(3,42=12.7, p<0.001) differences indicating that fidelity varied across the sites and that fidelity decreased in the later blocks. Post hoc analysis indicated that Block 1 differs from both Block 3 (p=0.002) and Block 4 (p<0.001), and Block 2 is also different from Block 4(p=0.032). Block by site interaction was not significant indicating that in general the decrease in fidelity over time was repeated at each site. This pattern of differences between sites and decrease in fidelity over time is shown in Figure 1.
Figure 1:
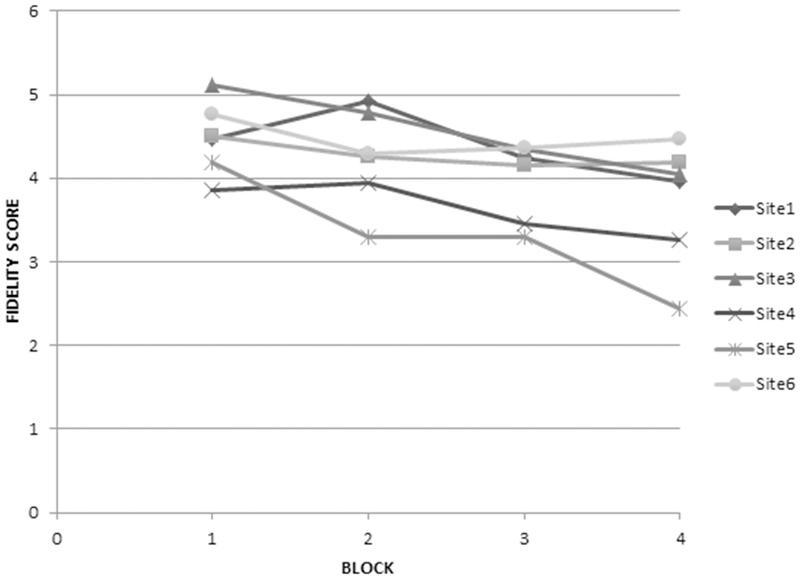
Estimated mean fidelity scores by phase and site
Spearman correlations showed that overall fidelity was not related to end of treatment percent IBW after controlling for baseline percent ideal body weight (r=0.088, p=0.48) for all 68 participants included in the full analysis. Likewise, change in IBW from baseline to end of treatment was not related to fidelity in blocks 1 and 2 (r= −.0839, p=0.35) or blocks 3 and 4 (r=.0983, p=0.32) for all 137 participants originally randomized to the study.
Descriptive statistics (means and standard deviation) for each item of the FBT fidelity instrument can be found in Table 2. A total mean score of >4.0 or higher (adequate fidelity) was achieved for many items throughout the 3 phases, however the proportion of items with adequate fidelity decreased markedly between Phase 1 and later phases, with 77% of items in Phase 1 having scores >4.0 as opposed to only 33% of items in Phases 2 and 3. The item with the highest rating of fidelity in phase 1 was assisting parents to convince their child to eat one more bite during the “family meal”. In phase two, the highest rated item was: continuing to support parents in the management of eating disorder symptoms. Finally, the highest rated item in Phase 3 was involving family in reviewing adolescent issues.
Discussion
Overall, our results of this exploratory study suggest that FBT can be delivered with adherence particularly in the first phase of treatment in a large multi-site study. Employing a measure of fidelity designed to assess therapist adherence, the findings from the study support the three exploratory hypotheses. As predicted, adherence incrementally decreased over time in the treatment. We found adherence to FBT was consistently higher in block 1 and 2 (considered phase 1) and then diminished in block 3–4 (phase 2 and 3) across all six sites. This finding is consistent with earlier research conducted by Couturier et al. 2010. A decline in therapist adherence to the treatment model is a common problem in eating disorder treatment studies (Waller, 2016; Kosomerly, Waller & Lafrance Robinson, 2015; Wisniewski, Hernandez & Waller, 2018). Specific to FBT, therapists may find it challenging to adhere to a narrow range of interventions that require an exclusive and persistent focus on food and re-feeding overtime regardless of the material presented by the patient and family. However, previous research has shown that early weight gain by session 4 of FBT is a strong predictor of successful outcome by end of treatment (Le Grange et al., 2014). Given the lack of studies on adherence in the early phase of treatment and rapid weight gain by session 4, research is needed to investigate this potential association. A persistent focus on food and meals declined in the final phase of FBT perhaps because the treatment modality encourages greater exploration of general adolescent issues and the relationship between the parents. It is possible that therapists had greater difficulties achieving adherence in phase 3 due to the broader therapeutic aims and goals of treatment. For instance, in the earlier stages of the model, there is greater emphasis on interventions designed to assist therapists to support families with weight and eating rehabilitation than in the later phase of the treatment. It is possible that more discrete aims may be added to the third phase of FBT in future iterations of the manual, thereby making the aims of this stage more concrete and accessible to adherence research. However, the goals of phase 3 are broad and diffuse allowing clinicians to address the unique issues that arise for adolescents and their family members. The presentation of wide-ranging issues in phase 3 makes it difficult to capture concretely what occurs in the final few sessions of this treatment.
The second hypothesis was that adherence would not be related to outcome. Our findings revealed that treatment adherence to FBT did not influence changes in percent ideal body weight in adolescents. We are unable to directly compare our results to other studies since to the best of our knowledge, this is the first study to examine therapist fidelity to the FBT model in adolescents with AN and its relationship to treatment outcomes such as weight. Research on the relationship between therapist treatment adherence and adolescent outcomes in other mental health disorders has produced mixed findings; previous researchers have attributed these equivocal findings to measurement issues (lack of reliable or valid fidelity instruments) (Teague et al., 2014) and the challenges of separating treatment adherence from other variables such as therapeutic alliance, therapist level of training/experience, or therapist’s own bias (Campbell et al., 2013). In previous studies, it has been shown that a strong therapeutic alliance can be formed in FBT (Forsberg et al., 2013), but no studies yet have examined both alliance and adherence to FBT. This is an important area for future exploration as previous research shows therapeutic alliance affects FBT outcomes, especially in the first phase, and only if weight gain persists throughout treatment (Pereira, Lock & Oggins, 2006; Isserlin &Couturier, 2012; Forsberg et al., 2015; Graves et al., 2017; Walker et al., 2017). Importantly, the measure utilized in our study only assessed treatment adherence to the model rather than the proficiency and competence of therapists using FBT. It is possible that the therapist’s competence delivering the treatment may be a better predictor of adolescent outcomes more so than adherence to the model. A new fidelity instrument for FBT has recently been reported which simultaneously measures competence and adherence to treatment for the first phase of this treatment modality. The Family Therapy Fidelity and Adherence Check (FBT-FACT) has sound psychometric properties and will be useful in future multi-site studies (Forsberg et al., 2015). Future studies of treatment fidelity in FBT will likely benefit from using this instrument which was not available at the time our study was conducted.
Our final hypothesis was that clinicians would achieve high adherence (>4.0 or higher) on items describing behaviorally oriented interventions and lower scores on items related to processes such as engaging siblings to support their affected sibling in non-food areas and exploring themes related to general adolescent developmental issues. As hypothesized, study therapists achieved adequate to high adherence on items related to model specific behavioural interventions (supporting parents to re-nourish their child such as eating one more bite and supporting parents to manage meals until adolescent can eat). Study therapists appeared to have low adherence on interventions related to family process issues including aligning siblings with the adolescent with AN in areas outside of the illness and assisting parents to build a relationship post-intensive treatment. This finding is in line with research conducted by Couturier et al. (2010) on a smaller sample size of participants (n=14) in a single site. The results of our study are also consistent with other research using standardized instruments that shows therapist adherence to core interventions in cognitive behavioural therapy to be acceptable for anxiety disorders (Edmunds et al., 2014) and post-traumatic disorder (Farmer et al., 2017; Lu et al., 2012). The results of our multi-site study suggest that therapists can successfully achieve adherence to the application of model-specific techniques such as prescribed behavioral interventions. In contrast to behavioural interventions, study therapists scored lower on items that were more process oriented (sibling involvement in assisting affected individual).
Due to increasing evidence that parental self-efficacy contributes to better treatment outcomes (Bryne, Accurso, Arnow, Lock & Le Grange, 2015), the overt focus on parental empowerment in re-nourishing the affected individual may lead to the marginalization of siblings in FBT. Although the involvement of all family members in FBT is explicitly emphasized, it is possible that the role of the sibling in FBT was not emphasized sufficiently in supervision in this study. Future research is required to determine which interventions delineated in the FBT measurement are salient predictors of adolescent and family outcomes. Further, it will be important for future studies to qualitatively assess why therapists have low adherence to certain aspects of manualized FBT but not others. Extrapolating from literature on therapist drift from manualized treatment, hypothesized reasons for therapist non-adherence may be personal beliefs about the utility of including siblings and process-oriented interventions, low therapist confidence in how to effectively integrate siblings, or lack of supervisory focus on the importance of these aspects (Waller & Turner, 2016).
There were site differences in adherence to FBT with some sites having significantly lower ratings compared to other sites, and some sites clearly performing better. In multisite studies, sites are expected to differ, and such differences provide an important test of the generalizability of the approaches being examined. The presence of site differences suggests that the training and supervisory processes utilized, while effective overall, were less effective in some sites than other sites. Although it not known what contributed to the differences among the sites, this finding suggests that researches may consider therapists, supervisors and organizational factors that may influence adherence to treatment modalities be investigated.
Although it was intended that all therapists would receive both weekly site level supervision and participate in the monthly paired site supervisions, therapists reported variability in the frequency of supervision with some receiving bi-weekly rather than weekly supervision. The factors that contributed to this deviation from the supervision protocol are not known. Because there were no standardized qualifications for the site supervisors, variation in skills and abilities in FBT may have contributed to variations in supervision and ultimately to therapist competence. Using site pairs to help prevent site drifts in supervision was designed to partially address this variability, but this measure appears to have not been successful at the site level. In a systematic review of multi-site studies in addictions, Baer et al., (2007) demonstrated an absence of methods for assessing the content and frequency of supervision and in a community mental health setting, supervision was highly variable across clinicians with little institutionally approved time allotment (Dorsey et al., 2017). Similarly, in another study that systematically examined the content of clinical supervision it was found that only half the time was spent discussing issues related to adherence to evidence-based practice models (Nedeem et al., 2013). A recent article by Waller et al., (2017) puts forward that supervision for therapists integrating evidence-based treatments for eating disorders may present its own challenges; there may be few supervisors for the number of clinicians and supervisors may have their own bias between clinicians. Further, questions of how accurate supervisors are in assessing skill in clinicians, and inflated confidence in self-reported skill from clinicians during supervision can complicate the utility of supervision for increased adherence.
Future Research Implications
Future research is needed to identify what factors may enhance adherence to family based treatment for Anorexia nervosa. To achieve this aim, we suggest that researchers consider employing different research designs. For instance, we recommend a dismantling design to ascertain which components of FBT (the fundamental principles or specific interventions such as weighing the patient prior to the session or the family meal) contribute to improved adolescent and family outcomes (Guidi et al., 2018). This type of design would potentially increase knowledge regarding whether therapist adherence to the principles of FBT or specific behavioural interventions are the ingredients that are integral to the treatment. Another potential design is to use observational studies or qualitative methods to obtain data about adherence to treatment from the therapists, parents and adolescents and to identify what circumstances contribute to drift to manualized FBT within and across sessions. Finally, researchers should consider documenting organizational factors, content and processes within the supervision session that may contribute to drift from the study and/or treatment protocols. Such information would help with the development of strategies to improve adherence to supervision protocols in multi-site studies and in efforts to scale up the implementation of FBT in routine clinical practice.
While the above suggestions would strengthen future research on FBT, we highly recommend researchers to investigate therapist adherence broadly when exploring the efficacy of psychotherapeutic interventions for eating disorders. Recent discussions within the community of ED specialists have aimed to understand key similarities and differences in ED treatment approaches (Geller & Srikameswaran, 2015). Evidence that supports adherence to the application of therapy and the most relevant pieces of each intervention are important tools for continuing to improve the efficacy of treatment.
This study had several strengths. First, it assessed treatment adherence in FBT for AN across multiple sites. The fidelity measurement was designed to assess adherence and provides specificity by explicitly delineating the components of each intervention, specifying which interventions should be delivered in each session and each phase (Schoenwald, Mehta, Frazier & Shernoff, 2013). Extensive training and periodic checks of recordings and completed ratings were conducted throughout the study for quality assurance purposes. Trained raters used fidelity measures while being blind to treatment outcomes. As recommended by Pereplectchikova and Kazdin (2007), a random selection of tapes was re-rated. This was followed by a meeting to achieve consensus between the lead assessor and the rater. Second, standardized training for the therapists was conducted at two different time points. Expert trainers used indirect methods (systematic review of the manual and literature on adolescence, eating disorders and families) and direct methods (role playing and presentation of various clinical cases) to train the therapists. In addition to these training opportunities, clinical supervision was offered to all the therapists across the six sites.
As with any study, there are also several limitations. Given the exploratory nature of our research, we looked at four distinct phases of FBT rather than 2 or 3 which would have increased our power to detect differences. We did this to identify if fidelity differed in the first couple of sessions of FBT in contrast to the earlier and later phases of treatment. At the time of data collection, the validated FBT-FACT fidelity instrument was not yet available. The adherence instrument utilized in this study was not validated; however, the use of an instrument that has yet to be validated for assessing adherence is not unique to this study. Schoenwald and Garland (2013) reported that only 35% of studies on psychological interventions for children and adults employed a validated treatment adherence measurement. The instrument used focused on the degree to which therapists adhered to interventions across all phases and specific sessions but did not measure therapist competency. We were not always able to code a tape due to inaudibility and attrition which resulted in significant reduction in the number of tapes available for analysis of the family meal, session 1 and phase 3. Also, the study used IBW as the only method of understanding recovery and future studies would benefit from also including a measure of psychological recovery or improvements in eating psychopathology. Finally, therapists in the current study elected to participate vs. studying a sample of therapists across one or many treatment sites. To this end, there may be differences in therapists who elect to participate in research studies and results may not be broadly generalized. It may be that therapists in the current study endorse using manuals and fidelity to evidence-based practice guidelines which may make them different from other therapists who do not engage in research (Thompson et al., 2012). However, this study included sites with novice and seasoned therapists with varying experience, and such variability is representative of what would be expected in community settings.
Conclusions
The findings of this study suggest that manualized FBT can be used in multi-site studies while achieving reasonable fidelity particularly in the earlier phases. Findings also showed that adherence is strongest in the first phase of treatment and that adherence varies between different aspects of FBT; notably there is reduced adherence to process related issues compared with behaviorally oriented techniques.
Given that this is the first article investigating therapist adherence to FBT, the authors support continued research in this critical area Research is needed to identify what aspect of the FBT manual are integral to its efficacy in improving treatment outcomes for adolescents with eating disorders while discarding components that are not needed. Improved adherence to the manual may ultimately lead to more reliable results both in research and in clinical practice which may benefit clinicians, patients and families alike. Enhanced knowledge about treatment adherence will be vital to improve training, inform dissemination and implementation efforts, and potentially suggest key mechanisms of action of therapy.
Highlights:
* FBT was delivered with adherence in the first phase of treatment across multiple sites
* Adherence to the behavioral aspects of FBT were greater than the process aspects of FBT
* Adherence to FBT was greater in early treatment and more drift from the model was detected in the later stages of treatment.
Acknowledgements:
We would like to thank the raters for assisting with this study including Elyssa Greenbaum, Kristina Klopfer, Ruth Masliyah, Lindsay Ross, Reva Schachter, and, Nicole Stonewall. We would also like to acknowledge all six site supervisors and therapists for their willingness to participate in the fidelity study. We would like to thank our research assistants (Eileen Lam and Victoria Freeman) for their assistance as well. Finally, we would like to acknowledge the significant contributions of the late Dr. Susan Bryson for her invaluable authorship and contributions to this research.
Funding:
This study was supported by the following grants from the National Institute of Mental Health: MH 076290 (Agras/Lock); MH 076254 (Brandt); MH 076251 (Halmi); MH 076250 (Johnson); MH 076286 (Kaye); MH 076255 (Wilfley); MH 076253 (Woodside).
Footnotes
Conflict of Interest Statement:
James Lock is a founding author of the Family-Based Treatment model. No other authors have a conflict of interest to declare.
Trial Registration:
clinicaltrials.gov. Identifier
References
- Andony LJ, Tay E, Allen KL, Wade TD, Hay P, Touyz S, … & Erceg‐Hurn DM (2015). Therapist adherence in the strong without anorexia nervosa (SWAN) study: A randomized controlled trial of three treatments for adults with anorexia nervosa. International Journal of Eating Disorders, 48(8), 1170–1175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agras WS, Lock J, Brandt H, Bryson SW, Dodge E, Halmi KA, … & Woodside B (2014). Comparison of 2 family therapies for adolescent anorexia nervosa: a randomized parallel trial. JAMA psychiatry, 71(11), 1279–1286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baer JS, Ball SA, Campbell BK, Miele GM, Schoener EP, & Tracy K (2007). Training and fidelity monitoring of behavioral interventions in multi-site addictions research. Drug and alcohol dependence, 87(2–3), 107–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baldwin SA, & Imel ZE (2013). Therapist effects: Findings and methods. Bergin and Garfield’s handbook of psychotherapy and behavior change, 6, 258–297. [Google Scholar]
- Borrelli B (2011). The assessment, monitoring, and enhancement of treatment fidelity in public health clinical trials. Journal of public health dentistry, 71, S52–S63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown LA, Craske MG, Glenn DE, Stein MB, Sullivan G, Sherbourne C, … & Roy‐Byrne P (2013). CBT competence in novice therapists improves anxiety outcomes. Depression and anxiety, 30(2), 97–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrne CE, Accurso EC, Arnow KD, Lock J, & Le Grange D (2015). An exploratory examination of patient and parental self‐efficacy as predictors of weight gain in adolescents with anorexia nervosa. International Journal of Eating Disorders, 48(7), 883–888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campos-Melady M, Smith JE, Meyers RJ, Godley SH, & Godley MD (2017). The effect of therapists’ adherence and competence in delivering the adolescent community reinforcement approach on client outcomes. Psychology of Addictive Behaviors, 31(1), 117. [DOI] [PubMed] [Google Scholar]
- Carroll C, Patterson M, Wood S, Booth A, Rick J, & Balain S (2007). A conceptual framework for implementation fidelity. Implementation science, 2(1), 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti DV (1994). Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychological assessment, 6(4), 284. [Google Scholar]
- Couturier J, Isserlin L, & Lock J (2010). Family-based treatment for adolescents with anorexia nervosa: A dissemination study. Eating Disorders, 18(3), 199–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Couturier J, Kimber M, & Szatmari P (2013). Efficacy of family‐based treatment for adolescents with eating disorders: A systematic review and meta‐analysis. International Journal of Eating Disorders, 46(1), 3–11. [DOI] [PubMed] [Google Scholar]
- Dorsey S, Pullmann MD, Kerns SE, Jungbluth N, Meza R, Thompson K, & Berliner L (2017). The juggling act of supervision in community mental health: Implications for supporting evidence-based treatment. Administration and Policy in Mental Health and Mental Health Services Research, 44(6), 838–852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edmunds JM, Read KL, Ringle VA, Brodman DM, Kendall PC, & Beidas RS (2014). Sustaining clinician penetration, attitudes and knowledge in cognitive-behavioral therapy for youth anxiety. Implementation Science, 9(1), 89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farmer CC, Mitchell KS, Parker-Guilbert K, & Galovski TE (2017). Fidelity to the cognitive processing therapy protocol: evaluation of critical elements. Behavior therapy, 48(2), 195–206. [DOI] [PubMed] [Google Scholar]
- Fitzpatrick KK, Accurso EC, Aspen V, Forsberg SE, LeGrange D, Lock J (2015) Conceptualizing fidelity in FBT as the field move forward: How we know when we’re doing it right? In Loeb K, Le Grange D, Lock J (editors) Family Therapy for Adolescent Eating and Weight Disorders: New Applications, New York, Routledge, 2015 418–439. [Google Scholar]
- Forsberg S, Fitzpatrick KK, Darcy A, Aspen V, Accurso EC, Bryson SW, … & Lock J (2015). Development and evaluation of a treatment fidelity instrument for family‐based treatment of adolescent anorexia nervosa. International Journal of Eating Disorders, 48(1), 91–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forsberg S, LoTempio E, Bryson S, Fitzpatrick KK, Le Grange D, & Lock J (2013). Therapeutic alliance in two treatments for adolescent anorexia nervosa. International Journal of Eating Disorders, 46(1), 34–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forsberg S, Lock J, Le Grange D Appendix V: Fidelity coding framework, New York: Routledge, 2018, pp 152–170. [Google Scholar]
- Geller J, & Srikameswaran S (2015). What effective therapies have in common, Advances in Eating Disorders, 3(2), 191–197. [Google Scholar]
- Gusella JL, Campbell AG, & Lalji K (2017). A shift to placing parents in charge: Does it improve weight gain in youth with anorexia?. Paediatrics & child health, 22(5), 269–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graves TA, Tabri N, Thompson‐Brenner H, Franko DL, Eddy KT, Bourion‐Bedes S, … & Isserlin L (2017). A meta‐analysis of the relation between therapeutic alliance and treatment outcome in eating disorders. International Journal of Eating Disorders, 50(4), 323–340. [DOI] [PubMed] [Google Scholar]
- Guidi J, Brakemeier EL, Bockting CL, Cosci F, Cuijpers P, Jarrett RB, … & Rief W (2018). Methodological recommendations for trials of psychological interventions. Psychotherapy and psychosomatics, 1–9. [DOI] [PubMed] [Google Scholar]
- Hogue A, Dauber S, Henderson CE, Bobek M, Johnson C, Lichvar E, & Morgenstern J (2015). Randomized trial of family therapy versus nonfamily treatment for adolescent behavior problems in usual care. Journal of Clinical Child & Adolescent Psychology, 44(6), 954–969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogue A, Henderson CE, Dauber S, Barajas PC, Fried A, & Liddle HA (2008). Treatment adherence, competence, and outcome in individual and family therapy for adolescent behavior problems. Journal of consulting and clinical psychology, 76(4), 544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holder N, Holliday R, Williams R, Mullen K, & Surís A (2018). A preliminary examination of the role of psychotherapist fidelity on outcomes of cognitive processing therapy during an RCT for military sexual trauma-related PTSD. Cognitive behaviour therapy, 47(1), 76–89. [DOI] [PubMed] [Google Scholar]
- Isserlin L, & Couturier J (2012). Therapeutic alliance and family-based treatment for adolescents with anorexia nervosa. Psychotherapy, 49(1), 46. [DOI] [PubMed] [Google Scholar]
- Jo B (2008). Bias mechanisms in intention-to-treat analysis with data subject to treatment noncompliance and missing outcomes. Journal of Educational and Behavioral Statistics, 33(2), 158–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kosmerly S, Waller G, & Robinson AL (2015). Clinician adherence to guidelines in the delivery of family‐based therapy for eating disorders. International Journal of Eating Disorders, 48(2), 223–229. [DOI] [PubMed] [Google Scholar]
- Little RJ, & Rubin DB (2014). Statistical analysis with missing data (Vol. 333). John Wiley & Sons. [Google Scholar]
- Lock J, Agras WS, Bryson S, & Kraemer HC (2005). A comparison of short-and long-term family therapy for adolescent anorexia nervosa. Journal of the American Academy of Child & Adolescent Psychiatry, 44(7), 632–639. [DOI] [PubMed] [Google Scholar]
- Lock J, & Le Grange D (2015). Treatment manual for anorexia nervosa: A family-based approach. Guilford Publications. [Google Scholar]
- Lock J, Le Grange D, Agras WS, Moye A, Bryson SW, & Jo B (2010). Randomized clinical trial comparing family-based treatment with adolescent-focused individual therapy for adolescents with anorexia nervosa. Archives of general psychiatry, 67(10), 1025–1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loeb KL, Wilson GT, Labouvie E, Pratt EM, Hayaki J, Walsh BT, … & Fairburn CG (2005). Therapeutic alliance and treatment adherence in two interventions for bulimia nervosa: A study of process and outcome. Journal of consulting and clinical psychology, 73(6), 1097. [DOI] [PubMed] [Google Scholar]
- Lu W, Yanos PT, Gottlieb JD, Duva SM, Silverstein SM, Xie H, … & Mueser KT (2012). Use of fidelity assessments to train clinicians in the CBT for PTSD program for clients with serious mental illness. Psychiatric Services, 63(8), 785–792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madden S, Miskovic-Wheatley J, Wallis A, Kohn M, Lock J, Le Grange D, … & Touyz S (2015). A randomized controlled trial of in-patient treatment for anorexia nervosa in medically unstable adolescents. Psychological medicine, 45(2), 415–427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marvin SE, Miklowitz DJ, O’brien MP, & Cannon TD (2016). Family‐focused therapy for individuals at clinical high risk for psychosis: treatment fidelity within a multisite randomized trial. Early intervention in psychiatry, 10(2), 137–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marvin SE, Miklowitz DJ, O’brien MP, & Cannon TD (2016). Family‐focused therapy for individuals at clinical high risk for psychosis: treatment fidelity within a multisite randomized trial. Early intervention in psychiatry, 10(2), 137–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nadeem E, Gleacher A, Pimentel S, Hill LC, McHugh M, & Hoagwood KE (2013). The role of consultation calls for clinic supervisors in supporting large-scale dissemination of evidence-based treatments for children. Administration and Policy in Mental Health and Mental Health Services Research, 40(6), 530–540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perepletchikova F, Treat TA, & Kazdin AE (2007). Treatment integrity in psychotherapy research: analysis of the studies and examination of the associated factors. Journal of consulting and clinical psychology, 75(6), 829. [DOI] [PubMed] [Google Scholar]
- Perepletchikova F, & Kazdin AE (2005). Treatment integrity and therapeutic change: Issues and research recommendations. Clinical Psychology: Science and Practice, 12(4), 365–383. [Google Scholar]
- Pereira T, Lock J, & Oggins J (2006). Role of therapeutic alliance in family therapy for adolescent anorexia nervosa. International Journal of Eating Disorders, 39(8), 677–684. [DOI] [PubMed] [Google Scholar]
- Peterson CB, Becker CB, Treasure J, Shafran R, & Bryant-Waugh R (2016). The three-legged stool of evidence-based practice in eating disorder treatment: research, clinical, and patient perspectives. BMC medicine, 14(1), 69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raudenbush SW, & Bryk AS (2002). Hierarchical linear models: Applications and data analysis methods (Vol. 1). Sage. [Google Scholar]
- Robbins MS, Feaster DJ, Horigian VE, Puccinelli MJ, Henderson C, & Szapocznik J (2011). Therapist adherence in brief strategic family therapy for adolescent drug abusers. Journal of consulting and clinical psychology, 79(1), 43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoenwald SK, & Garland AF (2013). A review of treatment adherence measurement methods. Psychological assessment, 25(1), 146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoenwald SK, Mehta TG, Frazier SL, & Shernoff ES (2013). Clinical supervision in effectiveness and implementation research. Clinical Psychology: Science and Practice, 20(1), 44–59. [Google Scholar]
- Snippe E, Schroevers MJ, Tovote KA, Sanderman R, Emmelkamp PM, & Fleer J (2018). Explaining variability in therapist adherence and patient depressive symptom improvement: The role of therapist interpersonal skills and patient engagement. Clinical psychology & psychotherapy. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Southam‐Gerow MA, & McLeod BD (2013). Advances in applying treatment integrity research for dissemination and implementation science: Introduction to special issue. Clinical Psychology: Science and Practice, 20(1), 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borrelli B, Sepinwall D, Ernst D, Bellg AJ, Sharp DL, Ogedegbe G, et al. A new tool to assess treatment fidelity and evaluation of treatment fidelity across 10 years of health behaviour research. J Consult Clin Psych 2005;75:852–860. [DOI] [PubMed] [Google Scholar]
- Teague GB, Mueser KT, & Rapp CA (2012). Advances in fidelity measurement for mental health services research: four measures. Psychiatric Services, 63(8), 765–771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson D, Cachelin F, Striegel‐Moore RH, Barton B, Shea M, & Wilson GT (2012). How many therapists? Practical guidance on investigating therapist effects in randomized controlled trials for eating disorders. International Journal of Eating Disorders, 45(5), 670–676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tschuschke V, Crameri A, Koehler M, Berglar J, Muth K, Staczan P, … & Koemeda-Lutz M (2015). The role of therapists’ treatment adherence, professional experience, therapeutic alliance, and clients’ severity of psychological problems: Prediction of treatment outcome in eight different psychotherapy approaches. Preliminary results of a naturalistic study. Psychotherapy Research, 25(4), 420–434. [DOI] [PubMed] [Google Scholar]
- Walker S, Srinivasan R, Fialko L, & Cini E (2017). Comparing family-based treatment with parent-focused treatment for adolescent anorexia nervosa. Archives of Disease in Childhood-Education and Practice, edpract-2017. [DOI] [PubMed] [Google Scholar]
- Waller G (2016). Treatment protocols for eating disorders: Clinicians’ attitudes, concerns, adherence and difficulties delivering evidence-based psychological interventions. Current psychiatry reports, 18(4), 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waller G, & Turner H (2016). Therapist drift redux: Why well-meaning clinicians fail to deliver evidence-based therapy, and how to get back on track. Behaviour research and therapy, 77, 129–137. [DOI] [PubMed] [Google Scholar]
- Weisz JR, Southam-Gerow MA, Gordis EB, Connor-Smith JK, Chu BC, Langer DA, … & Weiss B (2009). Cognitive–behavioral therapy versus usual clinical care for youth depression: An initial test of transportability to community clinics and clinicians. Journal of Consulting and Clinical Psychology, 77(3), 383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb CA, DeRubeis RJ, & Barber JP (2010). Therapist adherence/competence and treatment outcome: A meta-analytic review. Journal of consulting and clinical psychology, 78(2), 200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilfley DE, Welch RR, Stein RI, Spurrell EB, Cohen LR, Saelens BE, … & Matt GE (2002). A randomized comparison of group cognitive-behavioral therapy and group interpersonal psychotherapy for the treatment of overweight individuals with binge-eating disorder. Archives of general psychiatry, 59(8), 713–721. [DOI] [PubMed] [Google Scholar]
- Wisniewski L, Hernandez MEH, & Waller G (2018). Therapists’ self-reported drift from dialectical behavior therapy techniques for eating disorders. Eating behaviors, 28, 20–24. [DOI] [PubMed] [Google Scholar]


