Abstract
Hispanics/Latinos are the largest ethnic/racial group in the US and at high risk for Alzheimer’s disease and related dementia (ADRD). Yet, ADRD among diverse Latinos are poorly understood and disparately understudied or unstudied compared to other ethnic/racial groups that leave the nation ill-prepared for major demographic shifts that lay ahead in coming decades. The primary purpose of this Perspectives article is to provide a new research framework for advancing Latino ADRD knowledge, encompassing the unique sociocultural, cardiometabolic and genomic aspects of Latino health, aging and ADRD. In addition, we describe some of the research challenges to progress in Latino ADRD research. Lastly, we present the Study of Latinos – Investigation of Neurocognitive Aging (SOL-INCA) as an example of implementing this new framework for advancing Latino ADRD research.
Keywords: Epidemiology, neuroepidemiology, cognitive function, neurocognitive function, neuropsychology, Hispanics, Latinos, Hispanic/Latinos, population neuroscience
INTRODUCTION
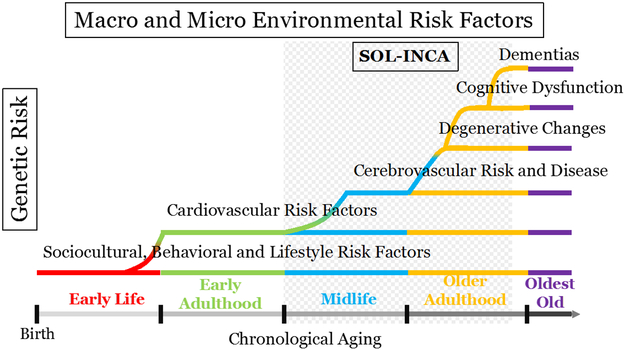
Alzheimer’s disease (AD) and related dementias (ADRD) are neurodegenerative disorders of aging that are leading causes of morbidity and mortality in the United States. ADRD affects many older adults and the risk increases with age, possibly affecting as many as 50% of adults over age 80-years.1 The US population is aging rapidly as life-expectancy increases due to public health improvements (e.g., decreased smoking), which have important implications for age-related disorders, particularly ADRD.2 Simultaneously, the US is growing increasingly ethnically/racially diverse. Over the next 30-years, the older Latino population is projected to increase 391%, which is more than any major ethnic/racial group.3 However, most past and ongoing ADRD research and clinical trials have included predominantly non-Latino White (hereafter White) study participants. Latinos comprise about one-fifth of an increasingly diverse America, and may be disproportionally affected by ADRD.4 Furthermore, the CDC projects the largest increase in ADRD will impact Latinos, which they attribute to disparities in cardiovascular disease (CVD) and its impact on brain health.5 The extant Latino ADRD research is based on outdated information that is fraught with inconsistencies and major gaps, which leaves US public health ill-prepared for expected ADRD expansion among Latinos. The Study of Latinos-Investigation of Latinos-Investigation of Neurocognitive Aging (SOL-INCA), which we describe below, provides a scientific framework for advancing the research on cognitive aging and disease in diverse Latinos (Figure 1).
Figure 1.
SOL-INCA a research framework for Latino cognitive aging and ADRD.
Epidemiologically, US ADRD prevalence estimates vary markedly between Latinoa backgrounds and range from roughly 21% Caribbean (i.e., Dominican and Puerto Rican; ages 65-years and older) to 4.8% for Mexican and Central American backgrounds (i.e., ages 60-years and older).6,7 Caribbean background ADRD incidence is comparable to Whites, but incidence for Mexicans is unknown.8 The reasons for this 4.3-fold difference in ADRD prevalence estimates between Latino backgrounds have not been examined for two decades leaving major scientific gaps for this significant population. In this Perspectives article, we will briefly describe existing research focusing on three key aspects of Latino cognitive health and ADRD research: sociocultural, cardiometabolic and genomic. In doing so, we will describe some challenges to progress and new opportunities for advancing Latino cognitive aging and ADRD research.
Latino diversity:
Latinos are genetically diverse, a diversity that closely follows the history of the Americas dating perhaps as far back as 25,000 years ago to the relatively brief 500-year colonial and current era.9 Highly advanced, large and genetically diverse populations of American Indians (Amerindians) occupied and adapted to the American continents for millennia. Mid-millennial European colonization and African forced migration to the Americas about 500 years ago dramatically altered the genetic diversity of Latinos. In general, three major genetic continental ancestries are represented among diverse Latinos: Amerindian (higher proportion in Mexicans, Central and South Americans); African (primarily Dominicans and Puerto-Ricans); and European (e.g., older Cuban adults).10
In sheer numbers, Latino health, in particular ADRD, is highly significant to the vitality of the US. In California, the nation’s most populous state, Latinos are the majority population and comprise nearly 40% of the population. Texas, the nation’s second most populous state, follows closely behind California as both states revert back to pre-US expansion Latino majority populations. Latinos living in the US have diverse Latin American origins with Mexican background accounting for nearly two-thirds (64.6%) of the population, and Puerto Ricans (9.5%), Cubans (3.6%), Dominican (3.0%) and Central Americans (8.3%) representing the other major Latino groups.2 Research that examines and understands how sociocultural and health profiles vary between diverse Latinos is still nascent.
Latino health:
Average Latino life-expectancy at birth (82.8y) exceeds that of Whites (78.8y) by 4-years.2 Paradoxically, Latino longevity exists despite sociodemographic disadvantages, high rates of diabetes and the lowest healthcare insurance coverage rates of any major ethnic/racial group in the US.2,11-13 Latino paradoxical longevity remains poorly understood scientifically suggesting new approaches are needed (e.g., genomics). For example, it is unknown if there is differential longevity between Latino groups. It has been suggested that the healthy immigrant effect explains Latino longevity in the US, but the few studies of older Latinos indicate that this healthy immigrant advantage endures into older adulthood.14,15 Socioeconomically, Latinos, on average, lag behind Whites and African Americans in education,16 and low education is a major risk for ADRD.17 Latino median annual household income is $17,500 lower than Whites, and poverty rates of Latinos are more than double that of Whites.2 Latinos have the highest uninsured rates for non-elderly and elderly adults. Latino longevity, high morbidity, low education and limited healthcare access form a perfect storm for expansions of age-related disorders, specifically ADRD.
Age-adjusted Latino cardiovascular health (CVH) is relatively good compared to Whites and Blacks, which is less indicative of good Latino CVH and more a testimony of the need for continued improvement in CVH for all Americans.18-20 Nevertheless, Latinos lead the nation in obesity (46.9% women; 37.9% men),21 which is associated with CVD, diabetes, stroke and ADRD. Recent findings from the HCHS/SOL indicate that CVD risk factors vary between Latino backgrounds.22,23 For example, the prevalence of type 2 diabetes among adults ages 18-74 years ranges from 18.3% among Mexican to 10.3% among South American backgrounds.11 Regrettably, some Latino CVD risks (e.g., diabetes) exceed that of Whites and if left unmitigated due to inaccessible healthcare will further increase vascular contributions to cognitive impairment and dementias and disease burden.
Genomics:
Genomically, we are at the frontier of improving the precision of Latino ADRD scientific knowledge by leveraging multiple powerful resources and tools. This is important because it is now known that apolipoprotein E genotypes vary between Latino backgrounds.24 Genome-wide association studies (GWAS), the preferred tool for discovering the genetic factors influencing common diseases, remain scarce among Latino populations. This is likely due to insufficient sample sizes needed to achieve reasonable statistical power to detect genetic effects. Furthermore, genetic replication studies, essential for rigorous genomic science, are especially challenging for studying the genetics of Amerindian ancestry groups due to data sparsity. Under-representation of Latino populations in genetic research represents missed opportunities for the application of genomic medicine in health research and care. While Latino genomic ADRD research is stymied by major gaps in available data, other health outcomes are also impacted due to the dearth of genomic data available for the largest Latino admixed subgroup. Nevertheless, new HCHS/SOL GWAS, whole genome sequencing and epigenetics research are beginning to emerge in the research literature.
Cognitive aging and ADRD research challenges:
There are many practical challenges to conducting neuroepidemiologic research among English- and Spanish-speaking Latinos from diverse backgrounds. First, appropriate, large and representative normative cognitive data are essential for improving test characteristics; however, such data do not currently exist for diverse Latinos. Therefore, the normative data must be generated de novo in order to control unwanted bias in cognitive assessments of Latinos. For example, in order to determine if the cognitive test score of a 70-year old, Spanish-speaking, Mexican American woman with 4-years of education is in the impaired range, it is essential to have test score data from a large and representative sample of healthy persons (e.g., stroke free) with comparable demographic characteristics with a wide range of cognitive abilities. Comparing the test scores of this hypothetical person with a highly educated, English-speaking person increases the likelihood of falsely identifying our Mexican American woman as cognitively impaired (false positive) or at the population-level, overestimating the prevalence of ADRD. The current state of Latino clinical practice and ADRD research leaves practitioners and investigators without objective references for identifying what is normal or abnormal cognitive function, except in obvious cases of severely advanced dementia. Secondly, representative sampling of Latinos from diverse backgrounds entails targeting and enrolling participants in distant regions with sufficiently large and specific Latino populations. Consequently, most Latino ADRD research has been driven by the practicalities of institutional propinquity to Latino populations, and less by representative population-based sampling. For example, Dominicans comprise about 3% of Latinos in the US; however, they are the most studied Latinos in ADRD research, in part, due to the proximity of outstanding research groups in the eastern US. Thirdly, test materials must be available in two languages, not one, which increases costs, time and work needed for initiating an inclusive Latino ADRD research study. Fourthly, although Latinos share the Spanish language, ethno-regional linguistic differences, if unattended to in test construction and implementation, can have important consequences for data quality and test invariance. For example, owl translates to buho in Castilian Spanish in Europe, but in Mexico, the most populous Spanish-speaking country globally, the word tecolote (from Náhuatl, tecolotl) and other Náhuatl-origin words are most commonly used and understood. Thus, neurocognitive tests developed or translated for use with a particular Latino group must undergo additional reviews by experts with knowledge of language differences among Latino backgrounds. Fifthly and in general, the current ADRD scientific workforce is small and must grow to meet the present and future ADRD research challenges facing this significant population. The workforce pipeline for Latino early stage investigators or those committed to Latino ADRD research careers is small. Further compounding the state of Latino ADRD research is the fact that Latino diversity is not well understood in general. ADRD findings for one group are often improperly generalized to all Latinos. Finally, creating and funding the necessary infrastructure and national network for designing and implementing a large study of diverse Latino ADRD de novo can be overwhelmingly costly. These and other challenges may partially explain the sustained current gaps and disparities in Latino ADRD research.
In summary, Latinos are a significant and growing part of the US population that is socioculturally, cardiometabolically and genetically diverse, and facing major risks for ADRD. There are significant gaps in scientific knowledge and major challenges to advancing cognitive aging and ADRD research among diverse Latinos. We posit that a new framework is needed for clarifying current understanding of cognitive aging and ADRD among diverse Latinos. In this Perspectives article, we describe a new research framework for advancing Latino cognitive aging and ADRD research. To do so, we present the Study of Latinos – Investigation of Neurocognitive Aging (SOL-INCA), which is a new and large study of cognitive health, aging and disorders in diverse middle-aged and older Latinos. This framework and SOL-INCA are predicated on the central concept that preventing Latino dementia in late life begins with understanding and modifying cardiovascular health decades earlier in midlife.25{Hachinski, 2019 #7475}
METHODS
Study design.
SOL-INCA is an ancillary study of Hispanic Community Health Study/Study of Latinos (HCHS/SOL). First, we will briefly describe HCHS/SOL to provide readers with the context of SOL-INCA. HCHS/SOL is the latest prospective cohort study of cardiovascular/pulmonary disease (CVPD) supported by the National Heart Lung and Blood Institute (NHLBI) and other National Institutes of Health (NIH) institutes. As with other NHLBI cohorts (e.g., Framingham Heart Study), HCHS/SOL and SOL-INCA data will become publically available. HCHS/SOL is a population-based, multisite, prospective cohort study (Visit 1 enrollment years 2008-2011). The sample design was formulated to estimate CVPD risk factors and disease prevalence and incidence for Latinos in general and diverse subgroups. Data were collected at four Field Centers located in US cities with sizable targeted Latino population concentrations. Each Field Center (Bronx, NY; Chicago, IL; Miami, FL; and San Diego, CA) recruited about 4,000 eligible, self-identified Latino adults (ages 18-74 years; N=16,415). Middle-aged and older Latinos (ages 45-74 years) were oversampled (n=9,652). Briefly, the HCH/SOL Baseline Field Center in-clinic visits were conducted in-person by bilingual/bicultural technicians who were trained to conduct anthropometry, blood draws, blood pressure readings, and other important CVPD risks. Included in the 6-hour in-clinic visit were several Reading Centers exams including: Audiometry, Echocardiography, Pulmonary, Neurocognition, and Nutrition. Only the oversampled middle-aged and older adults were administered cognitive tests.26 Biospecimens (e.g., blood, urine) were collected and assayed for key CVPD risk factors (e.g., triglycerides, hsCRP, CBC). Additional biospecimens were stored for later studies. Genomic data were collected on consenting participants. Detailed HCHS/SOL sampling methods and procedures have been published elsewhere and additional study information is available on the HCHS/SOL website: https://sites.cscc.unc.edu/hchs/).27,28 SOL-INCA efficiently leverages the HCHS/SOL cohort with its rich sociocultural, health and multilayered –omics data to enable a study cognitive health, aging and disorders among diverse middle-aged and older Latinos.
Neurocognitive Reading Center (NRC).
The Baseline cognitive battery included 4 tests: (1) Six-Item Screener (SIS; mental status);29 (2) Brief-Spanish English Verbal Learning Test (BSEVLT; verbal episodic learning and memory);30 (3) Controlled Oral Word Association (or Word Fluency; WF; verbal fluency) Test of the Multilingual Aphasia Examination; 31 and (4) Digit Symbol Subtest (DSS; processing speed).32 Trained bilingual/bicultural technicians conducted cognitive assessments on 9,652 eligible and consenting participants. Data quality was maintained using audio recordings of testing that were periodically reviewed to maintain data quality with standardized test administrations.
HCHS/SOL Visit 2 occurred between October 2014 and December 2017 and 11,623 HCHS/SOL participants returned for the second visit, which was on average 7-years after the Visit 1 Baseline. The Visit 2 protocol was much abbreviated, and the NRC and other Reading Centers (e.g., audiometry) were discontinued. In order to preserve cognitive assessments in HCHS/SOL, independent support for the SOL-INCA ancillary study to leverage the HCHS/SOL infrastructure and resources was obtained from the National Institute on Aging (R01AG048642). The HCHS/SOL Coordinating Center identified 7,420 potentially eligible participants, 50-years and older with baseline neurocognitive testing, who were screened at Visit 2 and completed the SOL-INCA Eligibility and Screening form. Out of this group 222 were considered ineligible, 569 were eligible and refused, and 6377 were eligible and agreed to participate. The overall eligible participant response rate for SOL-INCA was 88.7%. The response rates varied slightly by Field Center: Bronx 86.4%, Chicago 87.9%, Miami 91.3% and San Diego 88.7%. The specific aims of the SOL-INCA were to examine sociocultural, cardiometabolic and genomic risk and resilience factors for cognitive aging, decline and disorders. The relative youth of the HCHS/SOL and SOL-INCA cohorts affords unique midlife, preclinical stage windows into cognitive aging and Mild Cognitive Impairment (MCI).
The SOL-INCA cognitive test battery was expanded to achieve 3 goals to: 1) identify MCI endophenotypes, 2) conserve longitudinal assessments, and 3) do so efficiently with low participant and staff burden. Distributional plots for the cognitive tests included in SOL-INCA by Latino background are provided in Supplemental Figure 1. Participants were eligible for SOL-INCA if they had a Baseline cognitive assessment and were over age 50-years at SOL Visit 2. Trained bilingual/bicultural technicians administered the same Baseline cognitive battery plus the Trail Making Test (TMT; A&B) and NIH Toolbox Picture Vocabulary Test (PVT). The TMT is a test of executive function, and the PVT is a “crystalized knowledge” or “hold” test of general cognitive ability that was selected to complement the existing baseline battery.33 Additionally, self-reported cognitive decline was assessed with the 12-item Everyday Cognition (eCog-12) scale of (memory, language, visuospatial, planning, organization, and divided attention).34 Distributional plots for the eCog summary scores by Latino background are provided in Supplemental Figure 2. Lastly, we administered an Instrumental Activities of Daily Living (IADL) scale to assess functional status. SOL-INCA quality assurance procedures were similar to those at Baseline.35
Cognitive internal normative sample.
To overcome the current dearth of normative cognitive data needed to appropriately identify cognitively impaired participants in SOL-INCA, we used the “absolute” score approach, in which we compare a participant’s test performances to a sample of healthy controls (i.e. “robust norms”).36 In addition, we used significant cognitive decline scores (described below) to complement our absolute score approach. A major challenge was that no other sizable normative data exists for diverse Latinos (e.g., Central Americans). Therefore, we generated robust normative data from SOL-INCA interim data releases. Due to complex sampling procedures used in HCHS/SOL, each interim normative sample was largely representative of the target population. The SOL-INCA robust normative data excluded participants who self-reported neurologic disorders (e.g., stroke/transient ischemic attack, multiple sclerosis, Parkinson’s disease, brain tumor, dementia or anti-dementia medication use, highly elevated depressive symptoms [CESD-10>=20], neurosurgery or brain/skull radiation, and apoE44 carriers; Supplemental Table 1).
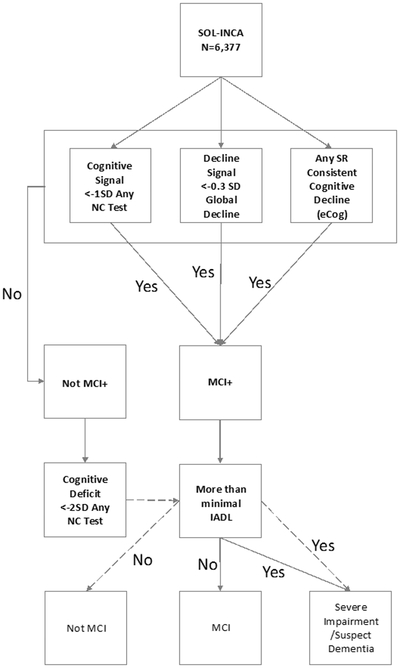
MCI Diagnostic criteria (Figure 2).
Figure 2.
SOL-INCA MCI Diagnostic Schema.
Note1: SR=Self-reported; SD= Standard deviation; NC=Neurocognitive; IADL=Instrumental Activity of Daily Living; eCog=Every day cognition.
Note 2: Participants with MCI Diagnosis must have 1) significant self-reported cognitive decline (eCog-12); 2) low age-, sex-, education-, and PVT-adjusted absolute cognitive test scores relative to SOL-INCA internal normative ranges, and significant global cognitive decline in test performances of at least −0.055 SD yearly; and 3) no to mild functional impairment (IADLs, e.g., managing medications).
In SOL-INCA, we used National Institute on Aging- Alzheimer’s Association (NIA-AA) criteria for MCI syndromes.37-39 SOL-INCA used a singlestage procedure to identify MCI syndromes in which MCI cases evinced: 1) significant self-reported cognitive decline (eCog-12); 2) low age-, sex-, education-, and PVT-adjusted absolute cognitive test scores (≦ −1 SD) relative to SOL-INCA internal normative ranges, and significant global cognitive decline in test performances of at least −0.055 SD yearly; and 3) no to mild functional impairment (IADLs, e.g., managing medications). We present the distribution for the eCog indicators by Latino background and age groups (50-59; 60-69; and 70+ years) in Supplemental Figure 3. We include the distributions of the absolute cognitive tests scores classification by age groups and Latino background in Supplemental Figure 4. Finally, we include the distribution of the IADL indicators in Supplemental Figure 5. The details of the analytical procedures used to operationalize MCI are available in supplementary text (Appendix 1).
Cardiovascular/Pulmonary disease measures.
The HCHS/SOL cohort is well characterized for CVPD risk factors, however, CVD risk factors are currently of primary interest to SOL-INCA (Supplemental Table 2). As such, SOL-INCA is well-positioned to leverage the HCHS/SOL’s rich information at critical developmental periods, such as midlife, to understand brain health, aging and diseases. A full description of the CVPD risk factors acquisition procedures are beyond the scope of this manuscript, and we refer interested readers to previous HCHS/SOL publications for further information.28,40
Genetics in SOL-INCA.
HCHS/SOL collected 80 mL of blood from consenting participants (n=12,278) at Baseline from which DNA was extracted and then genotyped on an Illumina custom array (SOL-HCHS Custom 15041502 B3) consisting of the Illumina Omni 2.5M array (HumanOmni2.5-8.v111, San Diego, CA). Ancestry-informative markers of about 150,000 custom SNPs were selected and included Amerindian population variants that have been previously identified as GWAS hits along with other candidate-gene polymorphisms.10 Genome-wide imputation was conducted with the 1000 Genome Project reference panel.41 Interested readers are referred to previously published works.42 ApoE genotyping was performed as part of SOL-INCA using commercial TaqMan assays and additional details are available elsewhere.24
Cohort characteristics.
Weighted descriptive characteristics of the SOL-INCA target population by Latino background are provided in Table 1. The average age was 63.4±8.2 years, 26% were over age 70-years, and 54.5% were female. Only two-fifths had >12-years of education, and 87% indicated Spanish as their language of preference.
Table 1.
Weighted descriptive characteristics of the SOL-INCA target population by Latino background.
| Dominican | Central American |
Cuban | Mexican | Puerto Rican |
South American |
Other | Overall | ||
|---|---|---|---|---|---|---|---|---|---|
| Age in years | |||||||||
| Mean (SD) | 62.6(8.0) | 62.7(8.9) | 65(6.9) | 62.1(8.2) | 64.5(8.4) | 63.4(9.7) | 63.3(5.8) | 63.4(8.2) | |
| Age (%) | |||||||||
| 50-59 | 42.4 | 40.9 | 32.4 | 44.4 | 33.0 | 39.2 | 42.2 | 38.7 | |
| 60-69 | 36.3 | 38.9 | 32.5 | 36.5 | 37.0 | 36.2 | 33.4 | 35.6 | |
| 70+ | 21.3 | 20.3 | 35.2 | 19.0 | 30.0 | 24.6 | 24.4 | 25.7 | |
| Sex (%) | |||||||||
| Female | 60.4 | 60.2 | 49.0 | 56.2 | 53.6 | 57.3 | 52.9 | 54.5 | |
| Education (in years) | |||||||||
| <12 | 45.7 | 43.0 | 23.7 | 48.4 | 42.8 | 24.2 | 31.2 | 38.6 | |
| 12 | 19.8 | 19.7 | 24.8 | 20.1 | 22.3 | 19.6 | 11.4 | 21.2 | |
| >12 | 34.6 | 37.3 | 51.5 | 31.6 | 34.9 | 56.2 | 57.4 | 40.2 | |
| Language Preference (%) | |||||||||
| Spanish | 96.8 | 96.7 | 96.2 | 89.4 | 54.5 | 96.6 | 75.7 | 86.8 | |
Note: SD= Standard Deviation
DISCUSSION
We are at the frontier of better understanding Latino diversity and its implications for a new framework on Latino ADRD research. ADRD research has advanced in the past decades; however, a significant one-fifth of the nation’s population has been left behind. The National Institute of Health, National Alzheimer's Project Act (NAPA), and ADRD Summits have prioritized inclusiveness in research and the workforce to reflect the nation’s ethnic/racial mosaic of taxpayers that support our scientific efforts to prevent and cure ADRD. However, ADRD research, including large consortia, has lagged behind in inclusion of ethnic/racial minorities resulting in grossly underpowered studies to yield meaningful results. Secondly, we are finding previously unreported variations between Latino groups in their sociocultural, genetic and health profiles indicating between-group variability should be examined before aggregating Latino groups in research.11,24,43 SOL-INCA represents a major opportunity to advance Latino ADRD research by efficiently leveraging the detailed sociocultural, cardiometabolic, and genomic data in a large, representative, prospective cohort study of cardiovascular disease. The SOL-INCA can also complement ongoing ADRD consortia with a large and well-characterized cohort of diverse Latinos. The prospective cohort study design enables unique early midlife windows into ADRD development at critical periods when lifestyle modification and pharmacotherapies may be most effective at ADRD prevention, prior to neurodegeneration and cognitive impairment. Given the demographic significance of Latinos and projected growth, it is vital that Latinos be well represented in research if we are to fully achieve national ADRD priorities.
To improve the precision of Latino ADRD research, specifying which Latino group that is being studied is essential and careful consideration of potential group differences should be considered prior to aggregating Latino groups to avoid imprecise results reporting. For example, while Cubans, Dominican and Puerto Ricans share Caribbean island origins and many cultural features; their socioeconomic and health profiles are quite different. Education levels are higher among Cubans compared to other groups in HCHS/SOL, which may reflect differences in their reasons for immigration and US policies that provided incentives and financial support to Cuban immigrants and not to other Latinos. Among Caribbean Latinos, smoking prevalence amongst Puerto Rican men (35.2%) and women (32.6%) are very high compared to Dominican men (11.0%) and women (11.7%).44 Aggregating Dominicans and Puerto Ricans in a study of older Caribbean Latinos invites selection bias due to differential survival related to tobacco use histories and early mortality from cancer and CVD events. (For additional nuanced variations in Latino culture and health, see Rodriguez et al.)45
It is our perspective that a comprehensive, lifecourse, multimodal research approach to Latino ADRD research can serve as a research framework for resolving disparities (Figure 1). ADRD risk begins with our genes at birth that may interact with various lifecourse factors, but to-date few studies of Latinos, save SOL-INCA, have had the capacity to examine GWAS, whole genome, epigenetic and other –omics data for neurodegeneration. CVPD risk factors also begin at birth, vary throughout the lifecourse and are associated with cerebrovascular disease risk (e.g., arteriolosclerosis, oligemia and blood-brain barrier dysfunction) and subacute and acute strokes.46 While excess CVPD risk is considered a leading cause of ADRD disparities among ethnic/racial minorities, there has been little research into mechanism by which excess CVPD contributes to ADRD disparities. Advanced biomarkers for AD and vascular contributions to cognitive impairment and dementia (VCID) hold promise for identifying at-risk individuals at preclinical phases of disease. Beta amyloid and tau neuroimaging techniques continue to advance and yield enhanced diagnostic information, but at no small cost. It is essential that all persons, including re underrepresented minorities, equitably have access to the best affordable diagnostic and research biomarkers, and provide culturally and linguistically appropriate results and access to early therapeutics. Blood-based biomarkers may gain acceptance, or not, with compelling data from representative and diverse study participants. An affordable, effective and inclusive approach would yield the greatest public health benefit in the US and globally.
The SOL-INCA MRI study, which is another HCHS/SOL ancillary study linked to the SOL-INCA, is currently is in the field acquiring new structural biomarker information on AD and vascular pathology. The field is rapidly advancing, and sets clear new goals for enhancing AD biomarkers in SOL-INCA. However, biomarkers are still surrogates of pathology and require targeted autopsy validation, which is a major challenge to the field. SOL-INCA collaborative efforts with Alzheimer’s Disease Centers are currently being developed to overcome these challenges. The National Alzheimer's Project Act (NAPA) goals are to effectively prevent and treat ADRD. In addition, a major priority of the NIH is to enhance and diversify the scientific workforce to meet the needs of our increasingly diverse nation. The HCHS/SOL and SOL-INCA are opening opportunities and training diverse, new investigators with fresh ideas and perspectives to advance their research careers while helping fill critical gaps in Latino ADRD science. As such, the SOL-INCA research platform serves as a framework for efficiently filling critical gaps and barriers to advancing ADRD science for the many Americans who call themselves Latinos.
Supplementary Material
Figure 3.
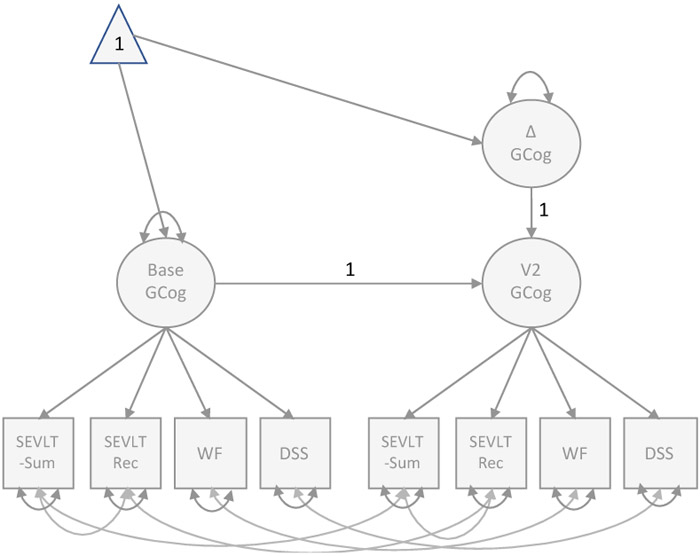
SOL-INCA Latent Change Score Model
Note: Multiple indicator univariate latent change score model. The latent construct of interest (GCOG) is measured at two time points (Baseline and SOL-INCA, six years later) each measured using four manifest variables (SEVLT-Sum SEVLT-Recall, Word Fluency, and Digit Symbol Substitution). Final model includes strict invariance and correlated residual errors over time. (see Kievett, 2017) 1
Acknowledgements:
The authors thank the staff and participants of HCHS/SOL for their important contributions. Investigators website - http://www.cscc.unc.edu/hchs/
Funding/Support:
This work is support by National Institute on Aging (R01AG048642, R01AG054548, R01AG061022, and R21AG056952). Dr. González also receives support from P30AG005131 and P30AG059299. The Hispanic Community Health Study/Study of Latinos was carried out as a collaborative study supported by contracts from the National Heart, Lung, and Blood Institute (NHLBI) to the University of North Carolina (N01-HC65233), University of Miami (N01-HC65234), Albert Einstein College of Medicine (N01-HC65235), Northwestern University (N01-HC65236), and San Diego State University (N01-HC65237). The following Institutes/Centers/Offices contribute to the HCHS/SOL through a transfer of funds to the NHLBI: National Institute on Minority Health and Health Disparities, National Institute on Deafness and Other Communication Disorders, National Institute of Dental and Craniofacial Research, National Institute of Diabetes and Digestive and Kidney Diseases, National Institute of Neurological Disorders and Stroke, NIH Institution-Office of Dietary Supplements.
Role of Funding Source: This work was supported by the National Institutes of Health and the National Institute on Aging in particular. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Financial Disclosures: The authors report no conflicts of interest that could inappropriately influence, or be perceived to influence, this work.
The terms Hispanic and Latino are commonly used interchangeably. We use the term Latino to specify US residents who have roots in Latin American, Spanish-speaking countries. The term Hispanic is derived from Latin Hispania and refers to the Iberian peninsula. Eligibility for this study included persons of Latin American background (i.e., Latino).
REFERENCES
- 1.Evans DA. Estimated prevalence of Alzheimer's disease in the United States. Milbank Q. 1990;68(2):267–289. [PubMed] [Google Scholar]
- 2.Census. American Community Survey. 2017.
- 3.Colby SL, Ortman JM. Projections of the Size and Composition of the US Population: 2014 to 2060. Population Estimates and Projections. Current Population Reports. P25–1143. US Census Bureau. 2015. [Google Scholar]
- 4.Mayeda ER, Glymour MM, Quesenberry CP, Whitmer RA. Inequalities in dementia incidence between six racial and ethnic groups over 14 years. Alzheimer's & Dementia: The Journal of the Alzheimer's Association. 12(3):216–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Matthews KA, Xu W, Gaglioti AH, et al. Racial and ethnic estimates of Alzheimer's disease and related dementias in the United States (2015-2060) in adults aged >/=65 years. Alzheimers Dement. 2019;15(1):17–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gurland BJ, Wilder DE, Lantigua R, et al. Rates of dementia in three ethnoracial groups. Int J Geriatr Psychiatry. 1999;14(6):481–493. [PubMed] [Google Scholar]
- 7.Haan MN, Mungas DM, Gonzalez HM, Ortiz TA, Acharya A, Jagust WJ. Prevalence of dementia in older Latinos: the influence of type 2 diabetes mellitus, stroke and genetic factors. Journal of the American Geriatrics Society. 2003;51(2):169–177. [DOI] [PubMed] [Google Scholar]
- 8.Stern Y, Gurland B, Tatemichi TK, Tang MX, Wilder D, Mayeux R. Influence of education and occupation on the incidence of Alzheimer's disease. Jama. 1994;271(13):1004–1010. [PubMed] [Google Scholar]
- 9.Raghavan M, Steinrucken M, Harris K, et al. Genomic evidence for the Pleistocene and recent population history of Native Americans. Science. 2015;349(6250):aab3884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Conomos MP, Laurie CA, Stilp AM, et al. Genetic diversity and association studies in US Hispanic/Latino populations: applications in the Hispanic Community Health Study/Study of Latinos. The American Journal of Human Genetics. 2016;98(1):165–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schneiderman N, Llabre M, Cowie CC, et al. Prevalence of Diabetes Among Hispanics/Latinos From Diverse Backgrounds: The Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Diabetes Care. 2014;37(8):2233–2239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Foundation” KF. Rate of Nonelderly Uninsured by Race/Ethnicity, U.S . 2016.
- 13.Hales CM, Fryar CD, Carroll MD, Freedman DS, Ogden CL. Trends in obesity and severe obesity prevalence in us youth and adults by sex and age, 2007-2008 to 2015-2016. JAMA. 2018;319(16):1723–1725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gonzalez HM, Ceballos M, Tarraf W, West BT, Bowen ME, Vega WA. The health of older Mexican Americans in the long run. Am J Public Health. 2009;99(10):1879–1885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gonzalez HM, Tarraf W, Haan MN. The metabolic syndrome, biomarkers, and the acculturation-health relationship among older Mexican Americans. J Aging Health. 2011;23(7):1101–1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gramlich J Hispanic dropout rate hits new low, college enrollment at new high. Pew Research Center Fact Tank, September 2017. [Google Scholar]
- 17.Fratiglioni L, Wang HX. Brain reserve hypothesis in dementia. J Alzheimers Dis. 2007;12(1):11–22. [DOI] [PubMed] [Google Scholar]
- 18.González HM, Tarraf W, Rodriguez CJ, et al. Cardiovascular health among diverse Hispanics/Latinos: Hispanic Community Health Study/Study of Latinos (HCHS/SOL) results. American heart journal. 2016;176:134–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shay CM, Ning H, Allen NB, et al. Status of Cardiovascular Health in US Adults: Prevalence Estimates from the National Health and Nutrition Examination Surveys (NHANES) 2003–2008. Circulation. 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lloyd-Jones DM, Hong Y, Labarthe D, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association's strategic Impact Goal through 2020 and beyond. Circulation. 2010;121(4):586–613. [DOI] [PubMed] [Google Scholar]
- 21.Flegal KM, Kruszon-Moran D, Carroll MD, Fryar CD, Ogden CL. Trends in obesity among adults in the United States, 2005 to 2014. Jama. 2016;315(21):2284–2291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Daviglus ML, Pirzada A, Durazo-Arvizu R, et al. Prevalence of Low Cardiovascular Risk Profile Among Diverse Hispanic/Latino Adults in the United States by Age, Sex, and Level of Acculturation: The Hispanic Community Health Study/Study of Latinos. J Am Heart Assoc. 2016;5(8). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Daviglus ML, Talavera GA, Aviles-Santa ML, et al. Prevalence of Major Cardiovascular Risk Factors and Cardiovascular Diseases Among Hispanic/Latino Individuals of Diverse Backgrounds in the United States. Jama-Journal of the American Medical Association. 2012;308(17):1775–1784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.González HM, Tarraf W, Jian X, et al. Apolipoprotein E genotypes among diverse middle-aged and older Latinos: Study of Latinos-Investigation of Neurocognitive Aging results (HCHS/SOL). Scientific Reports. 2018;8(1):17578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Khachaturian ZS, Kuller LH, Khachaturian AS. Strategic goals and roadmap for dementia prevention by stroke prevention. Alzheimer's & dementia: the journal of the Alzheimer's Association. 2019;15(7):865–869. [DOI] [PubMed] [Google Scholar]
- 26.González HM, Tarraf W, Gouskova N, et al. Neurocognitive Function Among Middle-aged and Older Hispanic/Latinos: Results from the Hispanic Community Health Study/Study of Latinos. Archives of Clinical Neuropsychology. 2015;30(1):68–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.LaVange LM, Kalsbeek WD, Sorlie PD, et al. Sample Design and Cohort Selection in the Hispanic Community Health Study/Study of Latinos. Annals of Epidemiology. 2010;20(8):642–649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sorlie PD, Aviles-Santa LM, Wassertheil-Smoller S, et al. Design and Implementation of the Hispanic Community Health Study/Study of Latinos. Annals of Epidemiology. 2010;20(8):629–641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Callahan CM, Unverzagt FW, Hui SL, Perkins AJ, Hendrie HC. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Med Care. 2002;40(9):771–781. [DOI] [PubMed] [Google Scholar]
- 30.González HM, Mungas D, Reed BR, Marshall S, Haan MN. A new verbal learning and memory test for English- and Spanish-speaking older people. J Int Neuropsychol Soc. 2001;7(5):544–555. [DOI] [PubMed] [Google Scholar]
- 31.Lezak M, Howieson DB, Loring DW. Neuropsychological Assessment. New York: Oxford University Press; 2004. [Google Scholar]
- 32.Wechsler D WAIS-R Manual. San Antonio, TX: Psychological Corporation; 1981. [Google Scholar]
- 33.Horn JL, Cattell RB. Refinement and test of the theory of fluid and crystallized general intelligences. Journal of Educational Psychology. 1966;57:253–270. [DOI] [PubMed] [Google Scholar]
- 34.Farias ST, Mungas D, Reed BR, et al. The measurement of everyday cognition (ECog): scale development and psychometric properties. Neuropsychology. 2008;22(4):531–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fillenbaum GG, Smyer MA. The Development, Validity, and Reliability of the Oars Multidimensional Functional Assessment Questionnaire. Journal of Gerontology. 1981;36(4):428–434. [DOI] [PubMed] [Google Scholar]
- 36.Ivnik RJ, Smith GE, Petersen RC, Boeve BF, Kokmen E, Tangalos EG. Diagnostic accuracy of four approaches to interpreting neuropsychological test data. Neuropsychology. 2000;14(2):163–177. [DOI] [PubMed] [Google Scholar]
- 37.Albert MS, DeKosky ST, Dickson D, et al. The diagnosis of mild cognitive impairment due to Alzheimer's disease: Recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers & Dementia. 2011;7(3):270–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Winblad B, Palmer K, Kivipelto M, et al. Mild cognitive impairment – beyond controversies, towards a consensus: report of the International Working Group on Mild Cognitive Impairment. Journal of Internal Medicine. 2004;256(3):240–246. [DOI] [PubMed] [Google Scholar]
- 39.APA. Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing: American Psychiatric Association; 2013. [Google Scholar]
- 40.Daviglus Ml TGAA-SM, et al. Prevalence of major cardiovascular risk factors and cardiovascular diseases among Hispanic/Latino individuals of diverse backgrounds in the United States. JAMA. 2012;308(17):1775–1784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Genome Project Consortium. An integrated map of genetic variation from 1,092 human genomes. Nature. 2012;491(7422):56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sofer T, Wong Q, Hartwig FP, et al. Genome-Wide Association Study of Blood Pressure Traits by Hispanic/Latino Background: the Hispanic Community Health Study/Study of Latinos. Scientific Reports. 2017;7(1):10348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.González HM, Vega WA, Williams DR, Tarraf W, West BT, Neighbors HW. Depression Care in the United States: Too Little for Too Few. Arch Gen Psychiatry. 2010;67(1):37–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kaplan RC, Bangdiwala SI, Barnhart JM, et al. Smoking Among U.S. Hispanic/Latino Adults: The Hispanic Community Health Study/Study of Latinos. American Journal of Preventive Medicine. 2014;46(5):496–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rodriguez CJ, Allison M, Daviglus ML, et al. Status of Cardiovascular Disease and Stroke in Hispanics/Latinos in the United States: A Science Advisory From the American Heart Association. Circulation. 2014;130(7):593–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zlokovic BV. Neurovascular pathways to neurodegeneration in Alzheimer's disease and other disorders. Nat Rev Neurosci. 2011;12(12):723–738. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.