Abstract
Introduction:
Many strategies to alleviate racial/ethnic disparities in surgical care target healthcare providers. Yet limited data exists about the perception of disparities among the range of clinical staff who work in perioperative settings. Such information could help initiate conversations about disparities in perioperative care and, if necessary, implement interventions to alleviate them. Our aim was to evaluate the association between sociodemographic characteristics, clinical position (physicians and non-physicians) and perception of perioperative disparities at a large tertiary care center.
Methods:
We surveyed perioperative staff at the institution using an anonymous online survey. Primary outcome was respondents’ perception of disparities in perioperative care at the institution due to patients’ insurance status/type, ability to speak English, education, and racial/ethnic minority status. The association between clinical position (physician vs. non-physician) and perception of disparities was assessed in bivariate and then multivariable analysis, adjusting for respondents’ race, sex, age, and years at the institution. Secondary outcomes included perception of disparities in perioperative care in the United States due to patients’ insurance status/type, ability to speak English, education, and racial/ethnic minority status.
Results:
217 completed questions that could be analyzed. Among these responders, 101 were physicians (46.5%), 165 (76.0%) were white, and 144 (66.4.%) were female. Bivariate and multivariate analysis revealed that physicians had higher perception of disparities in perioperative care at the institution based on patients’ ability to speak English, education, and racial/ethnic minority status. Physicians also had higher perceptions of disparities in perioperative care in the United States than non-physicians.
Conclusions:
Physicians reported higher perceptions of disparities in perioperative care than non-physicians, potentially explained by differences in training or contact with patients. Such findings serve as a first step at examining and discussing disparities in perioperative care and warrant further study.
Keywords: healthcare disparities, health personnel, race/ethnicity, perioperative
1. INTRODUCTION:
Many studies document racial/ethnic disparities in surgical care, including lower rates of certain types of surgeries,1,2 longer operative times,3 more postoperative complications,1,4 and longer length of postoperative hospital stay for racial/ethnic minority as compared to White patients.5 Some research suggests that other sociodemographic characteristics, including inability to speak English and low socioeconomic status, are linked to receipt of lower quality care.6,7
Although such disparities have been well-described, three previous studies demonstrated that surgical providers barely acknowledge them as facts. Only 36.6% of surveyed general surgeons,8 13% of surveyed cardiothoracic surgeons,9 and 9% of surveyed orthopedic surgeons10 endorsed a belief that racial/ethnic disparities exist in their respective specialties nationwide. Moreover, surgeons’ acknowledgement decreased dramatically when they considered their own practice settings; they were more likely to identify disparities nationwide than at their own hospital or offices.8,9,10
Studies have focused primarily on surgical outcomes and surgeons’ acknowledgment, with little data available about disparities throughout the perioperative period—from the preoperative check-in/holding area to the intraoperative operating room to the postoperative recovery room.11,12 Likewise, no studies, to our knowledge, have focused on other members of perioperative staff with whom a patient interacts on the day of surgery, including physicians (like anesthesiologists) or non-physicians (like nurses, patient care assistants, or certified surgical technicians). As hospitals and other organizations strategize to meet and alleviate disparities in care, one factor under consideration is providers’ knowledge and attitudes about disparities.6 Given that “provider” may signify a wide variety of staff, distinguishing among physician versus non-physician staff may help initiate and guide conversations about disparities in perioperative care for each group and subsequently delineate targeted interventions.
Given the absence of literature about disparities tied to perioperative workers, surveys of staff about disparities in perioperative care might focus more on perceptions rather than awareness or acknowledgement, emphasizing attitudes over actual circumstances. The objective of this study was to determine how clinical position as physician or non-physician was associated with different perceptions of perioperative disparities at a large urban tertiary care center. We compared physicians and non-physicians to mirror the traditional organizing dichotomy within healthcare settings.13 Given the absence of literature on this topic, we conducted an exploratory analysis as to whether non-physicians or physicians were more likely to perceive disparities in perioperative care at their institution and in the United States due to patients’ insurance status (1), ability to speak English (2), education (3), and racial/ethnic minority status (4). Finally, we evaluated the association of clinical position and other respondent demographics on perceptions of the impact of systemic factors (such as access to care) in explaining disparities in care.
2. MATERIALS AND METHODS:
The Institutional Review Board at our institution approved this study. Completion of the survey indicated informed consent, with no written informed consent obtained to ensure anonymity.
2.1. Recruitment of participants:
A recruitment email to possible participants was sent approximately one month prior to initiation of the study. The survey and its purpose were also presented at staff meetings so possible participants could ask questions. In July 2017, we sent an anonymous online self-administered survey to 1426 eligible participants who worked in the perioperative environment at the institution. After discussion with the Perioperative Services Department, we included staffing groups who had contact with patients: nurses and patient care assistants who work in the preoperative and postoperative holding areas, operating room nurses, certified scrub technicians, anesthesia technicians, and staff and trainee physicians (anesthesiologists, general surgeons, gynecologists, orthopedic surgeons, urologist, neurosurgeons, oral and maxillofacial surgeons). Three subsequent emails, approximately one week apart, were sent to encourage participation, making the survey available to all participants for one month.
2.2. Inclusion criteria:
Given our response rate, we recoded all nurses, patient care assistants, certified scrub technicians, and anesthesia technicians as “non-physicians.” A priori, to assure anonymity, physicians of different specialties and rank were coded as “physicians.”
2.3. Survey
Our survey (with 5 questions about participants’ work position, 10 multi-part questions about perceptions of disparities, and 7 demographic questions; available as Supplementary Material) was adapted from four separate studies8,9,14,15 for use among the perioperative staff at our institution. The survey, administered using REDCap, was modified to focus on perioperative care both at this institution and in the United States, and was reviewed by two survey researchers and three perioperative staff members outside our institution.
2.4. Survey items
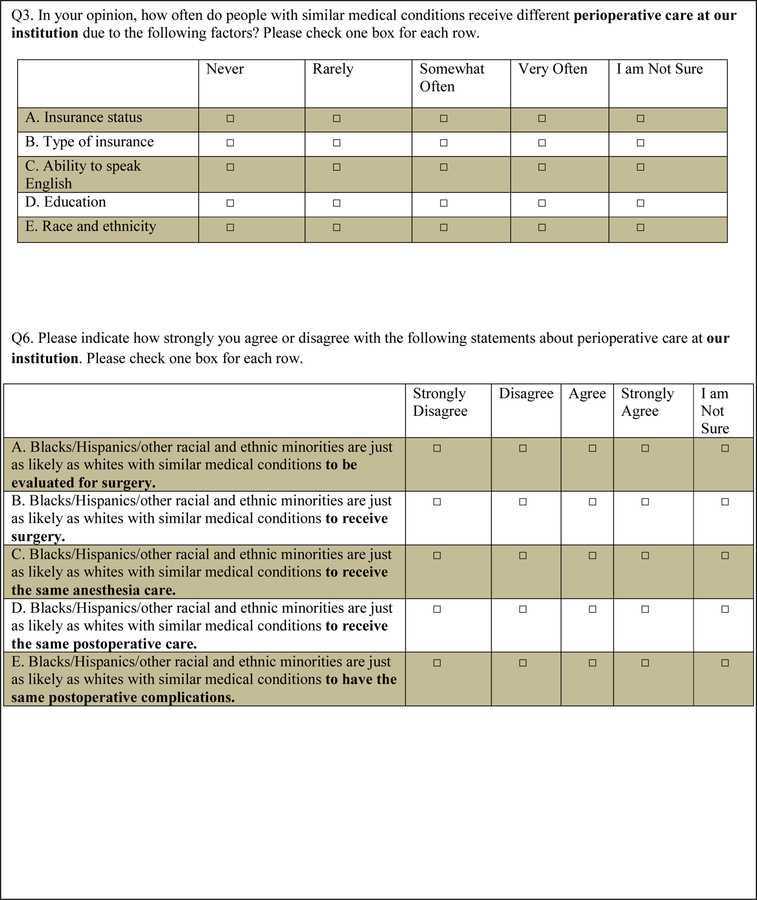
The primary outcomes were measured by two multi-part questions. One question (item 3) asked separately about perceptions of disparities in care for patients based on their type of insurance and their insurance status, ability to speak English, education, and race/ethnicity. The question asked respondents to indicate how often these factors manifested in different perioperative care, with possible answers ranging from ‘never’ (with a value of 1) to ‘often’ (with a value of 4) or ‘I am not sure’ (coded as missing). Another question (item 6) asked whether racial/ethnic minority patients received the same surgical, anesthetic or postoperative care, with possible answers ranging from ‘strongly agree’ (with a value of 1) to ‘strongly disagree’ (with a value of 4) or ‘I am not sure’ (coded as missing).’ See Figure 1 for exact wording of questions.
Figure 1.
Survey questions 3 and 6 (primary outcome). Full survey available in Supplementary Material.
Secondary outcomes were also measured using multi-part questions. One question (item 2) asked respondents to indicate how often they perceived that patients’ type of insurance and insurance status, ability to speak English, education, and race/ethnicity were associated with differences in perioperative care in the United States, with possible answers ranging from ‘never’ (with a value of 1) to ‘often’ (with a value of 4) or ‘I am not sure’ (coded as missing). Another question (item 5) asked whether racial/ethnic minority patients received the same surgical, anesthetic or postoperative care, with possible answers ranging from ‘strongly agree’ (with a value of 1) to ‘strongly disagree’ (with a value of 4) or ‘I am not sure’ (coded as missing).’ See Supplementary Material for exact wording of questions.
A final multi-part question (item 8) interrogated the contribution of systemic factors (access to doctors and hospitals, communication between doctors and patients, and time allotted for nonmedical aspects of care) to racial/ethnic disparities in perioperative care at the institution.
Answers to all questions were analyzed as continuous outcomes, from 1 to 4 with 1 corresponding to low perception of disparities and 4 corresponding to high perception of disparities. This analysis choice was made a priori in order to represent the continuum of answers. Respondents also completed questions about clinical position (the explanatory variable and thus, a mandatory question), personal demographics (age, race, sex, primary language) and work environment (years at institution): these items were used as covariates for adjustment in multivariable analyses.
2.5. Statistical Analysis
All analyses were conducted using SPSS 24 (IBM Corp. Released 2016. IBM SPSS Statistics for Windows, Version 24.0. Armonk, NY: IBM Corp). All hypothesis testing was two-tailed with significance interpreted as p<0.05.
Baseline participant demographics and characteristics were reported as frequency count (%). Chi-squared tests were used to calculate 2-sided p-values for comparisons between physicians and non-physicians in race, sex, age, and years of service at the institution.
The exposure of interest was physician/non-physician status. The primary outcomes of interest were perception of disparities in perioperative care at the institution based on patients’ insurance status/type (1), ability to speak English (2), education (3), and racial/ethnic minority status (4). Disparities in care due to patients’ insurance status/type was measured as a composite mean score of question 3a and 3b: “how often do people with similar medical conditions receive different perioperative care due to insurance status or insurance type?” Likewise, disparities in care due to patients’ ability to speak English was measured from question 3c, “how often do people with similar medical conditions receive different perioperative care due to ability to speak English,” and due to patients’ education was measured from question 3d: “how often do people with similar medical conditions receive different perioperative care due to education?” Finally, disparities in perioperative care due to patients’ race/ethnicity status was measured as a composite score from questions 3e, ‘how often do people with similar medical conditions receive different perioperative care due to race/ethnicity?’ and from 6a, 6b, 6c, 6d, 6e which asked whether racial/ethnic minority patients received the same surgical, anesthetic or postoperative care.
To test which clinical group was more likely to perceive disparities, an independent two-sample t-test was performed. Multivariable linear regression models tested the effects of clinical position on perception scores, adjusting for respondents’ race, sex, age, and years of service at the institution. Assumptions necessary to perform linear regression (including linearity of data, normality of residuals, homoscedasticity and noncollinearity) were verified. In addition, given non-normal distribution of data, results were confirmed with a linear regression model using natural log of the primary endpoints. Covariates were selected a priori. Although no previous literature speaks to how respondents’ race, sex, and age might influence perception, related literature on acknowledgement of disparities suggests that these factors may be influential.14,15 Years of service at the institution was added as a covariate at the suggestion of the Perioperative Services Department staff, given that perception of care at the institution may be influenced by length of affiliation.16
Secondary outcomes of interest were perception of disparities in perioperative care in the United States based on patients’ insurance status/type (1), ability to speak English (2), education (3), and racial/ethnic minority status (4). Disparities in care due to patients’ insurance status/type was measured as a composite mean score of question 2a and 2b: “how often do people with similar medical conditions receive different perioperative care due to insurance status or insurance type?” Likewise, disparities in care due to patients’ ability to speak English was measured from question 2c, “how often do people with similar medical conditions receive different perioperative care due to ability to speak English,” and due to patients’ education was measured from question 2d: “how often do people with similar medical conditions receive different perioperative care due to education?” Finally, disparities in perioperative care due to patients’ race/ethnicity status was measured as the composite score from questions 2e, ‘how often do people with similar medical conditions receive different perioperative care due to race/ethnicity?’ and from 5a, 5b, 5c, 5d, 5e which asked whether racial/ethnic minority patients received the same surgical, anesthetic or postoperative care. As with the primary outcome, we utilized bivariate and then multivariable analysis to test the effects of clinical position on composite scores of disparities in perioperative care.
We then evaluated, in bivariate analysis, the individual effect of respondents’ clinical position, age, race, and primary language on perception of the role of systemic factors on perioperative disparities at the institution. This outcome was measured from all the components of item 8 (a, b, c, d, e, f, g), which asked how much the following factors impacted racial/ethnic disparities in perioperative care at the institution: lower quality of care in minority prevalent settings, availability of doctors and hospitals in general and for surgical care, healthcare provider attitudes and beliefs, miscommunication between provider and patient, lack of time to address psychosocial issues and lack of continuity of care.
Responders were classified as complete if they answered at least one disparity question (either item 2, 3, 5, or 6 in totality) AND the demographic sections; incomplete responders were all other participants. All incomplete responses included clinical position as this question was mandatory for survey submission. Only surveys of complete responders (n=217) were included for bivariate and regression analysis. In post-hoc analysis, completed items from incomplete responders (n=169) were analyzed together with items from complete responders in bivariate analysis. “I’m Not Sure” was treated as a missing variable and was excluded from analysis.
3. RESULTS:
The survey was sent to 1426 members of the perioperative community, 714 non-physicians and 712 physicians. 386 responded (total response rate=25.8%). There were 217 complete responders. 181 staff fully completed items about perception of disparities in perioperative care at our institution due to patients’ insurance status, 202 staff about disparities due to patients’ ability to speak English, 195 staff answered questions about disparities due to patients’ education level, and 210 about disparities due to patients’ racial/ethnic minority status. 162, 176, 174, and 194 staff completed items about perceptions of disparities in perioperative care in the United States based on patients’ insurance status, ability to speak English, education, and race/ethnicity respectively. 206 staff completed item 8 about the contribution of systemic factors to racial/ethnic disparities in perioperative care at our institution.
Among responders, 101 were physicians (46.5%), 165 (76.0%) were White, and 144 (66.4%) were female. 39.2% of complete responders were 40 years old or younger (Table 1). Among non-physicians, 97 (44.7%) were nurses, 12 (5.5%) were certified scrub technologists, 4 (1.8%) were operating room assistants, 2 (0.9%) were patient care assistants, and 1 (0.5%) was an anesthesia technician.
Table 1:
Demographic variables of subjects
| Total | Physician | Non-physician | p-value | |
|---|---|---|---|---|
| Respondent, n (%) | 217 | 101 (46.5) | 116 (53.5) | |
| Female, n (%) | 144 (66.4) | 40 (39.6) | 104 (89.7) | p<0.001 |
| White, n (%) | 165 (76.0) | 67 (66.3) | 98 (84.4) | p=0.002 |
| Age </=40, n (%) | 85 (39.2) | 50 (49.5) | 35 (30.2) | p=0.004 |
| Years at | p=0.199 | |||
| Institution, n (%) | ||||
| 0–5 | 83 (38.2) | 47 (46.5) | 36 (31.0) | |
| 6–10 | 37 (17.1) | 13 (12.9) | 24 (20.7) | |
| 11–15 | 25 (11.5) | 10 (9.9) | 15 (12.9) | |
| 16–25 | 32 (14.7) | 14 (13.9) | 18 (15.5) | |
| >25 | 40 (18.4) | 17 (16.8) | 23 (19.8) |
3.1. Perception of disparities within institution
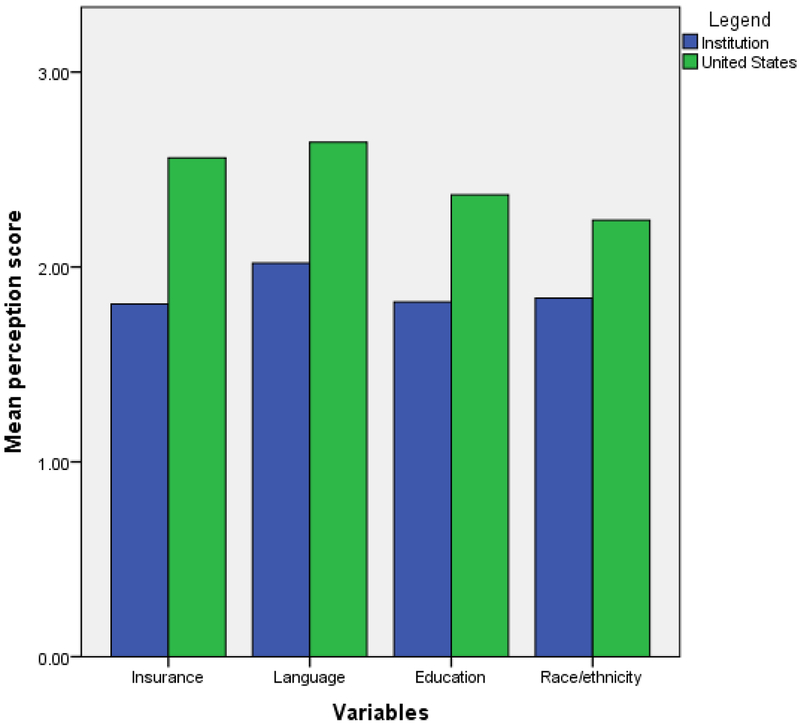
The perception of disparities in perioperative care at the institution was, on average, low based on patients’ insurance status/type (X=1.81; SD= 0.81), ability to speak English (X=2.02; SD: 0.94), education (X=1.82; SD: 0.78), and racial/ethnic minority status (X=1.84; SD: 0.68). See Figure 2.
Figure 2:
Mean perception scores of disparities in perioperative care both at the study institution and in the United States, based on patients’ insurance status/type, ability to speak English, education, and race/ethnicity. Higher numbers indicate higher perceptions of disparities.
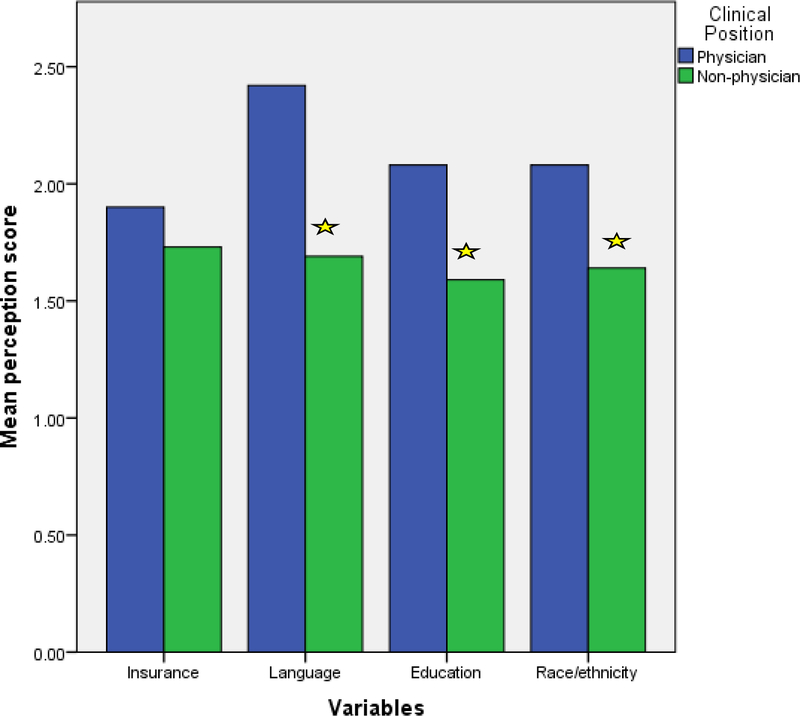
Bivariate analysis revealed that physicians as compared to non-physicians had higher perception of disparities in perioperative care at our institution based on patients’ ability to speak English (mean difference=0.73, p<0.001), education (mean difference=0.49, p<0.001) and race/ethnicity (mean difference=0.43, p<0.001), but not based on insurance status/type (p=0.14). See Figure 3. Similarly, non-White providers and younger staff had higher perceptions of perioperative disparities due to patients’ ability to speak English, education, and race/ethnicity at our institution than White or older staff members. Respondents’ sex was not associated with perception of disparities in any category.
Figure 3.
Bivariate analysis of perceptions of disparities in perioperative care at the study institution based on patients’ insurance status/type, ability to speak English, education, and race/ethnicity among physicians as compared to non-physicians. The star indicates a significant difference in perceptions (p<0.05).
In regression analysis adjusting for respondents’ race, sex, age, and years of service, physician status versus non-physician status was associated with a significant effect on perception of disparities in the institution’s perioperative care based on patients’ ability to speak English (B= 0.95, 95% CI: 0.68–1.22, p<0.001), education (B=0.60, 95% CI: 0.36–0.84, p<0.001) and race/ethnicity (B=0.56, 95% CI: 0.35–0.76, p<0.001), but not based on insurance status/type (p=0.56).
3.2. Perception of disparities in the United States
The average scores for perception of disparities in United States perioperative care based on patients’ insurance status (X=2.56; SD: 1.03), ability to speak English (X= 2.64; SD: 1.00), education (X=2.37; SD: 0.98), and racial/ethnic minority status (X=2.24; SD: 0.77) was representative of ‘agree.’ See Figure 2.
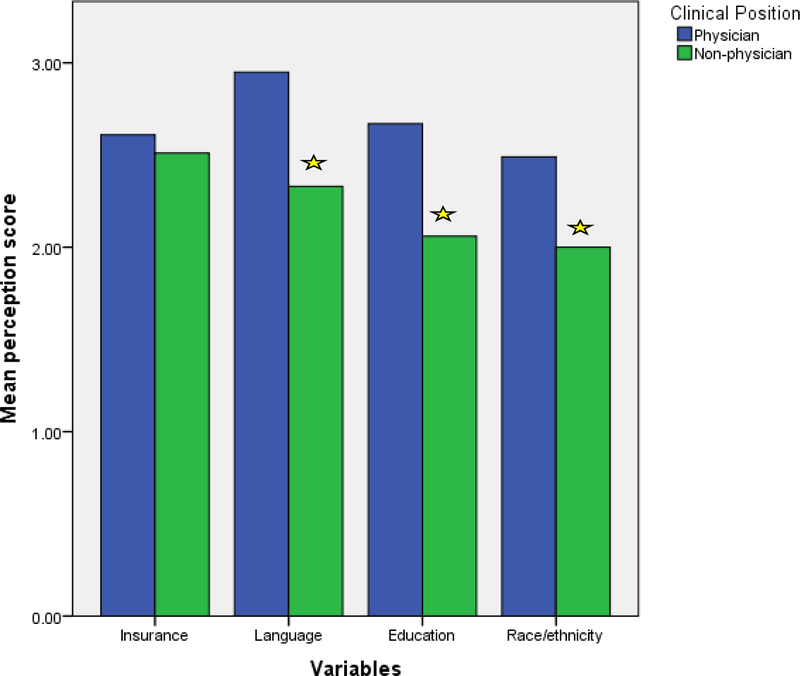
In bivariate analysis, both physicians and non-White staff had significantly higher perception of disparities in United States perioperative care than non-physicians and White staff based on patients’ ability to speak English, education, and race/ethnicity, but not insurance status/type. See Figure 4. There was no significant difference in perception based on respondents’ sex. Younger staff were more likely to perceive disparities based on patients’ ability to speak English, but not their insurance status, education, or race/ethnicity.
Figure 4.
Bivariate analysis of perceptions of disparities in perioperative care in the United States based on patients’ insurance status/type, ability to speak English, education, and race/ethnicity among physicians as compared to non-physicians. The star indicates a significant difference in perceptions (p<0.05).
In regression analysis adjusting for respondents’ race, sex, age, and years of service, physician versus non-physician status remained associated with a significant effect on perception of disparities in perioperative care at the institution based on patients’ ability to speak English (B= 0.89, 95% CI: 0.49–1.13, p<0.001), education (B=0.75, 95% CI: 0.43–1.08; p<0.001) and race/ethnicity (B=0.65 95% CI: 0.41–0.89; p<0.001), but not based on insurance status/type (p=0.43).
3.3. Perception of role of systemic factors in racial/ethnic disparities at our institution
Finally, bivariate analysis revealed that physicians were more likely to believe that racial/ethnic disparities in perioperative care were due to systemic factors as compared to non-physicians. Similarly, younger staff and staff who learned English as a second language had a greater impression about the role of systemic factors in disparities as compared to older staff, or staff who learned English as a first language. Race/ethnicity of respondents, however, was not associated with perception of such factors.
3.4. Incomplete responders
There were 169 incomplete responders. Among these participants, 49 (29%) were physicians, 85 (50.3%) were non-physicians, and 35 (20.7%) did not provide their clinical position. The majority (N=166; 98.2%) did not list their race, their sex (N=163; 96.4%) or their age (N=164; 97%). Among incomplete responders, the percentage of responses to specific questions ranged from approximately 32.5% completing items 2 and 3 to 4.1% completing item 8.
Post-hoc analysis in which the responses of incomplete responders were analyzed with those of complete responders were consistent with the findings of our planned bivariate analyses for the primary and secondary outcomes. Physicians as compared to non-physicians had significantly higher perception of disparities in perioperative care both at our institution and in the United States based on based on patients’ ability to speak English, education, and race/ethnicity.
4. DISCUSSION:
Our study is the first, to our knowledge, to examine perceptions of disparities among perioperative workers rather than awareness or acknowledgement. Given that no data exists characterizing disparities in perioperative care at our institution and minimal data at the national level, we focused on what people believe, not their recognition of existing disparities. Our study also differed in surveying a broad range of health care providers because we believe that patients’ experiences in the perioperative period are defined not only or even primarily by their interactions with a surgeon. Moreover, we were interested in whether clinical position affected perception of disparities because such information may be a starting point for considering how to initiate discussions about disparities among healthcare workers from different professional backgrounds.17 This topic is especially important when interventions to alleviate healthcare disparities focus on providers which include a wide range of staff in the perioperative period.
Our study, examining perioperative staff perceptions of disparities in care, found that the perioperative staff, including physicians and non-physicians, mostly did not perceive disparities in care at our institution, but did perceive them in the United States. Perioperative physicians, as compared to non-physician staff, had stronger impressions of disparities due to patients’ ability to speak English, education, and race/ethnicity, a difference that remained even after adjustments for covariates. Physicians were also more likely to perceive disparities in the United States as compared to non-physicians.
There are a several possible explanations for our findings of overall low perceptions of disparities among perioperative staff workers at our institution. On the one hand, these perceptions may reflect reality: it is possible that few disparities exist in perioperative care due to the institutional culture. On the other hand, low perceptions of disparities may also reflect the nature of work in the operating room. Staff often have limited exposure to an awake patient, patients are unconscious and under surgical drapes for much of the perioperative period, and staff may not be attuned to gauging disparities given the hectic routines of the operating room.
It is interesting to note that perceptions of disparities in care was higher when respondents were asked about the United States than when asked about the institution. This observation resonates with three related studies on surgeons’ awareness (not perceptions) of disparities. When asked about care in their respective specialties nationwide, anywhere from 9% to 36.6% of surgeons endorsed the presence of racial/ethnic disparities nationwide.8,9,10,14 But surgeons’ awareness of disparities in their own hospitals and individual practices was much lower,8,9,10,14 just as perceptions of disparities was much lower in our study when respondents reflected on their own institution and the United States. Our finding, together with those of previous studies, thus suggests that staff in all positions may have differential insights based on their own level of association and involvement with a practice; this may be useful information in institutional efforts aimed at talking about and intervening in disparities. Indeed, literature both in medicine and psychology explores and confirms this ‘bias blind spot.’18,19
Finally, differences in perceptions of disparities among physicians and non-physicians may have several reasons. First, physicians and non-physicians undergo different training, which may lead to heightened sensitivity to issues of health care disparities among physicians, perhaps due to the incorporation of modules on disparities in medical schools and postgraduate programs.20,21 On the other hand, non-physicians are a heterogeneous group whose preparation for their hospital jobs may not include such topics.22 Similarly, non-physicians and physicians perform different tasks and may not be equal witnesses to disparate care. Indeed, most non-physicians meet patients for a truncated portion of the perioperative period (such as, in the pre-operative holding room or in the operating room) whereas many physicians see them throughout their visit (from pre-operative holding room to operating room to post-operative recovery room). A third possible explanation for our findings is that perception of disparities may be linked to a greater number of years of education for physicians compared to some non-physician staff. Previous studies have found that more years of education are associated with greater awareness of health disparities,23 although these studies have not focused on differences within healthcare professions. Regardless, perceptions of disparities at our institution were low among both groups, highlighting that years of education is not necessarily associated with a high perception of disparities in the perioperative setting.
Our study had several limitations. First, we had a low response rate, potentially due to the sensitive nature of the topic, the email format, fear of identification, and the busy lives of those who work in the operating room.10 Indeed, the fact that questions 5 and 6 were skipped more frequently than questions 2 and 3 may indicate that some respondents did not have had the time to complete the survey. However, very few incomplete responders answered demographic questions, suggesting fear of identification or discomfort with the sensitive topic of disparities. Although the response rate is on par with at least one other survey study of healthcare workers on disparities,10 it may have led to nonresponse bias. We have minimal information on non-responders and incomplete responders because we elected to maintain anonymity to encourage honest responses. Yet our planned and post-hoc bivariate analyses did not result in different findings. It may be important to conduct qualitative work to solidify explanations for our results. Replicating our study in other institutions would also be informative of the generalizability of our findings.
A second limitation of our study is that it did not distinguish between physician or non-physician specialties. The training and mindset of anesthesiologists differ from that of general surgeons and both from that of orthopedic surgeons; likewise, the training and mindset of nurses in the pre-operative holding room may differ from that of certified surgical technologists. Another area for investigation might be to assess the perceptions among these individual groups. Finally, our results may not be generalizable, given that this study was conducted at a single tertiary care center.
The finding that non-physicians are less likely to perceive disparities in perioperative care for minority patients than physicians may help guide institutional efforts such as standardized trainings for all staff about disparities in perioperative care (including what they are and how they might manifest in everyday practice) and incorporation of interventions to increase equity in care into staff development meetings. Future research on disparities in perioperative care may also benefit from direct observation of staff’s behavior to match perceptions with reality. This study constitutes a first and much-needed step at examining disparities in care in perioperative settings.
Supplementary Material
ACKNOWLEDGEMENTS:
The authors gratefully acknowledge: Timothy Houle, PhD, Associate Professor, Department of Anesthesia, Critical Care, and Pain Medicine, Massachusetts General Hospital, Boston MA, USA; Hang Lee, PhD, Associate Professor of Medicine, Harvard Medical School, MGH Biostatistics Center
Funding:
The first author’s work on this study was supported by the National Institutes of Health T32 GM007592 (Research Training for Anesthetists).
Funding sources: Dr. Rosenbloom’s work on this research was supported by the National Institutes of Health T32 GM007592 (Research Training for Anesthetists; PI Miller).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declarations of interest: none
The authors have no conflicts of interest to declare.
REFERENCES:
- 1.Zhang W, Lyman S, Boutin-Foster C, et al. Racial and ethnic disparities in utilization rate, hospital volume, and perioperative outcomes after total knee arthroplasty. J Bone Jt Surg 2016;98:1243–1252. [DOI] [PubMed] [Google Scholar]
- 2.Wilson CT, Fisher E, Welch HG. Racial disparities in abdominal aortic aneurysm repair among male medicare beneficiaries. Arch Surg 2008;143:506–510. [DOI] [PubMed] [Google Scholar]
- 3.Silber JH, Rosenbaum PR, Ross RN, et al. Racial disparities in operative procedure time: the influence of obesity. Anesthesiology 2013;119:43–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sukumar S, Ravi P, Sood A et al. Racial disparities in operative outcomes after major cancer surgery in the United States. World J. Surg 2015; 39:634–643. [DOI] [PubMed] [Google Scholar]
- 5.Ravi P, Sood A, Schmid M, et al. Racial/ethnic disparities in perioperative outcomes of major procedures: Results from the national surgical quality improvement program. Ann Surg 2015;262:955–964. [DOI] [PubMed] [Google Scholar]
- 6.Torain MJ, Maragh-Bass AC, Dankwa-Mullen I, et al. Surgical disparities: A comprehensive review and new conceptual framework. J Am Coll Surg 2016;223:408–418. [DOI] [PubMed] [Google Scholar]
- 7.Lutfi W, Zenati MS, Zureikat AH, et al. Health disparities impact expected treatment of pancreatic ductal adenocarcinoma nationally. Ann Surg Oncol 2018;25:1860–1867. [DOI] [PubMed] [Google Scholar]
- 8.Britton BV, Nagarajan N, Zogg CK, et al. US surgeons’ perceptions of racial/ethnic disparities in health care: A cross-sectional study. JAMA Surg. 2016;151:2016–2018. [DOI] [PubMed] [Google Scholar]
- 9.Taylor SL, Fremont A, Jain AK, et al. Racial and ethnic disparities in care: The perspectives of cardiovascular surgeons. Ann Thorac Surg. 2006;81:531–536. [DOI] [PubMed] [Google Scholar]
- 10.Adelani MA, O’Connor MI. Perspectives of orthopedic surgeons on racial/ethnic disparities in care. J Racial Ethn Heal Disparities. 2017;4:758–762. [DOI] [PubMed] [Google Scholar]
- 11.Memtsoudis SG, Besculides MC, Swamidoss CP. Do race, gender, and source of payment impact on anesthetic technique for inguinal hernia repair? J Clin Anesth. 2006;18:328–333. [DOI] [PubMed] [Google Scholar]
- 12.Memtsoudis SG, Poeran J, Zubizarreta N et al. Anesthetic care for orthopedic patients: Is there a potential for differences in care? Anesthesiology 2016;124:608–623. [DOI] [PubMed] [Google Scholar]
- 13.Gordon S What we call healthcare professionals matters. The BMJ Opinion. https://blogs.bmj.com/bmj/2016/05/25/suzanne-gordon-what-we-call-healthcare-professionals-matters/; May 25 2019 Accessed February 28 2019.
- 14.Britton BV, Nagarajan N, Zogg CK, et al. Awareness of racial/ethnic disparities in surgical outcomes and care: Factors affecting acknowledgment and action. Am J Surg 2016;212:102–108.e2. [DOI] [PubMed] [Google Scholar]
- 15.Lurie N, Fremont A, Jain AK, et al. Racial and ethnic disparities in care: The perspectives of cardiologists. Circulation 2005;111:1264–1269. [DOI] [PubMed] [Google Scholar]
- 16.Ydav RP. Is job hopping a good practice? Entrepreneur. https://www.entrepreneur.com/article/322390; October 26 2018 Accessed February 28 2019.
- 17.Chin MH, Walters AE, Cook SC, Huang ES. Interventions to reduce racial and ethnic disparities in health care. Med Care Res Rev 2007;64:7S–28S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pronin E, Kugler MB. Valuing thoughts, ignoring behavior: The introspection illusion as a source of the bias blind spot. J Exp Soc Psychol 2007;43:565–578. [Google Scholar]
- 19.Sabin J, Nosek BA, Greenwald A, Rivara FP. Physicians’ implicit and explicit attitudes about race by MD race, ethnicity, and gender. J Health Care Poor Underserved 2009;20:896–913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vela MB, Kim KE, Tang H, et al. Innovative health care disparities curriculum for incoming medical students. J Gen Intern Med. 2008;23:1028–1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Office for Civil Rights. Medical school curriculum initiative. https://www.hhs.gov/civil-rights/for-individuals/special-topics/health-disparities/medical-school-curriculum-initiative/index.html; July 22 2014 Accessed June 4 2018.
- 22.Johns Hopkins Medicine Health Library. ‘Surgical team,’ The Johns Hopkins University, the Johns Hopkins Hospital, and the Johns Hopkins Health System Corportation. https://www.hopkinsmedicine.org/healthlibrary/conditions/surgical_care/surgical_team_85,P01413; Accessed February 28 2019.
- 23.Booske BC, Robert SA, Rohan AMK. Awareness of racial and socioeconomic health disparities in the United States: the national opinion survey on health and health disparities, 2008–2009. Prev Chronic Dis. 2011;8:A73,1–9. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.