Abstract
Background:
African American smokers suffer disproportionately from tobacco-related disease caused, in part, by lower rates of smoking cessation. We examined whether smoke-free home policies and delay discounting were differentially associated with cigarettes smoked per day (CPD) and nicotine dependence (ND) among African Americans and Whites.
Methods:
Secondary data analysis was conducted using data from 65 African American (n = 40) and White (n = 25) smokers who completed measures of CPD, ND, tobacco craving, stress, depression, home smoking policy, and delay discounting.
Results:
A significant interaction was found between race and home smoking policy on CPD (B= −11.21, p = .002) and ND (B = −3.42, p = .004). Smoke-free policies in the home were associated with fewer CPD and lower ND levels among Whites, but not among African Americans. Whites who allowed smoking in their homes had significantly greater mean CPD and higher mean ND than their counterparts who did not allow smoking in the home. Among African American smokers, there were no differences in CPD and ND among those who allowed smoking in their home versus those who did not. Conclusions: The findings extend the scientific literature by suggesting that a malleable environmental factor (home smoking policy) commonly associated with cessation among Whites does not have the same influence on cessation among African American.
Keywords: cigarette smoking, health disparities, home smoking policy, delay discounting
Smoking policies in the home have less influence on cigarettes per day and nicotine dependence level among African American than White smokers
Despite recent successes in tobacco control, cigarette smoking remains one of the most significant causes of premature death and disability in the United States.1,2 Although the prevalence of cigarette smoking is similar among African American and White adults and African Americans generally smoke fewer cigarettes than Whites, African Americans shoulder a disproportionate burden of the negative health consequences from smoking, including higher morbidity and mortality from nearly all tobacco-related cancers.3 Among African American men, smoking accounts for 20% of the excess risk in all-cause mortality above age 50.4 The increased burden of tobacco-related disease is caused, in part, by African Americans being significantly less likely to achieve long-term abstinence from smoking than Whites despite a higher proportion of African Americans reporting that they desire to quit and have tried to quit in the past year, contributing to already significant tobacco-related racial disparities.5–7 More detailed investigations are needed to understand how individual characteristics and environmental factors influence cessation among African Americans. Reducing tobacco-related racial health disparities is crucial to achieving racial health equity and reducing the cancer burden in the US.8
Smoking-related differences between African Americans and Whites are associated with a wide variety of individual characteristics and environmental factors including: socioeconomic status;9 tobacco advertising saturation;10 targeted tobacco industry marketing,11 cigarette prices,12,13 smoke-free home and work policies;14 impulsivity/delay discounting15 and discrimination.16 However, few studies examine the influences of multiple individual and environmental factors simultaneously.
Smoke-free policies in the home
Home smoking restrictions reduce cigarette consumption and nicotine dependence by limiting opportunities to smoke, disrupting habitual patterns, reducing nicotine intake, and/or increasing social pressure to quit. Smoke-free home policies are strongly associated with fewer cigarettes per day (CPD), more quit attempts, and more robust intentions to quit.17,18 Widespread implementation of smoke-free home policies is considered a highly effective population-based tobacco control strategy resulting in less exposure to combustible tobacco and positive effects on cessation as well as support for potentially reducing tobacco-related racial, ethnic, and socioeconomic disparities;5 however, smoke-free home policies might not work equally well for all populations.5,19 African Americans are less likely to be exposed to smoke-free home policies than Whites suggesting differential access across racial groups to a generally effective smoking cessation approach.5,20 Conceivably, there are factors influencing the implementation or effectiveness of this approach among African Americans.21 For example, African Americans may be less likely to voluntarily implement home smoking bans compared to Whites due to differences in housing quality or location (e.g., living in an impoverished urban neighborhood may make smoking outdoors more difficult) or greater exposure to neighborhoods with more pro-smoking norms.22,23 According to diminished returns theory,24,25 given African Americans have to contend with additional stressors such as structural racism, discrimination, and disproportionate societal barriers, they have to utilize more cognitive resources managing these deleterious experiences on a daily basis, which may make it harder for them to utilize the existing health-related resources and policies available to them (such as home smoking bans). Moreover, even when African Americans and Whites equally implement health related resources, there may also be differential gains in the benefits from those resources. Indeed, studies suggest the benefits of health or social resources are typically larger for those who are already advantaged (e.g., Whites), furthering racial health disparities.25–27
Nevertheless, it remains unclear whether racial differences in home smoking policies per se contribute to racial differences in consumption and nicotine dependence. If indeed this is case, then home smoking policies might become a productive target for intervention among African American homes.
Delay discounting
Delay discounting rate, the degree to which one de-values rewards as a function of time to their receipt, has robust generality and predictive validity for smoking28,29 Higher discounting rates are associated with less robust intentions to quit,30 higher nicotine dependence levels,31 and greater risk for relapse.32 African Americans demonstrate higher delay discounting rates than Whites in some studies.15 Cultural differences in decision making and racial differences in exposure to unpredictable and adverse events might adaptively contribute to differences in the value placed on immediate over delayed rewards,33 but no studies to date have prospectively examined racial differences in delay discounting rates and the extent to which these potential differences contribute to cigarette consumption and nicotine dependence.
The aim of this study was to examine racial differences in individual characteristics and environmental factors associated with CPD and nicotine dependence level in a sample of African American and White smokers enrolled in a parent study. All participants lived in New York City, a city known for robust tobacco control regulations. We focused on two factors likely to differentially affect cigarette use and nicotine dependence in African Americans: home smoking policy and delay discounting rates. We probed disparities between races in exposure to home smoking policies. We then used multiple regression models to examine the effects of delay discounting, smoking policies in the home, and race on the number of CPD and nicotine dependence levels. We hypothesized that less restrictive home smoking policies and higher delay discounting rates would be associated with a greater number of CPD and higher nicotine dependence levels, similar to other populations.
Method
Participants
This is a secondary analysis of cross-sectional data collected from participants enrolled in a study on racial differences in psychophysiological factors associated with cigarette smoking. Participants were recruited from January 2015 to October 2016 in the Harlem neighborhood and surrounding communities in NYC by placing flyers in the community and advertisements on craigslist and in local newspapers. The inclusion criteria were as follows: 1) self-identified as African-American or White; 2) physically healthy; 3) normal or corrected normal visual acuity; 4) 18 years or older; 5) fluent in English; 6) able to provide informed consent; and 7) smoking 5 or more CPD for at least 1 year. The exclusion criteria were as follows: 1) past or current DSMIV-TR psychotic-, mood-, or anxiety-disorders; 2) current DSM-IV-TR substance abuse or dependence (past abuse/dependence prior to 12 months before the study was permissible); 3) current hazardous alcohol use (for women: more than 7 drinks per week; for men: more than 14 drinks per week); 4) inability to pass a urine drug screen for substances of abuse; 5) diagnosed neurological syndrome (e.g., seizure disorders, brain trauma/tumor disorders); 6) poor vision acuity; 7) risk for suicide based on current mental state or history; 8) refusal to be audio-taped; 9) active use of medications for tobacco cessation and recent attempt to quit cigarette smoking (past 30 days); and 10) self-reported history of Attention-Deficit/Hyperactivity Disorder.
Procedures
This research was approved by the City University of New York institutional review board (IRB) and all procedures followed were in accordance with the ethical standards of the IRB and the Helsinki Declaration of 1975, as revised in 2008. Five hundred and fifty-one individuals contacted the study to express interest in participating. Individuals who met preliminary screening criteria over the telephone (n = 148) were invited for an in-person screening interview. Sixty-six individuals attended the in-person screen and were found to be eligible for participation. After written informed consent was collected for eligible participants, baseline assessment measures were administered, and participants were scheduled for the experimental session. Only the baseline measures were utilized for these analyses. Participants received $75 compensation for participation in the study.
Measures
Standard demographic data was collected (e.g., age, gender, race, educational level, employment status, household income, marital status). Clinical information collected included age of onset of regular cigarette use, number of years of regular smoking, average number of CPD; home smoking policy (i.e., whether they were allowed to smoke anywhere in their homes, yes/no); the Tobacco Craving Questionnaire-Short Form (TCQ-SF),34 the Perceived Stress Scale-4 (PSS-4),35 the Center for Epidemiological Studies Depression Scale – Revised (CESDR);36 the Barratt Impulsiveness Scale-11 (BIS-11);37 and the Fagerstrom Test for Nicotine Dependence (FTND),38 a 6-item measure used to assesses nicotine dependence. The FTND has adequate internal consistency, test-retest reliability, and convergent validity.39 A separate binary variable was created called time to first cigarette (TTFC), which consisted of the first item on the FTND recoded into two categories: smokes within 30 minutes of waking up (yes/no).
Delay discounting was assessed via a computerized task that assessed participants’ preferences for larger later versus smaller sooner rewards.40 In each trial, participants chose between an immediate, smaller (e.g., $500 now) and a later, larger amount of money (e.g., $1,000 later). Subsequent trials adjusted amounts depending on participants’ prior responses according to a decreasing-adjustment algorithm. The outcome was expressed as the natural logarithm of k in Mazur’s (1987) hyperbolic discounting model with k increasing as the preference for smaller sooner rewards increases.41
Statistical Analyses
Descriptive statistics were used to characterize participants (e.g., mean, standard deviation, frequency, etc.). Racial differences were examined with Chi-Square and t-tests. Pearson correlations were used to assess bivariate relations between all continuous variables within race.
Multiple regression models were developed with CPD and nicotine dependence (i.e., FTND score) as dependent variables. The main effects of race, home smoking policy, delay discounting, and interactions among race and home smoking policy and race and delay discounting were examined. An analysis of standardized residuals was carried out to identify outliers. Multicollinearity was assessed by reviewing tolerance and variance inflation statistics. The Durban Watson test was used to examine independence of errors. Histograms, p-plots, and scatterplots of standardized residuals were reviewed to determine whether errors were normally distributed, and the assumptions of homogeneity of variance and linearity were met. Cases with missing data were excluded listwise. We used an alpha level of .05 for all statistical tests.
Results
Participants (n= 65) included African American (n = 40) and White (n = 25) cigarette smokers. One participant was excluded from the analyses because she was an extreme outlier on the CPD variable. Participants were predominantly male (71%), middle-aged (45 years, SD = 9.62) smokers with low education levels and low incomes. The mean age of initiation of regular smoking was 19.54 (SD = 5.77); the mean years of smoking regularly was 21.34 (SD = 11.35); and the mean number of CPD was 12.43 (SD = 5.38). Participants were moderately dependent with a mean FTND score of 4.03 (SD = 2.3). See Table 1.
Table1.
Descriptive Comparisons by Race
| African- | Whites | ||
|---|---|---|---|
| Total | Americans | (n = 25) | |
| (n = 65) | (n = 40) | ||
| Mean (SD) or % | |||
| Male | 70.8% (n=46) | 65% (n=26) | 80% (n=20) |
| Age (years) | 44.95 (9.62) | 45.03 (9.45) | 44.84 (1.59) |
| Education (years)+ | 14.02 (1.90) | 13.69 (1.59) | 14.64 (2.19) |
| Education (categories) | |||
| Less than H.S. | 3.1 (n=2) | 2.5 (n=l) | 4.0 (n=l) |
| H.S. | 26.2 (n=17) | 32.5 (n=13) | 16.0 (n=4) |
| Some College | 41.5 (n=27) | 45.0 (n=18) | 36.0 (n=9) |
| College Graduate | 21.5 (n=14) | 17.5 (n=7) | 28 (n=7) |
| Some Graduate School | 7.7 (n=5) | 2.5 (n=l) | 16 (n=4) |
| Annual Income+ | |||
| <= $24,999 | 38.5% (n=35) | 40% (n=16) | 36% (n=9) |
| $25,000 – $49,000 | 29.2% (n=19) | 37.5% (n=15) | 16% (n=4) |
| $50,000+ | 32.3% (n=21) | 22.5% (n =9) | 48% (n=12) |
| Marital Status | |||
| Never Married | 49.2% (n=32) | 52.5% (n=21) | 44.0% (n=11) |
| Married | 18.5% (n=12) | 17.5% (n=7) | 12.0% (n=5) |
| Separated/Divorced/Widowed | 32.3% (n=21) | 30.0% (n=12) | 36.0% (n=9) |
| Age Started Smoking Regularly* | 19.54 (5.77) | 21.0 (6.45) | 17.2 (3.45) |
| Years Smoked Regularly+ | 21.34(11.35) | 19.38 (10.60) | 24.48 (12.01) |
| Mean CPD | 12.43 (5.38) | 11.78 (5.07) | 13.48 (5.80) |
| Menthol Cigarette Use (%Yes)* | 75.4% (n=49) | 87.5% (n=35) | 56% (n=14) |
| Smokeless Tobacco (%No) | 96.9% (n=63) | 97.5% (n=39) | 96% (n=24) |
| FTND-Total | 4.03 (2.300 | 4.22 (2.07) | 3.72 (2.65) |
| TTFC | |||
| < 5 mins (%yes) | 24.6% (n= 16) | 25% (n=10) | 24% (n=6) |
| < 30 mins (%yes)+ | 66.2% (n=43) | 75% (n=30) | 52% (n=13) |
| Allowed to Smoke in Home* | |||
| (%Yes) | 46.2% (n=30) | 57.5% (n=23) | 28% (n=7) |
| BIS-II Subscales | |||
| BIS-II Attentional | 13.92 (3.25) | 13.95 (3.27) | 13.88 (3.27) |
| BIS-II Motor+ | 20.25 (4.22) | 19.45 (4.42) | 21.52 (3.62) |
| BIS-II Nonplanning | 23.97 (4.77) | 24.25 (4.49) | 23.52 (5.25) |
| Delay Discounting* | −1.33 (.99) | −1.10 (1.02) | −1.69 (.85) |
| TCQ-SF Subscales | |||
| Emotionality | 9.74 (5.29) | 9.77 (5.32) | 9.68 (5.34) |
| Expectancy | 15.2 (4.86) | 15.03 (4.56) | 15.48 (5.40) |
| Compulsivity | 8.74 (4.85) | 8.40 (4.73) | 9.28 (5.09) |
| Purposefulness | 11.84 (4.84) | 11.75 (4.73) | 11.92 (5.11) |
| CESD-R | 11.60 (7.08) | 11.43 (6.37) | 11.88 (8.22) |
| PSS-4 | 7.32 (2.87) | 7.05 (3.35) | 7.76 (1.88) |
Note. HS = High School; CPD = Cigarettes Per Day; FTND = Fagerstrom Test for Nicotine Dependence (range 0–10); TTFC – Time to the first cigarette of the day, recoded from 4 categories to 2 categories; BIS-11 – Barratt Impulsiveness Scale 11 (subscale scores range from 8 to 44); TCQ-SF = Tobacco Craving Questionnaire-Short Form (subscale scores range from 3 to 21); CESD-R = Center for Epidemiological Studies Depression Scale -Revised (range 0–60-; Scores below 16 are not considered clinically significant); PSS-4 = Perceived Stress Scale – 4 items (range 0–16). Bootstrapping with 1,000 samples.
p < .05;
p<.10
There were no significant demographic differences between African American and White smokers. African Americans initiated regular smoking at an older age than Whites (M = 21.0, (SD = 6.45) vs M = 17.2, (SD = 3.45), t(63) = 3.09, p = .003, d = .73) and were more likely to smoke menthol cigarettes than Whites (X2 (1, N = 65) = 8.23, p = .004, r = .36). A greater proportion of African Americans had no smoke-free home policy (i.e., allowed smoking anywhere in their homes) than Whites (57.5% vs. 28%, X2 (1, N = 65) = 5.39, p=.02, r = .29). African Americans demonstrated higher delay discounting rates than Whites (M = −1.10; SD =1.02 versus M = −1.70; SD = 0.85), t(63) = 2.41, p = .019, d = .64). No differences between African Americans and Whites were found among the other measures. Bivariate correlations revealed that for African Americans, CPD was positively associated with the TCQ-SF compulsivity subscale (r (40) = .33, p<.05), stress level (r (40) = .50, p<.01), and distress/depression symptoms (r (40) = .44, p<.01). African Americans’ FTND scores were positively associated with three of the four TCQ-SF subscale scores: emotionality (r (40) = .43, p<.01), compulsivity (r (40) = .39, p<.05), and purposefulness (r (40) = .39, p<.05). The correlation between CPD and FTND was not significant for African Americans (r (40) = .21, p>.05). For Whites, CPD demonstrated positive associations with FTND (r (25) = .75, p<.01), the TCQ-SF compulsivity score (r (25) = .51, p<.05), the BIS-11 attentional subscale scores (r (25) = .40, p<.05), and a negative association with age started smoking regularly (r (25) = −.47, p<.05). FTND scores demonstrated positive associations with all four TCQ-SF subscale scores: emotionality (r (25) = .69, p<.01), expectancy (r (25) = .57, p<.01), compulsivity (r (25) = .55, p<.01), and purposefulness (r (25) = .59, p<.01). The correlations between CPD, FTND and perceived stress and depression scores were not significant among Whites.
Regression Analyses
Cigarettes Per Day:
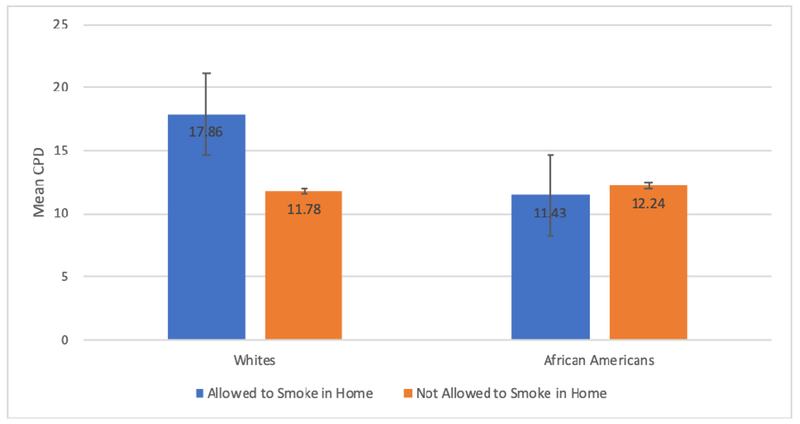
The model predicting CPD was significant (F(5,34) = 5.47, p = .007, R2 = .24), indicating that variables of race, smoking policy in the home, delayed discounting, the interaction between race and home smoking policy, and the interaction between race and delay discounting explained 24% of the variance in CPD. With other factors in the model accounted for, a significant main effect was found for home smoking policy (B = 10.33, SE = 2.79, t = 3.70, p<.01), where smoke-free policies were associated with smoking fewer CPD. A significant interaction was found between race and home smoking policy (B= −11.21, SE = 3.49, t = −3.21, p = .002). Smoke-free policies were associated with fewer CPD among Whites, but not among African Americans. See Table 2 and Figure 1.
Table 2.
Regression Model Predicting Cigarettes Per Day (n = 65)
| Variable | B | SE B | β |
|---|---|---|---|
| Constant | 12.41 | 3.08 | |
| Race: African Americans (vs Whites) | .62 | 2.31 | .04 |
| Allowed to Smoke in Home (Yes vs No) | 10.33 | 2.79 | .72* |
| Delay Discounting | .37 | 1.57 | .05 |
| Race x Allowed to Smoke in Home | −11.21 | 3.49 | −.74* |
| Race x Delay Discounting | −1.48 | 1.88 | −.16 |
| R2 = .24 | |||
| F = 5.47* |
p < .05
Figure 1.
Mean cigarettes per day (CPD) by race and home smoking policy. Error bars represent standard error.
Nicotine Dependence:
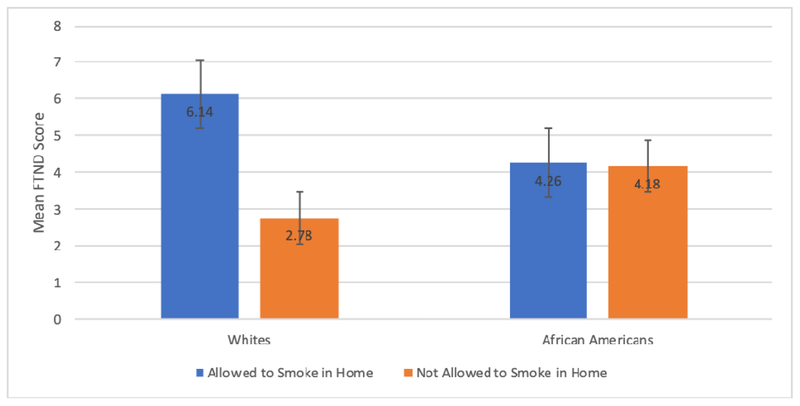
The model predicting nicotine dependence was significant (F(2, 60) = 4.80, p = .01, R2 = .22), indicating the variables race, smoking policy in the home, delayed discounting, the interaction between race and home smoking policy, and the interaction between race and delay discounting explained 22% of the variance in level of nicotine dependence. With other factors in the model accounted for, significant main effects were found for race (B = 1.63, SE = 0.75, t = 2.17, p = .034) and home smoking policy (B = 3.50, SE = .91, t = 3.85, p <.01). African Americans had significantly higher levels of nicotine dependence than Whites. Smoke-free home policies were associated with lower levels of nicotine dependence. A significant interaction was found between race and smoking policy in the home ((B = −3.42, SE = 1.14, t = −3.01, p = .004). Smoke-free home policies were associated with lower nicotine dependence among Whites, but not among African Americans. See Table 3 and Figure 2.
Table 3.
Model Predicting Level of Nicotine Dependence (n = 65)
| Variable | B | SE B | β |
|---|---|---|---|
| Constant | 1.82 | 1.00 | |
| Race: African Americans (vs Whites) | 1.63 | 0.75 | 0.35* |
| Allowed to Smoke in Home (Yes vs No) | 3.50 | 0.91 | 0.76*** |
| Delay Discounting | −0.57 | 0.51 | −0.24 |
| Race x Allowed to Smoke in Home | −3.42 | 1.14 | −0.71** |
| Race x Delay Discounting | 0.46 | 0.61 | 0.16 |
| R2 = .22 | |||
| F = 4.80* |
p < .05,
p<.01,
p<.001
Figure 2.
Mean Fagerstrom Test for Nicotine Dependence (FTND) total score by race and home smoking policy. Error bars represent standard errors.
Discussion
These findings add to our understanding of tobacco-related influences that have a disparate impact on African Americans. Widespread implementation of smoke-free home policies is considered a highly effective population-based tobacco control strategy resulting in less exposure to combustible tobacco and positive effects on cessation; however, in this sample, smoke-free home policies had a disparate impact on African American smokers. Unlike White smokers, African American smokers with smoke-free home policies did not smoke fewer CPD and did not show lower nicotine dependence levels. African Americans do not appear to benefit equally from smoke-free home policies. These findings suggest that this malleable environmental factor commonly associated with cessation among Whites does not have the same influence on cessation among African Americans and that tobacco control messages that focus on the development of smoke-free home policies might contribute to a growing list of tobacco control interventions and policies that add to the already significant tobacco-related racial disparities.5,16,17,19
The racial inequalities associated with smoke-free policies appear to be similar to the racial inequalities found in cigarette pricing. Cigarette tax increases are responsible for large increases in cigarette pricing with the overall effect of reducing cigarette consumption;42 however, the magnitude of the effect is greater for Whites than African Americans.12 Moreover, cigarette pricing is positively associated with quit attempts for Whites, but not for African Americans.13 Similar to smoke-free policies, tobacco tax policies are universalized interventions that appear to be amplifying the advantages of being White and adding to cumulative differences that widen preexisting tobacco-related disparities. [See Ceci et al. 2005 for discussion of unequal gains from universalized interventions in education.]26 Clearly, more research is needed to understand why African Americans do not benefit equally from some tobacco control policies and to develop tobacco control policies and interventions that have a pro-equity impact on African Americans.
Consistent with recent studies,18 we found a larger percentage of African Americans in this study allowed cigarette smoking anywhere in their homes compared to Whites and this has an impact on the consequent health effects of exposure to second hand smoke among smokers and non-smokers alike. Lower rates of home smoking restrictions may be partly due to lower rates of cigarette consumption among African Americans. Family members and smokers may be more tolerant of smoking fewer cigarettes in the home and thus may be less likely to insist on a smoke-free policy (cf., Gilpin et al.).17 Fewer smoke-free home policies among African Americans might also be due to different levels of socioeconomic status, which might create additional barriers to adoption; however, we found no differences in income or education between African Americans and Whites in this sample. Nonetheless, our African American participants might be less likely to voluntarily implement smoke-free home policies due to differences in housing quality or location (e.g., living in an impoverished urban neighborhood may make smoking outdoors more difficult) or greater exposure to neighborhoods with more pro-smoking norms.22,23
Our analyses also showed positive correlations among stress and depression levels and CPD among African American smokers. The combination of stress and psychological distress may contribute to smoking in the home as a strategy for managing negative feelings.43 Delay discounting did not have the expected relationship with CPD and nicotine dependence level either as a main effect or in an interaction with race. Although the main effect of delay discounting was not significant in the regression models, univariate analyses (Table 1) revealed that African American participants were more likely to choose smaller, more immediate rewards over larger rewards later, compared to White participants. This is consistent with a study of problem gamblers33 and in a large online sample of non-smokers and smokers.15 Racial differences in delay discounting have been attributed to cultural differences in decision-making or in exposure to unpredictable, adverse events contributing to an adaptive weighting of more immediate positive rewards over delayed future rewards. More research is needed to understand racial differences in delay discounting among smokers and what role, if any, delay discounting might have in contributing to tobacco-related racial disparities.
Consistent with the extant literature, African Americans were more likely to smoke menthol cigarettes, started smoking regularly at an older age, and smoked for fewer years than Whites. Menthol cigarette use has been associated with difficulties with quit attempts and smoking cessation, particularly among African Americans.44,45 The cooling, stimulating, and anesthetic effects of menthol may enhance the pleasure of smoking cigarettes, contribute to deeper inhalations and in turn promote greater nicotine intake, furthering the addiction process and contributing to lower likelihood of quitting and, in turn, enhanced risk of negative health effects.46
Our findings also revealed that the well-established measure of nicotine dependence, the FTND, was not associated with the same factors among African Americans and Whites. For instance, the FTND was not significantly associated with CPD among African Americans, but was highly associated with CPD among Whites. CPD is an item on the FTND and has a large impact on the overall FTND score. These findings are consistent with previous studies that have found the FTND to correlate with biochemical measures of nicotine consumption among Whites, but not African Americans. Nicotine dependence, as measured by the FTND, among African Americans appears to be more associated with the value and timing of cigarettes earlier in the day, and difficulty refraining from smoking in certain places and times.47 The limitations of this study include a small sample size, which may have limited our power to detect differences and associations. Findings may not be generalizable beyond urban, non-treatment seeking, smokers in NYC, and we also did not assess for other forms of tobacco consumption (e.g., little cigars, cigarillos, or cigars). Strengths include a comprehensive examination of individual characteristics and environmental factors among African American and White tobacco smokers, including factors that are novel in the extant literature.
Acknowledgments
Financial Support: This work was supported by the National Cancer Institute [Grant number 1P20CA192993 and 1P20CA192991].
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest: The authors declare that no conflicts of interest exist.
Research Involving Human Participants: Our research was approved by the City University of New York institutional review board and all procedures followed were in accordance with the ethical standards of the IRB and the Helsinki Declaration of 1975, as revised in 2008.
Informed Consent: Informed consent was obtained from all participants included in the study.
Ethical Standards: The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Contributor Information
Lesia M. Ruglass, Department of Psychology, The City College of New York, CUNY
James C. Root, Department of Psychiatry and Behavioral Sciences, Memorial Sloan Kettering Cancer Center
Naomi Dambreville, Department of Psychology, The City College of New York and The Graduate Center, CUNY
Alina Shevorykin, Department of Psychology and Mental Health Counseling, Pace University
Noshin Haque, Department of Psychiatry and Behavioral Sciences, Memorial Sloan Kettering Cancer Center
Vicki Sun, Sophie Davis School of Biomedical Education, CUNY School of Medicine
Christine E. Sheffer, Department of Health Behavior, Roswell Park Cancer Institute
Robert D. Melara, Department of Psychology, The City College of New York, CUNY
References
- 1.Warren GW, Alberg AJ, Kraft AS, Cummings KM. The 2014 Surgeon General’s report:“The Health Consequences of Smoking–50 Years of Progress”: A paradigm shift in cancer care. Cancer. 2014;120(13):1914–1916. doi: 10.1002/cncr.28695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lortet-Tieulent J, Sauer AG, Siegel RL, et al. State-level cancer mortality attributable to cigarette smoking in the United States. JAMA Intern Med. 2016;176(12):1792–1798. [DOI] [PubMed] [Google Scholar]
- 3.Jamal A, Phillips E, Gentzke AS, et al. Current Cigarette Smoking Among Adults—United States, 2016. Morb Mortal Wkly Rep. 2018;67(2):53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ho JY, Elo IT. The contribution of smoking to black-white differences in US mortality. Demography. 2013;50(2):545–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hill S, Amos A, Clifford D, Platt S. Impact of tobacco control interventions on socioeconomic inequalities in smoking: Review of the evidence. Tob Control. 2014;23(e2):e89–e97. [DOI] [PubMed] [Google Scholar]
- 6.Babb S, Malarcher A, Schauer G, Asman K, Ahmed J. Quitting smoking among adults—United States, 2000–2015. MMWR Morb Mortal Wkly Rep. 2017;65(52):1457–1464. [DOI] [PubMed] [Google Scholar]
- 7.U.S. Department of Health and Human Services (HHS). Tobacco Use Among U.S. Racial/Ethnic Minority Groups—African Americans, American Indians and Alaska Natives, Asian Americans and Pacific Islanders, and Hispanics: A Report of the Surgeon General. Atlanta, GA; 1998. [PubMed] [Google Scholar]
- 8.Fagan P, King G, Lawrence D, et al. Eliminating tobacco-related health disparities: Directions for future research. Am J Public Health. 2004;94(2):211–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ward E, Jemal A, Cokkinides V, et al. Cancer disparities by race/ethnicity and socioeconomic status. CA Cancer J Clin. 2004;54(2):78–93. [DOI] [PubMed] [Google Scholar]
- 10.Primack BA, Bost JE, Land SR, Fine MJ. Volume of tobacco advertising in African American markets: Systematic review and meta-analysis. Public Health Rep. 2007;122(5):607–615. doi: 10.1177/003335490712200508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yerger VB, Przewoznik J, Malone RE. Racialized geography, corporate activity, and health disparities: Tobacco industry targeting of inner cities. J Health Care Poor Underserved. 2007;18(6):10–38. [DOI] [PubMed] [Google Scholar]
- 12.Yao T, Ong MK, Max W, et al. Responsiveness to cigarette prices by different racial/ethnic groups of US adults. Tob Control. 2018;27(3):301–309. [DOI] [PubMed] [Google Scholar]
- 13.Keeler C, Max W, Yerger VB, et al. Effects of cigarette prices on intention to quit, quit attempts, and successful cessation among African American smokers. 2018. [DOI] [PubMed] [Google Scholar]
- 14.Shavers VL, Fagan P, Alexander LAJ, Clayton R, Doucet J, Baezconde-Garbanati L. Workplace and home smoking restrictions and racial/ethnic variation in the prevalence and intensity of current cigarette smoking among women by poverty status, TUS-CPS 1998–1999 and 2001–2002. J Epidemiol Community Heal. 2006;60(suppl 2):ii34–ii43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sheffer CE, Mackillop J, Fernandez A, et al. Initial examination of priming tasks to decrease delay discounting. Behav Processes. 2016;128:144–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alcalá HE, Sharif MZ, Morey BN. Misplaced trust: Racial differences in use of tobacco products and trust in sources of tobacco health information. Nicotine Tob Res. 2017:ntx080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gilpin EA, White MM, Farkas AJ, Pierce JP. Home smoking restrictions: Which smokers have them and how they are associated with smoking behavior. Nicotine Tob Res. 1999;1(2):153–162. [DOI] [PubMed] [Google Scholar]
- 18.Mills AL, White MM, Pierce JP, Messer K. Home smoking bans among US households with children and smokers: Opportunities for intervention. Am J Prev Med. 2011;41(6):559–565. [DOI] [PubMed] [Google Scholar]
- 19.Lorenc T, Petticrew M, Welch V, Tugwell P. What types of interventions generate inequalities? Evidence from systematic reviews. J Epidemiol Community Heal. 2013;67(2):190–193. [DOI] [PubMed] [Google Scholar]
- 20.Niederdeppe J, Fiore MC, Baker TB, Smith SS. Smoking-cessation media campaigns and their effectiveness among socioeconomically advantaged and disadvantaged populations. Am J Public Health. 2008;98(5):916–924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Trinidad DR, Pérez-Stable EJ, White MM, Emery SL, Messer K. A nationwide analysis of US racial/ethnic disparities in smoking behaviors, smoking cessation, and cessation-related factors. Am J Public Health. 2011;101(4):699–706. doi: 10.2105/AJPH.2010.191668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Latkin CA, Tseng T-Y, Davey-Rothwell M, et al. The Relationship between Neighborhood Disorder, Social Networks, and Indoor Cigarette Smoking among Impoverished Inner-City Residents. J Urban Heal. 2017;94(4):534–541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rees VW, Keske RR, Blaine K, et al. Factors influencing adoption of and adherence to indoor smoking bans among health disparity communities. Am J Public Health. 2014;104(10):1928–1934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Assari S, Mistry R. Educational Attainment and smoking status in a national sample of american adults; evidence for the blacks’ diminished return. Int J Environ Res Public Health. 2018;15(4 (763)):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Assari S Health disparities due to diminished return among black Americans: Public policy solutions. Soc Issues Policy Rev. 2018;12(1):112–145. [Google Scholar]
- 26.Ceci SJ, Papierno PB. The rhetoric and reality of gap closing: when the” have-nots” gain but the” haves” gain even more. Am Psychol. 2005;60(2):149. [DOI] [PubMed] [Google Scholar]
- 27.Assari S Unequal gain of equal resources across racial groups. Int J Heal policy Manag. 2018;7(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Baker F, Johnson MW, Bickel WK. Delay discounting in current and never-before cigarette smokers: Similarities and differences across commodity, sign, and magnitude. J Abnorm Psychol. 2003;112(3):382–392. [DOI] [PubMed] [Google Scholar]
- 29.Odum AL. Delay discounting: I’m ak, you’re ak. J Exp Anal Behav. 2011;96(3):427–439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Athamneh LN, Stein JS, Bickel WK. Will delay discounting predict intention to quit smoking? Exp Clin Psychopharmacol. 2017;25(4):273–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sweitzer MM, Donny EC, Dierker LC, Flory JD, Manuck SB. Delay discounting and smoking: Association with the Fagerström Test for Nicotine Dependence but not cigarettes smoked per day. Nicotine Tob Res. 2008;10(10):1571–1575. [DOI] [PubMed] [Google Scholar]
- 32.Sheffer CE, Christensen DR, Landes R, Carter LP, Jackson L, Bickel WK. Delay discounting rates: A strong prognostic indicator of smoking relapse. Addict Behav. 2014;39(11):1682–1689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Andrade LF, Petry NM. White problem gamblers discount delayed rewards less steeply than their African American and Hispanic counterparts. Psychol Addict Behav. 2014;28(2):599–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Heishman SJ, Singleton EG, Pickworth WB. Reliability and validity of a Short Form of the Tobacco Craving Questionnaire. Nicotine Tob Res. 2008;10(4):643–651. doi: 10.1080/14622200801908174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- 36.Eaton WW, Smith C, Ybarra M, Muntaner C, Tien A. Center for Epidemiologic Studies Depression Scale: A review and revision (CESD and CESD-R) In: Maruish ME, ed. The Use of Psychological Testing for Treatment Planning and Outcomes Assessment: Volume 3: Instruments for Adults. New York, NY: Routledge; 2004:363–377. [Google Scholar]
- 37.Patton JH, Stanford MS. Factor structure of the Barratt impulsiveness scale. J Clin Psychol. 1995;51(6):768–774. [DOI] [PubMed] [Google Scholar]
- 38.Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom K. The Fagerström test for nicotine dependence: A revision of the Fagerstrom tolerance questionnaire. Br J Addict. 1991;86(9):1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x [DOI] [PubMed] [Google Scholar]
- 39.Meneses-Gaya IC de Zuardi AW, Loureiro SR, Crippa JA de S. Psychometric properties of the Fagerström test for nicotine dependence. J Bras Pneumol. 2009;35(1):73–82. [DOI] [PubMed] [Google Scholar]
- 40.Koffarnus MN, Bickel WK. A 5-trial adjusting delay discounting task: Accurate discount rates in less than one minute. Exp Clin Psychopharmacol. 2014;22(3):222–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mazur JE. An adjusting procedure for studying delayed reinforcement In: Commons ML, Mazur JE, Nevin JA, Rachlin H, eds. Qantitative Analysis of Behavior (Volume 5). Hillsdale, NJ: Erlbaum; 1987:55–73. [Google Scholar]
- 42.Chaloupka FJ, Straif K, Leon ME. Effectiveness of tax and price policies in tobacco control. Tob Control. 2011;20(3):235–238. [DOI] [PubMed] [Google Scholar]
- 43.Leventhal AM. The sociopharmacology of tobacco addiction: Implications for understanding health disparities. Nicotine Tob Res. 2015;18(2):110–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Okuyemi KS, Faseru B, Sanderson Cox L, Bronars CA, Ahluwalia JS. Relationship between menthol cigarettes and smoking cessation among African American light smokers. Addiction. 2007;102(12):1979–1986. [DOI] [PubMed] [Google Scholar]
- 45.Stahre M, Okuyemi KS, Joseph AM, Fu SS. Racial/ethnic differences in menthol cigarette smoking, population quit ratios and utilization of evidence-based tobacco cessation treatments. Addiction. 2010;105(SUPPL.1):75–83. doi: 10.1111/j.1360-0443.2010.03200.x [DOI] [PubMed] [Google Scholar]
- 46.Kulak JA, Cornelius ME, Fong GT, Giovino GA. Differences in quit attempts and cigarette smoking abstinence between Whites and African Americans in the United States: Literature review and results from the International Tobacco Control US Survey. Nicotine Tob Res. 2016;18(suppl_1):S79–S87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schroeder JR, Moolchan ET. Ethnic differences among adolescents seeking smoking cessation treatment: A structural analysis of responses on the Fagerstrom Test for Nicotine Dependence. Nicotine Tob Res. 2007;9(1):137–145. [DOI] [PubMed] [Google Scholar]