Abstract
Rationale
This study evaluates the process and preliminary outcomes of Promoting Community Conversations About Research to End Suicide (PC CARES), an intervention that brings key stakeholders together so they can discuss suicide prevention research and find ways to put it into practice. Originally piloted in remote and rural Alaskan communities, the approach shows promise.
Method
Using a multi-method design, the study describes a series of locally-facilitated “learning circles” over 15 months and their preliminary results. Sign-in sheets documented participation. Transcriptions of audio-recorded sessions captured facilitator fidelity, accuracy, and the dominant themes of community discussions. Linked participant surveys (n=83) compared attendees’ perceived knowledge, skills, attitudes, and their ‘community of practice’ at baseline and follow-up. A cross-sectional design compared 112 participants’ with 335 non-participants’ scores on knowledge and prevention behaviors, and considered the social impact with social network analyses.
Results
Demonstrating feasibility in small rural communities, local PC CARES facilitators hosted 59 two to three hour learning circles with 535 participants (376 unique). Local facilitators achieved acceptable fidelity to the model (80%), and interpreted the research accurately 81% of the time. Discussions reflected participants’ understanding of the research content and its use in their lives. Participants showed positive changes in perceived knowledge, skills, and attitudes and strengthened their ‘community of practice’ from baseline to follow-up. Social network analyses indicate PC CARES had social impact, sustaining and enhancing prevention activities of non-participants who were ‘close to’ participants. These close associates were more likely take preventive actions than other non-participants after the intervention.
Conclusion
PC CARES offers a practical, scalable method for community-based translation of research evidence into selfdetermined, culturally-responsive suicide prevention practice.
Keywords: Suicide Prevention, Community Education, Alaska Native, Train-the-Trainer, Community Mobilization, Upstream Prevention, Community of Practice
1. Introduction
The issue of Indigenous youth suicide has been difficult to address in ways that are both scientifically-grounded and culturally-responsive (Rhoades, 2003; Goldston et al., 2008; Alaska Bureau of Vital Statistics, 2016; Mullany et al., 2009; Gone and Trimble, 2012; Gracey and King, 2009). For Indigenous youth in rural Alaska, suicide is a particularly significant problem. While among the general population, suicide rates tend to increase with age, in arctic Indigenous populations, the peak rates occur at ages 15 through 24 (Bjerregaard et al., 2004), with Inuit and Alaska Native (AN) young people in rural and remote communities having suicide rates almost 20 times higher than their North American counterparts (Lehti et al., 2009; Williams and Kulig, 2012; Berman, 2014)
The complex drivers of the problem are linked to the rapid social, economic, and political changes imposed on remote arctic Indigenous communities over the last 50–100 years (Willmon-Haque and BigFoot, 2008; Peters et al., 2014). Forced settlement and mandatory schooling, including residential schools, changed family structures, and young people’s experiences of growing up change people in significant ways (Kraus, 1974; Kraus and Buffler, 1979). These forms of colonization and intergenerational trauma can create conditions that increase suicide risk and can reduce people’s access to shared protective factors and processes (Gone and Alcántara, 2010). Considering this, suicide prevention must prioritize cultural and local knowledge, respond to local sensibilities and conditions, while also utilizing scientific prevention research to effectively address the issue. Reliance on mental health services for suicide prevention in rural AN communities is not adequate. In the participating region, 79% of suicide decedents and 62% of attempters received no mental health care (Wexler, 2006). The majority of AN youth refuse or never engage in mental health care, even when showing signs of anxiety, anger, depression, other mental distress (LeMaster et al., 2004; Beals et al., 2005; Oetzel et al., 2006), or when actively suicidal (Wexler et al., 2012; Freedenthal and Stiffman, 2007). One reason for this lack of mental health care, which is typically offered by non-Native providers, is often called only as a last resort (Wexler and Gone, 2012). From 1990 to 2009, 75% of the 510 suicide calls to mental health clinicians in the study region were deemed ‘imminent risk’. Late intervention makes service options extremely limited, often resulting in involuntary 48-h commitments 50 to 500 air miles away from home communities. This experience can mirror the historical traumas experienced by AN families whose children were involuntarily sent to residential schools as recently as the 1970s (Hirshberg, 2008). Indigenous youth across the U.S. underutilize mental health services due to stigma, distrust, and the cultural differences between them and providers, often seeking this help only when suicide risk is high (Duclos et al., Beals et al., 2005; Oetzel et al., 2006).
Often, a variety of people are in contact with vulnerable persons, but do not recognize suicide risk or know how to intervene early to prevent a crisis. In Northwest Alaska, people in informal support systems (family and friends) noticed something was wrong in 62% of all cases of suicidal behavior. Other recorded signs of suicide vulnerability include alcohol misuse (55% of all cases), school problems (51%), relationship conflicts (35%, plus another 12% involving intimate partner violence), and alcohol-related healthcare (31%) (Wexler et al., 2017). Of note, 40% of those who died by suicide in Northwest Alaska were seen in a health clinic for an alcohol-related injury in the 12 months prior to their death (Hill et al., 2007). Key stakeholders (e.g., educators, healthcare providers, family) must recognize these issues as possible warning signs for suicide, and have more tools to respond before a suicide crisis.
It is important to find ‘upstream’ and culturally relevant ways to reduce suicide risk to improve population health. ‘Upstream’ means primary and secondary prevention interventions that begin when someone shows signs of being at heightened risk for suicide, but before s/he becomes a lethal threat to him/herself. At this juncture, a variety of community-based prevention practices can reduce suicide risk if only family, community members, and workers knew how best to do so. Prevention strategies range from environmental (e.g., reduction of lethal means) to interpersonal (e.g., supportive conversations), and can be done by people in the daily lives of a young person when s/he shows vulnerability. This kind of informal safety net is especially important in remote AN communities, where there is limited behavioral health care infrastructure and few itinerant mental health care providers. Building on local infrastructure and expertise, our intervention—Promoting Community Conversations About Research to End Suicide (PC CARES)—provides a model for stakeholders to develop evidence-informed, coordinated, self-determined early responses to prevent suicide.
1.1. The PC CARES model
Grounded in adult learning theory, popular education strategies (Wexler et al., 2015; Wexler et al., 2016), and local and Indigenous protocols, PC CARES is a community learning-model developed in collaboration with Indigenous leaders and educational experts. The model gives local people information based on scientific research that they can use to prevent suicide. Building the capacity of local community members and local service providers (e.g., healthcare, education, etc.), PC CARES brings together multiple sectors within the community to engage in learning circles, which offer them a variety of ideas about effective prevention strategies to spark conversation, adaptation, and collaborative action. In a series of sessions, these stakeholders discuss scientific ‘best practices’, how they might apply it (or not) to their jobs and/or lives, and develop ideas for taking preventive actions in their jobs and homes. Hosted by local trained facilitators, learning circles can be tailored for each community and cultural context. The model is flexible, but basically follows the same structure each time.
The curriculum itself—what specific ‘best practices’ or scientific insights are shared —is developed in collaboration with community leaders. The kinds of research selected in this pilot study reflect local interest in balancing both risk and protective factors, sharing local research findings, and offering insights across multiple levels of prevention. In this pilot, the content of the nine sessions include (for more details, see pc-cares.org):
Historical Trauma and Suicide (King et al., 2009; Gracey and King, 2009).
The Role of Adults in Youth Suicide Prevention (Wexler, 2006)
Seasonality of Suicidal Behavior (Silveira et al., 2016)
Community Protective Factors (Berman, 2014; Chandler and Lalonde, 1998, 2004).
Importance of Listening Well (Barnett et al., 2018a,b; Barnett et al., 2018).
Reducing Lethal Means (Beautrais et al., 2005; Kim, 2018; Mann et al., 2005; Van Der Feltz-cornelis et al., 2011; Yip et al., 2012)
Support after an Attempt (Luoma et al., 2002, Motto and Bostrom, 2001).
Postvention as Prevention (Crepeau-Hobson, Leech, 2014, Wilson and Marshall, 2010; Cox et al., 2012; Goodwin-Smith et al., 2013).
PC CARES Review and Moving Forwarded.
Other sources describe the theoretical foundations of PC CARES (Wexler et al., 2016) or focus on the learning and behavioral outcomes of the 40-h facilitation training that prepares local people to host learning circles in their own communities (Wexler et al., 2017). The social network analysis article describes the methods used to measure social impact (Lee et al., 2018b) and further information about the PC CARES intervention and behavior change techniques is available online.
This paper reports the comprehensive process and preliminary outcomes of the pilot study. In the model, trained local PC CARES facilitators host monthly learning circles. Different kinds of research spark conversations among stakeholders so they can consider how (or if) that information fits their own understandings, context, and communities. Sessions then explore how participants, as individuals or as members of a group (e.g., family, clinic, school), can use the information for wellness and prevention. Participants explore possibilities and decide how they want to use the information. The model, in short, asks local facilitators to share “what we know” (10 min or less, bite-sized pieces of research evidence). Then participants spend the majority of time discussing its local and personal relevance, and exploring how they can apply the information to their lives, jobs, and communities. In this way, PC CARES positions scientific information as a catalyst to spark self-determined actions (Wexler et al., 2016).
2. Method
2.1. Objective
The objective of the study was to assess the process and preliminary learning and behavioral outcomes of a pilot intervention designed to strengthen local decision-making, relationships, and preventive actions to reduce suicide risk.
2.2. Study design
A mixed-method design was used to study the process and preliminary outcomes of PC CARES.
2.3. Measures
Process indicators document participation, fidelity to the structure of the model, and the accuracy of research interpretations occurring in a series of nine learning circles. Our process measures include analysis of discussions taking place in the community learning circles. Outcome indicators include self-reported learning outcomes over time: perceived knowledge, perceived skills, attitudes toward prevention, and sense of community of practice; and, self-reported behavioral outcomes of participants before and after they attend one or more learning circles. Lastly, social impact was measured by examining the self-reported prevention behavior of non-participants who are ‘close to’ PC CARES participants and those who are not.
2.4. Procedures
Facilitators in each village administered learning outcome surveys (LOS) to all participants before learning circle 1, and to any new participants attending subsequent learning circles. Participants completed the LOS with pen and paper, and the facilitator mailed them to the research team for analysis. Follow-up LOS and Suicide Prevention Behavior Surveys were administered electronically on computer tablets by research staff approximately three months after PC CARES learning circles ended in each village (12–16 months after the baseline survey). In addition, facilitators audio-recorded learning circles, which were transcribed for analysis.
2.5. Process indicators
Participation
Eligible participants were community residents or service providers, age 15 or older. Local facilitators tracked participation using attendance sheets and demographic surveys with age, gender, race, employment, and previous suicide prevention education. Facilitators mailed demographic surveys and attendance sheets to the research team, who calculated the number and percentage of participants in each demographic category, number of villages that participated in each learning circle, and total number of participants.
Transcripts of community learning circles
To better understand what happened in each village learning circle, facilitators asked permission to audio-record sessions. If everyone agreed, the facilitator audio-recorded the session, and sent the recording on a thumb drive to the researchers. Transcripts of these sessions helped us assess the accuracy of the information discussed and fidelity to which the facilitator carried out the curriculum (i.e., followed the learning circle process).
Curriculum fidelity and accuracy of research interpretation
Two independent raters used a Fidelity Tracking Sheet [see Appendix A] to code transcripts and assess whether facilitators followed the format in the Facilitator’s Guide and interpreted research information accurately. They used a three-point Information Accuracy Scale to rate both the accuracy of facilitators’ description of the research evidence, and participants’ understanding of the information. A score of one indicated that research was interpreted accurately, leading to the intended conclusions; a score of two indicated that research was interpreted accurately, but the conversation focused primarily on issues of wellness or suicide prevention not directly related to the research presented; and a score of three indicated that research evidence was interpreted inaccurately, leading to conclusions and conversations inconsistent with its intent. To calculate overall accuracy, the twos and threes were converted to zeros, and a 0/1 scale was used to calculate the percentage of learning circle accuracy.
Two independent raters also assessed fidelity to the PC CARES curriculum across several standard elements for each learning circle: agreements/safe talk, reflections, the sections: what we know, what we think, and what we want to do. Each element scored 0–1 for procedural components (i.e., presenting data, giving clear instructions) that are present (1), absent (0), or not captured (NA) on the recording when the audio missed some of the session. Scores across learning circles were averaged across the two raters.
2.6. Outcome indicators
Learning outcomes
Participants’ learning outcomes were documented through surveys done at baseline and three months after the intervention (approximately 15 months after the first learning circle in each community). Non-PC CARES participants answered the same survey questions at the follow-up time point. Baseline surveys were administered to participants with pen and paper at the first Learning Circle each participant attended. Follow-up surveys were administered to participants (and one-time surveys for non-participants) electronically three months after the last learning circle that was done in a community. The learning outcome questions fit into four specific constructs: the perceived skills subscale consisted of four items (Cronbach’s α=.72), the attitudes toward prevention subscale consisted of five items (α=0.63), the perceived knowledge subscale consisted of five items (α=0.75) and the community of practice subscale consisted of five items (α=0.72). (See Appendix B for all items).
Suicide prevention behaviors outcomes
At the follow-up time point, three months after the intervention concluded, 39-item suicide prevention behavior surveys were given to both former PC CARES participants (n=112) and non-participants (n=335). Survey respondents were recruited from the eight villages with the highest participation, and Respondent Driven Sampling (Lee et al., 2018a,b) was used in five of these villages to recruit non-participants. After completing a survey, individuals were given up to three “coupons,” to share with people close to them. The number of coupons given was determined by the village size and level of participation, and each coupon was worth five dollars if the person they gave it to also completed a survey. Data collection using Respondent Driven Sampling continued for two to three days. In total, 447 individuals completed the Suicide Prevention Behavior Surveys (see Appendix C).
The Suicide Prevention Behavior Survey asked respondents for demographic information, to identify which community members (from a provided list of PC CARES participants) they were ‘close to,’ binary (yes/no) questions about respondent behaviors related to suicide prevention, and whether they currently do those actions more, less, or the same as they used to. For example, the survey asked if respondents have “had conversations about making it harder for an ‘at risk’ person to get a loaded gun,” and “suggested ways community organizations could work together to increase wellness”. Each item fell under one of 13 categories. Eight of the categories relate directly to the content of the first eight learning circles. The remaining five categories addressed content across multiple learning circles: wellness promotion, primary prevention, secondary prevention, support within family, and open communication. There were three items for each category.
Social impact
The same dataset generated from the Suicide Prevention Behavior Survey was used to conduct social network analysis to understand the social effects of the intervention (Lee et al., 2018a,b) by considering the responses of non-participants who were ‘close to’ PC CARES participants and others who were not.
2.7. Analysis strategies
2.7.1. Process indicators
Discussion themes
Transcripts from the learning circles were thematically coded to categorize the kinds of discussions sparked by similar content across communities. Coding identified pre-conceived themes related to sections “what do we know”, “what do we think”, and “what do we want to do”, as well as open-ended codes to capture the main points of discussion. Community members from the participating communities helped determine these themes.
2.7.2. Outcome indicators
Learning outcomes
Construct scores were calculated as the average score of the items within the construct. To compare construct scores, authors calculated means, 95% confidence intervals, statistical significance, and effect sizes (Cohen’s d). The mean construct scores were: (1) the pre-survey scores of participants to the same participants’ follow-up scores using paired t-tests; (2) the pre-survey scores of PC CARES participants compared to non-participants using two-sample t-tests; and (3) follow-up scores of participants compared to non-participants using two sample t-tests. With Cohen’s d, effect sizes of 0.2 indicate a small effect size, 0.5 indicate medium effect size, and 0.8 indicate a large effect size (Zaiontz, 2015) (Table 2). In addition, a oneway analysis of variance with Bonferroni pairwise comparisons was used to compare follow-up scores for each construct across respondents who received four different dosages of the intervention. This compared scores for (1) trained facilitators, (2) participants in two or more learning circles, (3) participants in only one learning circle, and (4) non-participants.
Table 2.
a. Comparison of Learning Outcome Constructs for Participants (Pre) and Participants (Follow up)
| Construct | Mean for Participants (Pre) (n = 83) | SE (Pre) | Mean for Participants (EU) (n = 83) | SE (FU) | Difference (Participants (FL) m in u; Participants (Pre)) | SE (Difference) | 95% CI for Difference | Standardized Effect Size (Cohen’s d) |
| Perceived Skill*** | 3.64 | 0.088 | 4.04 | 0.074 | 0.40 | 0.093 | .219, .588 | 0.485 |
| Attitude toward Prevention | 3.84 | 0.065 | 3.91 | 0.066 | 0.07 | 0.064 | −.055, .201 | 0.120 |
| Perceived Knowledge*** | 3.27 | 0.085 | 3.84 | 0.074 | 0.57 | 0.094 | .385, .758 | 0.668 |
| Community of Practice** | 3.52 | 0.089 | 3.90 | 0.085 | 0.38 | 0.094 | .192, .567 | 0.443 |
| Construct | Mean for Participants (Pre) (n = 83) | SE (Pre) | Mean of Non Participants (n = 335) | SE (Non-participants) | Difference (Participants (Pre) minus Non Participants) | SE (Difference) | 95% CI for Difference | Standardized Effect Size (Cohen’s d) |
| Perceived Skill** | 3.64 | 0.088 | 3.90 | 0.034 | −0.26 | 0.081 | −.418, −.099 | 0.389 |
| Attitude toward Prevention* | 3.84 | 0.065 | 3.67 | 0.030 | 0.17 | 0.069 | .028, .301 | 0.283 |
| Perceived Knowledge*** | 3.27 | 0.085 | 3.62 | 0.034 | −0.35 | 0.080 | −.515, −.200 | 0.525 |
| Community of Practice** | 3.52 | 0.089 | 3.75 | 0.038 | −0.23 | 0.088 | −408. −.064 | 0.320 |
| Construct | Mean for Participants (FU) (n = 83) | SE (FU) | Mean of Non participants (n = 335) | SE (Non participants) | Difference (Participants (FU) minus Non- Participants) | SE (Difference) | 95% CI for Difference | Standardized Effect Size (Cohen’s d) |
| Perceived Skill | 4.04 | 0.074 | 3.90 | 0.034 | 0.14 | 0.077 | −.008, .297 | 0.237 |
| Attitude toward Prevention*** | 3.91 | 0.066 | 3.67 | 0.030 | 0.24 | 0070 | .101, .374 | 0.404 |
| Perceived Knowledge** | 3.84 | 0.074 | 3.62 | 0.034 | 0.22 | 0.077 | .061, .366 | 0.346 |
| Community of Practice | 3.90 | 0.085 | 3.75 | 0.038 | 0.15 | 0.087 | −.026, .314 | 0.212 |
Note:
indicates p < 0.05
indicates p < 0.01
indicates p < 0.001.
CI - Confidence Interval. FU - Follow Up. SE - Standard Error. Cohen’s d 0.2 = small effect size, 0.5 = medium effect size, 0.8 = large effect size (Zaiontz, 2015).
Behavioral outcomes
Outcomes were compared between participant (n=112) and non-participant (n=335) behaviors over the course of the three months since the end of the PC CARES intervention. With three prevention actions that could be taken within each category, responses were dichotomized into (1) those who did twi or more actions within the category and (2) those who did fewer than two actions in the category. Percentages of each group (participants and non-participants) who performed two or more actions per category were calculated using a chi-squared test with Cramer’s V (φ) used to indicate effect size. With Cramer’s V, effect sizes of 0.1 indicate a low effect size, 0.3 indicate a medium effect size, and 0.5 indicate a large effect size (Zaiontz, 2012).
Social impact
In the participating tight-knit communities, PC CARES participants are likely to influence non-participants’ who are ‘close to’ them by sharing their understandings and tools for suicide prevention (i.e., “social diffusion”) or support for prevention (i.e., “social reinforcement”). The social network methods used in this study measure these diffusion and group-dynamic outcomes to better understand the impact of PC CARES within the participating community context (Gest et al., 2011; Palinkas et al., 2013; Buchanan et al., 2007; Valente, TW et al., 2015; Christakis and Fowler, 2013).
The inclusion of relational data in the evaluation of PC CARES—through the identification and interviewing of people with ‘close’ (named) or ‘community’ (reached by coupon-based referrals) ties to PC CARES participants—allowed for the measurement of social network effects that may have influenced the spread of PC CARES social impact through network diffusion, social reinforcement, and other social dynamics.
Attending one learning circle is a small dose and not likely to have significant social impact; for this analysis, only facilitators and those who attended at least two learning circles were counted as participants. Relational data was rendered as sets of two-person dyads that could take one of four forms: dyads where both ego (person answering the survey) and alter (person with whom the ego is close) participated in PC CARES, ego participated and alter did not, alter participated and ego did not, or neither party participated. Comparisons across these four dyad classes allowed assessment of the role that social influence and diffusion of information to others in the community might play in individual outcomes (Lee et al., 2018a,b). Both the “treatment effects” of the intervention (where the intervention showed efficacy in creating positive behavior change) and “sustaining prevention effects” (where the intervention showed efficacy in maintaining an existing behavior across time despite potential behavior change) were tested. Eight different tests were used to assess the social network impacts on the overall efficacy of the intervention. The eight tests (as named in Appendix D) measure whether social factors such as friendship, kinship, or other social ties impacted the way that the intervention promoted positive change or sustained protective behaviors among PC CARES participants and people close to them (whether or not those close to the participants also attended the intervention themselves) (Lee et al., 2018a,b). This analysis method evaluates statistical significance, but does not produce effect sizes.
3. Results
3.1. Sample
Participants completed 193 pre-intervention learning outcome surveys and 112 follow up surveys with 83 having completed both. 57% of participants were lost to follow-up. Additionally, 335 non-participants and the same 112 participants completed LOS and the follow-up Suicide Behavior Prevention Surveys.
3.2. Participation
Ten villages, ranging in size from 100 to 3000 residents, held 59 PC CARES learning circles with 535 attendees over the 15-month pilot. Of these, 376 were unique participants (some of whom participated in more than one learning circle). Attendance averaged 7.73 participants per session, ranging from one to 50. Most PC CARES participants were female (64%) and 54% who answered were AN, 140 did not mark their ethnicity. It is likely that many of these unknowns are AN, with more than 80% of the population being Inupiaq. Participants’ ages were 3% teens, 13% young adults, 27% adults, 16% elders, and 41% unknown. About one-third of PC CARES participants were employed as service providers: school staff, family workers, law enforcement, and mental health workers.
Participation over the course of the learning circles decreased, with 163 people attending the first learning circle, and only 27 people attending the ninth one. Most people only attended one learning circle, with few people participating in four or more. In a region of 12 villages, facilitators from 11 different communities were trained and these local facilitators hosted at least one learning circle in 10 communities, and hosted five or more learning circles five communities (see Table 1, Table S2: Supplemental). According to local facilitators, job or location changes of facilitators, more pressing community concerns (i.e., fish runs, funerals, hunting opportunities), and misunderstandings about the on-going structure of the model contributed to declining participation over time.
Table 1.
Data collection instruments and respondents.
| Data Collection Instruments | PC CARES Trained Facilitators | PC CARES participants who attended 2 + LCs | PC CARES participants who attended 1 LC only | Non-PC CARES participants | Total |
|---|---|---|---|---|---|
| Learning Outcome Surveys (Pre) | 32 | 56 | 105 | NA | 193 |
| Learning Outcome Surveys (Follow Up) | 8 | 50 | 54 | 335 | 447 |
| Matched Surveys (Pre & Follow Up) | 7 | 35 | 41 | NA | 83 |
| Suicide Behavior Prevention Surveys | 8 | 50 | 54 | 335 | 447 |
Note. LC = Learning Circle. NA = Not applicable.
3.3. Fidelity to the model and accuracy in presenting the research in learning circles
Here, fidelity reflects facilitators’ adherence to the learning circle format. Results show fidelity to the curriculum approximately 80% of the time, ranging among villages from 71% to 90%. Learning circle two, which had a more complicated process than the other learning circles had the lowest fidelity at 60%, and learning circle seven had the highest fidelity at 92%. Tracking both facilitators and participants interpretation of the ‘what do we know’ data accurately, they did so about 80% of the time. There were no instances in which data was incorrectly presented or interpreted, but in 19% of learning circles, participants discussed tangential topics without explicitly demonstrating understanding of the information presented.
3.4. Themes from the learning circles
Audio recordings were allowed by participants for 52 of the 59 Learning Circles (LC) that took place. General sentiments about the PC CARES model and learning circles were positive. Participants expressed appreciation about the engaged learning process and liked that sessions were facilitated by local people. Many emphasized the importance of self-determination and culture for prevention. An example follows:
“It’s great to see people in the villages being in charge of their own. It’s a great model for us to work with. It has a lot of cultural pieces to it when we do our work and want to get well.”
In the first learning circle, participants appreciated the film, which featured local people discussing wellness and the multiple social determinants of suicide. For many, this understanding highlighted the importance of working together for wellness, saying,
“What I got from the video is involving the whole village as one. Involving everybody and letting them know that they do matter. They do have a purpose. They are important.” (LC1)
Across the vast majority of learning circles, participants talked about the simple ways in which they can be involved in prevention. Here is an example from learning circle two in which a local survey of youth and adults was shared in which youth advocated for adults to ‘talk to them’ as essential to prevention:
“One thing I will take away from this learning session is just getting the results from the survey - their [youth] view, their thoughts is most helpful in preventing suicide. Which is, ‘Talk to them!’ There are youth, children crying inside but they can’t or [are] not going to open up. Eventually they will open up if we give some time to listen. It was an eye-opener to see the result from the youth. ”
In the third learning circle, the content focuses on seasonality of increased suicidal behavior among youth in the region during the summer months (Silveira et al., 2016). One participant said:
“It really opened up my eyes as a parent to make sure that I have more structure in the home during the summer months and to keep things active in my family. I am so thankful for my mom for always involving my kids at camp in the summer.”
In LC 4, content focuses on community and institutional level factors that affect suicide risk. Participants talked about mobilizing their community:
“One thing we have recognized is that there isn’t very much participation. We don’t know what it is, you know, but to maybe get people kind of motivated and wanting to be out and engaging in the community. And to recognize we all have a role.”
LC 5 uses a paired activity to give participants a chance to practice active and non-judgmental listening in order to promote overall wellness. Participants shared their experience with the activity and some talked about how they might apply it in their lives:
“I felt like I unloaded myself to have someone listen to me as I talked. Some of us want to say something and always want to interrupt. It’s good to have their full attention to listening, no interrupting.”
LC 6 shows that making it 10 or more minutes harder for someone to access “lethal means” (like a loaded gun) can save lives. Participants talked about gun safety, and appreciated the “reminder”:
“It’s a good reminder for me. When my family is drinking. I’ve been always having to hide sharp objects and guns and everything.”
LC 7 uses a case study of “Jane Doe,” asking participants to think about what the best ways to support someone after an attempted suicide are, and shares an evidence-based approach of sending “non-demanding” letters (or texts) to someone after a suicide attempt (Motto and Bostrom, 2001). One participant commented:
“The reality is that a lot of people don’t know how to deal with it when someone attempts suicide. Like the individual you were talking about. Had someone intervened or told him he was amazing or worthwhile or ... would he have done the same thing?”
LC 8 focuses on postvention, and shares a table with two columns labeled “riskier” and “protective” with common examples of actions and narratives that can influence others. The table shows what can be done to lower the risk of contagion after a suicide in the community. This topic is difficult because it describes some common activities (e.g., hosting basketball tournaments in the person’s honor) as potentially dangerous (Cox et al., 2012; Jordan, 2017). The responses to this session were more mixed, with people wondering about some of the assertions in the table:
“Our main reaction - it opened our minds to new concepts about factors increasing or decreasing risk of suicide. Ideas that we’ve never heard before and we were a bit surprised by all the information in the paper.”
LC 9 asks participants to review what they discussed and learned throughout the monthly sessions, and to decide how (or if) they want to move forward. Discussions centered on what they learned and what the next steps could be:
“It is important to try and get everybody - one way. Sometimes turnout is not all that great. One way is going to each organization of what you want to do and that you want to have them all ... Visit each organization. Get their attention.”
These comments from participants demonstrate that many participants valued the process of PC CARES and shows some of the dominant themes emerging from the sessions.
3.5. Survey results
Eighty-three PC CARES participants answered both the pre- and follow-up surveys, and these matched surveys demonstrate positive change using paired t-tests in all four constructs: perceived knowledge, perceived skills, attitude towards prevention, and community of practice; and statistically significant change in perceived knowledge, skills, and community of practice with medium effect sizes (see online supplemental materials). These findings suggest that PC CARES participants have more knowledge, more skills, and a stronger ‘community of practice’ with which to make positive changes for prevention in their communities after attending two or more learning circles. When comparing the main construct scores of PC CARES participants’ at baseline to those of non-participants at follow-up, using two-sample t-tests, PC CARES participants surprisingly began the intervention with statistically significant lower scores than non-participants in perceived knowledge, perceived skills, and community of practice. After the intervention, participants showed higher scores than non-participants across all four constructs, but only perceived knowledge and more positive attitude toward prevention were significantly higher than non-participant scores, statistically, with small to medium effect sizes (See Table 2).
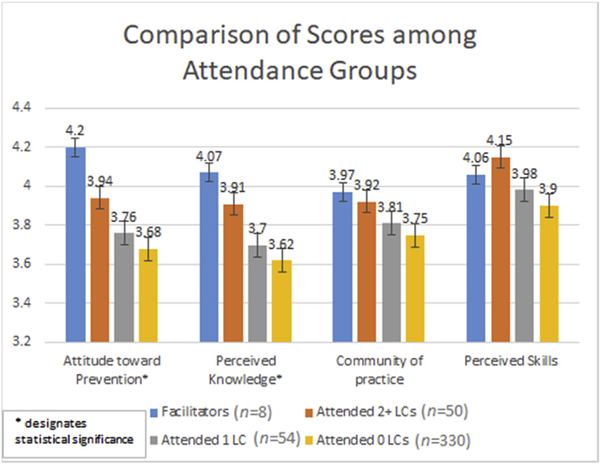
Our measures also document a dosage effect, with those who participated in more PC CARES education gaining the most in self-perceived knowledge of prevention, skills, and community of practice. Self-perceived skills for prevention, however, seemed to have a ceiling effect in that the PC CARES facilitators may have assessed their skill-level more harshly due to their deeper understanding of nuances and potential difficulty of applying such skills. Differences between groups based on number of learning circles attended were tested using one-way analysis of variance, followed by Bonferroni multiple comparisons. Self-perceived knowledge and attitudes toward prevention scores were statistically significantly higher among those who attended two or more learning circles compared to non-participants.
Prevention behavior outcomes of PC CARES participants and others
Approximately three months after the last learning circle, the Suicide Prevention Behavior survey showed that PC CARES participants reported more preventive actions compared to non-participants (in all but one category, Support after an Attempt). There was a statistically significant difference between the two groups in six of the 13 categories of prevention actions associated with PC CARES (see Table 3). Within these categories, community protective factors and wellness promotion have medium effect sizes, indicating that participants show the greatest difference in these kinds of prevention activities when compared to non-participants.
Table 3.
Percentage of Participants and Non-Participants who Performed 2 or More Prevention Actions in Each Construct.
| Construct | Percentage of participants who did 2 + actions in this construct (n = 112) | Percentage of non-participants who did 2 + actions in this construct (n = 335) | Prob > χ2 | Effect Size (Cramer’s V) |
|---|---|---|---|---|
| Historical Trauma and Colonization | 70% | 47% | < .01 | .195 |
| Seasonality | 71% | 63% | .11 | .077 |
| Support After an Attempt | 70% | 71% | .83 | −.011 |
| Primary Prevention | 67% | 51% | < .01 | .136 |
| Secondary Prevention | 79% | 76% | .43 | .037 |
| Support within Family | 80% | 70% | .03 | .105 |
| Role of Adults | 88% | 79% | .06 | .090 |
| Listening | 88% | 84% | .25 | .055 |
| Open Communication | 80% | 68% | .01 | .120 |
| Community Protective Factors | 60% | 23% | < .01 | .338 |
| Restrict Means | 63% | 57% | .34 | .046 |
| Postvention | 42% | 36% | .27 | .052 |
| Wellness Promotion | 67% | 33% | < .01 | .297 |
Note. For Cramer’s V, 0.1 indicates a small effect size, 0.3 indicates medium effect size, and 0.5 indicates a large effect size (Zaiontz, 2012). Items in boldface are statistically significant.
Social network results
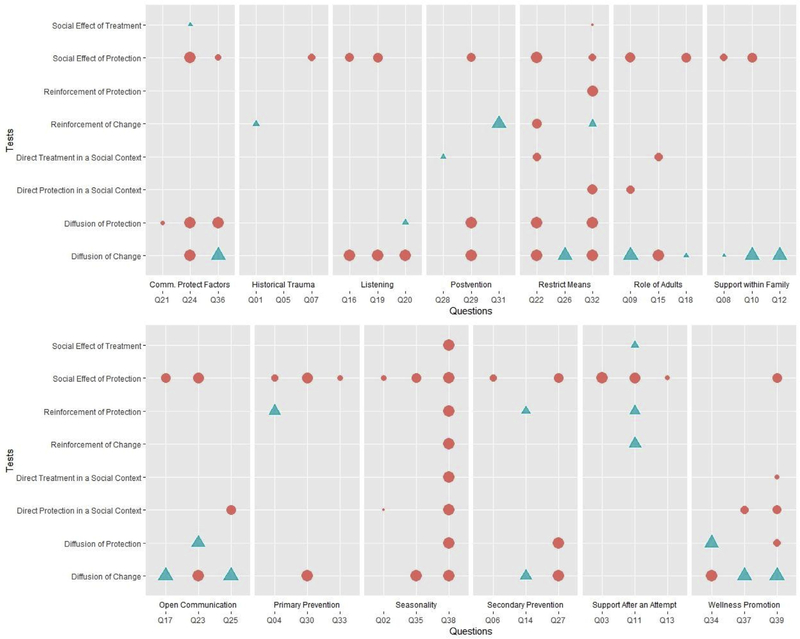
Fig. 2 presents the results of the PC CARES intervention in terms of social diffusion across the 13 categories (39 items) of prevention behaviors. A circle indicates a statistically significant positive behavior or attitude change in association with PC CARES, while a triangle suggests the opposite. The size of each symbol corresponds to how significant this relationship is—measured as the distance between the discovered data and a null model conforming to a beta distribution. Symbols that are larger thus suggest a more significant relationship between PC CARES and the behavior, attitude, or social impact discovered. Empty cells indicate that no significant relationship was found for a question given the respective measure.
Fig. 2.
Social Network Results: Significance size and directionality of eight tests from PC CARES prevention program. Note. Pink circles signify statistically significant positive change, and blue triangles signify statistically significant negative change. The size of the symbol corresponds the magnitude of association between PC CARES and the item. Empty cells indicate that no significant relationship was found for a question given the respective measure. See online supplements for the measures related to Q1 - Q39 (Appendix C) and for a description of the tests used (Appendix D). (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
PC CARES seems to have made important impact in terms of sustaining prevention. Twenty-six items (66.7%) showed significant positive effects with zero negative impacts. Individuals that had a close associate (e.g., friend or family member) participate in PC CARES were associated with a statistically significant continuation of prevention behaviors regardless of their own participation in PC CARES. Simply put, non-participants who were ‘close to’ PC CARES participants sustained or increased prevention activities without participating themselves.
4. Discussion
This intervention arose to address the health disparity of AN youth suicide in a rural and remote, under-resourced region of Alaska. Contributors to this health issue are complex and diverse, and often linked to colonization by local people (Rhoades, 2003; Goldston et al., 2008; Gracey and King, 2009). AN youth suicide, first documented in the participating region in the 1960s, coincides with unilateral imposition of educational, social, economic, and political (i.e., colonial) systems (Chance, 1990; Djulbegovic and Guyatt, 2017). In this context, it is imperative that suicide prevention includes—at its heart—cultural respect and a commitment to self-determination (Trout et al., 2018; Hacker et al., 2012). Additionally, efforts are likely to be more effective if they build on ‘best practices’ from research in ways that work for the communities involved (Brownson et al., 2012; Wallerstein and Duran, 2010). To achieve this end, PC CARES builds on local resources, aligns with cultural and social protocols, and invites local wisdom: inviting reflection, storytelling, and locally-determined actions in response to prevention science.
This culturally-situated, engaged, and personally-meaningful approach to translating research to practice is more likely to foster long-term learning and action when compared to instructive educational methods (Wallerstein and Duran, 2010; Swanson et al., 2015). Much suicide prevention education is instructive—focused on learning decontextualized knowledge and skills (Isaac et al., 2009)—rather than engaging in reflective and applied learning, which may be why outcomes have been disappointing in Indigenous communities (Wasserman and Faust, 1994; Mann et al., 2005). Our innovation then centers on creating a method in which solutions to complex problems, like AN youth suicide, will build on research, but be determined by the participating communities themselves (White, 2012). This approach shows promise for under-resourced communities that have limited access to practical research that could inform their collaborative work. This pilot shows promising evidence of building knowledge and skills, productive relationships, and spurring preventive actions for participants and those ‘close to’ them.
Thematic analysis of learning circles showed participants appreciated the engaged learning model led by local facilitators and illustrated how people engaged with the content. Transcripts documented participants questioning new information and discussing how it fit (or did not fit) their understandings and experiences, particularly with difficult content (LC 8). This ‘give and take’ with scientific information demonstrates a new way to translate prevention research to practice. Instead of a unidirectional approach, PC CARES shares scientific information and invites participants to consider how (or if) that knowledge can be used within the context of their experiences, understandings, roles, and constraints. This bidirectional dialogue about research considers local and cultural knowledge as equally important to dissemination and implementation.
The train-the-trainer model worked overall, but participation in the nine sessions declined over time (see online supplemental materials). Our community partners attribute this pattern to a number of factors: (1) people felt too busy to take the time to attend nine two to 3h learning circles, (2) some did not know that PC CARES had nine different learning circles, so they did not attend after the first one, and (3) the monthly timing may have dampened enthusiasm between sessions. Suggested improvements to the model include fewer learning circles over a shorter period of time. This modification allows people to engage more intensively in a focused effort, after which groups can decide how they want to continue. This approach seems feasible while also inviting flexibility as additional priorities come into view.
Our survey findings of learning and behavioral outcome indicators are promising with perceived knowledge, skills, attitudes toward prevention, and ‘community of practice’ outcomes moving in the predicted positive direction from pre-to follow-up, with statistically significant positive changes for three of the four constructs (see Table 2). Additionally, there was a basic dose-response when comparing PC CARES facilitators: people attending more and less sessions with one caveat. Facilitators did not assess their skill level as high as others at follow-up (see Fig. 1). When asked about this result, facilitators talked about having a more complex understanding of the possible difficulties in applying prevention skills in everyday life.
Fig. 1.
Comparison of Mean Learning Outcome Scores by dose of intervention. Note: * represents a statistically significant finding between those who completed 2 + LCs and those who attended 0 LCs. All other pair-wise comparisons among groups were non-significant.
Interestingly, the scores of non-participants, collected at the same time as the follow-up, were higher than the pre-scores of PC CARES participants. However, the participants’ scores caught up to non-participants in half of the constructs and exceeded them on the other two by follow-up (see Table 2). Although this cross-sectional data does not demonstrate cause and effect, it is encouraging. Furthermore, participants left learning circles with ideas for how they would utilize what they learned in their lives. Participants reported doing more preventive and health-promoting behaviors after participating in PC CARES, and did more than non-participants (see Table 3).
The social network data tracked social impact and demonstrated positive social effects: sustaining or enhancing prevention behaviors of people ‘close to’ intervention participants (see Fig. 2). This suggests that PC CARES participants influenced friends and families to maintain or to do more preventive behaviors when compared with people ‘not close’ to intervention participants. This finding is particularly important for health planners, demonstrating considerable diffusion via social mechanisms, which has important implications for intervention scaling. It suggests that the informal educational approach can reach people who are not predisposed to participate in prevention training. The potential for change is greater in these ‘close associates’ because they may not be motivated toward prevention (since they did not attend the intervention), but can be socially influenced by those who are (PC CARES participants).
4.1. Limitations
A randomized clinical trial was not feasible mainly due to our community partners’ preferences and the preliminary nature of the work. The pre-follow-up design does not account for other changes within the participating communities that may have influenced the results. Additionally, baseline surveys were not administered to non-participants to assess their level of perceived suicide prevention knowledge, skills, attitudes, and community of practice. Surprisingly, non-participants survey results, done only at follow-up, were higher than the pre-survey scores of participants. Non-participants scores, at the time of the baseline survey 15 months prior, are not known. Lastly, the pilot study did not measure the frequency of people’s prevention behavior before and after the intervention. Instead, PC CARES participants and others were asked if they had taken specific action in the past three months. If people indicated that they had, they were asked to assess whether they did this more, less, or the same as for the previous three months. Such perceptions may not be accurate. Social desirability likely played a factor in how people answered some questions in our survey. Despite these clear limitations, the study demonstrated several strengths, including confirming the feasibility and acceptability of our community mobilization approach to suicide prevention. Survey results show a significant increase in participants’ sense of ‘community of practice’ and perceived learning, and generally gave very positive feedback about both the process and the outcomes of the intervention.
5. Conclusions
Suicide prevention and mental health issues in Indigenous communities have been difficult to address, and one key factor for this difficulty is the need for both evidence-based and culturally-responsive, locally-relevant interventions (Wallerstein and Duran, 2010; Nelson and Wilson., 2017). PC CARES is one such approach. Results of the study indicate positive community impact, including gains in self-perceived knowledge, skills, and relationships associated with prevention. Additional social effects show positive, statistically significant sustained or increased prevention activities of people ‘close to’ PC CARES participants (66 of 91; 73%). Although more research is needed to investigate efficacy, the promising results indicate that PC CARES may offer under-resourced communities a practical, scalable method for translating research evidence into self-determined, locally and culturally-responsive suicide prevention practice.
Supplementary Material
Acknowledgements
The work reported on in this article was supported by funding from the National Institute of Mental Health (R34MH096884), the Substance Abuse and Mental Health Administration Maniilaq Association, NANA Corporation and Kawerak, Inc.
Footnotes
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.socscimed.2019.05.028.
References
- Alaska Bureau of Vital Statistics, 2016. Data and Statistics. Available at: http://dhss.alaska.gov/dph/VitalStats/Documents/PDFs/VitalStatistics_Annualreport_2016.pdf.
- Barnett ML, Gonzalez A, Miranda J, Chavira DA, Lau AS, 2018a. Mobilizing community health workers to address mental health disparities for underserved populations: a systematic review. Adm. Policy Ment. Health 45 (2), 195–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett ML, Lau AS, Miranda J, 2018b. Lay health worker involvement in evidence-based treatment delivery: a conceptual model to address disparities in care. Annu. Rev. Clin. Psychol 14, 185–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beals J, Manson SM, Whitesell NR, Spicer P, Novins DK, Mitchell CM, 2005. Prevalence of DSM-IV disorders and attendant help-seeking in 2 American Indian reservation populations. Arch. Gen. Psychiatr 62 (1) pp. 99–08. [DOI] [PubMed] [Google Scholar]
- Beautrais A, Collings S, Ehrhardt P, Henare K, 2005. Suicide Prevention: A Review of Evidence of Risk and Protective Factors, and Points of Effective Intervention. Ministry of Health Wellington. [Google Scholar]
- Berman M, 2014. Suicide among young Alaska Native men: community risk factors and alcohol control. Am. J. Public Health 104 (S3), S329–S335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjerregaard P, Kue Young T, Dewailly E, Ebbesson SO, 2004. Indigenous health in the Arctic: an overview of the circumpolar Inuit population. Scand. J. Publ. Health 32 (5), 390–395. [DOI] [PubMed] [Google Scholar]
- Brownson RC, Allen P, Duggan K, Stamatakis KA, Erwin PC, 2012. Fostering more-effective public health by identifying administrative evidence-based practices: a review of the literature. Am. J. Prev. Med 43 (3), 309–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchanan D, Miller F, Wallerstein N, 2007. Ethical issues in community-based participatory research: balancing rigorous research with community participation in community intervention studies. In: Progress in Community Health Partnerships, Research Education and Action, vol. 1 pp. 153–160. [DOI] [PubMed] [Google Scholar]
- Chance NA, 1990. The Inupiat and Arctic Alaska: an Ethnography of Development. Holt Rinehart & Winston. [Google Scholar]
- Chandler MJ, Lalonde C, 1998. Cultural continuity as a hedge against suicide in Canada’s First Nations. Transcult. Psychiatr 35 (2), 191–219. [Google Scholar]
- Chandler MJ, Lalonde C, 2004. Transferring whose knowledge? Exchanging whose best practices?: on knowing about indigenous knowledge and aboriginal suicide. Aborig. Policy. Res. : Setting Agenda Change. 2, 111–123. [Google Scholar]
- Christakis N, Fowler J, 2013. Social contagion theory: examining dynamic social networks and human behavior. Stat. Med 32, 556–577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox GR, Robinson J, Williamson M, Lockley A, Cheung YTD, Pirkis J, 2012. Suicide clusters in young people: evidence for the effectiveness of postvention strategies. Crisis J. Crisis Interv. Suicide Prev 33 (4), 208. [DOI] [PubMed] [Google Scholar]
- Crepeau-Hobson MF, Leech NL, 2014. The impact of exposure to peer suicidal self--directed violence on youth suicidal behavior: a critical review of the literature. Suicide Life-Threatening Behav. 44 (1), 58–77. [DOI] [PubMed] [Google Scholar]
- Djulbegovic B, Guyatt GH, 2017. Progress in evidence-based medicine: a quarter century on. The Lancet 390 (10092), 415–423. [DOI] [PubMed] [Google Scholar]
- Duclos CW, Beals J, Novins DK, Martin C, Jewett CS & Manson SM “Prevalence of common psychiatric disorders among American Indian adolescent detainees”, J. Am. Acad. Child Adolesc. Psychiatry, vol. 37, no. 8, pp. 866–873. [DOI] [PubMed] [Google Scholar]
- Freedenthal S, Stiffman AR, 2007. They might think I was crazy”: young American Indians’ reasons for not seeking help when suicidal. J. Adolesc. Res 22 (1), 58–77. [Google Scholar]
- Gest S, Osgood D, Feinberg M, Bierman K, Moody J, 2011. Strengthening prevention program theories and evaluations: contributions from social network analysis. Prev. Sci 12 (4), 349–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldston DB, Molock SD, Whitbeck LB, Murakami JL, Zayas LH, Hall GCN, 2008. Cultural considerations in adolescent suicide prevention and psychosocial treatment. Am. Psychol 63 (1), 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gone JP, Alcántara C, 2010. Suicide in native American communities: a transactional-ecological formulation of the problem. In: Routledge, pp. 180–206. [Google Scholar]
- Gone JP, Trimble JE, 2012. American Indian and Alaska Native mental health: diverse perspectives on enduring disparities. Annu. Rev. Clin. Psychol 8, 131–160. [DOI] [PubMed] [Google Scholar]
- Goodwin-Smith I, Hicks N, Hawke M, Alver G, Raftery P, 2013. Living beyond Aboriginal suicide: developing a culturally appropriate and accessible suicide postvention service for Aboriginal communities in South Australia. Adv. Ment. Health 11 (3), 238–245. [Google Scholar]
- Gracey M, King M, 2009. Indigenous health part 1: determinants and disease patterns. The Lancet 374 (9683), 65–75. [DOI] [PubMed] [Google Scholar]
- Hacker K, Tendulkar SA, Rideout C, Bhuiya N, Trinh-Shevrin C, Savage CP, DiGirolamo A, 2012. Community capacity building and sustainability: outcomes of community-based participatory research. Prog. Community. Health Partnersh.: Res. Educ. Action 6 (3), 349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill R, Perkins R, Wexler L, 2007. An analysis of hospital visits during the 12 months preceding suicide death in Northern Alaska. Alaska Med 49 (1), 16–21. [PubMed] [Google Scholar]
- Hirshberg D, 2008. It was bad or it was good”: Alaska Natives in past boarding schools. J. Am. Indian Educ 47 (3), 5. [Google Scholar]
- Isaac M, Elias B, Katz LY, Belik SL, Deane FP, Enns MW, Swampy Cree Suicide Prevention Team (12 members) 8, 2009. Gatekeeper training as a preventative intervention for suicide: a systematic review. Can. J. Psychiatr 54 (4), 260–268. [DOI] [PubMed] [Google Scholar]
- Jordan JR, 2017. Postvention is prevention—the case for suicide postvention. Death Stud. 41 (10), 614–621. [DOI] [PubMed] [Google Scholar]
- Kim J, 2018. Beyond the trigger: the mental health consequences of in-home firearm access among children of gun owners. Soc. Sci. Med 203, 51–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King M, Smith A, Gracey M, 2009. Indigenous health part 2: the underlying causes of the health gap. The Lancet 374 (9683), 76–85. [DOI] [PubMed] [Google Scholar]
- Kraus RF, 1974. Suicidal behavior in Alaska natives. Alaska Med. 16 (1), 2–6. [Google Scholar]
- Kraus RF, Buffler PA, 1979. Sociocultural stress and the American native in Alaska: an analysis of changing patterns of psychiatric illness and alcohol abuse among Alaska natives. Cult. Med. Psychiatr 3 (2), 111–151. [DOI] [PubMed] [Google Scholar]
- Lee HW, Melson M, Ivanich J, Habecker P, Gauthier GR, Wexler L, Khan B, Dombrowski K, 2018a. Mapping the structure of perceptions in helping networks of Alaska natives. PLoS One 13 (11) e0204343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee HW, Gauthier GR, Ivanich JD, Wexler LM, Khan B, Dombrowski K, 2018b. A method for assessing the success and failure of community-level interventions in the presence of network diffusion, social reinforcement, and related social effects. PLoS One. arXiv:1801.08612v1. [Google Scholar]
- Lehti V, Niemelä S, Hoven C, Mandell D, Sourander A, 2009. Mental health, substance use and suicidal behaviour among young indigenous people in the Arctic: a systematic review. Soc. Sci. Med 69 (8), 1194–1203. [DOI] [PubMed] [Google Scholar]
- LeMaster PL, Beals J, Novins DK, Manson SM, 2004. The prevalence of suicidal behaviors among northern plains American Indians. Suicide Life-Threatening Behav. 34 (3), 242–254. [DOI] [PubMed] [Google Scholar]
- Luoma JB, Martin CE, Pearson JL, 2002. Contact with mental health and primary care providers before suicide: a review of the evidence. Am. J. Psychiatry 159 (6), 909–916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mann J, Apter A, Bertolote J, Beautrais A, Currier D, Haas A, Mehlum L, 2005. Suicide prevention strategies: a systematic review. J. Am. Med. Assoc.: J. Am. Med. Assoc 294 (16), 2064–2074. [DOI] [PubMed] [Google Scholar]
- Motto JA, Bostrom AG, 2001. A randomized controlled trial of postcrisis suicide prevention. Psychiatr. Serv 52, 828–833. [DOI] [PubMed] [Google Scholar]
- Mullany B, Barlow A, Goklish N, Larzelere-Hinton F, Cwik M, Craig M, Walkup JT, 2009. Toward understanding suicide among youths: results from the white mountain Apache tribally mandated suicide surveillance system, 2001–2006. Am. J. Public Health 99 (10), 1840–1848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson Sarah E., Wilson Kathi, 2017. The mental health of Indigenous peoples in Canada: a critical review of research. Soc. Sci. Med 176, 93–112. [DOI] [PubMed] [Google Scholar]
- Oetzel J, Duran B, Lucero J, Jiang Y, Novins D, Manson S, Beals J, 2006. Rural American Indians’ perspectives of obstacles in the mental health treatment process in three treatment sectors. Psychol. Serv 3 (2), 117–128. [Google Scholar]
- Palinkas L, Holloway I, Rice E, Brown C, Valente T, Chamberlain P, 2013. Influence network linkages across implementation strategy conditions in a randomized controlled trial of two strategies for scaling up evidence-based practices in public youth-serving systems. Implement. Sci. 2013 8 (133), 1–11 vol. 8, no. 133, pp. 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters WM, Green JM, Gauthier PE, 2014. Native American Medicine: the Implications of History and the Embodiment of Culture. vol. 2 Multicultural Approaches to Health and Wellness in America, pp. 171. [Google Scholar]
- Rhoades ER, 2003. The health status of American Indian and Alaska native males. Am. J. Public Health 93 (5), 774–778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silveira ML, Wexler L, Chamberlain J, Money K, Spencer RMC, Reich NG, Bertone-Johnson ER, 2016. Seasonality of suicide behavior in Northwest Alaska: 1990–2009. Publ. Health 137, 35–43. [DOI] [PubMed] [Google Scholar]
- Swanson A, Bonnie R, Appelbaum P, 2015. Getting serious about reducing suicide: more “how” and less “why”. J. Am. Med. Assoc.: J. Am. Med. Assoc 314 (21), 2229–2230. [DOI] [PubMed] [Google Scholar]
- Trout L, McEachern D, Mullany A*, White L*, Wexler L+ +, 2018. Decoloniality as framework for Alaska Native youth suicide prevention: promoting community conversations about research to end suicide. Am. J. Community Psychol. 62 (3–4), 396–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valente T, Palinkas L, Czaja S, Chu K, Brown C, 2015. Social network analysis for program implementation. PLoS One 10 e0131712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Der Feltz-cornelis, Christina M, Sarchiapone M, Postuvan V, Volker D, Roskar S, Grum AT, Ibelshauser A, 2011. Best practice elements of multilevel suicide prevention strategies. Crisis 32 (6), 319–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallerstein N, Duran B, 2010. Community-based participatory research contributions to intervention research: the intersection of science and practice to improve health equity. Am. J. Public Health 100 (S1), S40–S46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wasserman S, Faust K, 1994. Social Network Analysis: Methods and Applications. Cambridge University Press. [Google Scholar]
- Wexler L, 2006. Inupiat youth suicide & culture loss: changing community conversations. Soc. Sci. Med. 63, 2938–2948. [DOI] [PubMed] [Google Scholar]
- Wexler L, Gone J, 2012. Examining cultural incongruities in western and indigenous suicide prevention to develop responsive programming. Am. J. Public Health 102 (5), 800–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wexler L, White J, Trainor B, 2015. Why an alternative to suicide prevention gatekeeper training is needed for rural Indigenous communities: presenting an empowering community storytelling approach. Crit. Public Health 25 (2), 205–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wexler L, McEachern D, DiFulvio G, Smith C, Graham LF, Dombrowski K, 2016. Creating a community of practice to prevent suicide through multiple channels: describing the theoretical foundations and structured learning of PC CARES. Int. Q Community Health Educ. 36 (2), 115–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wexler L, Silveira ML, Bertone-Johnson E, 2012. Factors associated with alaska native fatal and nonfatal suicidal behaviors 2001–2009: considering trends and discussing implications for prevention. Arch. Suicide Res 16 (4) 273–286.1. [DOI] [PubMed] [Google Scholar]
- Wexler L, Trout L, Rataj S, Kirk T, Moto R, McEachern D, 2017. Promoting Community Conversations about Research to End Suicide: learning and behavioural outcomes of a training-of-trainers model to facilitate grassroots community health education to address Indigenous youth suicide prevention. Int. J. Circumpolar Health 76 (1), 1345277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White J, 2012. Youth suicide as a “wild” problem: implications for prevention practice. Suicidology online 3, 42–50. [Google Scholar]
- Williams AM, Kulig JC, 2012. Health and Place in Rural Canada. Health in rural Canada, pp. 1–19. [Google Scholar]
- Willmon-Haque S, BigFoot SD, 2008. Violence and the effects of trauma on American Indian and Alaska Native populations. J. Emot. Abus 8 (1–2), 51–66. [Google Scholar]
- Wilson A, Marshall A, 2010. The support needs and experiences of suicidally bereaved family and friends. Death Stud. 34 (7), 625–640. [DOI] [PubMed] [Google Scholar]
- Yip PS, Caine E, Yousuf S, Chang S, Wu KC, Chen Y, 2012. Means restriction for suicide prevention. The Lancet 379 (9834), 2393–2399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaiontz C, 2012. Effect Size for Chi-Square Test. Retrieved from Real Statistics Using Excel: http://www.real-statistics.com/chi-square-and-f-distributions/effect-size-chi-square/.
- Zaiontz C, 2015. Standardized Effect Size. Retrieved from Real Statistics Using Excel: http://www.real-statistics.com/sampling-distributions/standardized-effect-size/.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.