Abstract
Background
Venous thromboembolism (VTE) is very rare in childhood. Nevertheless, its incidence has increased recently. This study aimed to identify risk factors for developing thrombosis in childhood cancers and other childhood diseases through the Korean Health Insurance Review and Assessment Service database.
Methods
Data were extracted from the Korean Health Insurance Review and Assessment Service database. Children and young adults from 1 month to 29 years of age were eligible, and 21,747 cases of VTE between January 2008 and December 2016 were identified.
Results
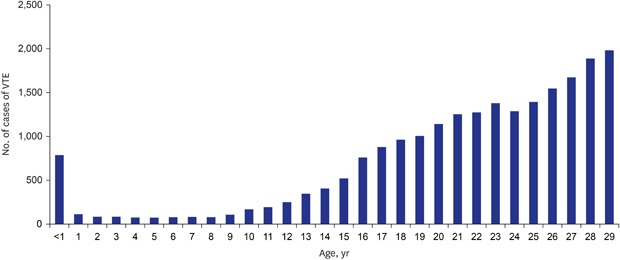
The VTE incidence was high in children younger than 1 year of age. After 1 year of age, its incidence decreased rapidly and gradually increased. The VTE incidence for children between 0 and 1 year of age was 10.23-fold higher than that for those between 1 and 5 years of age. Annual VTE incidence increased by year. The age-standardized annual incidence rates were 9.98 per 100,000 population in 2008 and 22.53 per 100,000 population in 2016. The age-standardized annual incidence rate increased 2.25-fold during the 8 years. The lower extremity was the most common site of venous thrombosis.
Conclusion
The incidence of VTE in a population younger than 30 years was 13.11 per 100,000 persons in Korea. We found a bimodal age distribution of the VTE incidence with peaks at infancy and again after 16 years. The incidence of portal vein thrombosis was high in infants, and infection and malignancy were the most common comorbidities in patients with VTE.
Keywords: Adolescent, Epidemiology, Pediatrics, Young Adult, Venous Thromboembolism
Graphical Abstract
INTRODUCTION
Venous thromboembolism (VTE) is a rare disease that is associated with severe venous thrombosis and obstruction. Nevertheless, its incidence has increased.1,2 With the development of treatment for pediatric patients with severe thrombosis and the increased VTE awareness, the rate of accurate diagnosis of pediatric thrombosis is increasing.1,3,4
Some studies have estimated VTE incidence in children.1,5,6 In these studies, the annual VTE incidence per 10,000 children per year was 0.07 to 0.14 or 5.3 per 10,000 hospital admissions and 24 per 10,000 neonatal intensive care unit (NICU) admissions.6,7 In tertiary care hospitals in the United States, the reported VTE incidence rates were higher and increased by 70% from 2001 to 2007, i.e., from 34 to 58 per 10,000 children.4 Risk factors for VTE in children include intravenous catheter use, surgery, trauma, malignancy, and chronic inflammatory conditions. The most common age of onset of VTE in children is < 1 year old, which is followed by adolescence.3,6,8,9,10
The purpose of this study is to identify the risk factors for thrombosis in children with cancer and other pediatric diseases as well as pediatric VTE incidence using the Health Insurance Review and Assessment Service (HIRA) database.
METHODS
Data sources
The National Health Insurance system is the only public medical insurance system operated by the Ministry for Health, Welfare, and Family Affairs in Korea. This universal health coverage system covers approximately 98% of the overall Korean population.11 The HIRA database contains information on over 46 million patients per year, which accounts for 90% of the total population in Korea and almost 80,000 healthcare service providers across Korea as of 2011. Moreover, claims data of the HIRA database include patients' diagnosis, treatment, procedures, surgical history, and prescription drugs, and serve as a valuable resource for healthcare service research.11,12,13
Case definition
We identified patients diagnosed as having VTE from January 2007 to December 2017 from the HIRA database using diagnostic codes based on the Korean Classification of Disease, sixth edition, which was a modified version of the International Classification of Disease. The process was performed automatically with a computer-based algorithm. The codes for central nervous system (CNS) VTE included G08 (intracranial and intraspinal phlebitis and thrombophlebitis), I63.6 (cerebral infarction due to cerebral venous thrombosis, nonpyogenic), and I67.6 (nonpyogenic thrombosis of the intracranial venous system). The codes for VTE of the extremity included I80.2 (phlebitis and thrombophlebitis of other deep vessels of the lower extremities) and I80.3 (phlebitis and thrombophlebitis of the lower extremities, unspecified). The codes for pulmonary embolism included I26 (pulmonary embolism), I26.0 (pulmonary embolism with mention of acute cor pulmonale), and I26.9 (pulmonary embolism without mention of acute cor pulmonale). The codes for intra-abdominal thrombosis included I81 (portal vein thrombosis), I82.2 (embolism and thrombosis of vena cava), and I82.3 (embolism or thrombosis of the renal vein). The codes for thrombosis of an unspecified site included I82 (other venous embolism or thrombosis), I82.8 (embolism and thrombosis of other specified veins), and I82.9 (embolism and thrombosis of unspecified vein). All International Classification of Diseases codes registered within the same period that the VTE were recorded were extracted as comorbidities.
Statistical analysis
Crude annual incidence rates (per 100,000 individuals) were determined using the number of individuals with VTE as the numerator and the annual Korean population based on the HIRA database as the denominator. The age-standardized incidence rate of VTE was directly adjusted to the mid-year population in 2010.
Ethics statement
This study was approved by the Institutional Review Board (IRB) of Yeungnam University Medical Center (IRB approval No. YUMC 2018-05-001). The need for informed consent was waived by the IRB.
RESULTS
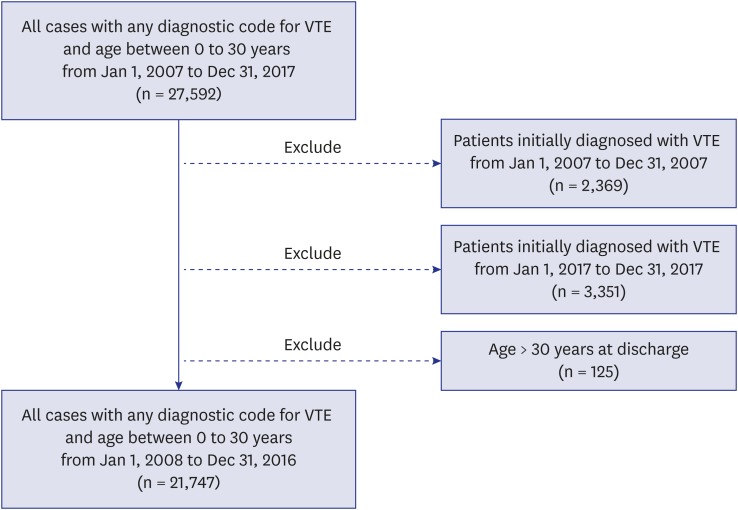
Overall, 27,592 cases with any diagnostic code for VTE (age 0–30 years) from January 1, 2007 to December 31, 2017 were identified. We excluded patients initially diagnosed as having VTE from January 1, 2007 to December 31, 2007 (n = 2,369) and those initially diagnosed as having VTE from January 1, 2017 to December 31, 2017 (n = 3,351). The reason for excluding patients in 2007 is that the patients diagnosed before 2007 may have been counted as new patients in 2007. The reason for excluding patients in 2017 is that the patients may be underestimated due to the delay in claiming data.
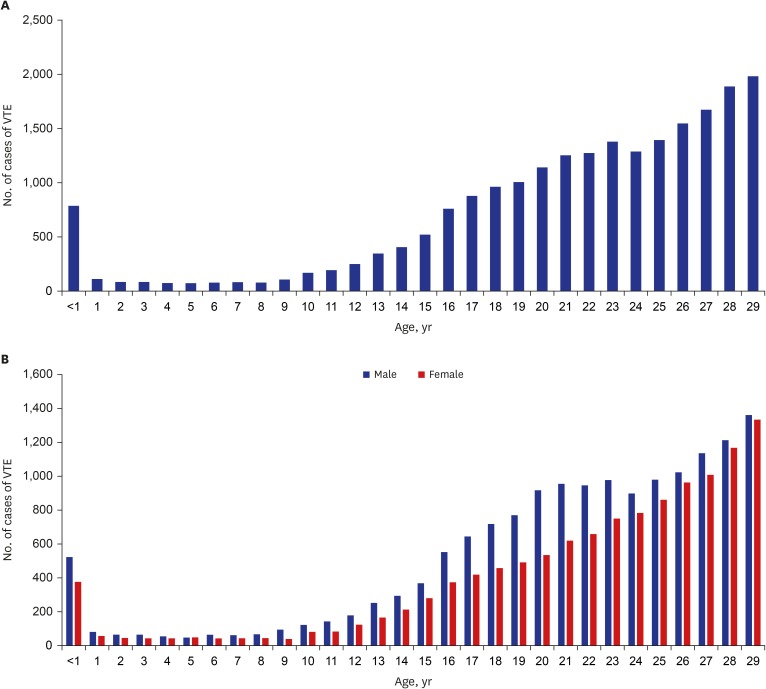
We also excluded those aged > 30 years at discharge (n = 125). Finally, 21,747 cases of VTE between January 2008 and December 2016 were included in the analysis (Fig. 1). In this study, the VTE incidence in the population < 30 years of age was 13.11 per 100,000 persons in Korea. We found a bimodal age distribution of VTE incidence with peaks at infancy and again after 16 years (Fig. 2).
Fig. 1. Flow chart of the case selection.
VTE = venous thromboembolism.
Fig. 2. Distribution of VTE incidence by age. (A) Distribution of VTE incidence in children and young adults. (B) Sexual distribution of VTE incidence in children and young adults.
VTE = venous thromboembolism.
The incidence of VTE was high in children younger than 1 year of age. After 1 year of age, VTE incidence tended to decrease rapidly and gradually increase after 9 years of age. The VTE incidence rate in children aged ≤ 1 year was 20.15 per 100,000 persons, which was 10.23-fold higher than that in children aged 1–5 years (Table 1).
Table 1. Incidence rate of venous thromboembolism by age group.
| Age group, yr | Annual incidencea (annual incidence rate)b | Overall incidence ratea | Relative riskb,c | M:F ratio | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | ||||
| 0–1 | 55 (12.4) | 53 (12.5) | 82 (18.3) | 75 (16.6) | 112 (24.1) | 104 (24.7) | 118 (28.1) | 95 (22.4) | 88 (22.4) | 20.2 | 10.2 | 1.41 |
| 1–5 | 53 (2.3) | 30 (1.3) | 40 (1.7) | 39 (1.7) | 53 (2.3) | 48 (2.0) | 47 (2.0) | 48 (2.1) | 53 (2.3) | 2.0 | 1.0 | 1.26 |
| 6–10 | 38 (1.3) | 45 (1.6) | 33 (1.2) | 66 (2.7) | 68 (2.9) | 44 (1.9) | 68 (2.9) | 69 (3.0) | 66 (2.8) | 2.3 | 1.1 | 1.57 |
| 11–15 | 156 (3.7) | 127 (3.1) | 139 (3.4) | 168 (4.2) | 173 (4.5) | 164 (4.5) | 246 (7.1) | 239 (7.3) | 286 (9.2) | 5.2 | 2.7 | 1.42 |
| 16–20 | 346 (10.4) | 339 (10.0) | 366 (10.5) | 468 (13.1) | 440 (12.4) | 448 (12.8) | 578 (16.9) | 711 (21.4) | 1,026 (31.5) | 15.5 | 7.8 | 1.58 |
| 21–25 | 567 (17.2) | 522 (16.5) | 551 (17.5) | 621 (19.8) | 606 (18.9) | 635 (19.1) | 764 (22.4) | 954 (27.3) | 1,347 (37.9) | 21.9 | 11.1 | 1.29 |
| 26–29 | 768 (23.2) | 726 (22.4) | 665 (21.6) | 735 (25.4) | 650 (24.2) | 633 (24.7) | 816 (32.3) | 915 (36.6) | 1,162 (46.2) | 28.5 | 14.5 | 1.06 |
Data are presented as number (%).
M:F ratio = male-to-female ratio.
aTotal number of patients by year; bAll rates are per 100,000 population, directly age-adjusted to the 2010 population; cRelative risk compared with that of the 1–5 years age group.
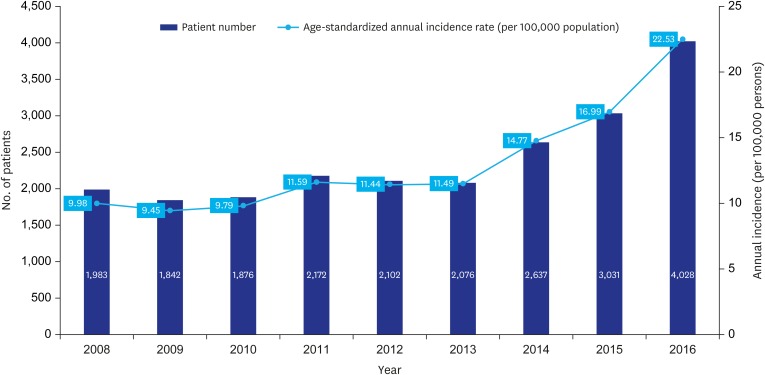
The number of patients younger than 1 year of age with VTE was 12.4 per 100,000 persons in 2008, which increased to 22.4 (80%) in 2016. During the same period, the rate of increase in VTE incidence among children aged 1–5 years was 2.3%, 6–10 years was 119%, 11–15 years was 149%, 16–20 years was 201%, 21–25 years was 119%, and 26–29 years 99%. VTE occurred more frequently in male patients than in female patients (ratio, 1.09) (Fig. 2B). There were statistically significant differences in the incidence of males and females at the ages of 6–10, 16–20, and 21–25 years old age group (Table 2). Moreover, the age-standardized annual incidence rates were 9.98 per 100,000 population in 2008 and 22.53 per 100,000 population in 2016, which showed that the age-standardized annual VTE incidence rate increased by 2.25-fold in 8 years (Fig. 3). In addition, the age-standardized annual VTE incidence rate in children aged 1–5 years was similar from 2008 to 2016. The incidence of VTE increased with age, and the 26–29-year-old age group had the highest number of patients with VTE. The highest rate of increase in VTE incidence was noted in patients aged 16–20 years.
Table 2. Sexual difference in incidence of venous thromboembolism.
| Age group, yr | Male | Female | Total | P value |
|---|---|---|---|---|
| < 28 days | 351 (59.4) | 240 (40.6) | 591 (100.0) | 0.317 |
| < 1 | 520 (58.0) | 376 (42.0) | 896 (100.0) | 0.317 |
| 1–5 | 289 (55.7) | 230 (44.3) | 519 (100.0) | 0.074 |
| 6–10 | 385 (61.0) | 246 (39.0) | 631 (100.0) | 0.047 |
| 11–15 | 1,217 (58.6) | 860 (41.4) | 2,077 (100.0) | 0.175 |
| 16–20 | 3,584 (61.2) | 2,274 (38.8) | 5,858 (100.0) | 0.009 |
| 21–25 | 4,742 (56.4) | 3,672 (43.6) | 8,414 (100.0) | 0.009 |
| 26–29 | 4,725 (51.4) | 4,472 (48.6) | 9,197 (100.0) | 0.386 |
| Total | 15,813 (56.1) | 12,370 (43.9) | 28,183 (100.0) | 0.284 |
Values are expressed as number (%).
Fig. 3. Annual incidence of venous thromboembolism in children and young adults.
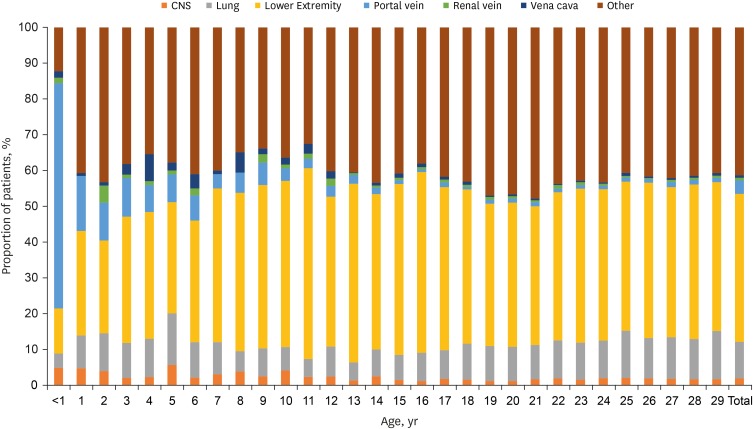
Furthermore, the lower extremity was the most common site of venous thrombosis (n = 12,608; 58%), which was followed by an unspecified site (12,593; 45.6%), the lung (3,696; 17.0%), portal vein, CNS, vena cava, and renal vein (Fig. 4). Portal vein thrombosis was the most common in children younger than 1 year of age, which was followed by other, lower extremity, CNS, lung, renal vein, and vena cava. The frequency of portal vein thrombosis decreased after 2 years of age, whereas that of the extremity and others increased. In addition, the incidence rate of CNS, renal vein, and vena cava thrombosis decreased with age, whereas that of lung and extremity thrombosis increased with age (Table 3).
Fig. 4. Distribution of the location of venous thromboembolism in children and young adults.
CNS = central nervous system.
Table 3. Location of venous thromboembolism in children and young adults.
| Location | No. (%) of patients by age group | |||||||
|---|---|---|---|---|---|---|---|---|
| 0–1 yr | 1–5 yr | 6–10 yr | 11–15 yr | 16–20 yr | 21–25 yr | 26–29 yr | Total | |
| CNS | 49 (4.8) | 19 (3.7) | 20 (3.2) | 38 (1.8) | 75 (1.3) | 146 (1.7%) | 151 (1.7) | 498 (1.8) |
| Lung | 41 (4.0) | 56 (10.8) | 48 (7.6) | 140 (6.7) | 537 (9.2) | 919 (10.9) | 1,085 (12.0) | 2,826 (10.2) |
| Lower extremity | 130 (12.7) | 162 (31.2) | 274 (43.4) | 975 (46.9) | 2,539 (43.3) | 3,495 (41.5) | 3,848 (42.5) | 11,423 (41.4) |
| Portal vein thrombosis | 647 (63.0) | 56 (10.8) | 32 (5.1) | 41 (2.0) | 61 (1.0) | 91 (1.1) | 112 (1.2) | 1,040 (3.8) |
| Renal vein thrombosis | 16 (1.6) | 8 (1.5) | 7 (1.1) | 18 (0.9) | 40 (0.7) | 53 (0.6) | 47 (0.5) | 189 (0.7) |
| Vena cava thrombosis | 18 (1.8) | 14 (2.7) | 17 (2.7) | 25 (1.2) | 40 (0.7) | 44 (0.5) | 51 (0.6) | 209 (0.8) |
| Other | 126 (12.3) | 204 (39.3) | 233 (36.9) | 840 (40.4) | 2,566 (43.8) | 3,666 (43.6) | 3,752 (41.5) | 11,387 (41.3) |
CNS = central nervous system.
Common comorbidities of VTE were infection (n = 2,449; 11/2%), malignancy (n = 1,666; 7.6%), diabetes mellitus (n = 961; 4.4%), congenital heart disease (n = 742; 3.4%), systemic connective tissue disease (n = 569; 2.6%), prematurity (n = 339; 1.5%), and nephrotic syndrome (n = 140; 0.6%) (Table 4).
Table 4. Comorbidities of patients with venous thromboembolism.
| Comorbidity | No. (%) of patients | |
|---|---|---|
| Infection | 2,449 (11.2) | |
| Malignancy | 1,666 (7.6) | |
| ALL | 133 (0.6) | |
| Non-ALL | 1,533 (7.0) | |
| DM | 961 (4.4) | |
| Congenital heart disease | 742 (3.4) | |
| Systemic connective tissue disease | 569 (2.6) | |
| SLE | 353 (1.6) | |
| Kawasaki disease | 24 (0.1) | |
| Other | 192 (0.9) | |
| Prematurity | 339 (1.5) | |
| Nephrotic syndrome | 140 (0.6) | |
| Thrombophilia | 55 (0.5) | |
ALL = acute lymphoblastic leukemia, DM = diabetes mellitus, SLE = systemic lupus erythematosus.
DISCUSSION
VTE is a rare disease that is increasingly recognized in pediatric practice. VTE typically occurs as a secondary complication of primary underlying diseases, such as sepsis, cancer, and congenital heart disease, and medical, surgical, or therapeutic interventions (e.g., central venous catheter [CVC]).2,14,15,16,17 In this study, VTE incidence in patients aged < 30 years was 13.11 per 100,000 persons in Korea. We also found a bimodal age distribution of VTE incidence with peaks at infancy and again after 16 years in children and adolescents. Infection was the most common comorbidity, followed by malignancies.
In the analysis of a Canadian registry, the VTE incidence was 5.3/10,000 hospital admissions and 0.07/10,000 population of patients < 18 years of age between 1990 and 1992.6 Thereafter, a study based on the healthcare database in Quebec, Canada found that the age-standardized VTE incidence rate in patients aged < 17 years was 0.29 per 100,000 person-years between 1994 and 2004.18 In the United States, a dramatic increase in VTE incidence in children from 2001 to 2007 was observed. The annual VTE incidence rate increased by 70%, i.e., from 34 to 58 cases per 10,000 hospital admissions.4 In this study, 21,747 VTE cases (age < 29 years) were identified between January 2008 and December 2016, and the age-standardized annual VTE incidence rate increased by 125%, i.e., from 9.98 per 100,000 population in 2008 to 22.53 per 100,000 population in 2016. A bimodal peak in population distribution of VTE incidence was observed. At ≤ 1 year of age, the VTE incidence was 20.15 per 100,000 persons, which was 10.23-fold higher than that in children aged 1–5 years. The incidence was low in children aged 1 to 15 years but gradually increased after 16 years of age.
In the study, the incidence increased steadily from 2008 to 2016 and was observed at all ages across neonate, infancy, children, adolescents and young adults. In the US, 63% of children with VTE reported at least one chronic complex medical condition, followed by cardiovascular condition (28%), followed by malignancy (14%) and neuromuscular condition (11%). In this study, due to the limitations of the HIRA database, there was a limit to the accurate analysis of chronic complex medical conditions in VTE patients. However, the analysis of disease codes associated with VTE revealed that there is a more than 2-fold increase in disease of musculoskeletal system and connective tissue, disease of digestive system, and disease of circulatory system. The cause of the increase in the incidence of VTE during the period 2006–2016 is due to the long-term survival of these patients with complex medical condition treated with advances in medical technology.
The incidence of VTE in this study tended to have male predominance at ages between 6–10 and 16–25 years in pediatric adolescents and young adults. However, the VTE incidence of females under 18 years of age was higher than males in the population-based cohort study in the United States, and the adolescent girl predominance was also reported in the nationwide population-based study in Denmark. These two studies explained that the prevalence of oral contraceptive was higher in females with VTE than in the background population because of early sexual initiation. In a recently developed clinical probability tool of the pediatric VTE diagnosis, male sex was considered to be a significant risk factor in pediatric age.19 In the study of Canada and the Netherlands 10–20 years ago, the sexual incidence rate was similar in the pediatric population, suggesting that the incidence rate of females increased gradually in recent adolescent age.5,6 Hong et al.20 analyzed the Korean HIRA database and showed that the incidence of VTE was higher in females at all ages, but the incidence of VTE was higher in males under 60 years of age. It can also be seen that VTE incidence is different in Asian populations compared to Western countries.21 These results suggest that the male predominance of VTE at young age in this result may be due to differences in social and cultural factors.
A single-center study from the United States revealed that the VTE incidence was 30 per 10,000 admissions, and young adults (18–21 years) and adolescents (14–17 years) had a significantly increased VTE incidence rate compared with children (2–9 years). A multicenter study of Korean pediatric VTE showed an overall incidence rate of 4.9 per 10,000 admissions.22
In our study, the incidence of VTE suddenly increased at ≥ 16 years of age. The respective incidence rates in patients aged 16–20, 21–25, and 26–29 years were 7.84-, 11.09-, and 14.47-fold higher than that in patients aged 1–5 years. The male-to-female ratio of VTE indicated a male predominance, although the difference in the incidence between male patients and female patients decreased starting at 25 years of age (Table 1).
Renal vein thrombosis, vena cava occlusion, and thromboembolic stroke mainly of venous origin are most common in neonates.16 Central line-associated VTEs have also been reported. Other locations of childhood thromboembolism (TE) are cerebral, portal, or mesenteric veins, and purpura fulminans was noted, albeit rarely.1
In a Canadian study, 97 thrombosis cases were identified in 22 Canadian and 42 international centers between 1990 and 1993. Eighty-nine percent of neonatal thrombosis was associated with intravascular catheter use and 29% with systemic infection. Twenty-one cases were identified as spontaneous renal venous thrombosis.7 In our study, portal vein (63%) was the most common VTE site, followed by the lower extremity (12.7%), CNS (4.8%), lung (4%), vena cava (1.8%), and renal vein (1.6%), among children aged < 1 year. The high incidence of portal vein thrombosis in the neonatal period could be attributed to intravascular catheter use and NICU admission due to prematurity. Amankwah et al.23 reported that the annual incidence of hospital-associated (HA) VTE was 1.4 cases per 1,000 NICU admissions. Mechanical ventilation, CVC, infection, major surgery, and length of stay of > 15 days were associated with HA-VTE.
The location of VTE varies with age, and the frequency of portal vein thrombosis is significantly reduced after 1 year of age. The incidence rate of CNS, renal vein, and vena cava thrombosis decreases with age, whereas that of lung and extremity thrombosis increases with age (Table 2).
In a United States study, cardiovascular disease was the most common complex chronic condition (18.4%), followed by malignancies (15.7%) and neuromuscular disease (9.9%).3 In our study, infection was the most common comorbidity (11.2%), followed by malignancies (7.6%), diabetes mellitus (4.4%), and congenital heart disease. The discrepancy in these findings could be due to differences in race, the incidence of VTE, and medical procedures.
TE is a major cause of morbidity and mortality in adult patients with cancer; however, data on TE in pediatric patients with cancer are insufficient. Choi et al.24 retrospectively analyzed pediatric cancer cases from six tertiary hospitals in Korea between January 2000 and July 2015. Of 3,611 pediatric patients with cancer, 33 (0.91%) had TE. Acute lymphoblastic leukemia was the most common underlying cancer, and the common risk factors were CVC use and steroid and L-asparaginase administration.
Ishola et al.25 studied the risk factors for and comorbidities of adolescent TE in a single-center study. They reported that in adolescents (age 12–21 years), 81% of patients had more than two risk factors at diagnosis. The risk factors included obesity (47%), surgery (27%), infection (27%), CVC (27%), immobility (22%), autoimmune disease (20%), and inherited thrombophilic disease (19%). Among them, obesity was the most notable risk factor and comorbidity, which is attributed with hypertension, diabetes, and coronary artery disease. Jaffray et al.26 reported on hospital-acquired pediatric VTE in a multicenter study, and the most prevalent risk factors were CVC, surgery, systemic steroid use, congenital heart disease, infection, and cancer.
This study has some limitations. Although the age at which the disease occurred was confirmed, comorbidities were not analyzed by age. We could not analyze the drugs used for VTE treatment, and because of the nature of the data, outcome or mortality due to treatment was also not evaluated.
In conclusion, although VTE is rare among children, its incidence has increased recently. This first nationwide large-data analysis study of pediatric VTE in Korea demonstrated that the VTE incidence in patients aged < 30 years is 13.11 per 100,000 persons. We also found a bimodal age distribution of VTE incidence with peaks at infancy and again after 16 years in children and adolescents. Portal vein thrombosis incidence is high in infants, and infection and malignancy are the most common comorbidities in patients with VTE.
Based on this study, the risk factors of pediatric VTE patients can be identified and used as basic data in the prevention and prophylaxis guidelines for pediatric adolescents and young adults.
Footnotes
Funding: This work was supported by the 2016 Yeungnam University Research Grant.
Disclosure: The authors have no potential conflict of interest to disclose.
- Conceptualization: Lee JM, Park ES, Choi HS, Lee KS.
- Data curation: Kim SW.
- Formal analysis: Kim SW.
- Investigation: Lee JM, Kim SW.
- Methodology: Lee JM, Kim SW, Park ES, Choi HS, Lee KS.
- Resources: Lee JM, Park ES, Choi HS, Lee KS.
- Software: Kim SW.
- Supervision: Lee JM, Lee KS.
- Validation: Lee JM.
- Writing - original draft: Lee JM.
- Writing - review & editing: Lee JM, Park ES, Choi HS.
References
- 1.Nowak-Göttl U, Janssen V, Manner D, Kenet G. Venous thromboembolism in neonates and children--update 2013. Thromb Res. 2013;131 Suppl 1:S39–S41. doi: 10.1016/S0049-3848(13)70019-7. [DOI] [PubMed] [Google Scholar]
- 2.Chalmers E, Ganesen V, Liesner R, Maroo S, Nokes T, Saunders D, et al. Guideline on the investigation, management and prevention of venous thrombosis in children. Br J Haematol. 2011;154(2):196–207. doi: 10.1111/j.1365-2141.2010.08543.x. [DOI] [PubMed] [Google Scholar]
- 3.Setty BA, O'Brien SH, Kerlin BA. Pediatric venous thromboembolism in the United States: a tertiary care complication of chronic diseases. Pediatr Blood Cancer. 2012;59(2):258–264. doi: 10.1002/pbc.23388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Raffini L, Huang YS, Witmer C, Feudtner C. Dramatic increase in venous thromboembolism in children's hospitals in the United States from 2001 to 2007. Pediatrics. 2009;124(4):1001–1008. doi: 10.1542/peds.2009-0768. [DOI] [PubMed] [Google Scholar]
- 5.van Ommen CH, Heijboer H, Büller HR, Hirasing RA, Heijmans HS, Peters M. Venous thromboembolism in childhood: a prospective two-year registry in The Netherlands. J Pediatr. 2001;139(5):676–681. doi: 10.1067/mpd.2001.118192. [DOI] [PubMed] [Google Scholar]
- 6.Andrew M, David M, Adams M, Ali K, Anderson R, Barnard D, et al. Venous thromboembolic complications (VTE) in children: first analyses of the Canadian Registry of VTE. Blood. 1994;83(5):1251–1257. [PubMed] [Google Scholar]
- 7.Schmidt B, Andrew M. Neonatal thrombosis: report of a prospective Canadian and international registry. Pediatrics. 1995;96(5 Pt 1):939–943. [PubMed] [Google Scholar]
- 8.Sandoval JA, Sheehan MP, Stonerock CE, Shafique S, Rescorla FJ, Dalsing MC. Incidence, risk factors, and treatment patterns for deep venous thrombosis in hospitalized children: an increasing population at risk. J Vasc Surg. 2008;47(4):837–843. doi: 10.1016/j.jvs.2007.11.054. [DOI] [PubMed] [Google Scholar]
- 9.Chopra V, Anand S, Hickner A, Buist M, Rogers MA, Saint S, et al. Risk of venous thromboembolism associated with peripherally inserted central catheters: a systematic review and meta-analysis. Lancet. 2013;382(9889):311–325. doi: 10.1016/S0140-6736(13)60592-9. [DOI] [PubMed] [Google Scholar]
- 10.Athale U, Siciliano S, Thabane L, Pai N, Cox S, Lathia A, et al. Epidemiology and clinical risk factors predisposing to thromboembolism in children with cancer. Pediatr Blood Cancer. 2008;51(6):792–797. doi: 10.1002/pbc.21734. [DOI] [PubMed] [Google Scholar]
- 11.Kim L, Kim JA, Kim S. A guide for the utilization of Health Insurance Review and Assessment Service National Patient Samples. Epidemiol Health. 2014;36:e2014008. doi: 10.4178/epih/e2014008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim DS. Special issue on the national health care system of South Korea. Soc Work Public Health. 2010;25(2):125–126. doi: 10.1080/19371911003648275. [DOI] [PubMed] [Google Scholar]
- 13.Kim DS. Introduction: health of the health care system in Korea. Soc Work Public Health. 2010;25(2):127–141. doi: 10.1080/19371910903070333. [DOI] [PubMed] [Google Scholar]
- 14.Young G. Anticoagulants in children and adolescents. Hematology (Am Soc Hematol Educ Program) 2015;2015(1):111–116. doi: 10.1182/asheducation-2015.1.111. [DOI] [PubMed] [Google Scholar]
- 15.Monagle P, Cuello CA, Augustine C, Bonduel M, Brandão LR, Capman T, et al. American Society of Hematology 2018 Guidelines for management of venous thromboembolism: treatment of pediatric venous thromboembolism. Blood Adv. 2018;2(22):3292–3316. doi: 10.1182/bloodadvances.2018024786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mahajerin A, Croteau SE. Epidemiology and risk assessment of pediatric venous thromboembolism. Front Pediatr. 2017;5:68. doi: 10.3389/fped.2017.00068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lipay NV, Zmitrovich AI, Aleinikova OV. Epidemiology of venous thromboembolism in children with malignant diseases: a single-center study of the Belarusian Center for Pediatric Oncology and Hematology. Thromb Res. 2011;128(2):130–134. doi: 10.1016/j.thromres.2011.03.014. [DOI] [PubMed] [Google Scholar]
- 18.Sabapathy CA, Djouonang TN, Kahn SR, Platt RW, Tagalakis V. Incidence trends and mortality from childhood venous thromboembolism: a population-based cohort study. J Pediatr. 2016;172:175–180.e1. doi: 10.1016/j.jpeds.2016.02.017. [DOI] [PubMed] [Google Scholar]
- 19.Kerlin BA, Stephens JA, Hogan MJ, Smoyer WE, O'Brien SH. Development of a pediatric-specific clinical probability tool for diagnosis of venous thromboembolism: a feasibility study. Pediatr Res. 2015;77(3):463–471. doi: 10.1038/pr.2014.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hong J, Lee JH, Yhim HY, Choi WI, Bang SM, Lee H, et al. Incidence of venous thromboembolism in Korea from 2009 to 2013. PLoS One. 2018;13(1):e0191897. doi: 10.1371/journal.pone.0191897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee LH, Gallus A, Jindal R, Wang C, Wu CC. Incidence of venous thromboembolism in Asian populations: a systematic review. Thromb Haemost. 2017;117(12):2243–2260. doi: 10.1160/TH17-02-0134. [DOI] [PubMed] [Google Scholar]
- 22.Lee S, Youn JH, Lim JY, Cheuh HW, Lee JM, Suh JK, et al. Childhood venous thromboembolism in Yeungnam region in Korea: multicenter study. Clin Pediatr Hematol Oncol. 2018;25(1):43–49. [Google Scholar]
- 23.Amankwah EK, Atchison CM, Arlikar S, Ayala I, Barrett L, Branchford BR, et al. Risk factors for hospital-sssociated venous thromboembolism in the neonatal intensive care unit. Thromb Res. 2014;134(2):305–309. doi: 10.1016/j.thromres.2014.05.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Choi HS, Kim HJ, Kang HJ, Lee JW, Shin HY, Park HJ, et al. Thromboembolism in children with cancer: a retrospective multicenter study in Korea. J Thromb Thrombolysis. 2019;47(4):558–565. doi: 10.1007/s11239-019-01808-x. [DOI] [PubMed] [Google Scholar]
- 25.Ishola T, Kirk SE, Guffey D, Voigt K, Shah MD, Srivaths L. Risk factors and co-morbidities in adolescent thromboembolism are different than those in younger children. Thromb Res. 2016;141:178–182. doi: 10.1016/j.thromres.2016.03.021. [DOI] [PubMed] [Google Scholar]
- 26.Jaffray J, Mahajerin A, Young G, Goldenberg N, Ji L, Sposto R, et al. A multi-institutional registry of pediatric hospital-acquired thrombosis cases: The Children's Hospital-Acquired Thrombosis (CHAT) project. Thromb Res. 2018;161:67–72. doi: 10.1016/j.thromres.2017.11.019. [DOI] [PubMed] [Google Scholar]