Abstract
Using updated data from the General Social Survey/National Death Index (GSS/NDI) study, we examined whether the relationship between structural stigma—measured by aggregating 4 items assessing prejudice towards homosexuality to the community level—and all-cause mortality is present among gay men/lesbian women. Our hypothesis is based on emerging evidence that indicators of structural stigma specific to homosexuality, such as those used in the GSS/NDI, uniquely predict health outcomes among this group. Because the GSS/NDI lacked an identity-based measure of sexual orientation, we tested our hypothesis by employing a strategy that has a relatively high degree of sensitivity and specificity for ascertaining individuals most likely to identify as gay or lesbian: restricting analyses to individuals who reported same-sex sexual partners in the past year. We compared this approach against an alternative strategy, which has weaker specificity for identifying gay men/lesbian women: restricting analyses to individuals who reported any lifetime same-sex sexual behaviors. After controlling for 6 individual-level factors and fixed effects of survey year, structural stigma was associated with mortality among individuals who reported past-year same-sex sexual partners (HR=1.95, 95% CI: 1.14, 3.31). Further, there was a dose-response relationship with mortality in this group, such that those residing in communities in the highest quartile of structural stigma had the greatest mortality risk, controlling for these same factors (HR=2.12, 95% CI: 1.03, 4.38). In sensitivity analyses, the effect size for structural stigma ranged from 1.54 to 2.30, indicating a consistent, but small-to-moderate, effect. In contrast, no association between structural stigma and mortality was observed among respondents who reported lifetime same-sex sexual partners, nor among those reporting only opposite-sex sexual partners. This analysis therefore delimits potential boundary conditions of the association between structural stigma related to same-sex sexuality and all-cause mortality, highlighting the conditions under which this association is (and is not) observed.
Keywords: stigma, prejudice, mortality, sexual minorities, USA
Stigma transpires when labeling, stereotyping, status loss, and discrimination co-occur within a context of unequal power (Link & Phelan, 2001). Over the last several years, scholars have argued that adopting a multi-level approach could offer important new insights into stigma processes, mechanisms, and outcomes (Major, Dovidio, & Link, 2017; Richman & Hatzenbuehler, 2014). This recognition is rooted in theoretical conceptualizations, which posit that stigma operates across multiple levels—individual, interpersonal, and structural—to create vulnerability to adverse psychosocial and health outcomes (Link & Phelan, 2001; Major & O’Brien, 2005). While most research has focused on individual and interpersonal forms of stigma, recent scholarship has begun to produce evidence that structural stigma—defined as “societal-level conditions, cultural norms, and institutional policies that constrain the opportunities, resources, and wellbeing of the stigmatized” (Hatzenbuehler & Link, 2014, p.2)—is a determinant of adverse outcomes for members of stigmatized groups (for reviews, see Hatzenbuehler, 2016; Link & Hatzenbuehler, 2016).
This research has tended to operationalize structural stigma through two measurement approaches: (1) institutional policies that intentionally restrict the opportunities of, or yield unintended consequences for, stigmatized individuals (e.g., Burris, 2006; Corrigan et al., 2005); and (2) dominant cultural norms regarding whether certain identities/statuses—such as race (Bonilla-Silva, 1997), mental illness (Corrigan, Morris, Michaels, Rafacz, & Rusch, 2012), and sexual orientation (Herek, 2007)—are socially devalued. When individual attitudes are aggregated to the community level, they become part of the social structure in that they both mirror and shape institutional policies and practices. While several studies have documented associations between community-level attitudes and mortality risk among racial/ethnic minorities (e.g., Chae et al., 2015; Lee, Muennig, Kawachi, & Hatzenbuehler, 2015; Leitner, Hehman, Ayduk, & Mendoza-Denton, 2016; Morey, Gee, Muennig, & Hatzenbuehler, 2018), only one, to our knowledge, has examined this relationship among sexual minorities (Hatzenbuehler et al., 2014). Following a failure to replicate this study (Regnerus, 2017), Hatzenbuehler and colleagues (2017) published a corrigendum, which reported a coding error that they discovered in their 2014 paper; once this error was corrected, there was no longer an association between structural stigma and mortality risk among the full sample of sexual minorities.
However, the analysis by Hatzenbuehler et al. (2014; 2017) combined both behaviorally bisexual and behaviorally homosexual respondents, despite a growing body of evidence indicating the importance of separating these two groups in studies of sexual minority health because these groups have different health profiles and health determinants (e.g., Bostwick, Boyd, Hughes, & McCabe, 2010; Dodge & Sandfort, 2007; Hatzenbuehler & Keyes, 2013; Hsieh & Ruther, 2016; Molina et al., 2015; Schrimshaw, Siegel, Downing, & Parsons, 2013; Ross, Dobinson, & Eady, 2010; Ross et al., 2018). This research suggests that Hatzenbuehler and colleagues’ (2014; 2017) approach of combining these two subgroups of sexual minorities may have obscured differential relationships between community-level prejudice and mortality risk if this association were present for one group but not the other.
Our paper explores this possibility. To develop our hypothesis and analytic approach, we draw on structural stigma theory, which posits specific effects of structural stigma on specific groups (Hatzenbuehler, 2016). That is, rather than utilizing a global structural stigma predictor that applies across all groups, researchers develop specific indicators of structural stigma, including aggregate measures of community-level prejudicial attitudes, that are relevant to particular stigmatized groups. This approach is consistent with social identity threat theories of stigma, which posit that stigma-induced identity threat, and the concomitant biopsychosocial responses, should only occur in contexts where a stressor that is relevant to one’s stigmatized social identity can be appraised as harmful (Major & O’Brien, 2005). Thus, studies have examined, for example, whether stigmatizing public attitudes towards people with psychological or emotional problems affect experiences of discrimination among individuals with mental illness (e.g., Evans-Lacko, Brohan, Mojtabi, & Thornicroft, 2012); whether community norms about suppression of AIDS-related prejudice contribute to perceptions of stigma among HIV-infected individuals (e.g., Miller, Grover, Bunn, & Solomon, 2011); and whether the anti-Muslim climate after 9/11 shaped birth outcomes among Arab-American women (Lauderdale, 2006). By and large, these studies find that these specific indicators of community-level prejudice uniquely influence outcomes among the stigmatized group exposed to these attitudinal contexts.
Prejudice related to bisexuality involves different stereotypic content than prejudice related to homosexuality, indicating that these are distinct constructs (Dodge, Herbenick, Friedman, et al., 2016; Eliason, 1997; Herek, 2002; Worthen, 2013). This research, together with the aforementioned literature documenting specific effects of community-level prejudice on specific stigmatized groups (e.g., Evans-Lacko et al., 2012; Miller et al., 2011), suggests that it is necessary to utilize different indicators of community-level prejudice for bisexual individuals than for gay men and lesbian women. However, the General Social Survey (GSS), which was used for the current paper, only included items that repeatedly assessed prejudice related to homosexuality. Importantly, recent research suggests that such indicators of community-level prejudice that are specific to exclusive same-sex sexuality uniquely predict health outcomes among gay men and lesbians. For instance, over a ten-year period in Sweden when two laws related to same-sex sexuality were passed (i.e., same-sex marriage, coverage for fertility treatments for lesbians) and when prejudicial attitudes towards homosexuality declined, psychological distress significantly decreased for gay men and lesbians but not for bisexual individuals (Hatzenbuehler, Branstrom, & Pachankis, 2018).
Based on the theory and empirical evidence reviewed above, we hypothesized that community-level prejudice related to homosexuality would increase mortality risk among gay men and lesbian women. Because the GSS/NDI study lacked an identity-based measure of sexual orientation, we tested our hypothesis by employing an established strategy, described below, that prior research indicates has a relatively high degree of sensitivity and specificity for ascertaining individuals most likely to identify as gay men or lesbian women (e.g., Dodge, Herbenick, Fu, et al., 2016). We used this strategy to examine whether community-level prejudice related to homosexuality is associated with mortality risk among this group. We compared this to the approach used by Hatzenbuehler et al. (2014; 2017), which had weaker specificity for identifying gay men/lesbian women, to better understand whether the null finding reported in that earlier study was attributable to insufficiently identifying the target population of gay men/lesbian women, the stigmatized group for whom this form of prejudice is thought to influence mortality risk. Further, we tested whether community-level prejudice related to homosexuality does not increase mortality risk among the non-stigmatized group (i.e., behaviorally heterosexual respondents). Such an analysis is considered a negative control approach (Lipsitch, Tchetgen, & Cohen, 2010), in that we test whether there is an association among a group where we would not theoretically expect it.
Methods
Data Sources
Our data come from the General Social Survey/National Death Index (GSS-NDI) study, in which participants from the General Social Survey (GSS) are linked prospectively to mortality data, obtained from the National Death Index (NDI). The GSS is a nationally representative sample of the U.S. non-institutionalized English-speaking population aged 18 and over. More details on the GSS/NDI study, including the linkage methodology, can be obtained elsewhere (Muennig, Johnson, Kim, Smith, & Rosen, 2011). Our analysis uses recently released data from 14 waves of GSS data from 1988–2010 linked to NDI data through 2014.
Measures
Classification of Sexual Minorities
As mentioned above, we hypothesized that the relationship between structural stigma and mortality risk would be present for gay men and lesbian women. Because the GSS/NDI did not include a measure of sexual identity until 2008, we employed an evidence-based approach that enabled us to use the behavioral indices of sexual orientation that were available in the GSS/NDI dataset to ascertain individuals most likely to identify as gay men/lesbian women: restricting analyses to individuals who reported same-sex sexual partners in the past year.
Support for our approach comes from two data sources. First, recently published data from the National Survey of Sexual Health and Behavior (NSSHB), a nationally representative survey of U.S. adults, indicated that respondents who report past-year same-sex sexual behaviors are more likely to identify as homosexual/gay than as bisexual. For example, among sexually active male respondents, 100% of men who identified as homosexual/gay had a same-sex sexual partner in the past 12 months, compared to only 63.6% of sexually-active bisexual men (Dodge, Herbenick, Fu, et al., 2016). Similar patterns were obtained for women: among sexually active respondents, 100% of women who identified as homosexual/lesbian had a same-sex sexual partner in the past 12 months, compared to only 27.7% of sexually-active bisexual women (Herbenick et al., 2018).
The second data source providing support for our approach comes from the 2008–2016 GSS (which was not linked to the NDI). Sensitivity/specificity analyses with these data (obtained from NORC at the University of Chicago, available at https://gssdataexplorer.norc.org/; analyses conducted using SAS 9.4) indicated that among sexually active GSS respondents, 96.9% of women and 96.2% of men who identified as gay/lesbian/homosexual reported any same-sex sexual behaviors in the past year. In contrast, only 65.4% of bisexual men and 40.5% of bisexual women reported any past-year same-sex sexual behaviors; this difference was statistically significant (, p<0.0001 for men; , p < 0.0001 for women). Further, restricting analyses to those with past-year same-sex sexual partners afforded 96.5% sensitivity for accurately identifying those who identified as gay/lesbian and 97.8% specificity for correctly identifying those who did not. These results provide further evidence that restricting analyses to individuals who reported same-sex sexual partners in the past year would enable us to correctly classify, with a relatively high degree of sensitivity and specificity, individuals most likely to identify as gay/lesbian. Sensitivity analyses that used an alternative approach for classifying this group (i.e., restricting analyses to those who reported exclusive same-sex partners in the past year) produced similar results to those reported below; see Supplemental Appendix (eTable 1).
Thus, based on the existing literature (e.g., Dodge, Herbenick, Fu, et al., 2016) and on these analyses from the 2008–2016 GSS sample, we examined the association between structural stigma and mortality risk among sexual minorities who reported any same-sex sexual behaviors in the past year (for the sake of brevity, we call this group “past-year sexual minorities”). We compared the association in this group to the association among sexual minorities who reported any lifetime same-sex sexual behaviors (for the sake of brevity, we call this group “lifetime sexual minorities”). This was the analytic sample used in the paper by Hatzenbuehler and colleagues (2014; 2017), which did not differentiate among subgroups of sexual minorities.
Measurement of sexual orientation
As described above, classification of sexual minority status was based on a behavioral measure of sexual orientation. Since 1988, respondents were asked the gender of their sexual partners over three time frames: past 12 months, past 5 years, and lifetime (since age 18).
For questions about past-year sexual experiences, respondents were asked, “Have your sex partners in the last 12 months been a) exclusively male, b) both male and female, c) exclusively female?” Men who responded “exclusively male” or “both male and female” were categorized as “past-year sexual minorities”; men who responded “exclusively female” were categorized as “past-year heterosexuals.” Similarly, women who responded “exclusively female” or “both male and female” were categorized as “past-year sexual minorities”; women who responded “exclusively male” were categorized as “past-year heterosexuals.” Respondents who said they did not know, the question was not applicable, or refused to answer were excluded.
For lifetime sexual experiences, we used a measure composed of several questions, consistent with the approach used by Hatzenbuehler et al. (2014; 2017). The first measured past-year sexual behavior, described above. The next asked, “Have your sex partners in the last five years been a) exclusively male, b) both male and female, c) exclusively female?” For this measure, respondents were categorized using the same criteria as above. The final two questions asked, “Now thinking about the time since your 18th birthday (including the past 12 months), how many female partners have you had sex with?” and “how many male partners have you had sex with?” The response option was open-ended; thus, while the vast majority of respondents provided a number for both of these questions, a small number (N=37) gave a qualitative answer (i.e., “some,” “more than one,” “several,” and “many/lots”). Respondents who reported a non-zero number of same-sex partners, as well as those who quantified the number of same-sex sex partners as “some,” “more than one,” “several,” or “many/lots,” were categorized as “lifetime sexual minorities.” Respondents who endorsed zero same-sex partners but at least one (or “some,” “more than one,” “several,” “many/lots”) opposite-sex partner across all three measures of sexual behavior were categorized as “lifetime heterosexuals.” Respondents who refused to answer, said they did not know, or replied with “garbled text,” a “dash or slash,” or an “X” were considered missing for this measure.
Of the 32,251 respondents assessed between 1988 and 2010, there were 1,524 (4.7%) sexual minorities who reported any same-sex behaviors across any of the three time frames. Among these, 629 (2.0%) reported any past-year same sex behaviors; these were the individuals most likely to identify as gay men/lesbian women, our subgroup of interest. Table 1 presents the demographic characteristics of the 1988–2014 GSS/NDI sample, stratified by sexual orientation groups.
Table 1.
Sample Demographics of the General Social Survey/National Death Index Study Respondents, by Sexual Behavior (1988–2014).
| Variable | Respondents with Any Same-Sex Sexual Partners in the Past Year (N=629) | Respondents with Any Same-Sex Sexual Partners in Their Lifetime (N=1,524) | Respondents with Only Opposite-Sex Sexual Partners in the Past Year (N=19,638) |
|---|---|---|---|
| Respondent Died by 2014 | 86 (13.7%) | 235 (15.4%) | 3,098 (15.8%) |
| Race | |||
| White | 492 (78.2%) | 1184 (77.7%) | 15,870 (80.8%) |
| Black | 93 (14.8 %) | 228 (15.0%) | 2,529 (12.9%) |
| Other Race | 44 (7.0%) | 112 (7.3%) | 1,239 (6.3%) |
| Sex | |||
| Male | 338 (53.7%) | 763 (50.1%) | 9,202 (46.9%) |
| Female | 291 (46.3%) | 761 (49.9%) | 10,436 (53.1%) |
| Age at Interview (years) | 38.8 (12.6) | 41.8 (15.0) | 41.7 (14.5) |
| Nativity | |||
| Immigrant | 59 (9.4%) | 153 (10.0%) | 1,637 (8.3%) |
| Born in US | 568 (90.3%) | 1368 (89.8%) | 17,940 (91.4%) |
| Socioeconomic Indicators | |||
| Income (ln) | 10.3 (1.0) | 10.2 (1.1) | 10.5 (1.0) |
| Years of Education | 14.1 (2.8) | 13.6 (3.0) | 13.5 (2.8) |
Structural stigma
In this analysis, structural stigma related to same-sex sexuality was operationalized as community-level prejudice related to homosexuality (for the sake of brevity, we hereafter to this measure as “structural stigma”). To create this measure, we used the four items of respondents’ attitudes towards homosexuality that had been repeatedly assessed in the GSS: (1) “If some people in your community suggested that a book in favor of homosexuality should be taken out of your public library, would you favor removing this book, or not?” (2) “Should a man who admits that he is a homosexual be allowed to teach in a college or university, or not?” (3) “Suppose a man who admits that he is a homosexual wanted to make a speech in your community. Should he be allowed to speak, or not?” (4) “Do you think that sexual relations between two adults of the same sex is always wrong, almost always wrong, wrong only sometimes, or not wrong at all?” Given that three of the four items had dichotomous response options, each was dichotomized such that a value of 1 indicated the presence of structural stigma (the last item was dichotomized at “not wrong at all” (0) vs. all other responses (1)). The Cronbach’s alpha for the four items was 0.86, indicating good reliability. We then combined the four items into a single summed value that was aggregated at the community level. In the GSS, the community level is defined as the “primary sampling unit” (PSU), composed of either metropolitan statistical areas (MSAs) or non-metropolitan counties that serve as an indicator of “life space” where individuals live, work, and play (Gibson, 1995). There were 263 PSUs in the GSS from 1988–2010 (the number of individuals sampled within any PSU ranged from 8 to 910, with a median of 115).
There are at least two possible ways to create the structural stigma score. One is to calculate structural stigma within a given year, which would enable us to capture exposure to structural stigma during the particular year in which the sexual minority respondent was surveyed. However, this approach was not possible with these data because not every PSU was sampled with the same number of respondents every wave. This sampling approach resulted in very small sample sizes within PSUs during some years, which precluded our ability to create reliable estimates of structural stigma for those years.
Thus, we chose an alternative approach to creating the structural stigma score, which involved pooling the four items across the years of observation in order to calculate one average structural stigma score for each PSU. This approach could potentially introduce some misclassification in the assigned structural stigma score if there were substantial changes in prejudice over the 22 years of the study. However, the GSS routinely updated the PSU codes every 10 years, resulting in no single PSU being consistently represented across the entire 22 years of study duration. Consequently, respondents’ prejudice values were only grouped by 4- to 10-year periods (the median length of observation for each PSU was 5 survey waves (range: 4–6 waves), or 7 years (range: 4–10 years)). As such, given how the PSUs were sampled in the GSS, the structural stigma values were unlikely to be systematically affected by any changes in community-level prejudice related to homosexuality that occurred over the study period with our pooled approach.
We operationalized structural stigma in two ways. First, we used a continuous measure of structural stigma, which uses the full range of variation in the structural stigma variable, increases statistical power, and eliminates the arbitrariness of different cut-points (e.g., median split). Second, we examined structural stigma as a four-level ordered categorical variable defined at the within-sample quartiles, in order to assess the potential for dose-response.
The four items comprising the structural stigma measure were missing for over one-third of the sample due to a planned missing design (i.e., individuals in the survey were randomized to receive different questions in order to maximize the breadth of item coverage while reducing respondent burden). We therefore conducted a complete cases analysis, where only individuals who received and answered all 4 items (N=16,633) were used to create the structural stigma score. A complete cases analysis should produce an estimate of the relationship between structural stigma and mortality risk that is minimally affected by systematic bias, given the planned missing design (we assume missingness is completely at random (Little, Jorgensen, Lang, & Moore, 2014; Rhemtulla & Little, 2012)). We also present the results using multiple imputation for the structural stigma variable as a sensitivity analysis, which produced similar findings (see Supplemental Appendix Section 3 for a description of the imputations and eTable 5 for the imputation results).
All-Cause Mortality
Information on all-cause mortality was obtained from the NDI, as described above. Respondents who had died by 2014 were coded as a 1, and those who survived the study period were coded as a 0 (censored). For the deceased, we created our time variable by subtracting the year of interview from the year of death, which represents the number of years lived by each respondent following the interview. For those who were still alive in 2014, we subtracted year of interview from 2014, which represents the number of years between the time a respondent was interviewed and the end of follow-up.
Covariates
We controlled for established individual-level risk factors for mortality, including: respondent racial/ethnic identification (White vs. Black vs. Other); sex (male or female); age at interview (continuous); nativity status (indicating whether the respondent was born outside the United States); household income (natural log, given the skewed distribution of the variable); and individual educational attainment (respondents’ number of years of formal education). We additionally controlled for fixed effects of survey year to account for differential time-to-follow-up between sexual minorities in communities with high vs. low levels of structural stigma (i.e., past-year sexual minorities in communities with high levels of structural stigma had significantly longer follow-up times than those in communities with low levels of structural stigma).
In addition to individual-level covariates, we controlled for three PSU-level factors. PSU-level education and income were measured by averaging respondents’ education level and income (natural log of income, as described above) to the PSU level. PSU-level conservativism was estimated by calculating the proportion of respondents who endorsed conservative political viewpoints (self-identified as “slightly conservative,” “conservative,” or “extremely conservative”) within the PSU. Structural stigma was strongly correlated with PSU-level education (r = −0.78) and PSU-level income (r = −0.53) and moderately correlated with PSU-level conservatism (r = 0.35), suggesting the potential for some multicollinearity. Given these concerns, we examined model fit (Akaike information criterion) with and without these additional PSU-level factors. These analyses indicated that the inclusion of the PSU-level factors provided no improvement in model fit to the data as compared to the models that only controlled for the individual-level covariates. Nevertheless, we decided to retain these PSU-level covariates to determine whether the magnitude of the association between structural stigma and mortality risk was substantially attenuated after control for these variables.
Mediator
Recent evidence indicates that community-level prejudice is associated with poor self-rated health (SRH) among sexual minorities (Hatzenbuehler, Flores, & Gates, 2017); in turn, SRH status differentiates heightened mortality risk (Idler & Benyamini, 1997). This research suggests that health, as measured by SRH, represents a potential mechanism linking structural stigma to mortality risk. Thus, we would expect that the magnitude of the association between the independent (structural stigma) and dependent (mortality) variable would be attenuated after adjusting for the mediator (SRH). SRH was examined as a dichotomous variable (fair/poor vs. good/excellent).
Statistical Analysis
We first conducted tests of the assumptions for proportional hazards, such as visualization of the log-log survival curves and inclusion of a structural stigma by log (time) interaction term in the model. Both tests revealed that the assumptions for proportional hazards were met.
Our primary hypothesis involved examining the association between structural stigma and mortality risk among those most likely to identify as gay men/lesbian women, i.e., respondents who reported any same-sex sexual behaviors in the past year. We compared the association in this group to the association among respondents who reported any lifetime same-sex sexual behaviors, the group examined by Hatzenbuehler and colleagues (2014; 2017). We next explored whether the association between structural stigma and mortality risk differed as a function of sexual orientation (i.e., past-year sexual minority vs. past-year heterosexual). To test this, we conducted an interaction between sexual orientation and structural stigma in the full sample, controlling for individual-level confounders and survey year. We further probed the interaction by stratifying the models by sexual orientation, comparing past-year sexual minorities to past-year heterosexuals.
The code for this paper is provided in the Supplemental Appendix. All analyses were conducted in R and were weighted to adjust for the complex sampling design. Because not every PSU was sampled every year (see above), PSUs with no data for certain survey waves were centered so as not to contribute to the overall variance in exposure. The spatial clustering of mortality deaths within PSUs was accounted for with the design variables rather than with a random effects (multi-level) model, as we were interested in population average effects rather than estimating between-PSU variance (Hubbard, Ahern, Fleischer, et al., 2010).
Results
Among sexual minorities with same-sex sexual partners in the past year, there were 86 (13.7%) deaths, compared to 235 (15.4%) deaths among sexual minorities with lifetime same-sex sexual partners.
Structural stigma and mortality risk among sexual minorities who reported past-year same-sex behaviors (i.e., “past-year sexual minorities”)
Among the 629 sexual minorities who reported same-sex behaviors in the last year at time of interview, structural stigma was associated with mortality risk in the model only adjusted for survey year (Model 1: HR=2.30, 95% CI: 1.45, 3.65; Table 2). Figure 1 depicts the Kaplan-Meier curves of survival time by structural stigma for this group. Structural stigma remained associated with mortality risk in the model controlling for established demographic risk factors for mortality—including age at interview, race, sex, and nativity status (Model 2: HR=1.79, 95% CI: 1.12, 2.87)—and in the model additionally controlling for the indicators of socioeconomic status, including household income and years of education (Model 3: HR=1.95, 95% CI: 1.14, 3.31). In the fourth final model controlling for the mediator (SRH), there was a reduction in the main effect Hazard Ratio from 1.95 to 1.68 (95% CI: 0.94, 3.01); however, the individual pathway from structural stigma to SRH was not statistically significant (AOR=0.63, 95% CI: 0.32, 1.22).
Table 2.
Cox Proportional Hazard Models Predicting Hazards of Death for Sexual Minorities Who Reported Any Same-Sex Sexual Partners in the Past 12 Months (N=629).
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | |
| Structural stigma | 2.30 (1.45, 3.65) | 1.79 (1.12, 2.87) | 1.95 (1.14, 3.31) | 1.68 (0.94, 3.01) |
| Year | 0.97 (0.91, 1.02) | 0.98 (0.93, 1.03) | 0.98 (0.93, 1.03) | 0.95 (0.90, 1.01) |
| Age at Interview | 1.05 (1.03, 1.07) | 1.04 (1.02, 1.07) | 1.05 (1.02, 1.08) | |
| Black | 1.21 (0.65, 2.28) | 1.27 (0.68, 2.36) | 1.03 (0.47, 2.27) | |
| Other Race | 2.65 (1.07, 6.55) | 2.48 (0.89, 6.85) | 3.23 (0.85, 12.21) | |
| Female | 0.39 (0.21, 0.70) | 0.41 (0.22, 0.76) | 0.41 (0.19, 0.87) | |
| Not US Born | 0.68 (0.27, 1.70) | 0.67 (0.24, 1.89) | 0.40 (0.08, 2.00) | |
| Household Income (log transformed) | 1.01 (0.73, 1.39) | 1.03 (0.71, 1.50) | ||
| Years of Education | 1.01 (0.93, 1.10) | 1.00 (0.91, 1.10) | ||
| Fair/Poor SelfRated Heath | 2.23 (1.10, 4.49) |
Notes. HR = Hazard Ratio. CI = Confidence Interval. Structural stigma was examined as a continuous variable, using the complete cases dataset. White is the reference category for the race variables.
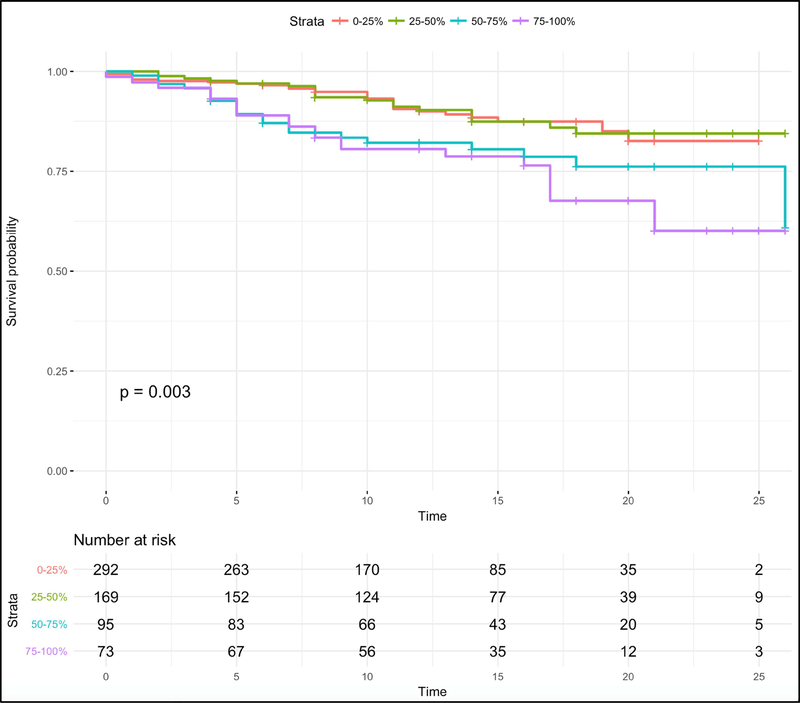
Figure 1.
Survival Time among Sexual Minorities Who Reported Any Same-Sex Sexual Partners in the Past 12 Months (N=629) by Quartile of Exposure to Structural Stigma.
When we examined the Hazard Ratios for structural stigma within each quartile, we found an ordered, dose-response relationship with mortality risk among the past-year sexual minority group (eTable 2, Supplemental Appendix). That is, compared to the lowest quartile, the largest HR for structural stigma was in the highest quartile (HR=2.12, 95% CI: 1.03, 4.38) and the smallest was in the second-to-lowest quartile (HR=1.00, 95% CI: 0.50, 1.99).
In models additionally controlling for PSU-level covariates (Table 3), structural stigma remained associated with mortality risk among past-year sexual minorities when controlling for PSU-level education (Model 5: HR=1.87, 95% CI: 0.84, 4.17), PSU-level income (Model 6: HR=1.54, 95% CI: 0.85, 2.79), and PSU-level conservatism (Model 7: HR=2.07, 95% CI: 1.19, 3.62), although the confidence intervals reflected increased imprecision when PSU-level education and income were added. While the coefficient for structural stigma was reduced with the inclusion of the PSU-level variables, the magnitude of the HRs for structural stigma in models that adjusted for the PSU-level variables (range: HR=1.54 to 2.07) was quite similar to the models that only adjusted for the individual-level covariates (range: HR=1.79 to 2.30). This suggests that, while the other PSU-level variables may partially confound or be mediated by the relationship between structural stigma and mortality, they do not fully explain the relationship.
Table 3.
Cox Proportional Hazard Models Predicting Hazards of Death for Sexual Minorities Who Reported Any Same-Sex Sexual Partners in the Past 12 Months (N=629) Controlling for Community-Level Covariates.
| Model 5 | Model 6 | Model 7 | Model 8 | |
|---|---|---|---|---|
| HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | |
| Structural stigma | 1.87 (0.84, 4.17) | 1.54 (0.85, 2.79) | 2.07 (1.19, 3.62) | 1.74 (0.73, 4.14) |
| Year | 0.98 (0.93, 1.03) | 0.98 (0.93, 1.03) | 0.98 (0.92, 1.03) | 0.98 (0.92, 1.03) |
| Age at Interview | 1.04 (1.02, 1.06) | 1.04 (1.02, 1.07) | 1.04 (1.02, 1.06) | 1.04 (1.02, 1.07) |
| Black | 1.27 (0.68, 2.36) | 1.35 (0.73, 2.49) | 1.25 (0.67, 2.33) | 1.34 (0.73, 2.46) |
| Other Race | 2.45 (0.88, 6.86) | 2.47 (0.92, 6.60) | 2.44 (0.88, 6.80) | 2.50 (0.92, 6.85) |
| Female | 0.41 (0.22, 0.77) | 0.40 (0.22, 0.75) | 0.41 (0.22, 0.76) | 0.40 (0.22, 0.75) |
| Not US Born | 0.68 (0.24, 1.93) | 0.73 (0.26, 2.01) | 0.67 (0.24, 1.87) | 0.72 (0.26, 2.01) |
| Household Income (log transformed) | 1.01 (0.73, 1.39) | 1.03 (0.74, 1.41) | 1.01 (0.73, 1.39) | 1.03 (0.75, 1.41) |
| Years of Education | 1.01 (0.93, 1.10) | 1.01 (0.93, 1.09) | 1.01 (0.93, 1.10) | 1.00 (0.93, 1.09) |
| Community-Level Covariates | ||||
| PSU Average Education | 0.97 (0.62, 1.53) | 1.07 (0.68, 1.67) | ||
| PSU Average Income (log transformed) | 0.50 (0.15, 1.62) | 0.49 (0.15, 1.64) | ||
| PSU % Conservative | 0.99 (0.95, 1.03) | 0.99 (0.95, 1.04) | ||
Notes. HR = Hazard Ratio. CI = Confidence Interval. PSU = Primary Sampling Unit. Structural stigma was examined as a continuous variable. White is the reference category for the race variables.
Structural stigma and mortality risk among sexual minorities reporting same-sex behaviors in their lifetime (i.e., “lifetime sexual minorities”)
In contrast to the results for the past-year sexual minorities, there was no relationship between structural stigma and mortality risk in any of the models (e.g., Model 3: HR=1.09, 95% CI: 0.76, 1.55) for the 1,524 sexual minorities who reported lifetime same-sex sexual partners (Table 4). Because this group included the 629 individuals who had past-year same-sex sexual behaviors, we also ran a sensitivity analysis among only the 895 individuals who reported lifetime same-sex sexual partners but no past-year same-sex sexual partners; the results were consistent among this group, with no association between structural stigma and mortality risk (e.g., Model 3: HR=0.74, 95% CI: 0.46, 1.19, eTable 3, Supplemental Appendix).
Table 4.
Cox Proportional Hazard Models Predicting Hazards of Death for Sexual Minorities Who Reported Any Same-Sex Sexual Partners in their Lifetime (N=1,524).
| Model 1 | Model 2 | Model 3 | |
|---|---|---|---|
| HR (95% CI) | HR (95% CI) | HR (95% CI) | |
| Structural stigma | 1.46 (1.10, 1.94) | 1.21 (0.87, 1.67) | 1.09 (0.76, 1.55) |
| Year | 0.99 (0.96, 1.02) | 0.99 (0.96, 1.02) | 0.99 (0.96, 1.02) |
| Age at Interview | 1.05 (1.04, 1.06) | 1.05 (1.04, 1.06) | |
| Black | 1.85 (1.29, 2.66) | 1.76 (1.15, 2.69) | |
| Other Race | 1.70 (0.87, 3.31) | 1.48 (0.74, 2.97) | |
| Female | 0.55 (0.39, 0.76) | 0.52 (0.37, 0.74) | |
| Not US Born | 0.68 (0.35, 1.33) | 0.59 (0.29, 1.23) | |
| Household Income (log transformed) | 0.99 (0.84, 1.17) | ||
| Years of Education | 0.95 (0.90, 1.00) |
Notes. HR = Hazard Ratio. CI = Confidence Interval. Structural stigma was examined as a continuous variable using the complete cases dataset. White is the reference category for the race variables.
Association between structural stigma and mortality risk by sexual orientation
To test whether the association between structural stigma and mortality risk differed as a function of sexual orientation (i.e., sexual minority vs. heterosexual), we first conducted an interaction between sexual orientation and structural stigma in the full sample, controlling for individual-level confounders and survey year (HR=1.45, 95% CI: 0.92, 2.27, p=0.11). In stratified analyses, structural stigma was associated with mortality risk among past-year sexual minorities, as shown above (Table 2). In contrast, there was no relationship between structural stigma and mortality risk among respondents reporting only opposite-sex sexual partners in the past year (i.e., “past-year heterosexuals”) in models controlling for individual-level risk factors (e.g., Model 3: HR=0.97, 95% CI: 0.89, 1.05; Table 5). These results were consistent in a sensitivity analysis among respondents reporting only opposite-sex sexual partners in their lifetime (i.e., “lifetime heterosexuals”), with no association between structural stigma and mortality risk in this group (e.g., Model 3: HR=1.00, 95% CI: 0.89, 1.11, eTable 4, Supplemental Appendix). Together, these results indicate that structural stigma increases mortality risk only for past-year sexual minorities.
Table 5.
Cox Proportional Hazard Models Predicting Hazards of Death for Respondents Who Reported Only Opposite-Sex Sexual Partners in the Past 12 Months (N=19,638).
| Model 1 | Model 2 | Model 3 | |
|---|---|---|---|
| HR (95% CI) | HR (95% CI) | HR (95% CI) | |
| Structural stigma | 1.20 (1.11, 1.30) | 1.07 (0.99, 1.16) | 0.97 (0.89, 1.05) |
| Year | 0.98 (0.97, 0.99) | 0.97 (0.96, 0.98) | 0.97 (0.96, 0.97) |
| Age at Interview | 1.06 (1.05, 1.06) | 1.06 (1.05, 1.06) | |
| Black | 1.68 (1.49, 1.89) | 1.50 (1.31, 1.71) | |
| Other Race | 1.16 (0.92, 1.46) | 1.16 (0.92, 1.46) | |
| Female | 0.68 (0.63, 0.73) | 0.66 (0.61, 0.72) | |
| Not US Born | 0.79 (0.66, 0.95) | 0.78 (0.64, 0.94) | |
| Household Income (log transformed) | 0.87 (0.83, 0.92) | ||
| Years of Education | 0.97 (0.95, 0.98) |
Notes. HR = Hazard Ratio. CI = Confidence Interval. Structural stigma was examined as a continuous variable using the complete cases dataset. White is the reference category for the race variables.
DISCUSSION
Our analysis shows that, controlling for numerous established individual-level risk factors for mortality (i.e., sex, race, age, nativity status, income, and education) as well as survey year, structural stigma was associated with mortality risk among respondents who reported same-sex sexual partners in the past year. The effect size for structural stigma in the sensitivity analyses ranged from 1.54 to 2.30, indicating a consistent, but small-to-moderate, effect. Adding other PSU-level factors minimally reduced the magnitude of the effect size for structural stigma, which may indicate some partial confounding or mediation, but does not change our interpretation of the results. The collinearity of these other PSU-level factors with structural stigma also reduced the precision of our structural stigma estimate and increased the confidence intervals.
While unmeasured confounding is always a potential issue when drawing inferences from observational data, three sets of findings improve our confidence in the inferences we draw about these relationships between structural stigma and mortality risk. First, we observed an ordered, dose-response relationship, such that past-year sexual minorities residing in communities in the highest quartile of structural stigma had the greatest mortality risk. Observation of a dose-response relationship strengthens inference, as confounding factors would be less likely to be distributed similarly across levels of the exposure of interest. Second, mortality risk was not elevated for behaviorally heterosexual respondents (i.e., those with only opposite-sex partners) who lived in communities with higher levels of structural stigma, indicating evidence of a negative control exposure (Lipsitch et al., 2010). This finding helps to rule out alternative explanations for these results, because if structural stigma were merely a proxy for other community-level factors (i.e., community-level SES), those other factors should operate similarly among both heterosexuals and sexual minorities, in contrast to the observed patterns we observed. Third, we provide evidence that our results are robust across several dimensions, including different ways of addressing missing data (complete cases, multiple imputation); different ways of classifying the past-year sexual minority group (exclusive vs. non-exclusive same-sex sexual partners); and different approaches for measuring structural stigma (continuous and four-level ordered categorical variables).
We also found an attenuation in the association between structural stigma and mortality risk among past-year sexual minorities when self-rated health (SRH) was included, consistent with a mediated pathway between structural stigma and mortality via SRH. However, this result should be interpreted with caution, for several reasons. First, we did not observe an association between structural stigma and SRH among past-year sexual minorities. Although this pathway is not required to document mediation (Hays & Rockwood, 2017), it does raise questions about how SRH is operating in these data. Second, due to the planned missing design of the GSS, SRH is highly missing (in 28% of the sample), which reduced our sample size of past-year sexual minorities by 203 respondents and the number of deaths by nearly a third, to 61 (from 86). Third, as shown in eTable 6 (Supplemental Appendix 4), the magnitude of the association between structural stigma and mortality risk among past-year sexual minorities was unchanged in models that imputed SRH. With these data, therefore, we are unable to adjudicate between the possibility that the change in magnitude of the hazard ratio for structural stigma is due to reduced power, or due to mediation. While these analyses of SRH do not affect our conclusion about a main effect relationship between structural stigma and mortality risk among past-year sexual minorities (our primary research question), they do leave open the questions of whether SRH is a mediator of this relationship, and what other pathways may underlie the association between structural stigma and mortality risk. Although this was not the focus of the current paper, it is an important direction for future research.
Prior research (e.g., Dodge, Herbenick, Fu, et al., 2016) and sensitivity/specificity analyses from the 2008–2016 GSS indicated that individuals who reported same-sex sexual partners in the past year—the subgroup of sexual minorities for whom we observed a significant association between structural stigma and mortality risk—are most likely to identify as gay men and lesbian women. Our results therefore suggest that structural stigma is associated with mortality risk among this group, consistent with recent research indicating that structural forms of stigma related to same-sex sexuality uniquely predict health outcomes among gay men/lesbians (e.g., Hatzenbuehler et al., 2018). However, in order to definitively test this hypothesis, future research is needed to replicate these findings with identity-based measures of sexual orientation, something that will become possible in future iterations of the GSS/NDI dataset. This replication will enable us to determine whether our results are stronger once we evaluate the relationship between structural stigma and mortality risk only among gay-and lesbian-identified respondents. Our measure of past-year same-sex sexual partners was relatively highly sensitive and specific in identifying gay men and lesbian women, but it included some respondents who would have identified as bisexual or heterosexual. Such misclassification introduces measurement error; however, including these respondents (i.e., those who identify as bisexual or heterosexual) would likely attenuate the effect size for structural stigma among past-year sexual minorities, thereby biasing us towards the null.
This replication would also enable us to evaluate whether there is an association between structural stigma and mortality risk among bisexually-identified respondents. Neither behavioral measure of sexual orientation that we used had particularly strong sensitivity/specificity for identifying bisexual individuals, making it difficult for us to answer this question with the GSS/NDI dataset. Specifically, the measure of past-year same-sex sexual behaviors is much less sensitive (47.5%) for identifying bisexual individuals than it is for identifying gay men and lesbians (96.5%). Further, while our measure of lifetime same-sex sexual behaviors afforded greater sensitivity (79.0%) for accurately identifying those who identified as bisexual, data from the 2008–2016 GSS indicate that only one-fifth of individuals who report lifetime same-sex sexual behaviors identify as bisexual.
In contrast to the results for past-year sexual minorities, we did not observe an association between structural stigma and mortality risk among respondents who reported lifetime same-sex sexual partners, which was the analytic group examined by Hatzenbuehler and colleagues (2014, 2017). Why did their approach fail to document an association between structural stigma and mortality risk among sexual minorities? If the relationship between structural stigma and mortality risk is apparent for gay men and lesbian women, as our analysis suggests, any approach that is less able to correctly identify (likely) gay/lesbian respondents and include them in the analytic sample would dilute an ability to detect an effect (i.e., bias one towards the null). The approach used by Hatzenbuehler and colleagues (2017)—which combined individuals who reported same-sex sexual partners in the past year with those who did not—appeared to do just that. While their approach had comparable sensitivity (97.6% vs. 96.5%) for correctly identifying those who do identify as gay/lesbian, it had weaker specificity for identifying those who do not identify as gay/lesbian (91.4% vs. 97.8%). Furthermore, Hatzenbuehler and colleagues’ (2017) approach of examining respondents with any same-sex sexual partners in their lifetime included a large number of individuals who likely identified as bisexual and heterosexual; as our analysis suggests, the inclusion of these groups would have obscured the ability to detect an association between structural stigma and mortality risk among a gay- and lesbian-identified sample. Consequently, even though examining past-year sexual minorities resulted in a smaller sample size (nearly a third smaller than the sample size in Hatzenbuehler and colleagues’ (2014; 2017) analysis of the full sample of sexual minorities), we were able to detect an association between structural stigma and mortality risk because of the greater specificity afforded by restricting the analytic sample to respondents most likely to identify as gay/lesbian (i.e., those who reported past-year same-sex behaviors). The Supplemental Appendix (Section 5) provides a detailed description of other differences between the two papers, and describes which differences, if any, could have contributed to the divergent findings. In sum, the main contribution of the current paper is that it delimits potential boundary characteristics of the association between structural stigma related to same-sex sexuality and mortality risk, highlighting the conditions under which this association is (and is not) observed.
We highlight two limitations of the study, both of which concern the ability to rule out alternative explanations for our results. First, while we controlled for numerous established risk factors for mortality at the individual level, we did not control for behavioral risk factors for mortality—including diet, smoking, and alcohol consumption—which are not routinely assessed in the GSS/NDI dataset. However, stigma contributes to each of these behavioral risk factors (eating: e.g., Major, Hunger, Bunyan, & Miller, 2014; smoking and drinking: e.g., Pascoe & Smart Richman, 2009), suggesting that they are on the causal pathway.
Second, because the GSS is a cross-sectional dataset, we only have information on residence at the time of interview and thus have limited data on geographic mobility into and out of communities with different levels of structural stigma, which could present an alternative explanation for these findings. Previous analyses from the GSS dataset (Hatzenbuehler, Flores, & Gates, 2017), however, have revealed only modest sexual orientation-related differences in mobility patterns (e.g., an estimated 38.1% of lesbian, gay, and bisexual respondents say they have lived in the same city since the age of 16 compared to 39.0% of heterosexual respondents); further, there was minimal evidence for different rates of geographic mobility based on self-reported health, suggesting that differential selection by health status is unlikely to explain our results.
Of course, evidence for a causal relationship between structural stigma and health inequalities cannot come from a single study but instead emerges from a multi-method, multi-outcome, multi-group approach across a series of studies and research groups. Over the last several years, this sort of evidence has begun to accumulate. Research among sexual minorities, for instance, has documented relations between structural stigma and health (as well as determinants of health, such as employment and hate crimes) across multiple methods, including cross-sectional designs (e.g., Riggle, Rostosky, & Horne, 2009), panel data with state fixed effects (e.g., Levy & Levy, 2017), cross-national comparisons (e.g., Berg, Ross, Weatherburn, & Schmidt, 2013), experience sampling studies (e.g., Frost & Fingerhut, 2016), difference-in-difference designs (e.g., Raifman, Moscoe, & Austin, 2017), and audit experiments (e.g., Tilcsik, 2011). Similar relationships have been observed with other stigmatized groups, including Blacks (e.g., Leitner et al., 2016), Latino and immigrant populations (e.g., Morey et al., 2018), Arab-Americans (Lauderdale, 2006), individuals with mental illness (e.g., Evans-Lacko et al., 2012), and individuals who are HIV-positive (e.g., Miller et al., 2011). Our analysis contributes to this growing empirical literature on the negative consequences of structural stigma for health and longevity among members of stigmatized groups.
Supplementary Material
Research Highlights.
We find a dose-response relationship between structural stigma and mortality risk.
The relationship holds after control for 6 established risk factors for mortality.
The relationship is specific to those who report past-year same-sex behaviors.
We show that this group is most likely to identify as gay men/lesbian women.
Thus, structural stigma may shape longevity among some sexual minority groups.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Berg RC, Ross MW, Weatherburn P, & Schmidt AJ (2013). Structural and environmental factors are associated with internalized homonegativity in men who have sex with men: Findings from the European MSM Internet Survey (EMIS) in 38 countries. Social Science & Medicine, 78, 61–69. doi: 10.1016/j.socscimed.2012.11.033. [DOI] [PubMed] [Google Scholar]
- Bonilla-Silva E (1997). Rethinking racism: Toward a structural interpretation. American Sociological Review, 63(3), 465–480. doi: 10.2307/2657316 [DOI] [Google Scholar]
- Bostwick WB, Boyd CJ, Hughes TL, & McCabe SE (2010). Dimensions of sexual orientation and the prevalence of mood and anxiety disorders in the United States. American Journal of Public Health, 100(3), 468–475. doi: 10.2105/AJPH.2008.152942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burris S (2006). Stigma and the law. Lancet, 367(9509), 529–531. doi: 10.1016/s0140-6736(06)68185-3 [DOI] [PubMed] [Google Scholar]
- Chae DH, Clouston S, Hatzenbuehler ML, Kramer MR, Cooper HL, Wilson SM, . . . Link BG (2015). Association between an internet-based measure of area racism and black mortality. PLoS One, 10(4), e0122963. doi: 10.1371/journal.pone.0122963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corrigan PW, Morris SB, Michaels PJ, Rafacz JD, & Rusch N (2012). Challenging the public stigma of mental illness: A meta-analysis of outcome studies. Psychiatric Services, 63(10), 963–973. doi: 10.1176/appi.ps.201100529 [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Watson AC, Heyrman ML, Warpinski A, Gracia G, Slopen N, & Hall LL (2005). Structural stigma in state legislation. Psychiatric Services, 56(5), 557–563. doi: 10.1176/appi.ps.56.5.557 [DOI] [PubMed] [Google Scholar]
- Dodge B, Herbenick D, Friedman MR, Schick V, Fu TC, Bostwick W, . . . Sandfort TGM (2016). Attitudes toward bisexual men and women among a nationally representative probability sample of adults in the United States. PLoS One, 11(10). doi: 10.1371/journal.pone.0164430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodge B, Herbenick D, Fu T-CJ, Schick V, Reece M, Sanders S, & Fortenberry JD (2016). Sexual behaviors of US men by self-identified sexual orientation: Results from the 2012 National Survey of Sexual Heath and Behavior. Journal of Sexual Medicine, 13(4), 637–649. [DOI] [PubMed] [Google Scholar]
- Dodge B, & Sandfort TGM (2007). A review of mental health research on bisexual individuals when compared to homosexual and heterosexual individuals Becoming visible: Counseling bisexuals across the lifespan. (pp. 28–51). New York, NY, US: Columbia University Press. [Google Scholar]
- Eliason MJ (1997). The prevalence and nature of biphobia in heterosexual undergraduate students. Archives of Sexual Behavior, 26(3), 317–326. doi: 10.1023/a:1024527032040 [DOI] [PubMed] [Google Scholar]
- Evans-Lacko S, Brohan E, Mojtabai R, & Thornicroft G (2012). Association between public views of mental illness and self-stigma among individuals with mental illness in 14 European countries. Psychological Medicine, 42(8), 1741–1752. doi: 10.1017/S0033291711002558 [DOI] [PubMed] [Google Scholar]
- Frost DM, & Fingerhut AW (2016). Daily exposure to negative campaign messages decreases same-sex couples’ psychological and relational well-being. Group Processes & Intergroup Relations, 19(4), 477–492. doi: 10.1177/1368430216642028 [DOI] [Google Scholar]
- Gibson JL (1995). The political freedom of African-Americans: A contextual analysis of racial attitudes, political tolerance, and individual liberty. Political Geography, 14(6), 571–599. doi: 10.1016/0962-6298(95)00055-F [DOI] [Google Scholar]
- Hatzenbuehler ML (2016). Structural stigma: Research evidence and implications for psychological science. American Psychologist, 71(8), 742–751. doi: 10.1037/amp0000068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Bellatorre A, Lee Y, Finch BK, Muennig P, & Fiscella K (2014). Structural stigma and all-cause mortality in sexual minority populations. Soc Sci Med, 103, 33–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Bellatorre A, Lee Y, Finch BK, Muennig P, & Fiscella K (2017). Corrigendum to “Structural stigma and all-cause mortality in sexual minority populations” [Soc. Sci. Med. 103 (2014) 33–41]. Social Science & Medicine. doi: 10.1016/j.socscimed.2017.11.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Branstrom R, & Pachankis JE (2018). Societal-level explanations for reductions in sexual orientation mental health disparities: Results from a ten-year, population-based study in Sweden. Stigma and Health, 3, 16–26. [Google Scholar]
- Hatzenbuehler ML, Flores AR, & Gates GJ (2017). Social attitudes regarding same-sex marriage and LGBT health disparities: Results from a national probability sample. Journal of Social Issues, 73, 508–528. [Google Scholar]
- Hatzenbuehler ML, & Keyes KM (2013). Inclusive anti-bullying policies and reduced risk of suicide attempts in lesbian and gay youth. Journal of Adolescent Health, 53(10), S21–26. doi: 10.1016/j.jadohealth.2012.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, & Link BG (2014). Introduction to the special issue on structural stigma and health. Social Science & Medicine, 103, 1–6. doi: 10.1016/j.socscimed.2013.12.017 [DOI] [PubMed] [Google Scholar]
- Hayes AF, & Rockwood NJ (2017). Regression-based statistical mediation and moderation analysis in clinical research: Observations, recommendations, and implementation. Behaviour Research and Therapy, 98, 39–57. [DOI] [PubMed] [Google Scholar]
- Herbenick D, Schick V, Fu T-C, Dodge B, Baldwin A, Reece M, . . . Fortenberry JD (2018). Sexual behaviors of U.S. women by self-identified sexual orientation: Results from the 2012 National Survey of Sexual Health and Behavior. Manuscript under review. [DOI] [PubMed] [Google Scholar]
- Herek GM (2002). Heterosexuals’ attitudes toward bisexual men and women in the United States. Journal of Sex Ressearch, 39(4), 264–274. doi: 10.1080/00224490209552150 [DOI] [PubMed] [Google Scholar]
- Herek GM (2007). Confronting sexual stigma and prejudice: Theory and practice. Journal of Social Issues, 63(4), 905–925. doi: 10.1111/j.1540-4560.2007.00544.x [DOI] [Google Scholar]
- Hsieh N, & Ruther M (2016). Sexual minority health and health risk factors: Intersection effects of gender, race, and sexual identity. American Journal of Preventive Medicine, 50(6), 746–755. doi: 10.1016/j.amepre.2015.11.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hubbard AE, Ahern J, Fleischer NL, Van der Laan M, Lippman SA, Jewell N, Bruckner T, & Satariano WA (2010). To GEE or not to GEE: Comparing population average and mixed models for estimating the associations between neighborhood risk factors and health. Epidemiology, 21(4), 467–474. doi: 10.1097/EDE.0b013e3181caeb90. [DOI] [PubMed] [Google Scholar]
- Lauderdale DS (2006). Birth outcomes for Arabic-named women in California before and after September 11. Demography, 43(1), 185–201. [DOI] [PubMed] [Google Scholar]
- Lee Y, Muennig P, Kawachi I, & Hatzenbuehler ML (2015). Effects of racial prejudice on the health of communities: A multilevel survival analysis. American Journal of Public Health, 105(11), 2349–2355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leitner JB, Hehman E, Ayduk O, & Mendoza-Denton R (2016). Blacks’ death rate due to circulatory diseases is positively related to whites’ explicit racial bias: A nationwide investigation using project implicit. Psychological Science, 27(10), 1299–1311. doi: 10.1177/0956797616658450 [DOI] [PubMed] [Google Scholar]
- Levy BL, & Levy DL (2017). When love meets hate: The relationship between state policies on gay and lesbian rights and hate crime incidence. Social Science Research, 61, 142–159. doi: 10.1016/j.ssresearch.2016.06.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link B, & Hatzenbuehler ML (2016). Stigma as an unrecognized determinant of population health: Research and policy implications. Journal of Health Politics, Policy and Law, 41(4), 653–673. [DOI] [PubMed] [Google Scholar]
- Link BG, & Phelan JC (2001). Conceptualizing stigma. Annual Review of Sociology, 27, 363–385. [Google Scholar]
- Lipsitch M, Tchetgen ET, & Cohen T (2010). Negative controls: A tool for detecting confounding and bias in observational studies. Epidemiology, 21, 383–388. doi: 10.1097/EDE.0b013e3181d61eeb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little TD, Jorgensen TD, Lang KM, & Moore EW (2014). On the joys of missing data. Journal of Pediatric Psychology, 39(2), 151–162. doi: 10.1093/jpepsy/jst048 [DOI] [PubMed] [Google Scholar]
- Major B, Dovidio JF, & Link BG (2017). The Oxford Handbook of Stigma, Discrimination, and Health. New York, NY: Oxford University Press. [Google Scholar]
- Major B, Hunger JM, Bunyan DP, & Miller CT (2014). The ironic effects of weight stigma. Journal of Experimental Social Psychology, 51, 74–80. doi: 10.1016/j.jesp.2013.11.009 [DOI] [Google Scholar]
- Major B, & O’Brien LT (2005). The social psychology of stigma. Annuual Review of Psychology, 56, 393–421. doi: 10.1146/annurev.psych.56.091103.070137 [DOI] [PubMed] [Google Scholar]
- Miller CT, Grover KW, Bunn JY, & Solomon SE (2011). Community norms about suppression of AIDS-related prejudice and perceptions of stigma by people with HIV or AIDS. Psychological Sciience, 22(5), 579–583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina Y, Marquez JH, Logan DE, Leeson CJ, Balsam KF, & Kaysen DL (2015). Current intimate relationship status, depression, and alcohol use among bisexual women: The mediating roles of bisexual-specific minority stressors. Sex Roles, 73(1–2), 43–57. doi: 10.1007/s11199-015-0483-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morey BN, Gee GC, Muennig P, & Hatzenbuehler ML (2018). Community-level prejudice and mortality among immigrant groups. Social Science & Medicine, 199, 56–66. doi: 10.1016/j.socscimed.2017.04.020 [DOI] [PubMed] [Google Scholar]
- Muennig P, Johnson G, Kim J, Smith TW, & Rosen Z (2011). The general social survey-national death index: An innovative new dataset for the social sciences. BMC Research Notes, 4, 385. doi: 10.1186/1756-0500-4-385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pascoe EA, & Smart Richman L (2009). Perceived discrimination and health: A meta-analytic review. Psychological Bulletin, 135(4), 531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raifman J, Moscoe E, & Austin SB (2017). Difference-in-differences analysis of the association between state same-sex marriage policies and adolescent suicide attempts. JAMA Pediatrics, 171(4), 350–356. doi: 10.1001/jamapediatrics.2016.4529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Regnerus M (2017). Is structural stigma’s effect on the mortality of sexual minorities robust? A failure to replicate the results of a published study. Social Science & Medicine, 188, 157–165. [DOI] [PubMed] [Google Scholar]
- Rhemtulla M, & Little T (2012). Tools of the trade: Planned missing data designs for research in cognitive development. Journal of Cognition and Development, 13(4), 425–438. doi: 10.1080/15248372.2012.717340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richman LS, & Hatzenbuehler M, L. (2014). A multilevel analysis of stigma and health: Implications for research and policy. Policy Insights from the Behavioral and Brain Sciences, 1(1), 213–221. doi: 10.1177/2372732214548862 [DOI] [Google Scholar]
- Riggle EDB, Rostosky SS, & Horne SG (2009). Marriage amendments and lesbian, gay, and bisexual individuals in the 2006 election. Sexuality Research and Social Policy. 6(1), 80–89. [Google Scholar]
- Ross LE, Dobinson C, & Eady A (2010). Perceived determinants of mental health for bisexual people: A qualitative examination. American Journal of Public Health, 100(3), 496–502. doi: 10.2105/AJPH.2008.156307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross LE, Salway T, Tarasoff LA, MacKay JM, Hawkins BW, & Fehr CP (2018). Prevalence of depression and anxiety among bisexual people compared to gay, lesbian, and heterosexual individuals: A systematic review and meta-analysis. Journal of Sex Research, 55(4–5), 435–456. doi: 10.1080/00224499.2017.1387755 [DOI] [PubMed] [Google Scholar]
- Schrimshaw EW, Siegel K, Downing MJ, & Parsons JT (2013). Disclosure and concealment of sexual orientation and the mental health of non-gay-identified, behaviorally bisexual men. Journal of Consulting and Clinical Psychology, 81(1), 141–153. doi: 10.1037/a0031272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tilcsik A (2011). Pride and prejudice: Employment discrimination against openly gay men in the United States. American Journal of Sociology, 117(2), 586–626. doi: 10.1086/661653 [DOI] [PubMed] [Google Scholar]
- Worthen MGF (2013). An argument for separate analyses of attitudes toward lesbian, gay, bisexual men, bisexual women, MtF and FtM transgender individuals. Sex Roles, 68(11), 703–723. doi: 10.1007/s11199-012-0155-1 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.