Abstract
Background
The study focuses on the influence of trochlear dysplasia on patellar tracking related to patellar instability.
Methods
Knee extension against gravity and dual-limb squatting were simulated with seven models representing knees being treated for recurrent instability. Trochlear depth was altered to represent lateral trochlear inclination (LTI) values of 6°, 12° and 24°. Repeated measures analyses compared patellar lateral shift (bisect offset index) across different LTI values. Peak bisect offset index during extension and squatting was correlated with patella alta (Caton-Deschamps index) and maximum lateral position of the tibial tuberosity.
Results
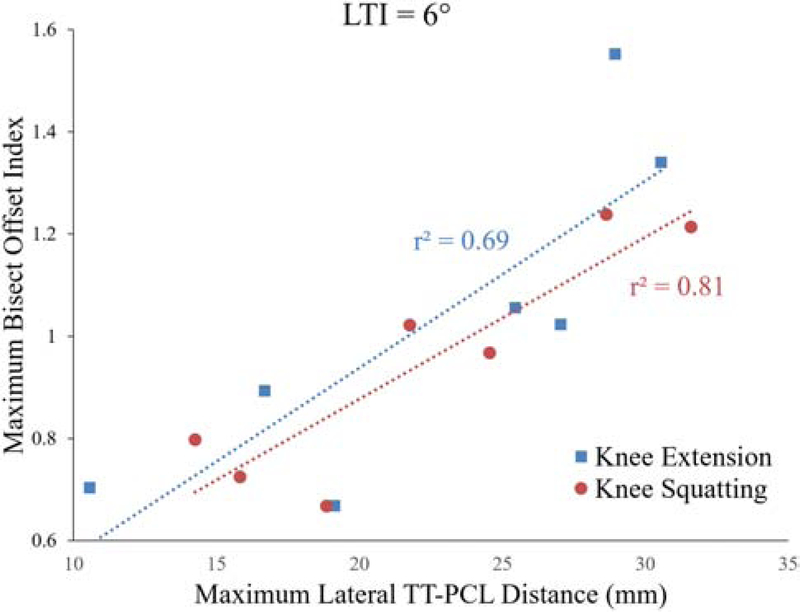
Bisect offset index varied significantly (p < 0.05) between different LTI values at multiple flexion angles throughout simulated knee extension and squatting. Average bisect offset values were 1.02, 0.95, and 0.86 for LTI = 6°, 12°, and 24°, respectively, at 0° of flexion for knee extension. The strongest correlation occurred between peak bisect offset index and lateral position of the tibial tuberosity for knee squatting with LTI = 6° (r2 = 0.81, p = 0.006). The strength of the correlation decreased as LTI increased. Caton-Deschamps was only significantly correlated with patellar tracking for LTI = 24° during knee squatting.
Conclusion
A shallow trochlear groove increases lateral patellar maltracking. A lateral tibial tuberosity in combination with trochlear dysplasia increases lateral patellar tracking and the risk of patellar instability. Patella alta has relatively little influence on patellar tracking in combination with trochlear dysplasia due to the limited articular constraint provided by the trochlear groove.
Keywords: Patellar instability, Trochlear dysplasia, Patellar tracking, Computational simulation
1-. Introduction
Patellar instability, generically describing patellar dislocation, patellar subluxation, and general symptomatic patellar instability, accounts for more than 20% of all injuries in runners [1]. Particularly, patellar dislocation is an acute knee injury causing significant functional impairment to young, active patients, with an incidence rate of 43 per 100,000 children below the age of 16 [2–5]. Patellar dislocations are associated with a tear of the medial patellofemoral ligament (MPFL), which is the primary passive stabilizer resisting lateral displacement of the patella [6]. Trochlear dysplasia (TD), patella alta, and a lateral position of the tibial tuberosity are also commonly associated with patellar instability [7,8]. In particular, TD refers to a pathological trochlear groove that limits the resistance to lateral subluxation [9,10], contributing to lateral patellar maltracking during knee function [11,12]. A shallow trochlear groove due to dysplasia has been noted in more than 90% of unstable knees [13,14]. TD is commonly associated with recurrent instability following initial conservative treatment, although most commonly in combination with other forms of pathology [15–17]. Trochleoplasty to deepen the trochlear groove is considered a viable surgical option to treat recurrent patellar instability associated with TD and lateral maltracking, with other options available for addressing a lateral position of the tibial tuberosity or patella alta as the primary pathology [18].
Previous studies focused on the influence of TD on patellar tracking have used two approaches to represent TD. Patellar tracking has been correlated with trochlear geometry within a population of subjects being treated for patellofemoral disorders, including a range of TD along with other pathological conditions [11,12,19], and within a population of cadaveric knees [20]. To focus specifically on TD, normal knees have been modified for parametric variation of trochlear depth [21–23]. The previous studies all showed that lateral patellar tracking increases as the depth of the trochlear groove decreases. Additional information is needed to improve assessment of the risk of recurrent patellar instability following an initial dislocation and the potential benefit of trochleoplasty, such as the influence of isolated variations in trochlear depth on patellar tracking for symptomatic knees and how both patella alta and lateral position of the tibial tuberosity interact with trochlear depth to influence patellar tracking.
The current study utilized computational simulation of dynamic function for knees being treated for recurrent patellar instability to evaluate the influence of TD on patellar tracking. Dynamic simulation was used to characterize how isolated variations in trochlear depth influence patellar tracking for symptomatic knees. How the influence of patella alta and lateral position of the tibial tuberosity on patellar tracking varies with trochlear depth was also evaluated.
2-. Materials and methods
2-1-. Computational models of subjects
Computational models were created to represent seven knees from subjects being treated for recurrent patellar instability. The subjects included five females. The average age was 15.8 years, ranging from 12 to 20 years. The study was approved by the Institutional Review Boards (IRB’s) of the two treating institutions, and each subject provided informed consent. The computational model of each knee was reconstructed (3D Doctor, Able Software Corp; Mimics, Materialise) from a high-resolution MRI scan (3.0 T, proton density weighted, slice thickness ranging from 0.6 mm to 1.5 mm). Shape of the bones and cartilage surfaces, orientation and attachment points for the quadriceps and hamstrings muscles, and attachment points for the anterior and posterior cruciate ligaments and patellar tendon were also obtained from reconstruction of the MRI scans.
2-2. Simulated motion
The multibody dynamic simulation approach has been previously described in detail [24,25]. Each model was individually validated by simulating a functional activity performed by the corresponding subject during diagnostic imaging. The functional activity performed was knee extension against gravity for two subjects and isometric knee extension against resistance at multiple positions of knee flexion for five subjects. The simulations produced patellar tracking patterns similar to those measured from the subjects, including peak lateral tracking near full extension [11]. Root-mean-square errors for comparisons between simulated lateral patellar shift and tilt and measurements based on diagnostic imaging of the subjects were 2.7 mm and 3.7°, respectively [25]. Simulations also produced correlations between knee anatomy and patellar tracking similar to those determined from the subjects [26].
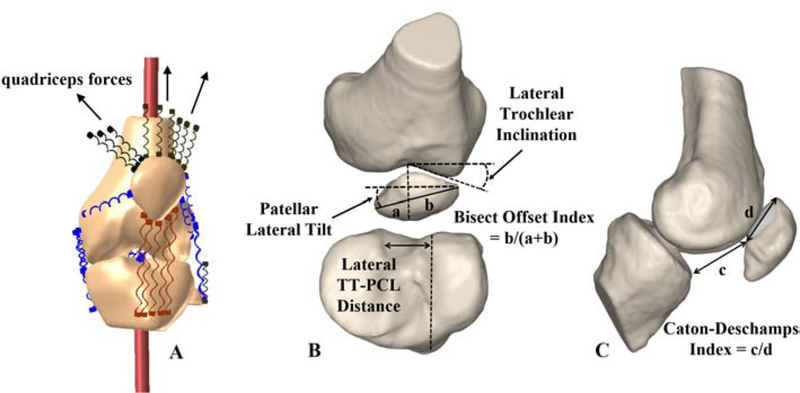
The models included ligaments, tendons, joint capsule, and retinacular structures represented by tension-only springs, including assigned properties for stiffness, damping, and pre-strain at full extension based on previous studies [27–31]. The MPFL was not included in the medial retinacular structures to account for injury following an instability episode. Forces were applied to the knee to represent quadriceps and hamstring muscles (Figure 1–A). The quadriceps force was divided among the vastus medialis obliquus, vastus lateralis, and combination of the vastus intermedius, rectus femoris, and vastus medialis longus based on previous studies [32,33]. Due to the weakened state, only 5% of the quadriceps force was applied through the vastus medialis obliquus, with approximately 21% applied through the vastus lateralis and approximately 74% through the combination of the vastus intermedius, rectus femoris, and the vastus medialis longus. The motion of anatomical coordinate systems fixed to the femur and tibia [34] determined tibiofemoral flexion based on the floating axis convention [35]. Patellofemoral and tibiofemoral contacts were represented by simplified Hertzian contact [36,37].
Figure 1.
Computational model for multibody dynamic simulation for one knee (A). Measures used to quantify bisect offset index, patellar lateral tilt, lateral TT-PCL distance, lateral trochlear inclination (B), as well as Caton-Deschamps index (C) are shown.
Reprinted from The Knee, Vol. 25, Elias, John J. et al., “Dynamic Tracking Influenced by Anatomy Following Medial Patellofemoral Ligament Reconstruction: Computational Simulation.”, 262–270, Copyright (2018), with permission from Elsevier.
For evaluation of trochlear dysplasia, loading and boundary conditions were applied to all models to represent knee extension against gravity from 50° of flexion to full extension (0° of flexion), and dual-limb knee squatting from 0° to 90° of flexion. The two separate activities were simulated to represent examination of the knee in a clinical setting and a more demanding functional activity. For knee extension, the total quadriceps force was set for each knee to initiate motion (average of 470 N at 50°), decreasing to a level that maintained continuous motion to full extension (average of 342 N at 0°). The total hamstrings force was set to one-sixth of the quadriceps force to provide the relatively low co-activation during knee extension [38]. Dual-limb knee squatting was represented with loading and boundary conditions based on in vitro simulation of dynamic knee squatting [39,40] that produced continuous knee flexion. An ankle joint was represented with three rotational degrees of freedom. A hip joint was simulated to allow flexion/extension, varus/valgus rotation, and proximal/distal translation. A total hamstrings force equal to one-third of the quadriceps force [41] was applied, with a constant 200 N body weight applied at the hip. A hip moment was implemented solely to initiate the squatting motion and was eliminated within the first few degrees of flexion to avoid effects on overall quadriceps forces for squatting, as well as patellofemoral and tibiofemoral kinematics.
2-3-. Systematic modification of trochlear morphology
An automated algorithm was developed (MATLAB, Mathworks, MA) to systematically modify the trochlear groove for the computational models. The algorithm focused on lateral trochlear inclination (LTI) (Figure 1–B) as a measure of trochlear depth based on the angle between the lateral facet of the trochlear groove (the line connecting the deepest point and the most anterior point of the lateral ridge of the trochlear groove) and the posterior condylar axis of the femur. LTI has previously been correlated with patellar tracking [11,12,26]. The algorithm quantified the reference LTI within an axial slice of the femur at the level of the most posterior points on the femoral condyles. For axial slices spanning the trochlear groove, the deepest point of the groove and the most prominent point of the lateral trochlear ridge were identified. Points at the reference slice were elevated or lowered in proportion to their depth to alter LTI to produce reference values of 6°, 12° and 24°. The lowest and highest LTI values approximately span the range of severely dysplastic to normal LTI values [42–44], while 12° represents the lowest LTI that would typically be considered non-dysplastic [45]. Linearly proportional changes were applied in a radial direction throughout the groove to maintain a smooth transition to unmodified proximal and distal ends. The cartilage surface was adjusted accordingly by maintaining a constant cartilage thickness map on the trochlear surface. The algorithm was capable of accurately altering trochlear geometry of the computational 3D knee models, with root-mean-square errors of 0.65° between the desired and measured reference LTI values.
2-4-. Characterization of patellar tracking and anatomy
Patellar lateral tracking and pathologic anatomy were characterized based on previously described parameters extracted from the computational models [11,12]. Patellar tracking was expressed by bisect offset index (portion of patellar width lateral to the deepest point of the trochlear groove) and patellar lateral tilt at 5° intervals of knee flexion throughout the simulation (Figure 1–B). Lateral position of the tibial tuberosity was quantified in terms of the lateral tibial tuberosity to posterior cruciate ligament attachment (TT–PCL) distance. The lateral TT–PCL distance is the distance from the patellar tendon attachment on the tibial tuberosity to the medial border of the posterior cruciate ligament attachment on the tibia in a lateral direction determined by the posterior condylar axis of the femur, and has previously been correlated with patellar tracking [11,26]. Patella alta was characterized by the Caton–Deschamps index (Figure 1–C), the ratio of the distance from the distal point of the patellar cartilage to the anterior–superior border of the tibia to the articular length along the patella. Caton-Deschamps index has been shown to be more strongly correlated with patellar tracking than Insall-Salvati index [46].
2-5-. Statistical analysis
Statistical analysis focused on the relationship between trochlear geometry and patellar tracking. Normality of the data distribution was evaluated at each studied flexion angle with Shapiro-Wilk tests (SPSS, IBM Analytics). At flexion angles with a normal data distribution, the tracking parameters were compared across different LTI values using repeated-measures Analysis of Variance (ANOVA) followed by post-hoc Student-Newman-Keuls tests. For flexion angles at which the data did not pass normality tests, non-parametric Friedman tests followed by post-hoc Student-Newman-Keuls comparisons were conducted to compare tracking parameters across different LTI values. To investigate the effect of TD severity on the correlations between patellar tracking and other types of pathology, stepwise multivariate linear regression analyses (SPSS, IBM Analytics) were performed to correlate bisect offset index and patellar lateral tilt with CD index and lateral TT-PCL distance for each LTI value. The analyses only included the maximum values of bisect offset index, lateral tilt, CD index, and lateral TT-PCL distance for each simulation to focus on the largest levels of lateral patellar tracking and pathology. The square of the correlation coefficient, r2, was quantified for each regression analysis. The standardized β coefficients, determining the relative predictive values of the independent variables, were also quantified to compare the correlations across different LTI values. For all statistical analyses, significance level was set at p < 0.05. A p-value of 0.10 was required to enter the stepwise multivariate linear regressions.
Results
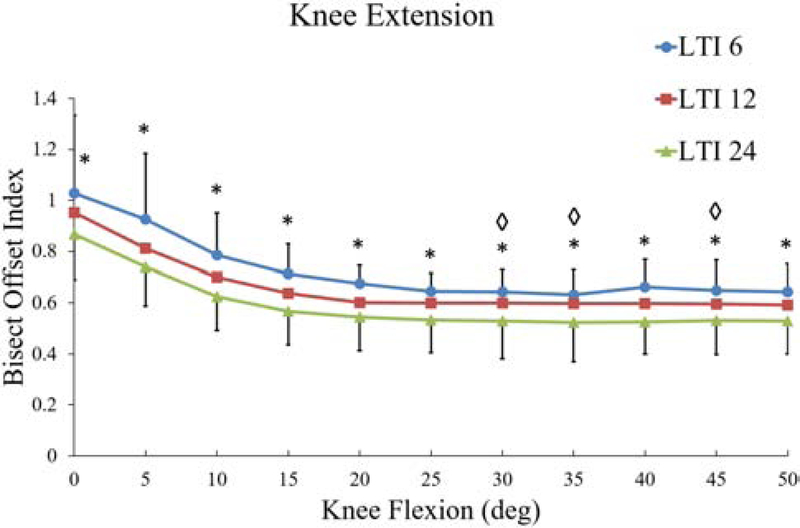
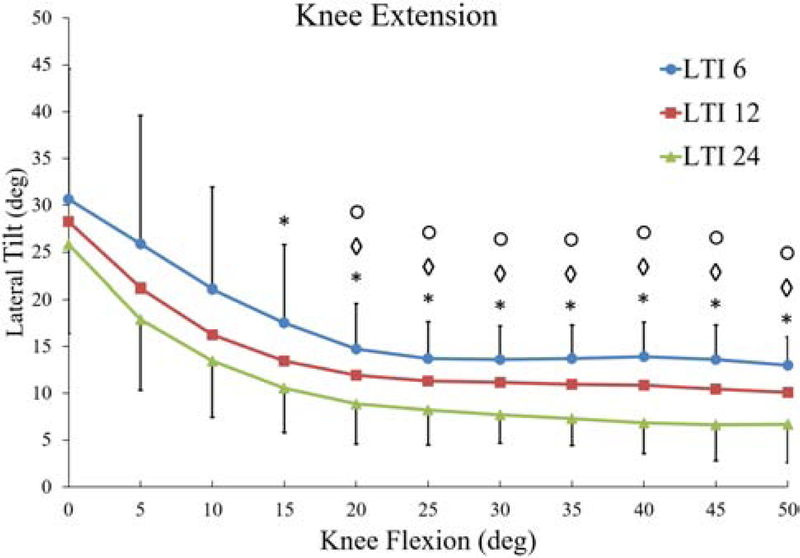
For simulated knee extension, the patella tracked more laterally as the LTI decreased. The bisect offset index peaked at full extension, with at least one significant difference between LTI values noted for all flexion angles from 0° to 50° (Figure 2). At 0° of flexion, the average (± standard deviation) bisect offset values were 1.02 ± 0.31, 0.95 ± 0.25, and 0.86 ± 0.18 for LTI values of 6°, 12°, and 24°, respectively. Significant differences in patellar tilt between LTI values occurred from 15° to 50°, with the difference in average lateral tilt between LTI = 6° and 24° approximately equal to 7° (Figure 3).
Figure 2.
Average (±SD) bisect offset index throughout simulated knee extension. * and ◊ indicate significant differences between LTI = 6° vs. 24°, and 6° vs. 12°, respectively.
Figure 3.
Average (±SD) patellar lateral tilt throughout simulated knee extension. *, ◊, and ○ indicate significant differences between LTI = 6° vs. 24°, 6° vs. 12°, and 12° vs. 24°, respectively.
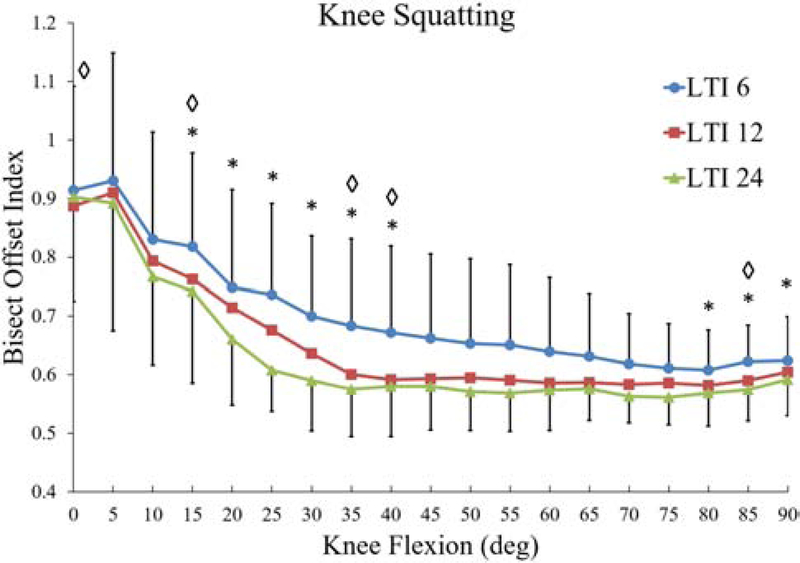
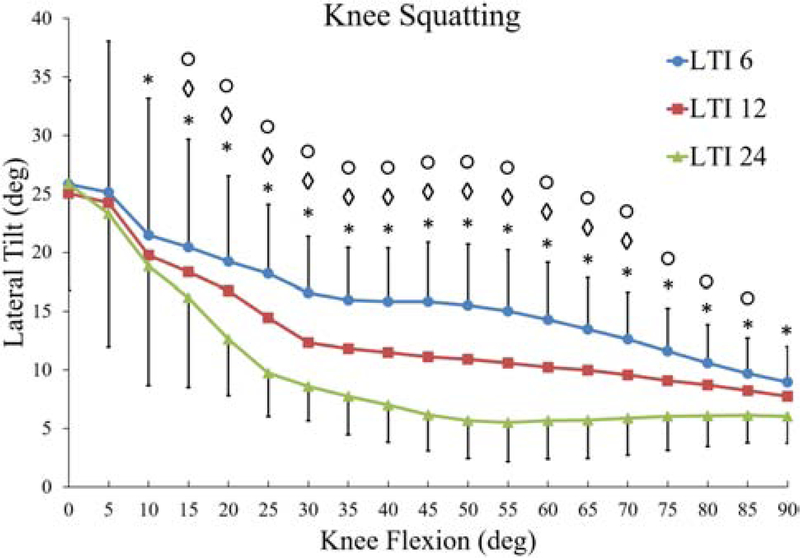
For simulated knee squatting, similar to knee extension against gravity, the patella tracked more laterally for cases with lower LTI. The largest significant differences in bisect offset index occurred from 15° to 40° of knee flexion (Figure 4). The average bisect offset index was greatest at low flexion angles for all conditions, with a peak value of approximately 0.9 ± 0.2 for all conditions. By 15°, the average bisect offset values were 0.71 ± 0.12, 0.64 ± 0.12, and 0.57 ± 0.13 for the LTI = 6°, 12°, and 24°, respectively. Patellar lateral tilt decreased more consistently from 10° to 90° of flexion, with the largest significant differences in average patellar tilt on the order of 10° (Figure 5).
Figure 4.
Average (±SD) bisect offset index throughout simulated knee squatting. * and ◊ indicate significant differences between LTI = 6° vs. 24°, and 6° vs. 12°, respectively.
Figure 5.
Average (±SD) patellar lateral tilt throughout simulated knee squatting. *, ◊, and ○ indicate significant differences between LTI = 6° vs. 24°, 6° vs. 12°, and 12° vs. 24°, respectively.
Lateral patellar tracking was correlated with lateral TT-PCL distance for a shallow trochlear groove (Table 1). The strongest correlation occurred between peak bisect offset index and lateral TT-PCL distance for knee squatting with LTI = 6° (r2 = 0.81, p = 0.006, β = 0.9, Figure 6). Similar correlations were identified for knee extension, with r2 = 0.69, p = 0.02, and β = 0.83 for the correlation between bisect offset index and lateral TT-PCL distance with LTI = 6°. The strength of the correlation between patellar tracking and lateral TT-PCL distance decreased as LTI increased to represent greater trochlear depth. CD index was excluded from all stepwise multivariate regression analyses, except for LTI = 24° during knee squatting, where it replaced lateral TT-PCL distance in the regression model, indicating an exclusive significant correlation with BO and lateral tilt.
Table 1.
Results of multivariate linear regression analyses relating bisect offset index and patellar lateral tilt to lateral TT-PCL distance and Caton-Deschamps (CD) index for separate LTI groups. For each regression, either CD index or lateral TT-PCL was eliminated from the analysis due to p > 0.10.
| r2 | p-Value |
Standardized β Coefficient | ||
|---|---|---|---|---|
| lateral TT-PCL | CD index | |||
| Knee Extension | ||||
| LTI 6° | ||||
| Bisect offset | 0.69 | 0.02 | - | 0.83 |
| Lateral Tilt | 0.73 | 0.015 | - | 0.85 |
| LTI 12° | ||||
| Bisect offset | 0.67 | 0.025 | - | 0.82 |
| Lateral Tilt | 0.64 | 0.03 | - | 0.80 |
| LTI 24° | ||||
| Bisect offset | 0.61 | 0.038 | - | 0.78 |
| Lateral Tilt | 0.46 | 0.09 | - | 0.68 |
| Knee Squatting | ||||
| LTI 6° | ||||
| Bisect offset | 0.81 | 0.006 | - | 0.90 |
| Lateral Tilt | 0.74 | 0.013 | - | 0.86 |
| LTI 12° | ||||
| Bisect offset | 0.78 | 0.008 | - | 0.88 |
| Lateral Tilt | 0.76 | 0.01 | - | 0.87 |
| LTI 24° | ||||
| Bisect offset | 0.65 | - | 0.028 | 0.81 |
| Lateral Tilt | 0.65 | - | 0.028 | 0.81 |
Figure 6.
Maximum bisect offset index vs. maximum lateral TT–PCL distance for the seven models during simulated knee squatting and extension for LTI = 6°. Best fit regression lines and the square of the correlation coefficient are shown.
Discussion
The results of the study indicate that TD significantly influences patellar lateral tracking throughout the entire range of knee motion in patients with symptomatic patellar instability. In particular, a shallow trochlear groove, characterized by a low LTI value, is linked with significantly higher patellar lateral shift and tilt. The average peak bisect offset index at full extension for LTI = 6° during knee extension of 1.02 indicates a high risk of patellar instability [47]. The peak bisect offset values of 0.95 and 0.86 for LTI values of 12° and 24°, considered to be just above the threshold for dysplasia and normal, respectively, still represent lateral maltracking, but with a significantly lower risk of patellar instability [47]. For knee squatting, significantly elevated lateral maltracking related to a shallow trochlear groove was mainly observed starting at 15° of knee flexion (Figures 4 and 5), as the patella is entering the trochlear groove. Failure of the groove to capture the patella during flexion causes patellar dislocation. The results of this study are in general agreement with the existing literature showing an increase in lateral tracking as the LTI decreases in knees being treated for patellar instability [11,12] and increased lateral tracking for isolated variation of trochlear depth [21–23]. By spanning the clinical range of trochlear dysplasia, the current results indicate that knees meeting clinical standards for TD are at high risk for recurrent instability following an initial instability episode and that deepening the groove can reduce the risk of continued instability.
The regression analyses indicate that severity of TD affects the extent to which patella alta and a lateral tibial tuberosity contribute to lateral maltracking. Regression analyses indicate an increasingly strong correlation between maximum lateral tracking of the patella and lateral TT-PCL distance as LTI decreases, as demonstrated by an increase in the β coefficient and r2. A significant correlation between tuberosity position and patellar lateral tracking in patients being treated for patellar instability has been shown previously [11]. With minimal articular constraints acting on the patella from a shallow trochlear groove, the position of the tibial tuberosity, and the resulting orientation of the patellar tendon, significantly influences patellar tracking. CD index was only significantly correlated with patellar tracking for the highest LTI value during knee squatting. With a normal trochlear groove, patella alta delaying entry of the patella into the groove can be a primary contributor to lateral maltracking. The lower influence of patella alta on patellar tracking when combined with TD is likely due to the already limited articular constraint provided by the trochlear groove, with minimal loss in constraint with delayed entry of the patella into the groove. In line with the current results, previous studies showed elevated lateral tracking related to patella alta in knees not being treated for patellar instability [48–51]. Previous studies based on subjects being treated for patellar instability did not show a significant correlation between CD index and patellar tracking [11,12], likely due to a high rate of trochlear dysplasia in the symptomatic knees.
The correlations relating CD index and lateral TT-PCL distance to lateral maltracking for variations in LTI should be understood due to the multiple forms of anatomical pathology that are typical of knees being treated for recurrent instability [15–17]. While the results indicate TD is associated with a high risk of recurrent instability, and a potential need for surgical stabilization, the combination of TD and a lateral position of the tibial tuberosity is especially problematic. For knees with patella alta, deepening the trochlear groove is likely to improve patellar tracking, but unresolved alta may mean patellar tracking is not restored to normal levels.
The study analyzed two separate functional activities. While the results of simulated knee extension against gravity are related to clinical examination of patellar maltracking through characterization of tracking patterns, such as a J-sign [23,52,53], knee squatting represents an activity more likely to induce knee instability due to the trochlear groove not capturing the patella at low flexion angles. Because minimal variations occurred in patellar tracking during knee extension for flexion angles deeper than 40°, simulation of knee extension was limited to 50°, compared to 90° for knee squatting. Several factors can contribute to differences in tracking patterns between knee squatting and knee extension. The femur was fixed in place for knee extension, but was allowed additional degrees of freedom during squatting. The average bisect offset index and patellar lateral tilt near 0° of flexion were higher in simulated knee extension compared to squatting, likely due to the larger quadriceps forces at 0° during horizontal knee extension to resist gravity. More demanding activities with elevated quadriceps forces or tibial external rotation at low flexion angles that would induce instability episodes were not represented to allow for evaluation of motion over the full range of flexion for each knee. Future studies focused specifically on dislocation events are warranted. Overall, the results from knee extension and squatting indicate that TD influences patellar maltracking related to patellar instability throughout the full range of flexion.
Compared to previous studies that have investigated the effects of TD on patellar tracking during knee function [11,12,21–23], the present study benefits from a unique combination of including other forms of anatomical pathology and parametric variation of trochlear depth. Hence, only the current study characterized the influence of isolated variations in TD on patellar maltracking while including other forms of pathology and evaluated the interaction between TD and measures of patella alta and a lateral position of the tibial tuberosity.
The computational simulation approach also includes limitations. While knee anatomy, including articular shape, ligament attachments and muscle orientations, was based on high resolution MRI scans, many properties were based on previously published data, rather than individualized for the subjects. Properties from the literature include elastic properties and resting lengths for springs representing ligaments, tendons and retinacular structures, as well as applied muscle forces. The models also accounted for only quadriceps and hamstrings muscles, without accounting for muscles that cross the hip joint, and only represented relatively young subjects. While the scope of the current study focused on the effect of TD on patellofemoral kinematics, future work should also investigate articular pressure distributions to identify potential correlations between anatomical abnormalities such as TD and excessive contact pressures associated with patellofemoral pain and osteoarthritis. The trochlear groove was altered without applying corresponding modifications on the patellar articular surface, influencing congruity of the patellofemoral joint. Although the patellar surface is not altered during a trochlear deepening procedure, this isolated alteration is a limitation for observations related to the influence of TD on the risk of recurrent instability. The observations related to surgical deepening of the trochlear groove do not specifically apply to any type of trochleoplasty, as trochleoplasty typically includes additional anatomical changes, such as eliminating the trochlear bump and lateralizing the groove [54]. The limitations related to congruence and representation of trochleoplasty were necessary for a general characterization of how TD influences patellar tracking relevant to initial assessment of the risk of recurrent instability and surgical planning to stabilize the patella.
Conclusions
The current simulations of knee function with parametric variation in the trochlear depth indicate a shallow trochlear groove increases lateral patellar maltracking and the risk of recurrent instability. Other pathologies associated with patellar instability should also be considered when assessing the risk of continued instability or planning surgical treatment. In particular, for knees with TD, the limited articular resistance leads to a significant influence of the position of the tibial tuberosity on patellar tracking, so that the combination of TD and a laterally positioned tuberosity is more of a concern than isolated TD. Patella alta has relatively little influence of patellar tracking in combination with TD due to the overall limited articular constraint provided by the groove, but may contribute to elevated lateral tracking following surgical deepening of the trochlear groove.
Acknowledgements
Research reported in this publication was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health under Award Number R21AR069150.
Footnotes
Declarations of Interest: none
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- [1].Redziniak D, Diduch D, Mihalko W, Fulkerson J. Patellar instability. J Bone Jt Surg 2009;91:2264–75. [PubMed] [Google Scholar]
- [2].Nietosvaara Y, Aalto K, Kallio PE. Acute patellar dislocation in children: incidence and associated osteochondral fractures. J Pediatr Orthop 1994;14:513–5. doi:8077438. [DOI] [PubMed] [Google Scholar]
- [3].Atkin DM, Fithian DC, Marangi KS, Stone ML, Dobson BE, Mendelsohn C. Characteristics of patients with primary acute lateral patellar dislocation and their recovery within the first 6 months of injury. Am J Sports Med 2000;28:472–9. doi: 10.1177/03635465000280040601. [DOI] [PubMed] [Google Scholar]
- [4].Stefancin JJ, Parker RD. First-time traumatic patellar dislocation: a systematic review. Clin Orthop Relat Res 2007;455:93–101. doi: 10.1097/BLO.0b013e31802eb40a. [DOI] [PubMed] [Google Scholar]
- [5].Apostolovic M, Vukomanovic B, Slavkovic N, Vuckovic V, Vukcevic M, Djuricic G, et al. Acute patellar dislocation in adolescents: Operative versus nonoperative treatment. Int Orthop 2011;35:1483–7. doi: 10.1007/s00264-011-1265-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Desio SM, Burks RT, Bachus KN. Soft Tissue Restraints to Lateral Patellar Translation in the Human Knee. Am J Sports Med 1998;26:59–65. doi: 10.1177/03635465980260012701. [DOI] [PubMed] [Google Scholar]
- [7].Steensen RN, Bentley JC, Trinh TQ, Backes JR, Wiltfong RE. The prevalence and combined prevalences of anatomic factors associated with recurrent patellar dislocation: A magnetic resonance imaging study. Am J Sports Med 2015;43:921–7. doi: 10.1177/0363546514563904. [DOI] [PubMed] [Google Scholar]
- [8].Christensen TC, Sanders TL, Pareek A, Mohan R, Dahm DL, Krych AJ. Risk Factors and Time to Recurrent Ipsilateral and Contralateral Patellar Dislocations. Am J Sports Med 2017;45:2105–10. doi: 10.1177/0363546517704178. [DOI] [PubMed] [Google Scholar]
- [9].Hopper GP, Leach WJ, Rooney BP, Walker CR, Blyth MJ. Does degree of trochlear dysplasia and position of femoral tunnel influence outcome after medial patellofemoral ligament reconstruction? Am J Sports Med 2014;42:716–22. doi: 10.1177/0363546513518413. [DOI] [PubMed] [Google Scholar]
- [10].Nelitz M, Williams RS, Lippacher S, Reichel H, Dornacher D. Analysis of failure and clinical outcome after unsuccessful medial patellofemoral ligament reconstruction in young patients. Int Orthop 2014;38:2265–72. doi: 10.1007/s00264-014-2437-4. [DOI] [PubMed] [Google Scholar]
- [11].Elias JJ, Soehnlen NT, Guseila LM, Cosgarea AJ. Dynamic tracking influenced by anatomy in patellar instability. Knee 2016;23:450–5. doi: 10.1016/j.knee.2016.01.021. [DOI] [PubMed] [Google Scholar]
- [12].Biyani R, Elias JJ, Saranathan A, Feng H, Guseila LM, Morscher MA, et al. Anatomical factors influencing patellar tracking in the unstable patellofemoral joint. Knee Surg Sports Traumatol Arthrosc 2014;22:2334–41. doi: 10.1007/s00167-014-3195-y. [DOI] [PubMed] [Google Scholar]
- [13].Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: An anatomic radiographic study. Knee Surgery, Sport Traumatol Arthrosc 1994;2:19–26. doi: 10.1007/BF01552649. [DOI] [PubMed] [Google Scholar]
- [14].Nelitz M, Lippacher S, Reichel H, Dornacher D. Evaluation of trochlear dysplasia using MRI: Correlation between the classification system of Dejour and objective parameters of trochlear dysplasia. Knee Surgery, Sport Traumatol Arthrosc 2012;22:120–7. doi: 10.1007/s00167-012-2321-y. [DOI] [PubMed] [Google Scholar]
- [15].Balcarek P, Oberthür S, Hopfensitz S, Frosch S, Walde TA, Wachowski MM, et al. Which patellae are likely to redislocate? Knee Surg Sports Traumatol Arthrosc 2014;22:2308–14. doi: 10.1007/s00167-013-2650-5. [DOI] [PubMed] [Google Scholar]
- [16].Jaquith BP, Parikh SN. Predictors of Recurrent Patellar Instability in Children and Adolescents After First-time Dislocation. J Pediatr Orthop 2015;00:1–7. doi: 10.1097/BPO.0000000000000674. [DOI] [PubMed] [Google Scholar]
- [17].Arendt EA, Askenberger M, Agel J, Tompkins MA. Risk of Redislocation After Primary Patellar Dislocation: A Clinical Prediction Model Based on Magnetic Resonance Imaging Variables. Am J Sports Med 2018;46:3385–90. doi: 10.1177/0363546518803936. [DOI] [PubMed] [Google Scholar]
- [18].Weber AE, Nathani A, Dines JS, Allen AA, Shubin-Stein BE, Arendt EA, et al. An algorithmic approach to the management of recurrent lateral patellar dislocation. J Bone Jt Surg - Am Vol 2016;98:417–27. doi: 10.2106/JBJS.O.00354. [DOI] [PubMed] [Google Scholar]
- [19].Powers CM. Patellar kinematics, part II: the influence of the depth of the trochlear groove in subjects with and without patellofemoral pain. Phys Ther 2000;80:965–73. doi: 10.1093/ptj/80.10.965. [DOI] [PubMed] [Google Scholar]
- [20].Ahmed AM, Duncan NA. Correlation of patellar tracking pattern with trochlear and retropatellar surface topographies. J Biomech Eng 2000;122:652–60. doi: 10.1115/1.1322036. [DOI] [PubMed] [Google Scholar]
- [21].Van Haver A, De Roo K, De Beule M, Labey L, De Baets P, Dejour D, et al. The Effect of Trochlear Dysplasia on Patellofemoral Biomechanics: A Cadaveric Study With Simulated Trochlear Deformities. Am J Sports Med 2015;43:1354–61. doi: 10.1177/0363546515572143. [DOI] [PubMed] [Google Scholar]
- [22].Fitzpatrick CK, Steensen RN, Tumuluri A, Trinh T, Bentley J, Rullkoetter PJ. Computational analysis of factors contributing to patellar dislocation. J Orthop Res 2016;34:444–53. doi: 10.1002/jor.23041. [DOI] [PubMed] [Google Scholar]
- [23].Amis AA, Oguz C, Bull AMJ, Senavongse W, Dejour D. The effect of trochleoplasty on patellar stability and kinematics. J Bone Joint Surg Br 2008;90-B:864–9. doi: 10.1302/0301-620X.90B7.20447. [DOI] [PubMed] [Google Scholar]
- [24].Elias JJ, Kelly MJ, Smith KE, Gall KA, Farr J. Dynamic Simulation of the Effects of Graft Fixation Errors During Medial Patellofemoral Ligament Reconstruction. Orthop J Sport Med 2016;4. doi: 10.1177/2325967116665080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Elias JJ, Jones KC, Lalonde MK, Gabra JN, Rezvanifar SC, Cosgarea AJ. Allowing one quadrant of patellar lateral translation during medial patellofemoral ligament reconstruction successfully limits maltracking without overconstraining the patella. Knee Surgery, Sport Traumatol Arthrosc 2017. doi: 10.1007/s00167-017-4799-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Elias JJ, Jones KC, Rezvanifar SC, Gabra JN, Morscher MA, Cosgarea AJ. Dynamic tracking influenced by anatomy following medial patellofemoral ligament reconstruction: Computational simulation. Knee 2018;25:262–70. doi: 10.1016/J.KNEE.2018.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Blankevoort L, Kuiper JH, Huiskes R, Grootenboer HJ. Articular contact in a three-dimensional model of the knee. J Biomech 1991;24:1019–31. doi: 10.1016/0021-9290(91)90019-J. [DOI] [PubMed] [Google Scholar]
- [28].Conlan T, Garth WP, Lemons JE. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am 1993;75:682–93. doi: 10.2106/00004623-199305000-00007. [DOI] [PubMed] [Google Scholar]
- [29].Shin CS, Chaudhari AM, Andriacchi TP. The influence of deceleration forces on ACL strain during single-leg landing: A simulation study. J Biomech 2007;40:1145–52. doi: 10.1016/j.jbiomech.2006.05.004. [DOI] [PubMed] [Google Scholar]
- [30].Stäubli H-U, Schatzmann L, Brunner P, Rincón L, Nolte L-P. Quadriceps tendon and patellar ligament: Cryosectional anatomy and structural properties in young adults. Knee Surgery, Sport Traumatol Arthrosc 1996;4:100–10. doi: 10.1007/BF01477262. [DOI] [PubMed] [Google Scholar]
- [31].Besier TF, Gold GE, Delp SL, Fredericson M, Beaupré GS. The influence of femoral internal and external rotation on cartilage stresses within the patellofemoral joint. J Orthop Res 2008;26:1627–35. doi: 10.1002/jor.20663. [DOI] [PubMed] [Google Scholar]
- [32].Makhsous M, Lin F, Koh JL, Nuber GW, Zhang LQ. In vivo and noninvasive load sharing among the vasti in patellar malalignment. Med Sci Sports Exerc 2004;36:1768–75. doi: 10.1249/01.MSS.0000142302.54730.7F. [DOI] [PubMed] [Google Scholar]
- [33].Zhang LQ, Wang G, Nuber GW, Press JM, Koh JL. In vivo load sharing among the quadriceps components. J Orthop Res 2003;21:565–71. doi: 10.1016/S0736-0266(02)00196-1. [DOI] [PubMed] [Google Scholar]
- [34].Elias JJ, Carrino JA, Saranathan A, Guseila LM, Tanaka MJ, Cosgarea AJ. Variations in kinematics and function following patellar stabilization including tibial tuberosity realignment. Knee Surg Sports Traumatol Arthrosc 2014;22:2350–6. doi: 10.1007/s00167-014-2905-9. [DOI] [PubMed] [Google Scholar]
- [35].Grood ES, Suntay WJ. A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech Eng 1983;105:136–44. doi: 10.1115/1.3138397. [DOI] [PubMed] [Google Scholar]
- [36].Guess TM, Liu H, Bhashyam S, Thiagarajan G. A multibody knee model with discrete cartilage prediction of tibio-femoral contact mechanics. Comput Methods Biomech Biomed Engin 2013;16:256–70. doi: 10.1080/10255842.2011.617004. [DOI] [PubMed] [Google Scholar]
- [37].Purevsuren T, Elias JJ, Kim K, Kim YH. Dynamic simulation of tibial tuberosity realignment: model evaluation. Comput Methods Biomech Biomed Engin 2014;18:1606–10. doi: 10.1080/10255842.2014.936857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Escamilla RF, Fleisig GS, Zheng N, Barrentine SW, Wilk KE, Andrews JR. Biomechanics of the knee during closed kinetic chain and open kinetic chain exercises. Med Sci Sports Exerc 1998;30:556–69. doi: 10.1097/00005768-199804000-00014. [DOI] [PubMed] [Google Scholar]
- [39].Elias JJ, Mattessich SM, Kumagai M, Mizuno Y, Cosgarea AJ, Chao EY. In vitro characterization of the relationship between the Q-angle and the lateral component of the quadriceps force. Proc Inst Mech Eng Part H J Eng Med 2004;218:63–7. doi: 10.1243/095441104322807767. [DOI] [PubMed] [Google Scholar]
- [40].Kumagai M, Mizuno Y, Mattessich SM, Elias JJ, Cosgarea AJ, Chao EY. Posterior cruciate ligament rupture alters in vitro knee kinematics. Clin Orthop Relat Res 2002;395:241–8. doi: 10.1097/00003086-200202000-00029. [DOI] [PubMed] [Google Scholar]
- [41].Elias JJ, Faust AF, Chu Y-H, Chao EY, Cosgarea AJ. The Soleus Muscle Acts as an Agonist for the Anterior Cruciate Ligament: An in Vitro Experimental Study. Am J Sports Med 2003;31:241–6. doi: 10.1177/03635465030310021401. [DOI] [PubMed] [Google Scholar]
- [42].Stefanik JJ, Roemer FW, Zumwalt AC, Zhu Y, Gross KD, Lynch JA, et al. Association between measures of trochlear morphology and structural features of patellofemoral joint osteoarthritis on MRI: The MOST study. J Orthop Res 2012;30:1–8. doi: 10.1002/jor.21486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Carrillon Y, Abidi H, Dejour D, Fantino O, Moyen B, Tran-Minh VA. Patellar Instability: Assessment on MR Images by Measuring the Lateral Trochlear Inclination—Initial Experience. Radiology 2000;216:582–5. doi: 10.1148/radiology.216.2.r00au07582. [DOI] [PubMed] [Google Scholar]
- [44].Nelitz M, Theile M, Dornacher D, Wölfle J, Reichel H, Lippacher S. Analysis of failed surgery for patellar instability in children with open growth plates. Knee Surgery, Sport Traumatol Arthrosc 2012;20:822–8. doi: 10.1007/s00167-011-1599-5. [DOI] [PubMed] [Google Scholar]
- [45].Batailler C, Neyret P. Trochlear dysplasia: Imaging and treatment options. EFORT Open Rev 2018;3:240–7. doi: 10.1302/2058-5241.3.170058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Pal S, Besier TF, Beaupre GS, Fredericson M, Delp SL, Gold GE. Patellar maltracking is prevalent among patellofemoral pain subjects with patella alta: An upright, weightbearing MRI study. J Orthop Res 2013;31:448–57. doi: 10.1002/jor.22256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Tanaka MJ, Bollier MJ, Andrish JT, Fulkerson JP, Cosgarea AJ. Complications of medial patellofemoral ligament reconstruction: common technical errors and factors for success: AAOS exhibit selection. J Bone Joint Surg Am 2012;94:e87. doi: 10.2106/JBJS.K.01449. [DOI] [PubMed] [Google Scholar]
- [48].Ward SR, Terk MR, Powers CM. Patella alta: Association with patellofemoral alignment and changes in contact area during weight-bearing. J Bone Jt Surg - Ser A 2007;89:1749–55. doi: 10.2106/JBJS.F.00508. [DOI] [PubMed] [Google Scholar]
- [49].Simmons E, Cameron JC. Patella alta and recurrent dislocation of the patella. Clin Orthop Relat Res 1992. doi: 10.1097/01241398-199207000-00054. [DOI] [PubMed] [Google Scholar]
- [50].Geenen E, Molenaers G, Martens M. Patella alta in patellofemoral instability. Acta Orthop Belg 1989;55:387–93. [PubMed] [Google Scholar]
- [51].Magnussen RA, De Simone V, Lustig S, Neyret P, Flanigan DC. Treatment of patella alta in patients with episodic patellar dislocation: a systematic review. Knee Surg Sports Traumatol Arthrosc 2014;22:2545–50. doi: 10.1007/s00167-013-2445-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Sheehan FT, Derasari A, Fine KM, Brindle TJ, Alter KE. Q-angle and J-sign: Indicative of Maltracking Subgroups in Patellofemoral Pain. Clin Orthop Relat Res 2010;468:266–75. doi: 10.1007/s11999-009-0880-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Smith TO, Davies L, O’Driscoll M-L, Donell ST. An evaluation of the clinical tests and outcome measures used to assess patellar instability. Knee 2008;15:255–62. doi: 10.1016/J.KNEE.2008.02.001. [DOI] [PubMed] [Google Scholar]
- [54].Fucentese SF, Schöttle PB, Pfirrmann CWA, Romero J. CT changes after trochleoplasty for symptomatic trochlear dysplasia. Knee Surgery, Sport Traumatol Arthrosc 2007;15:168–74. doi: 10.1007/s00167-006-0140-8. [DOI] [PubMed] [Google Scholar]