Abstract
Background
The aim of this study was to study the determinants of nonadherence to immunosuppressant drugs in liver transplant (LT) recipients using personalised interview and questionnaire methods.
Methods
The study was conducted on adult LT recipients (deceased donor liver transplant [DDLT] and living donor liver transplant [LDLT]) from the Indian subcontinent, at post-LT clinic visit between July and December 2016. Recipient details included baseline demography, comorbidity, psychological status, details of addiction, indication and type of transplant. Details on financial support for transplantation, admissions for rejection, infection and posttransplant complications were obtained from the hospital records. An adherence questionnaire was completed by direct interview and using a questionnaire.
Results
Sixty-seven LT recipients (56 males, median age 48.17 years) constituted the study group. Overall, 11 patients (16.47%) were nonadherent to treatment. LDLT recipients were more adherent than DDLT recipients. Nonadherent recipients were believers in alternative systems of medicine. Medication-related factors such as improper dosing, meagre drug knowledge difficulty in remembering drug dose and timings and economic constraints in continuing medical treatment were statistically significant in nonadherent recipients. Although variation in the tacrolimus levels were significantly more common in the nonadherent group, acute cellular rejection and infection were not statistically different.
Conclusions
The prevalence of nonadherence was 16.5%. Determinants of nonadherence were DDLT, belief in alternative medications, high regimen complexity, poor knowledge about medications and cost issues with long-term medications.
Keywords: liver, transplant, adherence, India
Abbreviations: ACR, Acute cellular Rejection; CAM, Complementary and Alternative Medicine; DDLT, Deceased Donor Liver Transplant; LDLT, Living Donor Liver Transplant; LT, liver transplantation
The term compliance has been defined by the World Health Organization as “the extent to which a patient's behaviour coincides with the clinical prescription”.1 Adherence to medical treatment is based not only on taking drugs at proper time and dosage but also on regular hospital visits, undergoing recommended blood tests and other investigations and finally reporting medical complications if any to the treating physician. Patients who refrain to follow one or more of the aforementioned parameters are labelled as nonadherent.2, 3
Immunosuppressive therapy is an absolute necessity in patients who underwent liver transplant (LT) to avoid graft rejection. Nonadherence with treatment leads to graft rejection and graft loss.4, 5, 6 Assessment of nonadherence is challenging in the absence of accurate objective measurement techniques.2, 7, 8 Schweizer et al9 were the first to report nonadherence in 15%–18% of a cohort of solid organ transplant recipients. Confirming the importance of adherence, they reported that 91% of noncompliant kidney transplant recipients suffered death or graft loss.9 Several studies thereafter4, 5, 6, 10, 11 have evaluated nonadherence using different study methods. They reported nonadherence rates ranging from 5.6 to 73%.
Although liver transplantation as a treatment modality has been developing exponentially in Asia over the last 10–15 years, there has been limited literature assessing the prevalence of drug noncompliance. The present study was undertaken to define the determinants of nonadherence to medications in LT recipients using interview and questionnaire methods.
Materials and methods
This cross-sectional study was conducted at the Institute of Liver Disease and Transplantation, Gleneagles Global Health City, Chennai. All adult LT recipients of Indian origin (both deceased donor liver transplant [DDLT] and living donor liver transplant [LDLT]), attending posttransplant clinic over a six-month period between July and December 2016 were enrolled in the study. Patients within 3 months of LT were excluded from the study because they are usually closely monitored. Patients were enrolled after obtaining written informed consent.
All recipients were counselled during pretransplant workup about the long-term follow-up after LT, the importance of adherence to medications and the approximate recurrent expenditure likely to be incurred after LT, i.e., Rs 40,000/- ($500) approximately for the initial 3 months and Rs 15,000/- ($200) thereafter. The details of medications and follow-up protocol at our institute are mentioned in Table 1. The importance of compliance was reiterated during the inpatient stay, and patients and caregivers were tested to confirm knowledge of their medications before discharge and during posttransplant clinic visits.
Table 1.
Details of Initial Medications and Follow-up—Institutional Protocol.
Medication protocol
Continue 5 mg indefinitely in case of AIH and repeated rejections.
Biweekly tests (initial 6 weeks)—Blood counts, liver function tests, renal function tests, serum magnesium and tacrolimus blood levels Radiological investigations as per requirement Regular visit to the posttransplant OP clinic Local patients First 6 weeks: Biweekly visit; for 3 months: once a week; for 1 year thereafter: once a month; beyond one year: once in three months Outstation patients First three months, as local patients; later, follow-up with referral physician Correspondence via email in structured format |
AIH, autoimmune hepatitis, BD, twice daily; UDCA, ursodeoxycholic acid; OP, out patient
In the absence of an approved Indian proforma for assessing medication adherence, a simple questionnaire was formulated as per clinical experience of the team, and major parameters likely to affect adherence were included. Before finalisation of the study protocol, the questionnaire was piloted in 20 recipients of Indian origin. Six questions were modified for language based on the feedback provided to improve comprehension.
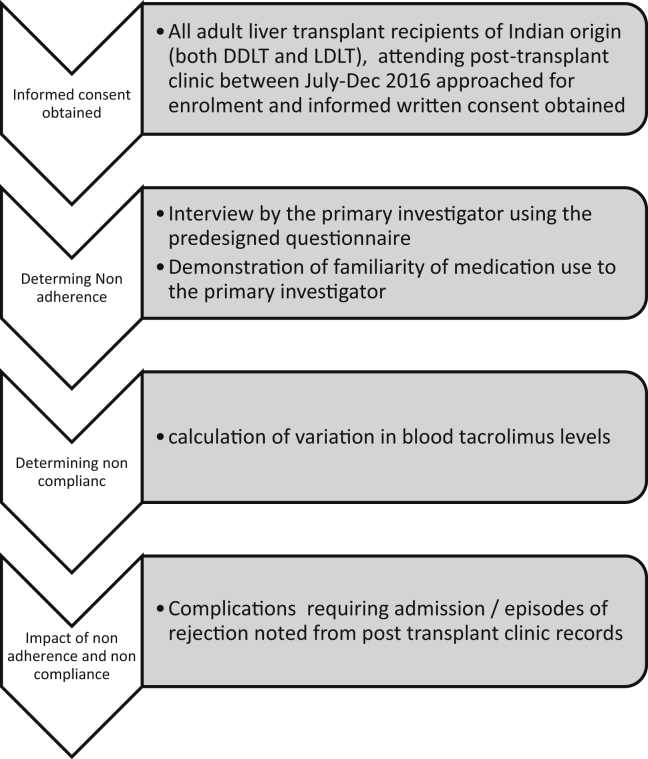
The algorithm for patient recruitment and assessment in the study is shown in Figure 1. The questionnaire was completed by the patients under the supervision of an investigator (M.J.). The questionnaire included demographic details, socioeconomic parameters as per modified Kuppuswamy socioeconomic scale,12 physician-related factors and medication-related factors. The patients were asked to demonstrate their familiarity with names of medications, dosage and schedule under direct observation by the investigator (M.J.). This included immunosuppressive agents and nonimmunosuppressive medications such as supplements and specific medications for diabetes, hypothyroidism, coronary heart disease, hypertension and hepatitis B or C virus infection. Use of complementary and alternative medications (CAM), if any, during follow-up was also recorded in the questionnaire. Table 2 highlights the points assessed in the questionnaire.
Figure 1.
The study design.
Table 2.
Proforma Used for the Study.
| Demographic details |
|---|
|
| Socioeconomic status |
 |
|
Clinical variables
|
Psychosocial variables
|
| Physician related factors |
| Doctor interaction- time: adequate/not adequate |
| Explanation: adequate/not adequate |
| Details of dosing: adequate/not adequate |
| Adverse effects of medication: adequate/inadequate |
| Medication related factors |
| Do you take your drugs daily in prescribed dosage? Always/most of the time/change doses as per will/rarely |
| Drug related factors | Details of medications | ||
| Name of drugs | know | Know a little | Do not know |
| Knowledge about medication | yes | little | Do not know |
| No. of drugs | <5 | 5–10 | >10 |
| Daily tablet count | <10 | 10–20 | >20 |
| Regimen complexity | Simple | Difficult but can remember | Extremely difficult |
| Total pill burden | Can manage | Difficult to manage | Impossible to manage |
| Health care costs | Can afford easily | Expensive (afford with difficulty) | Out of reach |
| Treatment knowledge |
|---|
| All drugs |
| Immunosuppression |
| Non immunosuppression drugs |
| Chronic disease drugs |
| Demonstrated regimen use |
|---|
| All drugs |
| Immunosuppression |
| Non immunosuppression drugs |
| Chronic disease drugs |
| Nonadherence by self reporting and demonstration-yes/no | ||||||
| Tacrolimus levels | ||||||
| Date | ||||||
| Levels | ||||||
| Rehospitalisation-Date and indication | ||||||
LDLT, living donor liver transplant; DDLT, deceased donor liver transplant; ; UHID, unique hospital identification number; CGHS, Central Government Health Scheme; DM, diabetes mellitus; HTN, hypertension; TB, tuberculosis; CKD, chronic kidney disease.
Tacrolimus trough values were tested on the day of interview. Tacrolimus levels were also noted for the preceding two visits and three subsequent visits to assess variation in blood tacrolimus levels. Details of post-LT admissions for rejection, infection and other complications were extracted from hospital records for the preceding duration (at least 3 months—maximum one year).
Adherence questionnaire was completed on the day of visit to the posttransplant clinic. Patients were considered nonadherent when they failed to demonstrate the dosing schedule for one or more prescribed immunosuppressant drugs. Variability in blood tacrolimus levels was reported as the standard deviation (SD) of six consecutive blood tacrolimus levels. An SD greater than 2.5 was considered as a surrogate marker of nonadherence. This is based on earlier studies that reported that an SD greater than 2.5 indicated nonadherence and predicted graft rejection.13, 14
Statistical Tests
The data collected were tabulated in a Microsoft Excel sheet. Patients were divided into two groups: adherent (group I) and nonadherent (group II). Chi-square test and comparison of proportions were used for statistical analysis. Sensitivity and specificity of tacrolimus SD levels for predicting adherence was calculated. A P value < 0.05 was considered statistically significant.
This study protocol was approved by the institutional ethics committee (via Letter number HR/2016/MS/010).
Results
A total of 93 Indian patients were expected to follow up during the study period. Six patients missed out on follow-up, and 20 did not visit the centre but communicated their reports via email or telephonically. Thus, the study group consisted of 67 patients (56 males; median age, 48 years). Eleven patients (16.5%) were nonadherent to the medication schedule. It was noted that patients who were nonadherent missed an average of 3.2 doses/week/patient of medications, whereas those found adherent by study definition missed 2.4 doses/week/patient (P 0.08).
Table 3 shows the demographic characteristics of patients in the adherent and nonadherent groups. Patients in both the groups were similar in terms of age, indication for LT and duration since transplant. There was no statistical difference in education and socioeconomic parameters. However, nonadherent patients were more likely to have undergone a DDLT (P < 0.04) and more frequently believed in CAM (P < 0.01).
Table 3.
Baseline Characteristics of Adherent and Adherent Patients.
| Parameters | Adherent (n = 56) | Nonadherent (n = 11) | P value |
|---|---|---|---|
| Age in years (median, range) | 47.74 (21–69) | 51.09 (23–64) | 0.32 |
| Married | 51 (91%) | 10 (90.9%) | 0.28 |
| Modified Kuppuswamy status (for socioeconomic status) | |||
| Upper | 23 (41%) | 4 (36.4%) | 0.92 |
| Upper middle | 17 (30.4%) | 4 (36.4%) | |
| Middle/lower middle | 16 (28.6%) | 3 (27.3%) | |
| Family size | |||
| 0–4 | 33 (59%) | 5 (45.5%) | 0.41 |
| 5 or more | 23 (41%) | 6 (54.5%) | |
| Residence | |||
| Rental | 4 (7%) | 0 | 0.36 |
| Self-owned | 52 (93%) | 11 (100%) | |
| Financial support | |||
| Self-funded | 30 (53.6%) | 6 (54.5%) | 0.30 |
| Loan/insurance | 15 (26.8%) | 1 (9.1%) | |
| Liquidation of immovable assets | 11 (19.6%) | 4 (36.4%) | |
| Government funding | None | None | |
| Funding for posttransplant care | |||
| Loan/insurance | 6 (10.7%) | 3 (27.3%) | 0.35 |
| Liquidation of immovable assets | 20 (35.71%) | 1 (9.1%) | |
| Self-payment | 30 (53.6%) | 7 (63.6%) | |
| Indication for transplant | |||
| Alcohol | 19 (33.9%) | 6 (54.5%) | 0.19 |
| Other etiologies | |||
| Hepatotropic viruses | 4 (7.14%) | 0 | 0.64 |
| NASH/cryptogenic | 16 (28.57%) | 4 (36.4%) | |
| Others | 9 (16%) | 1 (9.1%) | |
| HCC | 3 (5.35%) | 0 | |
| Combinations | 5 (8.92%) | 0 | |
| Type of transplant | |||
| LDLT | 34 (61%) | 3 (27.3%) | 0.041 |
| DDLT | 22 (39%) | 8 (72.7%) | |
| Duration since liver transplantation | |||
| <1 year | 30 (53.6%) | 6 (54.5%) | 0.64 |
| 1–2 years | 15 (26.8%) | 4 (36.4%) | |
| >2 years | 11 (19.6%) | 1 (9%) | |
| Alcohol intake (recidivism) | 2 (3.5%) | 2 (18.2%) | 0.06 |
| Comorbidities | |||
| None | 43 (76.8%) | 6 (54.5%) | 0.1 |
| DM | 6 (10.7%) | 3 (27.3%) | |
| HTN | 3 (5.35%) | 0 | |
| DM + HTN | 4 (7%) | 1 (9.1%) | |
| Others | – | 1 (9.1%) | |
| Preoperative psychiatric assessmentrowhead | |||
| Depression | – | – | |
| Anxiety | 2 | 1 | |
| Combination of the two dependence (alcohol, smoking or drugs) | 1 | – | |
| Belief in CAM | 6 (10.7%) | 5 (45.5%) | 0.01 |
LDLT, living donor liver transplant; DDLT, deceased donor liver transplant; CAM, complementary and alternative medications; NASH, non alcoholic steatohepatitis; HCC, hepatocellular carcinoma; DM, diabetes mellitus; HTN, hypertension.
There were no statistical differences in pretransplant counselling factors (Table 4). However, the high regimen complexity (P = 0.006) such as proper dosing, poor drug knowledge and difficulty in remembering drug dose and timings was frequent amongst nonadherent recipients, who also reported economic constraints in continuing medical treatment (P = 0.003) (Table 5).
Table 4.
Pretransplant Counselling Responses.
| Questions | Response | Gp I | Gp II | P value |
|---|---|---|---|---|
| Was need for lifelong immunosuppression explained to you? | Yes | 53 (95) | 11 (100) | 0.43 |
| Were you informed regarding cost and side effects of post liver Tx medications? | Yes | 52 (93%) | 9 (81.8%) | 0.24 |
| Were you informed about the repeated blood tests required in the post op period and the likely cost of each test? | Yes | 49 (87.5%) | 10 (90.9%) | 0.75 |
| Use of CAM | Yes | 19 (34%) | 5 (45.5%) | 0.47 |
| Is doctor interaction time adequate? (in pretransplant and posttransplant setting) | Yes | 47 (84%) | 7 (63.6%) | 0.12 |
| Is explanation by the doctor adequate? | Yes | 46 (82%) | 7 (63.6%) | 0.17 |
| Is drug dosage explained adequately by the doctors? | Yes | 46 (82%) | 10 (90.9%) | 0.47 |
| Were you counselled regarding the potential drug side effects in detail? | Yes | 40 (71.5%) | 7 (63.6%) | 0.60 |
CAM, complementary and alternative medications; Gp, group.
Table 5.
Medication-Related Factors and Their Impact on Adherence.
| Questions | Response | Group I | Group II | P value |
|---|---|---|---|---|
| Medication-related problems | None | 8 (14%) | 0 | 0.53 |
| Too many tablets | 26 (46.4%) | 4 (36.4%) | ||
| Timing difficult to maintain | 16 (28.6%) | 3 (27.3%) | ||
| Need someone to administer drugs | 6 (10.71%) | 2 (18.2%) | ||
| Do you take drugs daily in prescribed dosages | Always | 47 (84%) | 5 (45.5%) | 0.048 |
| Most of the time | 9 (16%) | 4 (36.4%) | ||
| Rarely | – | 2 (18.2%) | ||
| Name of drugs | Good knowledge | 45 (80.4%) | 4 (36.4%) | 0.010 |
| Know a little | 7 (12.6%) | 5 (45.5%) | ||
| No knowledge | 4 (7%) | 2 (18.2%) | ||
| Knowledge about drug effects and use | Good knowledge | 44 (79%) | 3 (27.3%) | 0.003 |
| Know a little | 8 (14%) | 6 (54.5%) | ||
| No knowledge | 4 (7%) | 2 (18.2%) | ||
| No. of drugs used daily | <5 | 26 (46.4%) | 4 (36.4%) | 0.174 |
| 5–10 | 19 (34%) | 2 (18.2%) | ||
| >10 | 11 (19.7%) | 5 (45.5%) | ||
| Daily tablet count | <10 | 24 (42.9%) | 4 (36.4%) | 0.92 |
| 10–20 | 19 (34%) | 4 (36.4%) | ||
| >20 | 13 (34.1%) | 3 (27.3%) | ||
| Regimen complexity | Simple | 18 (32.1%) | 1 (9.1%) | 0.006 |
| Difficult but can remember | 35 (62.5%) | 6 (54.5%) | ||
| Extremely difficult | 3 (5.4%) | 4 (36.4%) | ||
| Cost of medications | Can afford easily | 2 (3.5%) | 1 (9.1%) | 0.003 |
| Expensive but can afford | 38 (67.9%) | 2 (18.2%) | ||
| Expensive and manage with difficulty | 10 (17.9%) | 6 (54.5%) | ||
| Out of reach | 2 (3.5%) | 2 (18.2%) |
Bold represents that these p values are significant.
Although variations in the tacrolimus levels were significantly more common in the nonadherent group, acute cellular rejection and infection were not statistically different (Table 6). This could be due to small number of patients and short follow-up assessment. Four patients (2 in each group) reported recidivism.
Table 6.
Effect of Nonadherence on Complications and Tacrolimus Levels.
| Group I | Group II | P value | |
|---|---|---|---|
| Acute cellular rejection | 4 (7%) | 2 (18.2%) | 0.23 |
| Infections requiring hospitalisation | 2 (3.5%) | 0 | 0.54 |
| Tacrolimus variation >2.5 SD | 17 (30.3%) | 10 (90.9%) | 0.0002 |
SD, standard deviation.
Discussion
Drug nonadherence after LT has been extensively studied in the West. High medication costs, age less than 40 years, psychiatric disorders and medication-related side effects have been implicated in nonadherence.9, 11, 15 Dobbels et al16 reported that low social support, higher education levels, pretransplant nonadherence to medications and lower conscientiousness were independent pretransplant predictors of nonadherence in the posttransplant period. However, there are limited data from South Asia. Factors specific to this part of the world include lower per capita income, high out-of-pocket medical expenditure and lower education and awareness levels. Popularity of CAM has the potential to increase nonadherence levels. On the contrary, other factors specific to this region such as close-knit family patterns and highly selective access to such high-end treatments may lead to better drug adherence. In our study, none of the factors such as indication for LT, marital status, occupation, socioeconomic support and financial status were associated with nonadherence. Nonadherence was common in patients who underwent DDLT and those who believed in CAM. Nonadherence could be higher in patients who underwent DDLT because of several factors such as unknown donor, prolonged waiting period before transplant, feeling just lucky to get the organ and lower family pressure to maintain compliance because no family donor (spouse/sibling/child) is involved. We noted that although a significant number of nonadherent patients believed in CAM, only few of them admitted to using them. Concurrent CAM use is quite common in India. Ayurveda, followed by homoeopathy drugs, is commonly used by patients, and three-fourths of them do not inform their physicians about CAM use. They are mostly started on advice of a relative or friend, and no or fewer side effects are the commonest reason for their use.17None of our patients stopped immunosuppressive medications but admitted to taking CAM additionally.
Alcohol relapse (recidivism) is defined as any alcohol intake after surgery and is considered as nonadherent behaviour.18 Four patients (2 from adherent and 2 from nonadherent group) reported alcohol use after LT. This relapse rate is lower than 10–50% relapse reported at the end of five years.19, 20 All these patients were transplanted for alcohol-related liver disease, and thus, the recidivism rate was 16% (4/25).
None of the physician-related parameters such as interaction time and explanation regarding adverse effects and dose had an impact on adherence. However, medication-related factors such as high regimen complexity, poor knowledge about medications and cost issues with long-term medications had a significant impact on adherence in the patient's cohort. Variability in tacrolimus levels (SD > 2.5 μg per dL) was higher in the nonadherent group. This suggests that variability of tacrolimus levels may be a good marker to adherence in patients. However, one-third of patients in group I also had tacrolimus variation of >2.5 mcg/dl SD. The sensitivity and specificity of tacrolimus SD variation in our cohort were 90.9% (confidence interval [CI], 58.7–99.7%) and 69.6% (CI, 5.9–81.2%), respectively. Although tacrolimus level is an important surrogate indicator of nonadherence, sometimes patients may have a low level because of their inherent drug metabolism properties. It may be noted that in this study, despite variation in tacrolimus level in the nonadherence group, acute cellular rejection rates were not different. However, this may be due to the low number of patients overall.
Some of the factors for nonadherence can be improved by education, closer follow-up and psychoeducational services.21, 22, 23 LT is not just about carrying out a transplant with surgical success and physicians identifying complications. Much of posttransplant wholesome care is dependent on team work. In today's era, the medical social worker is a liaison who assumes a very important role in drug compliance: frequent phone calls, home visits, alerting the physician of recidivism, early identification of financial and social issues. Transplant psychologist and support groups function similarly. Without the support of these vital ancillary services, the long-term outcomes cannot be improved.
The present study has tried to address the issue of medication adherence for the first time in Indian setting. Although numerous factors such as DDLT, belief in CAM and several medication-related parameters were found more frequently in the nonadherent group, their causal relationship with nonadherence cannot be established because of small sample size and lack of objective measures to accurately measure them. Moreover, we noted that the difference in doses missed per week per patient was only 0.8 and not statistically significant. Thus, the interplay between various factors studied is complex and difficult to assess completely with the present sample size and study design. Studies with larger patient numbers are warranted to have more definitive conclusions. Place of stay and liver transplantation for acute liver failure may influence medication adherence. Most patients in the present study (61) were from outside Chennai, and none of the patients underwent LT for acute liver failure. Thus, these factors were not analysed. Long-term follow-up would be more useful to assess medication adherence. It is more likely for patients on long-term follow-up to get noncompliant despite the regimens getting simpler after one year of transplant. Moreover, 26 patients who missed their visits during the study period could also have been noncompliant. A lot of patients in India do not actually visit the transplant centre very frequently after initial few years of LT. These patients tend to assess periodic liver biochemistry and communicate with the transplant centre. This was done by 20 of our patients. However, based on study criteria, they were excluded from the study. Studies with larger numbers and including more patients with longer follow-ups would be ideal to address noncompliance comprehensively.
In conclusion, as the aim of liver transplantation is to provide a better and productive life to the recipient, drug adherence remains central to the management. The present study highlights the problems faced by Indian patients in the posttransplant period. Multidisciplinary teams including professional educators, psychologists, social workers, surgeons and physicians can ensure drug adherence.
For the future, the present questionnaire needs validation. Patient-friendly regimens, drug reminder apps, medication folders and cost-effective transplant management are needed to ensure enhanced adherence.
Conflicts of interest
The authors have none to declare.
References
- 1.Sabate E., editor. Adherence to Long-Term Therapies: Evidence for Action. World Health Organization; Geneva, Switzerland: 2003. [Google Scholar]
- 2.Laederach-Hofmann K., Bunzel B. Noncompliance in organ transplant recipients: a literature review. Gen Hosp Psychiatry. 2000;22:412–424. doi: 10.1016/s0163-8343(00)00098-0. [DOI] [PubMed] [Google Scholar]
- 3.Rodríguez A., Díaz M., Colón A., Santiago-Delpín E.A. Psychosocial profile of noncompliant transplant patients. Transplant Proc. 1991;23:1807–1809. [PubMed] [Google Scholar]
- 4.Mor E., Gonwa T.A., Husberg B.S., Goldstein R.M., Klintmalm G.B. Late-onset acute rejection in orthotopic liver transplantation—associated risk factors and outcome. Transplantation. 1992;54:821–824. doi: 10.1097/00007890-199211000-00010. [DOI] [PubMed] [Google Scholar]
- 5.O'Carroll R.E., McGregor L.M., Swanson V., Masterton G., Hayes P.C. Adherence to medication after liver transplantation in Scotland: a pilot study. Liver Transplant. 2006;12:1862–1868. doi: 10.1002/lt.20828. [DOI] [PubMed] [Google Scholar]
- 6.Stilley C.S., DiMartini A.F., de Vera M.E. Individual and environmental correlates and predictors of early adherence and outcomes after liver transplantation. Prog Transplant. 2010;20:58–66. doi: 10.7182/prtr.20.1.c903845857104k83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hathaway D.K., Combs C., De Geest S., Stergachis A., Moore L.W. Patient compliance in transplantation: a report on the perceptions of transplant clinicians. Transplant Proc. 1999;31:10S–13S. doi: 10.1016/s0041-1345(99)00113-x. [DOI] [PubMed] [Google Scholar]
- 8.Dobbels F., Vanhaecke J., Desmyttere A., Dupont L., Nevens F., De Geest S. Prevalence and correlates of self-reported pretransplant nonadherence with medication in heart, liver, and lung transplant candidates. Transplantation. 2005;79:1588–1595. doi: 10.1097/01.tp.0000158430.06507.87. [DOI] [PubMed] [Google Scholar]
- 9.Schweizer R.T., Rovelli M., Palmeri D., Vossler E., Hull D., Bartus S. Noncompliance in organ transplant recipients. Transplantation. 1990;49:374–377. doi: 10.1097/00007890-199002000-00029. [DOI] [PubMed] [Google Scholar]
- 10.Berlakovich G.A., Langer F., Freundorfer E. General compliance after liver transplantation for alcoholic cirrhosis. Transpl Int. 2000;13:129–135. doi: 10.1007/s001470050298. [DOI] [PubMed] [Google Scholar]
- 11.Drent G., Haagsma E.B., Geest S.D. Prevalence of prednisolone noncompliance in adult liver transplant recipients. Transpl Int. 2005;18:960–966. doi: 10.1111/j.1432-2277.2005.00170.x. [DOI] [PubMed] [Google Scholar]
- 12.Sharma R. Indian Pediatr; 2017 Aug 26. Revised Kuppuswamy's Socioeconomic Status Scale: Explained and Updated. pii: S097475591600090. [PubMed] [Google Scholar]
- 13.Miloh T., Annunziato R., Arnon R. Improved adherence and outcomes for pediatric liver transplant recipients by using text messaging. Pediatrics. 2009;124:e844–e850. doi: 10.1542/peds.2009-0415. [DOI] [PubMed] [Google Scholar]
- 14.Lieber S.R., Volk M.L. Nonadherence and graft failure in adult liver transplant recipients. Dig Dis Sci. 2013;58:824–834. doi: 10.1007/s10620-012-2412-0. [DOI] [PubMed] [Google Scholar]
- 15.Rovelli M., Palmeri D., Vossler E., Bartus S., Hull D., Schweizer R. Noncompliance in organ transplant recipients. Transplant Proc. 1989;21:833–834. [PubMed] [Google Scholar]
- 16.Dobbels F., Vanhaecke J., Dupont L. Pretransplant predictors of posttransplant adherence and clinical outcome: an evi-dence base for pretransplant psychosocial screening. Transplantation. 2009;87:1497–1504. doi: 10.1097/TP.0b013e3181a440ae. [DOI] [PubMed] [Google Scholar]
- 17.Sharma A., Agrawal A. Complementary and alternative medicine (CAM) use among patients presenting in out-patient department at tertiary care teaching hospital in southern Rajasthan, India – a questionnaire based study. Altern Integr Med. 2015;4:187. [Google Scholar]
- 18.Pera M., Garcı'a-Valdecasas J.C., Grande L. Liver transplantation for alcoholic cirrhosis with anti-HCV antibodies. Transplant Int. 1997;10:289–292. doi: 10.1007/s001470050059. [DOI] [PubMed] [Google Scholar]
- 19.Mackie J., Groves K., Hoyle A. Orthotopic liver transplantation for alcoholic liver disease: a retrospective analysis of survival, recidivism, and risk factors predisposing to recidivism. Liver Transplant. 2001;7:418–427. doi: 10.1053/jlts.2001.23789. [DOI] [PubMed] [Google Scholar]
- 20.Tome S., Lucey M.R. Timing of liver transplantation in alcoholic cirrhosis. J Hepatol. 2003;39:302–307. doi: 10.1016/s0168-8278(03)00290-3. [DOI] [PubMed] [Google Scholar]
- 21.Shemesh E., Annunziato R.A., Shneider B.L. Improving adherence to medications in pediatric liver transplant recipients. Pediatr Transplant. 2008;12:316–323. doi: 10.1111/j.1399-3046.2007.00791.x. [DOI] [PubMed] [Google Scholar]
- 22.Annunziato R.A., Emre S., Shneider B.L. Transitioning healthcare responsibility from caregivers to patient: a pilot study aiming to facilitate medication adherence during this process. Pediatr Transplant. 2008;12:309–315. doi: 10.1111/j.1399-3046.2007.00789.x. [DOI] [PubMed] [Google Scholar]
- 23.Borella V., Germani G., Lazzaro S. Psychoeducational intervention to improve patient adherence after liver transplantation [abstract] Liver Transplant. 2010;16:S229. [Google Scholar]