Abstract
While adverse childhood experiences (ACEs), as described by the CDC-Kaiser Permanente Study, are reportedly common in both high and low-income settings, evidence on the epidemiology of ACEs in low-income settings is scarce. This study aimed to determine the prevalence of ACEs reported in young adulthood and assess their association with childhood maternal, household and community factors. We used data from the 22–23 year wave of the Birth to Twenty Plus (Bt20+) study in South Africa, the largest and longest running birth cohort in Africa. With ACEs as the main outcome measure, their association with childhood factors was assessed using regression models. As demonstrated in high-income settings, ACEs are highly prevalent in this young adult population in a middle income country. Both household and community socio-economic status in childhood was associated with the experience of ACEs and the likelihood of experiencing multiple ACEs. The attenuation of significance in adjusted models suggested that individual ACEs are correlated and may exert their effects through other ACEs. Interventions for the prevention of ACEs need to be directed not only at individuals but households as well as communities.
Keywords: Developmental biology, Epidemiology, Public health, Quality of life, Interrelated, Abuse, Clustering, Household dysfunction, ACE score, Adverse childhood experiences, Neglect, Adversity, Early childhood development
Developmental biology; Epidemiology; Public health; Quality of life; Interrelated; Abuse; Clustering; Household dysfunction; ACE score; Adverse childhood experiences; Neglect; Adversity; Early childhood development.
1. Introduction
Extensive research has been conducted globally on childhood abuse and maltreatment and their effect on health and well-being [1]. However, the concept of adverse childhood experiences (ACEs) as a set of specified exposures was first described in the seminal “CDC-Kaiser Permanente Adverse Childhood Experiences (ACE) Study” [2]. The ACE study described adverse experiences as “common, stressful and traumatic exposures affecting the (neuro) development of children” [3]. The ACE hypothesis posits that adverse or stressful childhood experiences such as abuse and neglect, or growing up in a dysfunctional household, create common vulnerability to social, emotional and cognitive impairments that lead to increased risk of poor health behavior, social adjustment and physical and mental illness [3]. ACEs are more than child maltreatment and the neglect of a child's needs, and incorporate household and environmental influences as well [1].
The first wave of the study conducted in 1995/1996 included seven adverse events in the definition of ACEs, namely sexual, physical and emotional abuse, and household dysfunction (household substance abuse, household mental illness, domestic violence and household member with a history of imprisonment) [2]. The second wave in 1997 updated the list to ten with the addition of emotional and physical neglect and parental divorce or separation [2, 3, 4]. The latter study also became the basis for expert recommendations to expand the definition of ACEs to include exposures experienced in high income as well as low to middle income countries (LMICs), including the domains of socio-economic status, peer to peer and community violence [5].
Adverse childhood experiences are common, in both high income and LMICs. In the ACE study, approximately 60% of the sample experienced at least one ACE and more than 10 percent experienced 5 or more ACEs [3]. A later survey in the USA also found a 60 percent prevalence of at least one ACE, and data from Wales showed a 47% prevalence [6, 7]. Eighty-five percent of a Brazilian adolescent cohort reported experiencing at least one ACE, with females experiencing more adverse events [8]. In Vietnam, 76% of a sample of university students reported experiencing at least one ACE [9]. Though not using the ACE definition stated above, studies conducted in South Africa suggest high rates of individual exposures. For example, in a prospective survey of both rural and urban adolescents, 18.3% and 19.5% reported frequent physical and emotional abuse, respectively [10]. According to Jewkes et.al, 54.7% and 56.4% of rural South African women and men experienced emotional abuse respectively, 41.6% and 39.6%, respectively experienced emotional neglect and 39.1% and 16.7% experienced sexual abuse before the age of 18 [11].
ACEs have a cumulative impact on health and well-being [1]. In order to measure this more accurately, Felitti et al. proposed computing an ACE score, which is the sum of the defined exposures, measured dichotomously, ranging from 0-10 [2,4,12]. Strong dose-response relationships have been observed between the ACE score and adult health outcomes [13, 14, 15]. Higher ACE scores are not only associated with increased health risk behaviours and risk of disease and poor social adjustment, but also with increased odds of reporting multiple adverse outcomes [7, 16]. Examining the ACEs as a set of exposures and using the cumulative ACE score enables these relationships with health and wellbeing outcomes to be more precisely elucidated and quantified.
Scientific advances support the assertion that early life stress disrupts neurodevelopment, leaving lasting effects on brain structure and function [17]. Early life adversity can produce biological memories that weaken multiple developing body systems such as the stress response, cardiovascular and immune systems, and metabolic regulatory controls [18, 19]. Childhood maltreatment has been linked to reduced grey matter volumes in the hippocampus and the orbitofrontal cortex among other brain regions [20, 21]. These effects can last well into adulthood and have been linked to poor health and behavioral outcomes [18, 19].
Several child, household and community factors have been linked to childhood maltreatment and abuse. Girls are reported to have a higher risk of being sexually abused than boys, as well as experiencing greater adversity in general [8, 22]. Household factors such as HIV-related illness and poverty may increase the risk of child abuse [10]. In Brazil, being of non-White race, low family income, low maternal schooling, absence of mother's partner, maternal smoking, and poor maternal mental health significantly increased the risk of a higher ACE score [8]. Living in a poor neighborhood is associated with a higher number of ACEs and conversely, neighborhoods with large numbers of affluent families are associated with lower ACE scores [12]. Child maltreatment is usually concentrated in poorer neighborhoods and neighborhood structural factors, particularly economic markers, are consistently linked to abuse and neglect. Socio-economic context also potentially confounds the relationship between ACEs and outcomes in later life [12]. Children who have previously been maltreated are also at an increased risk of being maltreated again [23].
There is evidence from high-income countries on the prevalence of ACEs, as defined by the ACE study, but such research is scarce in LMICs. Partly due to the paucity of data, the study of child adversity has tended to focus on single exposures such as sexual or physical abuse, despite emerging evidence that ACEs co-occur and are interrelated [4, 14]. The objectives of this study are to determine the prevalence of ACEs, as defined in the ACE study, together with additional measures relevant to an LMIC, and to assess their association with childhood maternal, household and community factors in a long-term birth cohort study in South Africa.
2. Methods
2.1. Study design and context
A cross-sectional analysis of data from the Birth to Twenty Plus (Bt20+) study was conducted. Bt20+ is the longest running birth cohort in Africa, following up urban children and tracking their growth, health, well-being and educational progress [24]. Based in Soweto, Johannesburg, a densely populated suburb in the Greater Johannesburg Metropolitan area, the study began at the dawn of freedom from the Apartheid regime in South Africa, a time characterized by increased freedom of movement and rapid unplanned urbanization [24]. The Apartheid regime created a system of so-called race classification which legally differentiated between Whites of European origin, Indians (a collection of different people from the South East Asian region, mainly from India), Coloreds (people of mixed ancestry) and Black people (of African descent). Participation in society was differentiated in freedom and quality on a continuum from Whites to Indians to Coloreds to Black people. The terminology is retained because it carries the legacy of decades of oppression and discrimination, the effects of which are still evident [24]. Data for this study come from data collected when the cohort was aged between 22 and 23 years and measured, among other things, education and employment, general health, ACEs, as well as general life events.
2.2. Participants/study population
At the start, 3 273 singleton children born to women who resided in Soweto between April and June 1990 and resident in the area for at least six months post-partum were recruited into the study [24]. Of these, 1 636 participants were surveyed at 22–23 years of age.
2.3. Measures
The main outcome measure is adverse childhood experiences (ACEs). Demographic factors of the participants in young adulthood were collected to describe the sample. Additional measures included maternal, household and community factors measured between birth and 18 years. All questionnaires were administered face-to-face, bar the ACE questionnaire which was completed by the participant.
2.3.1. Demographic factors at 22 years
Demographic information included marital status, socio-economic status and graduation from high school. Marital status is a binary variable with the categories single/widowed/divorced and married or living together. The latter were collapsed together because cohabitation is common at that age in South Africa, with the median age at first marriage 30 and 34 years for females and males respectively between 2009 and 2013 [25,26]. Socio-economic status was measured using a sum of household assets and analyzed as a continuous variable. The young adults were asked whether they had graduated from secondary school or not, and this variable is also binary.
2.3.2. Adverse childhood experiences
ACEs were retrospectively measured at 22–23 years of age using a modified Adverse Childhood Experiences Study Questionnaire [4]. The questionnaire was self-administered. A total of thirteen ACEs were assessed in this study. Data on chronic illness, unemployment and parental death were also collected in addition to the ten ACEs [4] used in the ACE study based on recommendations to include some experiences that may be prevalent in low-income settings [5, 27, 28]. Five of the ACEs were the child's own experience of abuse or neglect and the remainder were household experiences namely witnessing domestic violence, parental divorce, parental death, substance abuse in the household, a household member being incarcerated and mental illness and other chronic illness of a household member and unemployment of a parent or caregiver. Table 1 in Supplementary Information shows the questions used to assess ACEs experienced. A point was allocated to each ACE exposure for which a participant answered yes to at least one of the questions, i.e. only one point could be allocated to each ACE.
Table 1.
Prevalence of ACEs and demographic factors of participants surveyed in the 22–23 year wave of the Bt20 + survey, Soweto, South Africa, n = 1636.
| Variable | Male n (%) | Female n (%) | Total n (%) | Percent missing data (based on sample of 1636) | p-value (chi2 and ANOVA) |
|---|---|---|---|---|---|
| Marital status | |||||
| Single | 414 (55) | 371 (45) | 785 (50) | ||
| Relationship | 341 (45) | 450 (55) | 791 (50) | 1.5 | 0.000 |
| SES at 22 years | Median: 10 (Range 1–13) | Median: 10 (Range 1–13) | 2.2 | 0.583 | |
| Completed secondary education | |||||
| No | 356 (47) | 263 (32) | 619 (40) | ||
| Yes | 401 (53) | 548 (68) | 949 (60) | 3.0 | 0.000 |
| Any ACEa | |||||
| No | 72 (12) | 77 (12) | 149 (12) | ||
| Yes | 520 (88) | 549 (88) | 1069 (88) | 5.0 | 0.941 |
| Cumulative ACEs_5a | |||||
| None | 72 (12) | 77 (12) | 149 (12) | ||
| 1 ACE | 106 (18) | 135 (22) | 241 (20) | ||
| 2 ACEs | 106 (18) | 108 (17) | 214 (18) | ||
| 3 ACEs | 93 (16) | 91 (15) | 184 (15) | ||
| 4 or more | 215 (36) | 215 (34) | 430 (35) | 23.0 | 0.600 |
| Cumulative ACEs_3a | |||||
| None | 72 (12) | 77 (12) | 149 (12) | ||
| Low | 434 (73) | 452 (72) | 886 (73) | ||
| High | 86 (15) | 97 (16) | 183 (15) | 23.0 | 0.884 |
| ACE score | Median: 3 (Range: 0–11) | Median: 3 (Range0-11) | Median: 3 (Range 0–11) | 23.0 | 0.983 |
| Emotional abuse | |||||
| No | 519 (69) | 572 (70) | 1091 (70) | ||
| Yes | 232 (31) | 240 (30) | 472 (30) | 1.7 | 0.566 |
| Sexual abuse | |||||
| No | 707 (97) | 754 (95) | 1461 (96) | ||
| Yes | 22 (3) | 40 (5) | 62 (4) | 5.0 | 0.046 |
| Physical abuse | |||||
| No | 665 (91) | 742 (93) | 1407 (92) | ||
| Yes | 67 (9) | 52 (7) | 119 (8) | 4.9 | 0.048 |
| Emotional neglect | |||||
| No | 555 (74) | 562 (69) | 1117 (71) | ||
| Yes | 198 (26) | 252 (31) | 450 (29) | 1.4 | 0.041 |
| Physical neglect | |||||
| No | 648 (86) | 734 (90) | 1382 (88) | ||
| Yes | 103 (14) | 78 (10) | 181 (12) | 1.7 | 0.011 |
| Domestic violence | |||||
| No | 657 (88) | 700 (87) | 1357 (87) | ||
| Yes | 93 (12) | 108 (13) | 201 (13) | 2.0 | 0.570 |
| Parental divorce/separation | |||||
| No | 357 (56) | 369 (54) | 726 (55) | ||
| Yes | 281 (44) | 311 (46) | 592 (45) | 17.0 | 0.537 |
| Parental death | |||||
| No | 521 (69) | 602 (74) | 1123 (72) | ||
| Yes | 231 (31) | 212 (26) | 443 (28) | 1.5 | 0.040 |
| Substance abuse | |||||
| No | 521 (69) | 613 (75) | 1134 (72) | ||
| Yes | 233 (31) | 204 (25) | 437 (28) | 1.2 | 0.009 |
| Mental illness | |||||
| No | 674 (90) | 707 (87) | 1381 (88) | ||
| Yes | 79 (10) | 110 (13) | 189 (12) | 1.3 | 0.071 |
| Incarceration | |||||
| No | 552 (73) | 652 (80) | 1204 (77) | ||
| Yes | 202 (27) | 163 (20) | 365 (23) | 1.3 | 0.001 |
| Chronic illness | |||||
| No | 562 (75) | 591 (73) | 1153 (74) | ||
| Yes | 191 (25) | 222 (27) | 413 (26) | 1.5 | 0.384 |
| Unemployment | |||||
| No | 409 (54) | 479 (59) | 888 (57) | ||
| Yes | 345 (46) | 338 (41) | 683 (43) | 1.2 | 0.080 |
Totals add up to 1218 due to cross-tabulation with gender: five of those with full ACE data had missing gender data.
ACEs were analyzed as single variables and as an ACE score which was computed by summing the number of ACEs to which each person was exposed. Several categorical variables were created based on the ACE score:
-
1.
Binary variables were created to indicate the proportion of participants who had experienced at least one, two, three, four, five or six ACEs in their lifetime.
-
2.
A variable with five ACE score categories was created to indicate those who experienced no ACEs, one, two, three and four or more ACEs, to allow comparability with similar studies.
2.3.3. Child, maternal, household and community factors
These variables were collected between pregnancy and two years of age, at 16 years of age as well as at 18 years of age. Questionnaires were administered by trained research assistants to the caregivers or the participants themselves.
2.4. Participant's gender
The participant's gender was recorded at birth.
2.5. Mother's age at birth
The mother's age in years was collected during the antenatal visit.
2.6. Mother's education
Information on the mother's highest level of education was collected during the antenatal visit and updated during data collection in the first two years of the child's life. Education was divided into four categories: no formal education, Grades 1–7 (primary), Grades 8–12 (secondary) and post school training.
2.7. Mother's marital status
This variable was measured during the antenatal visit and updated during data collection in the first two years of the child's life, with two categories, namely single/divorced/widowed/separated and married/living together.
2.8. Father's presence
The presence of the participant's father in the household before the age of two was recorded and treated as a dichotomous variable in the analysis.
2.9. Socio-economic status
We assessed socio-economic status (SES) by creating a composite score based on responses to a questionnaire on assets in the household at birth as well as at 16 years of age. Assets include, for example, a refrigerator, motor car, television etc. The total score was used to create a dichotomous variable denoting relatively lower and higher SES. A variable to determine change in SES between the two time-points was also created. In the absence of reliable income data in the Bt20 + Study, household assets have been demonstrated to be a stable proxy for income and purchasing power [29]. Household assets have been widely used to measure SES level and wealth. They are used to indicate the household's ability to endure emergencies and economic shocks and are a measure of cumulative wealth over time [30, 31, 32]. Unpublished work by the study team showed that the asset data, combined in several ways, remains stable [33]. At 18 years of age the participants were asked questions regarding the SES of their community. For this analysis we created a community SES variable from two of these questions: “How do you describe your neighborhood in terms of wealth?” and “Do you think people living outside of your neighborhood see your neighborhood as being: very poor, poor, average, wealthy or very wealthy?” The same response options were used for the first question as well. A dichotomous variable was created by summing the scores of the two questions and defining a score of five or less as lower community SES and a score above five as higher community SES. SES at 22 years was used as a continuous variable.
2.10. Statistical analysis
All analyses were carried out using STATA version 14.2 [34].
2.10.1. Descriptive statistics
The prevalence of each ACE exposure was determined and tabulated by gender, as well as demographic characteristics of the sample. The chi-square test and ANOVA were used to examine gender differences.
2.10.2. Association between childhood factors and ACEs
Univariate and multivariate logistic regression was used to test associations between childhood factors and ACEs: the binary ACE variable indicating the experience of any ACE, the cumulative ACE score index, and the individual ACEs. Variables significant at the 80% level in the univariate analysis were retained in the multivariate models.
2.11. Ethics
Ethics approval for the Bt20 + study was obtained from the Human Research Ethics Committee of the University of the Witwatersrand Clearance Certificate Number: M111182. Approval for this analysis was sought from the same: Clearance Number: M160921. All participants and/or their caregivers gave informed written consent for the data reported.
3. Results
3.1. Characteristics of the sample and prevalence of ACEs
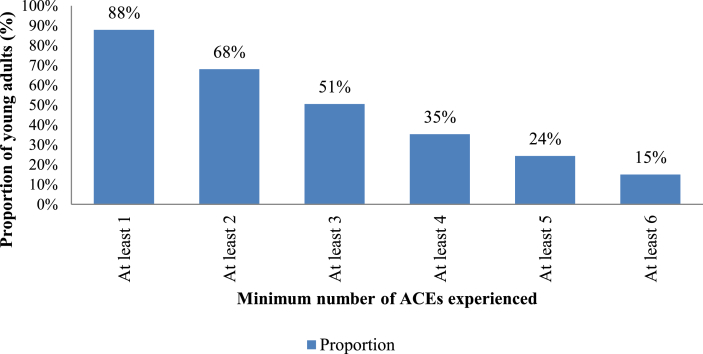
Figure 1 presents the sample flowchart displaying the number of participants in the present analysis. Table 1 presents the descriptive statistics of the sample surveyed at 22 years of age. Forty-eight percent of the sample was male and 52% female. Sexual and physical abuse were the lowest reported ACEs (4% and 8% respectively), while unemployment of a parent or caregiver and parental divorce or separation had the highest prevalence at 43% and 45% respectively. The prevalence of the other two additional ACEs, parental death and chronic illness, were also among the highest reported, 28% and 26% respectively. Significant differences between males and females in education and marital status at 22 years of age were apparent. There were also significant differences between males and females in the experience of sexual abuse, emotional and physical neglect, parental death, household substance abuse, mental illness and legal trouble or incarceration of a household member.
Figure 1.
Bt20 + sample flow chart Flow diagram showing how the analytical sample was derived.
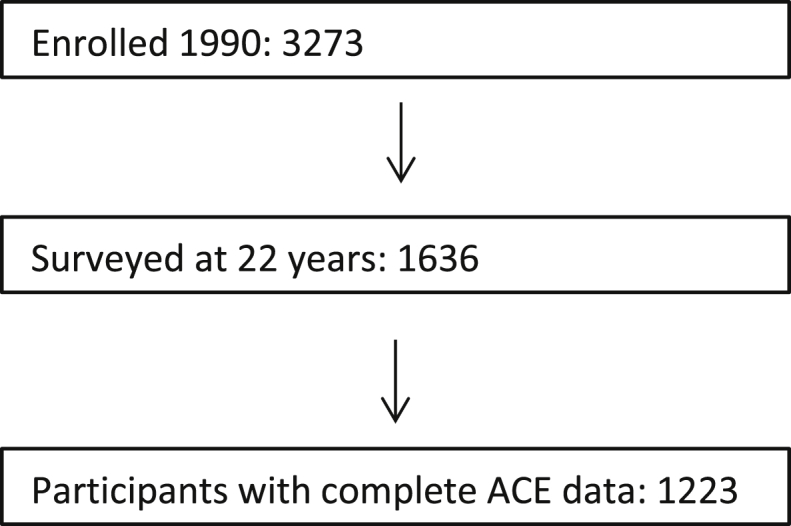
Of the 1636 participants who were surveyed at 22 years of age, 1223 had complete ACE data i.e. data on all the ACEs as reflected in the ACE score variables. Twelve percent of these (149) reported no ACEs and 1074 (88%) reported at least one ACE. The highest ACE score for this sample was 11 out of 13. Over one third of respondents reported experiencing four or more ACEs and 15% experienced 6 or more ACEs as indicated in Figure 2. Those who had full ACE data were used in the regression models.
Figure 2.
Proportion of young adults experiencing a minimum number of ACEs. The bar chart illustrates the proportion of the sample that reported a minimum of one up to six ACEs.
3.2. Missing data
Included in Table 1 is a column illustrating the percentage of participants with missing data for each variable, based on the sample surveyed of 1636 participants. All the variables except for parental divorce had less than 10% missing values. Out of the 1223 young adults that had complete ACE data, one percent had missing marital status data, and approximately two percent had missing education and SES data. Table 2 in Supplementary Information displays how the demographic characteristics of participants who had full ACE data compared those that had incomplete ACE data. Having incomplete ACE data was correlated to marital status and secondary school completion. We also compared the childhood factors of those surveyed at 22 years old and those not surveyed (results not presented). A significant difference was noted in SES at sixteen and eighteen years of age, with those who were surveyed more likely to be of a higher SES level.
Table 2.
Adjusted childhood factors associated with individual abuse and neglect ACEs in the Bt20 + Study, Soweto, South Africa, n = 1223.
| Variable | Abuse: Adjusted OR (95% CI) |
Neglect: Adjusted OR (95% CI) |
|||
|---|---|---|---|---|---|
| Sexual | Emotional | Physical | Physical | Emotional | |
| Gender | |||||
| Male | Ref | - | Ref | Ref | Ref |
| Female | 1.67 (0.93–3.00) | 0.70 (0.46–1.08) | 0.67 (0.45–0.99) | 1.18 (0.91–1.53) | |
| Maternal age | -ˆ | - | - | - | - |
| Maternal education | |||||
| No formal education | Ref | - | - | - | - |
| Standard 1-5 | 0.17 (0.02–1.85) | ||||
| Standard 6-10 | 0.34 (0.04 (2.86) | ||||
| Post school training | 0.80 (0.09–7.38) | ||||
| Maternal marital status | |||||
| Single/widowed | - | Ref | - | Ref | - |
| Married/living together | 0.82 (0.62–1.09) | 0.75 (0.48–1.18) | |||
| SES at birth | |||||
| Low | Ref | Ref | Ref | Ref | - |
| High | 1.42 (0.80–2.53) | 0.87 (0.67–1.14) | 0.79 (0.50–1.24) | 0.67 (0.40–1.14) | |
| SES at 16 years | |||||
| Low | - | Ref | Ref | Ref | Ref |
| High | 0.98 (0.73–1.31) | 0.93 (0.57–1.51) | 0.55 (0.34–0.88) | 0.83 (0.62–1.12) | |
| Change in SES (birth to 16 years) | |||||
| None | - | - | - | Ref | Ref |
| Increase | 0.94 (0.55–1.61) | 1.23 (0.89–1.70) | |||
| Decrease | 1.73 (0.96–3.11) | 1.18 (0.80–1.73) | |||
| Community SES at 18 | |||||
| Low | Ref | Ref | Ref | Ref | Ref |
| High | 0.55 (0.31–0.98) | 0.70 (0.53–0.93) | 0.81 (0.50–1.29) | 0.54 (0.36–0.81) | 0.66 (0.50–0.88) |
| Father home | |||||
| No | - | - | - | Ref | - |
| Yes | 0.67 (0.41–1.09) | ||||
Bold: p < 0.05; ˆvariables with no results were not entered into multivariate model for that outcome.
3.3. Maternal, household and community factors associated with experiencing single ACE exposures
We explored the association of childhood factors with single ACE exposure, and the adjusted regressions are presented in Tables 2 and 3. Higher SES, both in the household (at birth and at 16 years of age) and in the community were significantly negatively associated with several ACE exposures such as physical neglect, sexual and emotional abuse and drug abuse. Community SES remained significantly associated with sexual and emotional abuse as well as physical and emotional neglect, with those residing in higher SES communities having more than 50% fewer odds of experiencing these ACEs. Participants who had older mothers at birth were less likely to witness domestic violence and live with a chronically ill household member compared to those who had younger mothers.
Table 3.
Adjusted childhood factors associated with individual household dysfunction ACEs in the Bt20 + Study, Soweto, South Africa, n = 1223.
| Variable | Household dysfunction Adjusted OR (95% CI) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Domestic violence | Parental divorce | Parental death | Substance abuse | Mental illness | Incarceration | Chronic illness | Unemployment | |
| Gender | ||||||||
| Male | -ˆ | - | Ref | Ref | Ref | - | - | Ref |
| Female | 0.79 (0.61–1.02) | 0.76 (0.59–0.99) | 1.39 (1.00–1.92) | 0.77 (0.61–0.98) | ||||
| Mother's age | 0.96 (0.93–0.99) | 0.98 (0.96–1.00) | - | - | - | 0.99 (0.97–1.01) | 0.98 (0.95–0.99) | 0.98 (0.96–1.00) |
| Mother's education | ||||||||
| No formal education | - | - | Ref | - | - | - | - | - |
| Standard 1-5 | 1.53 (0.31–7.42) | |||||||
| Standard 6-10 | 1.65 (0.35–7.75) | |||||||
| Post school training | 1.18 (0.23–6.02) | |||||||
| Marital status | ||||||||
| Single/widowed | - | Ref | Ref | Ref | - | - | Ref | Ref |
| Married/living together | 0.69 (0.51–0.94) | 0.76 (0.57–1.02) | 1.33 (1.02–1.73) | 1.05 (0.77–1.44) | 0.72 (0.54–0.96) | |||
| SES at birth | ||||||||
| Low | - | Ref | Ref | Ref | - | Ref | Ref | Ref |
| High | 0.94 (0.72–1.23) | 0.86 (0.66–1.12) | 0.68 (0.52–0.90) | 0.77 (0.58–1.03) | 0.84 (0.65–1.09) | 0.71 (0.55–0.91) | ||
| SES at 16 years | ||||||||
| Low | Ref | Ref | - | Ref | Ref | - | Ref | |
| High | 0.77 (0.54–1.10) | 0.63 (0.47–0.86) | 0.74 (0.55–0.99) | 1.28 (0.88–1.86) | 0.79 (0.58–1.07) | 0.51 (0.39–0.68) | ||
| Change in SES (birth to 16 years) | ||||||||
| None | ||||||||
| Increase | ||||||||
| Decrease | - | - | - | - | - | - | - | - |
| Community SES at 18 years | ||||||||
| Low | Ref | Ref | ||||||
| High | - | - | - | 0.79 (0.59–1.05) | - | - | 0.88 (0.66–1.18) | - |
| Father home | ||||||||
| No | Ref | Ref | Ref | - | - | - | Ref | Ref |
| Yes | 1.50 (0.91–2.46) | 0.65 (0.44–0.98) | 0.63 (0.45–0.88) | 0.98 (0.69–1.41) | 0.93 (0.67–1.29) | |||
Bold: p < 0.05; ˆvariables with no results were not entered into multivariate model for that outcom.
3.4. Maternal, household and community factors associated with cumulative ACEs
The associations between childhood factors and cumulative ACEs are presented in Table 4. Only maternal marital status and SES at 16 years of age remained significantly associated with experiencing at least one ACE after adjusting for the other factors. The patterns of association and effect sizes were similar for the two ACE score indices. In adjusted analyses, higher household SES at 16 years of age and maternal marital status reduced the odds of ever experiencing ACEs as well as experiencing multiple ACE events. The effect of community SES and SES at birth remained protective but was insignificant after adjusting for the other ACEs.
Table 4.
Unadjusted and adjusted association of childhood factors with cumulative ACE score indices in the Bt20 + Study, Soweto, South Africa, n = 1223.
| Variable | Experiencing at least one ACE |
ACE score categories [5] |
||
|---|---|---|---|---|
| Unadjusted OR (95% CI) | Adjusted OR (95% CI)a | Unadjusted OR (95% CI) | Adjusted OR (95% CI) | |
| Gender | ||||
| Male | Ref | - | Ref | - |
| Female | 0.99 (0.70–1.39) | 0.99 (0.70; 1.39) | ||
| Mother's age | 0.98 (0.96–1.01) | - | 0.98 (0.96; 1.01) | - |
| Mother's education | ||||
| No formal education | Ref | - | Ref | - |
| Standard 1-5 | 0.60 (0.07–4.92) | 0.60 (0.07; 4.92) | ||
| Standard 6-10 | 0.61 (0.08–4.75) | 0.61 (0.08; 4.75) | ||
| Post school training | 0.49 (0.06–4.09) | 0.49 (0.06; 4.09) | ||
| Maternal marital status | ||||
| Single/widowed | Ref | Ref | Ref | Ref |
| Married/living together | 0.54 (0.38–0.76)*** | 0.64 (0.42–0.98)** | 0.54 (0.38–0.76)*** | 0.64 (0.42–0.98)** |
| SES at birth | ||||
| Low | Ref | Ref | Ref | Ref |
| High | 0.78 (0.53–1.14)* | 0.87 (0.52–1.46) | 0.78 (0.53–1.14)* | 0.87 (0.53–1.46) |
| SES at 16 years | ||||
| Low | Ref | Ref | Ref | Ref |
| High | 0.42 (0.27–0.64)*** | 0.51 (0.26–0.99)** | 0.37 (0.22–0.63)*** | 0.51 (0.26–0.99)** |
| Change in SES (birth to 16 years) | ||||
| None | Ref | Ref | Ref | - |
| Decrease | 1.00 (0.65–1.57) | 1.00 (0.58–1.74) | 1.00 (0.65; 1.57) | |
| Increase | 1.48 (0.81–2.69)* | 1.22 (0.63–2.35) | 1.48 (0.81; 2.69) | |
| Community SES at 18 years | ||||
| Low | Ref | Ref | Ref | Ref |
| High | 0.57 (0.36–0.89)** | 0.60 (0.35–1.01) | 0.58 (0.36–0.89)** | 0.60 (0.35–1.01) |
| Father home | ||||
| No | Ref | Ref | Ref | Ref |
| Yes | 0.48 (0.23–1.00)** | 0.56 (0.25–1.27) | 0.48 (0.23; 1.00)* | 0.56 (0.25; 1.27) |
*p ≤ 0.2; **p ≤ 0.05; ***p ≤ 0.001.
Variables significant at 0.2 entered into the adjusted models.
4. Discussion
Our results show that ACEs measured using a modified Kaiser Permanente ACE Study questionnaire, are highly prevalent in a middle-income young adult urban population, with 88% reporting at least one ACE during childhood and 35% experiencing at least four. Using only the original 10 ACE Study exposures, the prevalence of any ACE was 77%, while 21% of the sample reported four or more ACEs. Maternal marital status and age, household and community SES were the most salient childhood factors associated with both single ACEs and the cumulative score. Most associations between childhood factors and single ACE exposures were attenuated by the addition of other factors in the models.
4.1. Prevalence of ACEs
We report prevalence rates higher than those reported in high-income countries, both using the 10-item score and our modified 13-item score [7, 17]. The prevalence of sexual and physical abuse was, however, lower in this study compared to other studies, while most forms of household dysfunction were generally higher, including parental divorce/separation [6, 7, 17]. Differences in the reporting of abuse have been attributed to the type of sample included in the study: random versus purposive or convenience samples, or samples taken from at-risk populations versus general population samples [35]. The age of the victim when the abuse or maltreatment happened as well as the mode of questionnaire administration may also influence self-report rates [36]. A systematic review of literature covering both high income and middle income countries found prevalence rates of experiencing four or more ACEs ranging between one and thirty-two percent, with the highest prevalence being from a middle income country [37]. It seems that ACEs are more prevalent in poorer compared to richer countries, indicative of the urgency of preventing ACEs in these settings that face multiple public health burdens in the context of limited health and social resources.
Our three additional ACEs were fairly prevalent in this study group. These exposures should be taken into account when measuring ACEs in lower income communities. Independent of any association with health outcomes, they may be part of important pathways to illness. Markers of poverty have been linked to childhood sexual and psychological abuse and subsequently symptoms of depression among young South African men [38]. Further analysis with path analysis methods would be beneficial to determine what role these exposures play in the occurrence of ACEs and their link with poor outcomes.
Data on the prevalence of cumulative ACEs are essential for reducing inequality in LMICs. Adverse early life experiences create inequalities by compromising children's development and later health and wellbeing trajectories. These inequalities, which exist within or between populations, originate prenatally and can become more firmly entrenched due to exposure to cumulative adverse experiences [39]. With more than 250 million children below the age of five years in LMICs not reaching their full potential due to developmental risks, ACE prevention becomes a matter of social justice. Early integrated interventions are of critical importance to protect the next generation and are a potentially cost-effective way to prevent age-related disease in adulthood [19, 39].
4.2. Childhood factors
The association between community SES and abuse is an important finding in this generally low SES population. Research shows that both neighborhood disadvantage and affluence have an effect on the experience of ACEs: greater disadvantage increases the risk of high ACE scores while affluence reduces the risk [12]. Many studies have shown that neighborhood factors correlate with maltreatment rates, the most consistent associations being with indicators of the economic status or resources of the neighborhood [40]. Possible explanations that have been put forward for these findings are that the differences are due to exposure to concentrated levels of inequality and disability that are characteristic of poor neighborhoods together with characteristics of the youth living in these areas [12]. Others have postulated that the link is through parental interaction with the environment, with parents who have positive perceptions of their neighborhood context less likely to maltreat their children because of the potential protective capacity of neighborhood supports [41].
Higher household SES was protective against experiencing any ACEs, as well as experiencing four or more ACEs, compared to no ACEs. These findings match those reported by Hatcher et.al with the interpretation that poverty is a key context for children experiencing abuse and maltreatment, and low SES may also compound deleterious effects of the abuse [38]. Household poverty has been reported as a mediator between child maltreatment and chronic illness [10]. Lower household SES may also increase parental stress and thus put children at risk of maltreatment [8]. The association of household SES during childhood with unemployment in the household as an ACE could possibly be an indication of the vicious cycle that can occur in poor households that have limited access to education and other means of improving their status. Interventions to prevent ACEs, therefore, also need to address access to education and socio-economic empowerment for households and communities. Our analysis did not find any significant associations between change in household SES and the experience of ACEs. However, adult household SES for people who have experienced ACEs has been found to mediate the relationships between ACEs and health outcomes [42], potentially creating an enabling environment for socio-economic change that may help to mitigate the effect of ACEs.
Family structure and the absence of the father in the home in childhood have a significant impact on the occurrence of ACEs. Our results show that single maternal marital status was significantly associated with children experiencing more ACEs compared to children whose mothers were married or had a live-in partner. Research on the effect of family structure on overall child well-being indicates that children from two-parent homes fare better, a relationship that is postulated to be mediated by economic resources, parental socialization, and lower family stress [43]. This effect may be due to selection factors in that marriage may not necessarily help to make people feel happy, healthy, secure but that such individuals, who are more likely to be stable parents, are more likely to marry in the first place [43]. In Canada maternal single marital status was also reported to be associated with allegations of child maltreatment [44]. Further evidence from Sub-Saharan Africa suggests independent associations between paternal orphaning and parental absence and children experiencing sexual violence, with girls being at higher risk of sexual abuse [45]. In South Africa, a study conducted in the Western Cape found that family satisfaction ranked lower among households with absent fathers, partly due to limited economic resources [46]. It is also possible that in the present study the divorce and separation captured in the ACEs retrospective report occurred before two years of age and hence the association between divorce/separation as an ACE and absent fathers. Further exploration is needed in this cohort on the role of family structure on the occurrence of ACEs.
4.3. Inter-relation and co-occurrence of ACEs
The attenuation of associations between childhood factors and some of the ACEs in the adjusted models points to possible interrelationships between the ACEs, with some ACEs potentially acting as mediators. For example, household poverty has been found to mediate the association between chronic illness in the household and child maltreatment [10].
The cumulative risk hypothesis posits that additive risk factors increase the probability of adverse outcomes [47, 48]. Use of the ACE score to capture the co-occurrence and cumulative impact of ACEs is coherent with this, as well as with evidence emerging from the neuroscientific field. Prolonged exposure to maltreatment early in life and attendant increases in stress hormones can influence the structural and functional plasticity of the brain, which in turn can affect patterns of emotional expression and regulation, stress reactivity, recovery, and coping, and perhaps even the rate of bodily aging [49]. The investigation of childhood maltreatment needs to go beyond examination of single abuse exposures to investigating the household environment as well. The presence of one ACE should elicit a search for others, taking into account that the apparent effects of one ACE may not necessarily be attributable to that ACE alone.
4.4. Strengths and limitations of study
To our knowledge this is the first study to investigate the prevalence of ACEs in an African country using an extended definition to that of the Kaiser Permanente ACE study [4]; as such, it adds to the still scant body of evidence from LMICs [37]. We were able to use longitudinally collected childhood factors to investigate their impact on the reporting of ACEs experienced during the first 18 years of life. These results add to the body of knowledge on the prevalence of ACEs in LMICs and contribute to disentangling the intricate connections between them. The availability of robust local data from a long-running cohort study also means the findings are immediately relevant to the context [50].
Limitations of this study were firstly, as was done in the CDC-Kaiser Permanent Study; the experience of ACEs was retrospectively measured and open to recall bias. Contemporary individual characteristics such as chronic stress may influence the recall of some events [28]. The participant may also have experienced adverse events very early in childhood that they may not recall. Secondly, due to the analysis being cross-sectional, temporality could not be stablished. There was no data available on the exact time of the experiences, how intense the abuse was and how long it lasted. Nonetheless, the use of an ACE score gives some indication of multiple, though not necessarily repeated or enduring, exposure. Some of the childhood factors may have changed between birth and 18 years of age and this was not accounted for. Face-to-face interviews for the demographic questionnaires may also have caused reporting bias, for example over-reporting of SES. The community SES variable was derived from questions that may be subjective, but no other measures of community wealth were available.
1636 participants from the original cohort were surveyed at 22 years of age, an attrition rate of 50%. In addition, only 1223 of those surveyed had complete ACE data and were used in the modelling analyses. Table 3 in Supplementary Information shows a comparison of demographic characteristics between participants surveyed at 22 with full ACE data and those surveyed but with missing ACE data. There were no differences in gender and SES. However those who were not surveyed were less likely to be married and to have completed secondary schooling. Attrition may introduce selection bias where the distribution of unmeasured confounders depends on whether the participants remained in the study or not, threatening the internal validity of the study. It may also compromise external validity and reduce the generalizability of results [51]. We do not claim that our results are generalizable to the entire population of South Africa. However, the cohort was large at the start in order to mitigate the effects of attrition on internal validity.
5. Conclusion
ACEs are highly prevalent in this cohort of young adults. SES is an important factor in the experience of ACEs. This finding is important because the impact of ACEs on behaviors, emotional and social well-being, and physical health has been shown to be cumulative [11, 13, 15, 22, 52]. Parents, households and communities need help and support to create and maintain environments that are conducive for healthy child and adolescent development. A multi-setting, multi-sector approach is needed to coordinate service provision in areas that seem unrelated, such as employment and income protection, community safety, drug and alcohol rehabilitation, treatment of mental illness and rehabilitation of ex-convicts, all of which have a major impact on the home environment and hence child development.
Declarations
Author contribution statement
Mercy Manyema: Conceived and designed the experiments; Analyzed and interpreted the data; Wrote the paper.
Linda Richter: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Competing interest statement
The authors declare no conflict of interest.
Funding statement
The Birth to Twenty Plus Study was funded by the SA Medical Research Council, the Wellcome Trust (UK), the Human Sciences Research Council and the University of the Witwatersrand, Johannesburg. MM and LMR are supported by the DST-NRF Centre of Excellence (CoE) in Human Development at the University of the Witwatersrand, Johannesburg, South Africa. None of the funders had a role in the design of the study and collection, analysis and interpretation of data, and in writing the manuscript. The support of the DST-NRF Centre of Excellence in Human Development at the University of the Witwatersrand, Johannesburg, South Africa towards this research is hereby acknowledged. Opinions expressed and conclusions arrived at, are those of the authors and are not to be attributed to the CoE in Human Development.
Additional information
No additional information is available for this paper.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Kalmakis K.A., Chandler G.E. Adverse childhood experiences: towards a clear conceptual meaning. J. Adv. Nurs. 2014;70(7):1489–1501. doi: 10.1111/jan.12329. [DOI] [PubMed] [Google Scholar]
- 2.Felitti V.J., Anda R.F., Nordenberg D., Williamson D.F., Spitz A.M., Edwards V. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the Adverse Childhood Experiences (ACE) Study. Am. J. Prev. Med. 1998;14(4):245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 3.Anda R., editor. Conference in Anacortes. WA on June; 2007. The health and social impact of growing up with adverse childhood experiences: the human and economic costs of the status quo. [Google Scholar]
- 4.Dong M., Anda R.F., Felitti V.J., Dube S.R., Williamson D.F., Thompson T.J. The interrelatedness of multiple forms of childhood abuse, neglect, and household dysfunction. Child Abuse Neglect. 2004;28(7):771–784. doi: 10.1016/j.chiabu.2004.01.008. [DOI] [PubMed] [Google Scholar]
- 5.Anda R.F., Butchart A., Felitti V.J., Brown D.W. Building a framework for global surveillance of the public health implications of adverse childhood experiences. Am. J. Prev. Med. 2010;39(1):93–98. doi: 10.1016/j.amepre.2010.03.015. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention . Centers for Disease Control and Prevention; Atlanta, GA, USA: 2009. Adverse Childhood Experiences Reported by Adults — Five States. 2010 December 2010. Report No. [Google Scholar]
- 7.Bellis M.A., Ashton Kathryn, Hughes Karen, Ford Katharine, Bishop Julie, Paranjothy Shantini. Public Health Wales Centre for Public Health, Liverpool John Moores University; Wales: 2015. Adverse Childhood Experiences and Their Impact on Health-Harming Behaviours in the Welsh Adult Population. [Google Scholar]
- 8.Soares A.L.G., Howe L.D., Matijasevich A., Wehrmeister F.C., Menezes A.M., Gonçalves H. Adverse childhood experiences: prevalence and related factors in adolescents of a Brazilian birth cohort. Child Abuse Neglect. 2016;51:21–30. doi: 10.1016/j.chiabu.2015.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tran Q.A., Dunne M.P., Vo T.V., Luu N.H. Adverse childhood experiences and the health of university students in eight provinces of Vietnam. Asia Pac. J. Public Health. 2015;27(8_suppl):26S–32S. doi: 10.1177/1010539515589812. [DOI] [PubMed] [Google Scholar]
- 10.Meinck F., Cluver L.D., Boyes M.E. Household illness, poverty and physical and emotional child abuse victimisation: findings from South Africa’s first prospective cohort study. BMC Public Health. 2015;15(1):444. doi: 10.1186/s12889-015-1792-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jewkes R.K., Dunkle K., Nduna M., Jama P.N., Puren A. Associations between childhood adversity and depression, substance abuse and HIV and HSV2 incident infections in rural South African youth. Child Abuse Negl. 2010;34(11):833–841. doi: 10.1016/j.chiabu.2010.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baglivio M.T., Wolff K.T., Epps N., Nelson R. Predicting adverse childhood experiences: the importance of neighborhood context in youth trauma among delinquent youth. Crime Delinq. 2017;63(2):166–188. [Google Scholar]
- 13.Bellis M.A., Hughes K., Leckenby N., Hardcastle K., Perkins C., Lowey H. Measuring mortality and the burden of adult disease associated with adverse childhood experiences in England: a national survey. J. Public Health. 2014;37(3):445–454. doi: 10.1093/pubmed/fdu065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dube S.R., Felitti V.J., Dong M., Giles W.H., Anda R.F. The impact of adverse childhood experiences on health problems: evidence from four birth cohorts dating back to 1900. Prev. Med. 2003;37(3):268–277. doi: 10.1016/s0091-7435(03)00123-3. [DOI] [PubMed] [Google Scholar]
- 15.Cluver L., Orkin M., Boyes M.E., Sherr L. Child and adolescent suicide attempts, suicidal behavior, and adverse childhood experiences in South Africa: a prospective study. J. Adolesc. Health. 2015;57(1):52–59. doi: 10.1016/j.jadohealth.2015.03.001. [DOI] [PubMed] [Google Scholar]
- 16.Gonçalves Helen, Soares A.L.G., Santos APGd, Ribeiro C.G., Bierhals I.O., Vieira L.S. Adverse childhood experiences and consumption of alcohol, tobacco and illicit drugs among adolescents of a Brazilian birth cohort. Cadernos de Saúde Pública [online] 2016;32(10) doi: 10.1590/0102-311X00085815. [DOI] [PubMed] [Google Scholar]
- 17.Anda R.F., Felitti V.J., Bremner J.D., Walker J.D., Whitfield C., Perry B.D. The enduring effects of abuse and related adverse experiences in childhood. Eur. Arch. Psychiatry Clin. Neurosci. 2006;256(3):174–186. doi: 10.1007/s00406-005-0624-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shonkoff J.P., Garner A.S., Siegel B.S., Dobbins M.I., Earls M.F., Garner A.S. The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129(1):e232. doi: 10.1542/peds.2011-2663. [DOI] [PubMed] [Google Scholar]
- 19.Danese A., Moffitt T.E., Harrington H., Milne B.J., Polanczyk G., Pariante C.M. Adverse childhood experiences and adult risk factors for age-related disease: depression, inflammation, and clustering of metabolic risk markers. Arch. Pediatr. Adolesc. Med. 2009;163(12):1135–1143. doi: 10.1001/archpediatrics.2009.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dannlowski U., Stuhrmann A., Beutelmann V., Zwanzger P., Lenzen T., Grotegerd D. Limbic scars: long-term consequences of childhood maltreatment revealed by functional and structural magnetic resonance imaging. Biol. Psychiatry. 2012 Feb 15;71(4):286–293. doi: 10.1016/j.biopsych.2011.10.021. PubMed PMID: 22112927. Epub 2011/11/25. eng. [DOI] [PubMed] [Google Scholar]
- 21.Teicher M.H., Anderson C.M., Polcari A. Childhood maltreatment is associated with reduced volume in the hippocampal subfields CA3, dentate gyrus, and subiculum. Proc. Natl. Acad. Sci. U. S. A. 2012;109(9):E563–E572. doi: 10.1073/pnas.1115396109. PubMed PMID: 22331913. Epub 02/13. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gilbert R., Widom C.S., Browne K., Fergusson D., Webb E., Janson S. Burden and consequences of child maltreatment in high-income countries. The Lancet. 2009;373(9657):68–81. doi: 10.1016/S0140-6736(08)61706-7. [DOI] [PubMed] [Google Scholar]
- 23.Hindley N., Ramchandani P.G., Jones D.P.H. Risk factors for recurrence of maltreatment: a systematic review. Arch. Dis. Child. 2006 07/13 05/24/accepted;91(9):744–752. doi: 10.1136/adc.2005.085639. PubMed PMID: PMC2082913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Richter L., Norris S., Pettifor J., Yach D., Cameron N. Cohort Profile: mandela's children: the 1990 birth to twenty study in South Africa. Int. J. Epidemiol. 2007 June 1;36(3):504–511. doi: 10.1093/ije/dym016. 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.SA S. Statistics South Africa; Pretoria, South Africa: 2013. Marriages and Divorces. [Google Scholar]
- 26.Senekal A. 2017. Domestic Partnerships. Greeff Attorneys, Tyger Valley. [cited 2019 4 March]. Available from: https://greeffattorneys.co.za/2017/07/26/domestic-partnerships/ [Google Scholar]
- 27.Finkelhor D., Shattuck A., Turner H., Hamby S. A revised inventory of adverse childhood experiences. Child Abuse Neglect. 2015;48:13–21. doi: 10.1016/j.chiabu.2015.07.011. [DOI] [PubMed] [Google Scholar]
- 28.Cronholm P.F., Forke C.M., Wade R., Bair-Merritt M.H., Davis M., Harkins-Schwarz M. Adverse childhood experiences: expanding the concept of adversity. Am. J. Prev. Med. 2015;49(3):354–361. doi: 10.1016/j.amepre.2015.02.001. [DOI] [PubMed] [Google Scholar]
- 29.Griffiths P.L., Rousham E.K., Norris S.A., Pettifor J.M., Cameron N. Socio-economic status and body composition outcomes in urban South African children. Arch. Dis. Child. 2008;93(10):862–867. doi: 10.1136/adc.2006.112649. [DOI] [PubMed] [Google Scholar]
- 30.Basto-Abreu A., Barrientos-Gutiérrez T., Zepeda-Tello R., Camacho V., Gimeno Ruiz de Porras D., Hernández-Ávila M. The relationship of socioeconomic status with body mass index depends on the socioeconomic measure used. Obesity. 2018;26(1):176–184. doi: 10.1002/oby.22042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Galobardes B., Shaw M., Lawlor D.A., Lynch J.W., Davey Smith G. Indicators of socioeconomic position (part 1) J. Epidemiol. Community Health. 2006 Jan;60(1):7–12. doi: 10.1136/jech.2004.023531. PubMed PMID: 16361448. Pubmed Central PMCID: PMC2465546. Epub 2005/12/20. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Saif-Ur-Rahman K.M., Anwar I., Hasan M., Hossain S., Shafique S., Haseen F. Use of indices to measure socio-economic status (SES) in South-Asian urban health studies: a scoping review. Syst. Rev. 2018;7(1):196. doi: 10.1186/s13643-018-0867-6. PubMed PMID: 30447696. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Desmond C. 2010. Measuring Socio-Economic Status in the Birth to Twenty Cohort. [Google Scholar]
- 34.StataCorp L.P. 2014. Stata Statistics/Data Analysis. College Station, USA. [Google Scholar]
- 35.Stoltenborgh M., Van Ijzendoorn M.H., Euser E.M., Bakermans-Kranenburg M.J. A global perspective on child sexual abuse: meta-analysis of prevalence around the world. Child. Maltreat. 2011;16(2):79–101. doi: 10.1177/1077559511403920. [DOI] [PubMed] [Google Scholar]
- 36.Bottoms B.L., Peter-Hagene L.C., Epstein M.A., Wiley T.R., Reynolds C.E., Rudnicki A.G. Abuse characteristics and individual differences related to disclosing childhood sexual, physical, and emotional abuse and witnessed domestic violence. J. Interpers Violence. 2016;31(7):1308–1339. doi: 10.1177/0886260514564155. [DOI] [PubMed] [Google Scholar]
- 37.Hughes K., Bellis M.A., Hardcastle K.A., Sethi D., Butchart A., Mikton C. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. The Lancet Public Health. 2017;2(8):e356–e366. doi: 10.1016/S2468-2667(17)30118-4. [DOI] [PubMed] [Google Scholar]
- 38.Hatcher A.M., Gibbs A., Jewkes R., McBride R.-S., Peacock D., Christofides N. Effect of childhood poverty and trauma on adult depressive symptoms among young men in peri-urban South African settlements. J. Adolesc. Health. 2019;64(1):79–85. doi: 10.1016/j.jadohealth.2018.07.026. [DOI] [PubMed] [Google Scholar]
- 39.Walker S.P., Wachs T.D., Grantham-McGregor S., Black M.M., Nelson C.A., Huffman S.L. Inequality in early childhood: risk and protective factors for early child development. Lancet. 2011;378(9799):1325–1338. doi: 10.1016/S0140-6736(11)60555-2. [DOI] [PubMed] [Google Scholar]
- 40.Coulton C.J., Crampton D.S., Irwin M., Spilsbury J.C., Korbin J.E. How neighborhoods influence child maltreatment: a review of the literature and alternative pathways. Child Abuse Neglect. 2007;31(11–12):1117–1142. doi: 10.1016/j.chiabu.2007.03.023. [DOI] [PubMed] [Google Scholar]
- 41.Kim B., Maguire-Jack K. Community interaction and child maltreatment. Child Abuse Neglect. 2015;41:146–157. doi: 10.1016/j.chiabu.2013.07.020. [DOI] [PubMed] [Google Scholar]
- 42.Font S.A., Maguire-Jack K. Pathways from childhood abuse and other adversities to adult health risks: the role of adult socioeconomic conditions. Child Abuse Neglect. 2016;51:390–399. doi: 10.1016/j.chiabu.2015.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Brown S.L. Marriage and child well-being: research and policy perspectives. J. Marriage Fam. 2010;72(5):1059–1077. doi: 10.1111/j.1741-3737.2010.00750.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Parrish J.W., Young M.B., Perham-Hester K.A., Gessner B.D. Identifying risk factors for child maltreatment in Alaska. Am. J. Prev. Med. 2011;40(6):666–673. doi: 10.1016/j.amepre.2011.02.022. 2011/06/01/ [DOI] [PubMed] [Google Scholar]
- 45.Kidman R., Palermo T. The relationship between parental presence and child sexual violence: evidence from thirteen countries in sub-Saharan Africa. Child Abuse Neglect. 2016;51:172–180. doi: 10.1016/j.chiabu.2015.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Roman N.V., Isaacs S.A., Davids C., Sui X.-C. How well are families doing? A description of family well-being in South Africa. Family Medicine and Community Health. 2016;4(3):9–18. [Google Scholar]
- 47.Chartier M.J., Walker J.R., Naimark B. Separate and cumulative effects of adverse childhood experiences in predicting adult health and health care utilization. Child Abuse Neglect. 2010;34(6):454–464. doi: 10.1016/j.chiabu.2009.09.020. [DOI] [PubMed] [Google Scholar]
- 48.Sameroff A.J. Developmental systems and psychopathology. Dev. Psychopathol. 2000;12(3):297–312. doi: 10.1017/s0954579400003035. Epub 09/01. [DOI] [PubMed] [Google Scholar]
- 49.McEwen B.S., Gianaros P.J. Central role of the brain in stress and adaptation: links to socioeconomic status, health, and disease. Ann. N. Y. Acad. Sci. 2010;1186(1):190–222. doi: 10.1111/j.1749-6632.2009.05331.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.The Lancet Adversity in childhood: how the past defines the future. The Lancet. 2016;388(10058):2324. doi: 10.1016/S0140-6736(16)32172-9. [DOI] [PubMed] [Google Scholar]
- 51.Kristman V.L., Manno M., Cote P. Methods to account for attrition in longitudinal data: do they work? A simulation study. Eur. J. Epidemiol. 2005;20(8):657–662. doi: 10.1007/s10654-005-7919-7. PubMed PMID: 16151878. Epub 2005/09/10. eng. [DOI] [PubMed] [Google Scholar]
- 52.Crouch E., Strompolis M., Bennett K.J., Morse M., Radcliff E. Assessing the interrelatedness of multiple types of adverse childhood experiences and odds for poor health in South Carolina adults. Child Abuse Neglect. 2017;65:204–211. doi: 10.1016/j.chiabu.2017.02.007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.