Abstract
Introduction
Pharyngeal and laryngeal cancers are highly curable; however survivors are at high risk for long-term dysphagia after radiation. To address lack of access to preventive care in community settings, we developed a responsive web-based application to help patients adhere to preventive swallowing exercises and cope with radiation side effects. We conducted an interim study analysis to determine website usage characteristics and to examine the effect size for future trials.
Methods
Pharyngeal and laryngeal cancer patients were recruited for enrollment by speech language pathologists before primary radiation and introduced to the interactive website. The program (English and Spanish) features tracking logs for preventive exercises, instructional videos, patient stories and search features. Patients' self-reported swallowing function was assessed with the MD Anderson Dysphagia Inventory (MDADI) at baseline and at 6 months. Adherence to preventive exercises was assessed during the 10 week intervention. Number of unique website visits, total duration of website exposure, and rankings of the most popular webpages were calculated. Preliminary regression models were run using adherence and MDADI as outcomes.
Results
Of the 160 enrolled, 96 had 10-week adherence data and 61 had 6-month MDADI data. The average age was 63 (SD = 12.26), 49.4% were from rural counties, 44% had a high school education or lower, and 42% reported annual income of $30,000 or less. The average number of visits was 5.49 (SD = 9.96) and the average total time spent with the website was 41.09 min (SD =88.48). Preliminary analyses indicated that number of unique visits to the website was independently associated with increased adherence to preventive exercises (p = .001–.008).
Conclusion
Our website showed significant effects in promoting adherence to swallowing exercises. However, our return visit rate showed that the platform needs improvement in navigability and usability for this older population undergoing challenging treatment in community settings with low resources.
Keywords: Patient engagement, Community-based care, Head and neck cancer, Adherence, Self-management
Highlights
-
•
An adherence and coping website was developed for community-based head and neck cancer patients undergoing curative radiation
-
•
The website content utilized self-management concepts to promote adherence
-
•
During the 10-week program, patients averaged 5.5 unique visits and spent an average of 41 minutes total.
-
•
Adherence to swallowing and trismus exercises was significantly associated with increased number of unique webpage visits
1. Introduction
It is estimated that 30,280 Americans will develop laryngeal or pharyngeal cancers in 2019, with 7210 expected deaths (Siegel et al., 2019). Long-term SEER-9 data show increases in oropharyngeal cancer 5-year survival rates from 35.4% for those diagnosed in 1975 to 74.7% for those diagnosed in 2010 (Surveillance and End Results (SEER) Programe, 2015). High-dose radiation treatment is a component of their management and can cause permanent sequelae, including fibrosis of swallowing muscles and dysphagia (Eisbruch et al., 2004; Cooper et al., 1995). Unfortunately, once fibrosis of the swallowing muscles has developed, there is little hope of restoring normal function (Cooper et al., 1995; Nguyen et al., 2004; Vainshtein et al., 2015). An estimated 39 to 63% of patients develop radiation-associated dysphagia within a 1–2 year period after treatment, the severity of which ranges from not being able to swallow foods without liquid assist, to being completely dependent on percutaneous gastrostomy (PEG) tube feeding (Mortensen et al., 2013; Caudell et al., 2008; Group MAHaNCSW et al., 2016; Caudell et al., 2010; Caglar et al., 2008; Hoxbroe Michaelsen et al., 2017; Logemann et al., 2008). While typically underappreciated at the time of cancer diagnosis and treatment, radiation-associated dysphagia negatively impacts quality of life and may lead to progressive malnutrition and increased risk of aspiration (Nguyen et al., 2006; Eisbruch et al., 2002; Roe et al., 2014; Wilson et al., 2011).
Modern radiation techniques try to avoid unnecessary radiation dose to swallowing structures, but in addition, swallowing exercises during radiation may be effective in preventing dysphagia. These exercises target the base of tongue, pharyngeal constrictors and suprahyoid strap muscles to promote strength, mobility and endurance. The preponderance of existing studies show that speech language therapies are effective in preventing and reducing radiation-associated dysphagia (Carnaby-Mann et al., 2011; Carnaby-Mann and Crary, 2010; van der Molen et al., 2011; Kulbersh et al., 2006; Kotz et al., 2012; Nguyen et al., 2007; Cousins et al., 2013; Zhen et al., 2012; Lazarus et al., 2014; Martin-Harris et al., 2015; Mashhour et al., 2018). Patients are usually asked to complete exercises that focus on jaw, head and neck mobility, swallowing movements and speech function, at a frequency of 3–4 sets a day lasting a total of 15–20 min per day (Shinn et al., 2013; Cnossen et al., 2017; Hutcheson et al., 2013; Wells et al., 2016; Hutcheson and Lewin, 2013). Our group has published data suggesting that exercise therapy during radiation reduces the incidence of post-treatment dysphagia in advanced oropharynx cancer patients (Shinn et al., 2013).
Despite the potential benefit to long-term swallowing, patient adherence to prescribed swallowing exercises ranges from 30% (Cnossen et al., 2017) to 86% (Shinn et al., 2013; van der Molen et al., 2009; Krekeler et al., 2018), depending on how adherence was defined. Cancer patients' nonadherence to difficult regimens is complex and resistant to change (Martin et al., 2005; Sirur et al., 2009). Head and neck cancer patients have compelling reasons for nonadherence, such as radiation side effects, a limited sense of urgency in the absence of overt signs of dysphagia, and forgetting to complete exercises with the competing demands of treatment.
Very few head and neck cancer patients treated outside of tertiary cancer centers will learn swallowing exercises before fibrosis occurs, let alone receive specialized support for adherence to these difficult exercises during radiation. All head and neck cancer patients need and deserve evidence-based speech pathology evaluation and preventive services as well as support programs to help them adhere to their preventive care; however, these services may not reach the vast majority of patients who are treated in community care settings (Arora et al., 2014). In the case of head and neck cancer, rural and community medical centers do not typically employ the services of full-time speech pathologists since these cancers are relatively rare. The U.S. Bureau of Labor Statistics reported in 2017 that only 13% of all speech pathologists worked in adult medical settings, with fewer numbers trained in the specialized area of dysphagia prevention and rehabilitation in head and neck cancer patients (Bureau of Labor Statistics USDoL, 2017).
In light of the national shortage of professionals who can provide preventive therapy for patients who are at-risk for dysphagia, inexpensive mobile health technologies such as the iPhone Swallowing App have been introduced commercially. However, it is unknown whether these untested applications are effective, due to the complex nature of the swallowing exercises and need for individualized instruction from certified speech pathologists.
A self-management psychosocial intervention, PREPARE, is an evidence-based approach to increase patient adherence to preventive exercises during radiation, PREPARE targets several determinants of nonadherence to preventive swallowing exercises. Ten weekly modules are organized by week of radiation, timed to coincide with the somewhat predictable worsening of physical and psychological side effects associated with radiation to the throat. Quotes from former radiation patients modeling adaptive emotional attitudes toward adherence are interspersed throughout the modules (“I did every exercise, even the hard ones. And now I can eat everything”). The purpose of this study is to describe the adaptation of the PREPARE intervention to a mobile platform to enhance its dissemination potential in a community cohort of head and neck cancer patients. The secondary purpose of the study was to conduct exploratory analyses regarding the impact of the website to patient adherence to swallowing exercises.
2. Method
2.1. Participants
Head and neck cancer patients who attended speech pathology appointments at the Texas Health Care (THC)-otolaryngology clinic in Fort Worth were enrolled onto study by THC speech pathologists. All patient data was collected by THC providers, de-identified and transferred to MD Anderson. Patient usage data was also de-identified by having all patients use unique study number IDs and user-generated passwords at login. Patients were eligible if they: were about to begin a new radiation treatment for oropharyngeal, laryngeal, hypopharyngeal, nasopharyngeal, oral tongue, or an unknown primary cancer with cervical metastases; had at least locally advanced disease (stages II–IV); were at least 18 years of age; spoke English or Spanish; and were oriented to time and place. Patients were excluded if they had other cancer diagnoses, except non-melanoma skin cancer, or had previous head and neck surgery (excluding tonsillectomy or partial laryngectomy).
2.2. Measures
2.2.1. Main outcome: adherence to swallowing exercises
Adherence was a continuous variable ranging from 0 to 1 and was defined as the number of weeks in which the participant had reported performing all prescribed swallowing exercises within the last 24 h, divided by the number of weeks that the participant had been reached by phone during the 10 week study period. For the first 30 participants enrolled onto the study, adherence assessments were attempted every week by phone. Since participants were difficult to reach, we later amended this procedure to assessing adherence at week 3 of radiation, at the end of radiation, and at the 10 week follow-up (4 weeks post-radiation). THC speech pathologists conducted the telephone assessments.
2.2.2. The MD Anderson Dysphagia Inventory (MDADI)
The MD Anderson Dysphagia Inventory (MDADI) measures swallowing-related quality of life (QOL) in patients with swallowing dysfunction. It evaluates the patient's physical (P), emotional (E) and functional (F) perceptions of swallowing dysfunction. This instrument has high internal consistency (0.85 to 93), and demonstrated good construct validity with the SF-36 subscales (Chen et al., 2001).
2.2.3. Side effects
Pain was measured with the Brief Pain Inventory (BPI), a 9-item self-report measure specifically designed to assess pain severity and pain interference (Daut et al., 1983). Internal consistencies for pain intensity range from 0.78 to 0.96 and pain interference from 0.83 to 0.95 (Atkinson et al., 2010). Fatigue was measured with the Brief Fatigue Inventory (BFI), a 9-item self-report measure similar in format to the BPI (Mendoza et al., 1999). The BFI's internal consistency is 0.96 and correlates well with measures of performance status and with physiological markers known to be associated with fatigue (Mendoza et al., 1999).
2.2.4. Demographic and medical information
Demographic and medical information were collected at the beginning of radiation therapy. Age at study entry, gender, race, educational level, marital status, stage of disease, disease site, receipt of induction and/or concurrent chemotherapy were abstracted from the THC medical record, de-linked and uploaded to REDCap.
2.2.5. Patient engagement metrics
Patient engagement metrics were captured with MATOMO web analytics. Unique visits were defined as a visit to the website >30 min since the last log-in. Total visit duration was measured in seconds and only counted those visits that lasted longer than a single pageview. The number of times a page was visited was counted and ranked to determine the most popular features of the website. To estimate decline in engagement over time, we counted the number of unique page views for each week's content, as this was the best measure available. Page views were counted instead of unique visits as it was possible for patients to skip to different weeks within a single visit.
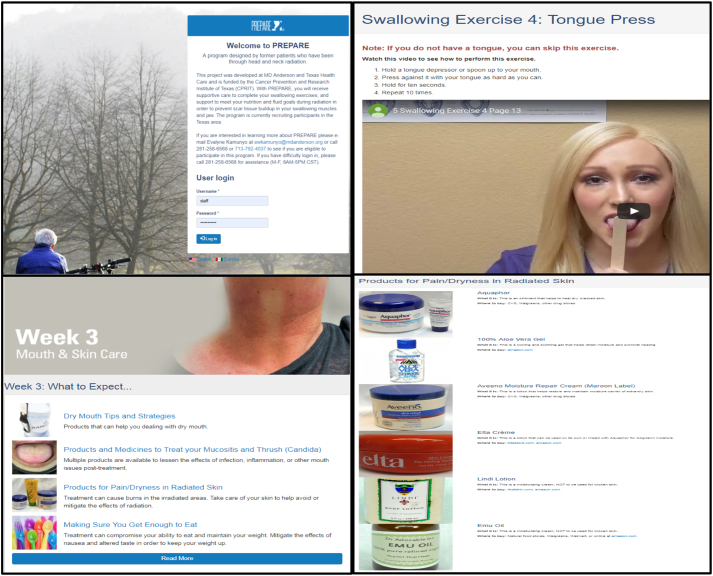
2.3. Intervention
To increase the scalability of PREPARE, we adapted the original intervention to a web-based platform. The online PREPARE platform was developed by Radiant Digital, LLC, over the course of 8 months in a series of 10 planning sprints. System architecture and design were developed first as wireframes to capture all user interface requirements and later sprints addressed back-end data management and interactive features such as diet and weight tracking and graphing features: Patients were able to enter in daily values of weight, food intake and exercise counts to view cumulative graphs of weight loss or gain, adherence to exercise and oral intake. In addition, patients could enter their radiation start date so that web page content (which is organized by week of radiation) automatically opened to the patient's current week of radiation. To maximize patient engagement, video, audio, and photographs were utilized instead of text to demonstrate recipes, swallowing and trismus exercises and convey personal narratives from former patients. Tracking and search features were developed and beta-tested with staff and then pilot patients at THC. The website demonstrates all features on desktop, phone or tablet. All content was edited to be consistent with a 5th-grade reading level in the U.S. The entire website was available in Spanish, provided by certified Spanish translation services. The web-based intervention included the following components adapted from the original PREPARE intervention (Fig. 1a–c).
Fig. 1.
Screenshots of various PREPARE website features.
2.3.1. Demonstration of swallowing exercise videos
Demonstration of swallowing exercise videos with accompanying verbal instruction. Unless otherwise specified, the following exercises were part of the standard regimen prescribed to head and neck cancer patients about to start radiation: the Shaker I and II, Mendelsohn, jaw stretching, Supraglottic swallow and base of tongue exercises (Masako and effortful swallow). Each of these exercises were to be repeated 3–5 times per set, with 2 sets of exercises to be performed every day. Some exercises, such as the Shaker I and II, were withheld for various reasons during radiation, such as the patient having prior neck injury or cervical fusion. In addition, patients were taught trismus prevention exercises and asked to perform them twice a day. Patients in the study were advised that videos of all exercises were available on the website for their reference.
2.3.2. Self-management adherence strategies
PREPARE utilizes Leventhal & Leventhal's theory of Self-Regulation, which posits that illness perceptions shape patients' understanding of their illness, which in turn affects coping (Cameron and Leventhal, 2003). PREPARE addresses the theory's five dimensions of illness perceptions (identity, cause, consequences, control and timing). Identity is addressed by framing preventive exercises as a necessary path back to normalcy after treatment instead of an unimportant chore. The intervention teaches the link between radiation and radiation-associated fibrosis of swallowing muscles (cause) and presents several accounts of patients being able to swallow normally after performing their exercises during radiation (consequences). Since throat radiation side effects tend to follow a somewhat predictable sequence of worsening pain, loss of taste and impaired swallowing over the 6–7 week treatment period, PREPARE times the introduction of topics to the week of radiation when each symptom was most likely to begin. Our intervention emphasizes personal control by presenting multiple strategies for each radiation side effect and encouraged patients to try new strategies on subsequent webpages if a strategy failed.
2.3.3. Self-management coping strategies
Over-the-counter mouth rinses and skin lotions recommended by former patients were organized by order of effectiveness. Simple recipes for patients who did not regularly cook at home and other feeding strategies were provided. The common experience of losing all sense of taste during radiation was normalized to reduce participants' anxiety. Practical communication strategies designed to curb tendencies to nag or argue during this stressful period were also presented to spouses and caregivers. Realistic expectations for recovery after radiation were presented in the later weeks of the intervention to reduce the risk of discouragement (Fig. 2).
Fig. 2.
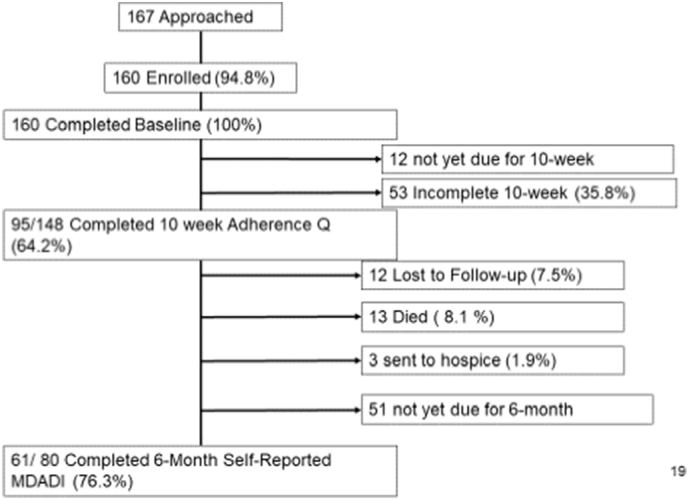
Consort.
2.4. Procedure
This program was deemed non-human subjects research by the institutional review board at M. D. Anderson since THC provided the website as part of their usual care and since personally identifiable information was not collected. At a later date, institutional approval was obtained through a separate protocol to analyze the deidentified patient data that is reported herein. All patients at THC were counseled by speech pathology as part of their usual care to anticipate common radiation side effects, taught the rationale for preventive exercises, and given visual demonstrations of the exercises until the patient could perform them independently. After being enrolled onto the study, THC speech pathologists showed the participant how to log in to the website and oriented him or her to its various features. Technical assistance with the website was limited to this single session at the beginning of radiation. At study entry, THC providers collected demographics, non-identifying disease and treatment information, and self-reported swallowing function. The adherence assessment asked participants whether they had performed all swallowing and trismus exercises within the past 24 h. For the first 30 participants, these assessments were attempted on a weekly basis by THC speech pathologists via telephone. Since participants were difficult to reach, this procedure was amended after the 30th participant to attempt to assess adherence at week 3, at the end of radiation and at the 10 week follow-up (4 weeks post-radiation). THC staff collected adherence to swallowing and trismus exercises data during the 10th week of the program and self-reported swallowing function again at 6 months. All data was de-linked from patient identifiers and uploaded to the Research Electronic Database Capture (REDCap) system housed behind MD Anderson's firewall. Identifying-disease information (such as radiation start date) could only be uploaded to the patient's website after the patient had logged in anonymously with a study identification number.
2.5. Analysis
Summary statistics where used to describe the demographic and clinical characteristics of the study population. We tested for changes in MDADI from baseline to 6 months using a one tailed paired t-test. To assess whether demographic characteristics were associated with 10-week adherence to preventive exercises, simple linear regression models where conducted with adherence as our outcome. Predictor variables of interest were age, race, marital status, stage, education, rural living, and the primary predictor, unique visits. Models for adherence included robust standard error estimation (due to their non-normal distribution). Model diagnostics were assessed for all regression models to assess assumptions of residuals. All statistical analysis were performed using Stata/MP v15.0 (College Station, TX).
3. Results
One hundred sixty-seven patients were approached for entry into the study and 160 were enrolled. At the time of this report, all patients had baseline data, 95 (59%) had 10-week follow-up data and 61 (38%) had 6-month follow-up data (see CONSORT, Fig. 1). Sixty-two participants had at least three complete assessments of adherence within the past 24 h and 84 participants had less than three assessments and were not included in the adherence analysis. The average number of completed sets of swallowing exercises reported within the past 24 h was 2.34. The average age was 63 years (SD = 12.26), 49.4% were from rural counties, 44% had a high school education or lower, and 42% reported annual income of $30,000 or less (Table 1).
Table 1.
Summary statistics of the demographic and clinical characteristics of the study population (n = 160).
| Characteristic | N | % |
|---|---|---|
| What is your age? | ||
| N | 160 | |
| Mean (SD) | 63.29 (12.26) | |
| Median (min-max) | 64.00 (24.00–91.00) | |
| What is your race? | ||
| Hispanic | 11 | 6.88 |
| Non-Hispanic White | 140 | 87.50 |
| Black or African American | 6 | 3.75 |
| American Indian or Alaska Native | 2 | 1.25 |
| Native Hawaiian or Pacific Islander | 1 | <0.01 |
| What is your highest level of education | ||
| Did not receive a high school diploma/GED | 15 | 9.49 |
| High school diploma/GED | 50 | 31.65 |
| Technical/vocational degree | 7 | 4.43 |
| Some college credits or 2-year college degree | 49 | 31.01 |
| Bachelor's degree | 29 | 18.35 |
| Master's degree | 5 | 3.16 |
| M.D., Ph.D., or other doctorate degree | 3 | 1.90 |
| Education dichotomized into HS v HS+ | ||
| High school, GED, vocational or did not finish HS | 72 | 45.57 |
| Some college credits or bachelor's degree | 86 | 54.43 |
| Employment | ||
| Full-time | 57 | 35.63 |
| Part time | 5 | 3.13 |
| Not seeking nor employed | 10 | 6.25 |
| Seeking but not employed | 7 | 4.38 |
| Retired | 71 | 44.38 |
| Homemaker | 5 | 3.13 |
| Student | 2 | 1.25 |
| Disabled | 5 | 3.13 |
| Marital status | ||
| Single living alone | 18 | 11.25 |
| Single living with significant other | 7 | 4.38 |
| Married living with spouse | 98 | 61.25 |
| Married but living apart | 1 | 0.63 |
| Separated | 1 | 0.63 |
| Divorced | 20 | 12.50 |
| Widowed | 15 | 9.38 |
| Living alone | ||
| No, living with someone | 105 | 65.63 |
| Lives alone | 55 | 34.38 |
| Occupation | ||
| Managerial/professional (college degree or more): e.g., executive manager, te | 46 | 29.49 |
| Technical (associate degree, junior college): e.g., health workers, artists | 15 | 9.62 |
| Clerical/retail: e.g., secretaries, receptionists, sales persons | 17 | 10.90 |
| Service Occupations: e.g., housekeeper, restaurant worker, cosmetologist, ch | 7 | 4.49 |
| Operators/labors: e.g., bus driver, janitor, machine operators | 43 | 27.56 |
| Homemaker | 5 | 3.21 |
| Student | 1 | 0.64 |
| Unemployed | 10 | 6.41 |
| Other | 12 | 7.69 |
| What is your income before taxes? | ||
| No income | 15 | 9.74 |
| Less than $5000 | 6 | 3.90 |
| $5001–$10,000 | 6 | 3.90 |
| $10,001–$20,000 | 20 | 12.99 |
| $20,001–$30,000 | 20 | 12.99 |
| $30,001–$50,000 | 30 | 19.48 |
| $50,001–$75,000 | 28 | 18.18 |
| More than $75,000 | 29 | 18.83 |
| Chemotherapy status | ||
| Concurrent chemotherapy | 82 | 67.77 |
| Induction chemotherapy | 2 | 1.65 |
| Both induction and concurrent chemotherapy | 2 | 1.65 |
| No chemotherapy | 35 | 28.93 |
| AJCC disease stage | ||
| 1 | 4 | 3.36 |
| 2 | 10 | 8.40 |
| 3 | 33 | 27.73 |
| 4 | 72 | 60.50 |
| Early vs late stage disease | ||
| Stages I & II | 14 | 11.76 |
| Stages III–IV | 105 | 88.24 |
| Disease sites | ||
| Larynx | 30 | 18.75 |
| Oropharynx | 49 | 30.62 |
| Hypopharynx | 3 | 1.87 |
| Nasopharynx | 4 | 2.5 |
| Oral cavity yes | 35 | 21.87 |
| Other | 38 | 23.75 |
| Rural | ||
| Urban | 81 | 50.63 |
| Rural | 79 | 49.38 |
3.1. User engagement metrics
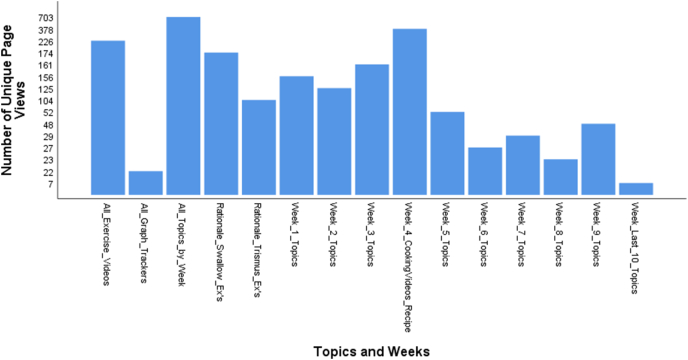
The average number of visits was 5.49 (SD = 9.96) and the average total time spent with the website was 41.09 min (SD =88.48; Table 2). The topics which were visited the most were (in rank order) 1) recipes and cooking video demonstrations (378 unique page views), 2) Swallowing and Trismus exercise video demonstrations (226 unique page views), 3) Rationale of swallowing exercises (174 unique page views), 4) Week 3 webpages (164 unique page views), 5) Week 1 webpages (156 unique page views), 6) week 2 webpages (125 unique page views), Week 4 (104 unique page views), Week 5 (52 unique page views), Week 9 (48 unique page views), Week 7 (29 unique page views), Week 6 (27 unique page views), Week 8 (23 unique page views), and week 10 (7 unique page views; Fig. 3).
Table 2.
Summary statistics of outcomes MDADI and swallowing adherence.
| Characteristic | N |
|---|---|
| TRISMUS adherent yes/no | |
| N | 95 |
| Mean (SD) | 0.51 (0.41) |
| Median (min-max) | 0.50 (0.00–1.00) |
| Swallowing adherent yes/no | |
| N | 95 |
| Mean (SD) | 0.53 (0.43) |
| Median (min-max) | 0.50 (0.00–1.00) |
| Total visit duration, per user (in seconds) | |
| N | 132 |
| Mean (SD) | 2465.21 (5308.51) |
| Median (min-max) | 710.50 (0.00–37,033.00) |
| Number of unique visits | |
| N | 132 |
| Mean (SD) | 5.49 (9.96) |
| Median (min-max) | 2.50 (1.00–95.00) |
| Number of unique page views | |
| N | 132 |
| Mean (SD) | 47.89 (111.28) |
| Median (min-max) | 11.50 (1.00–970.00) |
| Functional MDADI baseline | |
| N | 156 |
| Mean (SD) | 75.35 (16.40) |
| Median (min-max) | 76.00 (24.00–100.00) |
| Physical MDADI baseline | |
| N | 156 |
| Mean (SD) | 72.01 (20.45) |
| Median (min-max) | 68.00 (20.00–100.00) |
| Emotional MDADI baseline | |
| N | 156 |
| Mean (SD) | 78.59 (18.52) |
| Median (min-max) | 80.00 (24.00–100.00) |
| Functional MDADI 6 months | |
| N | 61 |
| Mean (SD) | 45.93 (21.47) |
| Median (min-max) | 40.00 (20.00–100.00) |
| Physical MDADI 6 months | |
| N | 60 |
| Mean (SD) | 52.43 (22.86) |
| Median (min-max) | 50.00 (20.00–100.00) |
| Emotional MDADI 6 months | |
| N | 61 |
| Mean (SD) | 45.81 (24.02) |
| Median (min-max) | 40.00 (20.00–100.00) |
Fig. 3.
Engagement by topics and weeks.
3.2. Adherence to exercises
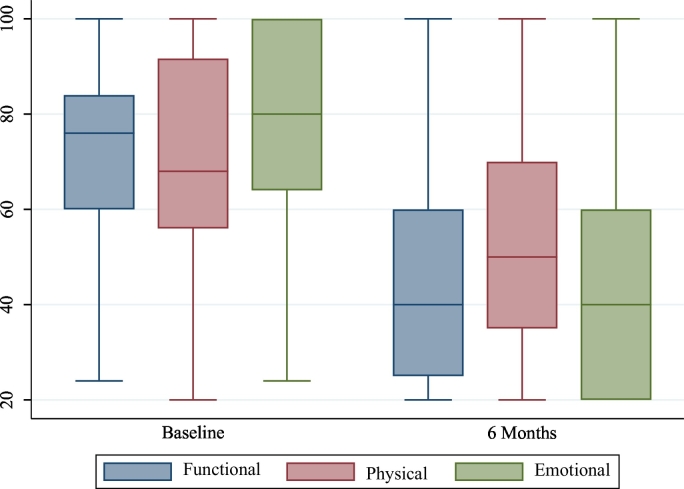
Of the patients who completed adherence interview data, 51% indicated that they were adherent to trismus exercises and 53% to swallowing exercises. Compared to baseline, 6-month self-reported swallowing function had significantly declined in all three domains (Table 3 and Fig. 4). Results for the preliminary regression models are presented in Table 4. For each additional unique visit to the website, adherence to both trismus and swallowing exercises increased on average by 0.02 units after controlling for age, race, education, disease stage and county status.
Table 3.
Paired t-test for MDADI between baseline and 6 months.
| MDADI | Time | N | Mean | SD | 95% LB | 95% UB | p-Value |
|---|---|---|---|---|---|---|---|
| Functional | Baseline | 59 | 72.27 | 18.22 | 67.52 | 77.02 | <0.001 |
| 6 months | 59 | 46.74 | 21.36 | 41.17 | 52.31 | ||
| Difference | 59 | 25.53 | 32.88 | 16.96 | 34.10 | ||
| Physical | Baseline | 58 | 71.80 | 20.65 | 66.38 | 77.23 | <0.001 |
| 6 months | 58 | 52.86 | 23.14 | 46.78 | 58.95 | ||
| Difference | 58 | 18.94 | 34.98 | 9.74 | 28.14 | ||
| Emotional | Baseline | 59 | 77.42 | 18.89 | 72.50 | 82.35 | <0.001 |
| 6 months | 59 | 46.53 | 24.10 | 40.25 | 52.81 | ||
| Difference | 59 | 30.89 | 35.03 | 21.76 | 40.02 |
Fig. 4.
Box plot of MDADI scores.
Table 4.
Linear regression models on outcomes.
| Multivariable |
|||||||
|---|---|---|---|---|---|---|---|
| Outcome | Step | Characteristic | Model N | Beta | 95% LB | 95% UB | p-Value |
| TRISMUS | 1 | What is your age? | 0.00 | −0.01 | 0.01 | 0.651 | |
| Non-Hispanic White (ref: other) | 0.00 | −0.42 | 0.41 | 0.985 | |||
| Living with S.O. (ref: living along) | 63 | 0.19 | −0.05 | 0.42 | 0.116 | ||
| HS+ (ref: some HS) | 0.17 | −0.05 | 0.39 | 0.127 | |||
| Stage III/IV (ref: stage I/II) | −0.02 | −0.31 | 0.28 | 0.901 | |||
| Rural living (ref: Urban) | −0.08 | −0.29 | 0.13 | 0.458 | |||
| 2 | What is your age? | 58 | 0.00 | −0.01 | 0.01 | 0.912 | |
| Visits | 0.02 | 0.01 | 0.03 | 0.003 | |||
| Non-Hispanic White (ref: other) | 0.08 | −0.45 | 0.60 | 0.77 | |||
| Living with S.O. (ref: living along) | 0.14 | −0.10 | 0.38 | 0.249 | |||
| HS+ (ref: some HS) | 0.11 | −0.12 | 0.33 | 0.354 | |||
| Stage III/IV (ref: stage I/II) | 0.04 | −0.23 | 0.31 | 0.756 | |||
| Rural living (ref: Urban) | −0.06 | −0.28 | 0.17 | 0.62 | |||
| Swallowing | 1 | What is your age? | 0.00 | −0.01 | 0.01 | 0.703 | |
| Non-Hispanic White (ref: other) | −0.06 | −0.50 | 0.39 | 0.795 | |||
| Living with S.O. (ref: living along) | 63 | 0.16 | −0.09 | 0.40 | 0.216 | ||
| HS+ (ref: some HS) | 0.11 | −0.14 | 0.35 | 0.389 | |||
| Stage III/IV (ref: stage I/II) | 0.08 | −0.23 | 0.39 | 0.615 | |||
| Rural living (ref: Urban) | −0.08 | −0.31 | 0.15 | 0.469 | |||
| 2 | What is your age? | 58 | 0.00 | −0.01 | 0.01 | 0.961 | |
| Visits | 0.02 | 0.01 | 0.03 | 0.008 | |||
| Non-Hispanic White (ref: other) | 0.01 | −0.58 | 0.60 | 0.969 | |||
| Living with S.O. (ref: living along) | 0.11 | −0.15 | 0.36 | 0.418 | |||
| HS+ (ref: some HS) | 0.04 | −0.22 | 0.30 | 0.769 | |||
| Stage III/IV (ref: stage I/II) | 0.14 | −0.18 | 0.45 | 0.382 | |||
| Rural living (ref: Urban) | −0.05 | −0.28 | 0.19 | 0.679 | |||
Bolded p-values indicated significance at the p<.05 cutoff.
4. Discussion
PREPARE is an ongoing web-based intervention designed to promote adherence and coping during radiation in head and neck cancer patients. During a single session at the beginning of radiation, speech pathologists at Texas Health Care introduced patients to the website and provided instructions for logging in and navigation. While the limited contact with human technical support may be adequate for populations who are not undergoing rigorous cancer treatment, our approach may have proved to be overly ambitious, as our average usage rate was 5.5 visits over the ten weeks. Informal feedback from patients after their treatment indicated that physical side effects (pain from mouth sores, weakness from losing weight during radiation and nausea) limited their willingness to log in to the website. Increased time introducing the various practical strategies designed to counter these common radiation side effects may help increase the unique visit rate in the future.
Within the literature assessing user engagement with digital mental health self-help interventions for non-cancer populations, engagement metrics include dropout rates, average number of minutes per day, completion rates for modular fixed-length programs, and download rates (Fleming et al., 2018). For example, a recent study evaluating aggregated user traffic for 59 mental health apps within the general population showed a median 30-day retention rate of 3.3%, with steep declines in usage rates from day 1 (after app installation) to day 10 (Baumel et al., 2019). Other reviews have shown similar steep declines in engagement with open access websites for depression and anxiety (Christensen et al., 2009). Because our patients were encouraged to access the specific topics that were most relevant to them throughout radiation, they were allowed access to all webpages at any time of the study period, i.e., the progression through the weekly sessions was not controlled. Therefore, we unable to translate the number of website visits to a length of time in which the patient remained engaged. A somewhat comparable metric is to examine engagement by week of radiation, and these data show that number of unique page views followed a general decline from Week 1 (156 page views) to week 10 (7 page views). However, the number of page views was highest for week 3 (161 page views) and week 4 content (104 page views and an additional 378 page views for cooking and recipes, which were presented in week 4). Week 3's web pages introduced strategies for dry mouth, mucositis, thrush, nausea and loss of taste. The content in week 4 contained all eating strategies, recipes and cooking video demonstrations, as well as strategies for fatigue. Peaks in weeks 3–4 webpage views may reflect the popularity of the content rather than the length of time that patients remained engaged in the intervention, as it is possible that patients may have accessed week 3 and 4 content primarily when they were first introduced to the website. Given the somewhat predictable pattern of mucositis, loss in taste and difficulty eating manifesting in the 3rd and 4th weeks of radiation however, the peak in views for Weeks 3–4 are more likely a reflection of the fact that patients engaged in the website during these weeks as they encountered these side effects.
Regarding our exploratory objective, we were surprised to see that one metric of engagement, number of visits, was significantly related to self-reported adherence to preventive swallowing and trismus exercises. However this result should be interpreted with caution as the rate of missing data was quite high, 58% (84 participants had completed 3 or fewer of the weekly telephone adherence assessments and were not included in this secondary analysis). It is possible that the association between number of visits and adherence may have been spurious. Patient adherence to exercises may have been increased by the regular telephone contact with THC speech pathologists assessing weekly (and later biweekly) adherence to exercises; the regular telephone assessments may have not only increased adherence but cued participants to visit the website more often.
We were encouraged by the relatively high enrollment rate among this socioeconomically diverse sample, which may underscore patients' perceived need for supportive technologies during radiation to the throat. Demographic factors such as education, income and county status were not significantly associated with adherence to the preventive exercises, which ran counter to our expectations. Further analyses on the relationship between socioeconomic factors and patient engagement metrics will be conducted. While reading and literacy levels were not measured in this study, the proportion of those who had a bachelor's degree or higher was lower than that of the age-matched census group in the U.S. (18% versus 25–29.6%) (USCB, 2016). Informal feedback from our patients indicated that the extensive use of visual media was easy to understand.
5. Conclusion
Exposure to the web-based adherence self-management program was significantly associated with increased adherence to preventive swallowing and trismus exercises during radiation. However, patient engagement metrics and written feedback indicated that the platform needs improvement in navigability and usability for this older population undergoing challenging treatment in community settings with low resources.
Funding sources
This study was supported by the following grants: NIDCR DE019141, CPRIT PP150077, NCI CA016672.
Declaration of competing interest
All authors have participated in (a) conception and design, or analysis and interpretation of the data; (b) drafting the article or revising it critically for important intellectual content; and (c) approval of the final version.
References
- Arora S., Thornton K., Komaromy M. 2014;89(1) doi: 10.1097/ACM.0000000000000051. [DOI] [PubMed] [Google Scholar]
- Atkinson T.M., Mendoza T.R., Sit L. The Brief Pain Inventory and its “pain at its worst in the last 24 hours” item: clinical trial endpoint considerations. Pain Med. 2010;11:337–346. doi: 10.1111/j.1526-4637.2009.00774.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumel A., Muench F., Edan S. Objective user engagement with mental health apps: systematic search and panel-based usage analysis. J. Med. Internet Res. 2019;21 doi: 10.2196/14567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bureau of Labor Statistics USDoL . Pathologists -SL (ed) U.S. Government Printing Office; Washington D.C.: 2017. Occupational employment statistics, May 2017. [Google Scholar]
- Caglar H.B., Tishler R.B., Othus M. Dose to larynx predicts for swallowing complications after intensity-modulated radiotherapy. Int. J. Radiat. Oncol. Biol. Phys. 2008;72:1110–1118. doi: 10.1016/j.ijrobp.2008.02.048. [DOI] [PubMed] [Google Scholar]
- Cameron L., Leventhal H. Routledge; New York: 2003. The Self-regulation of Health and Illness Behavior. [Google Scholar]
- Carnaby-Mann G.D., Crary M.A. McNeill dysphagia therapy program: a case-control study. Arch. Phys. Med. Rehabil. 2010;91:743–749. doi: 10.1016/j.apmr.2010.01.013. [DOI] [PubMed] [Google Scholar]
- Carnaby-Mann G., Crary M., Schmalfuss L. “Pharyngocise”: randomized controlled trial of preventative exercises to maintain muscle structure and swallowing function during head and neck chemoradiotherapy. Int. J. Radiat. Oncol. Biol. Phys. 2011 doi: 10.1016/j.ijrobp.2011.06.1954. In press:In press. [DOI] [PubMed] [Google Scholar]
- Caudell J., Schaner P., Meredith R. Factors associated with long-term dysphagia after definitive radiotherapy for locally advanced head and neck cancer. International Journal of Radiation Biology Oncology and. Physics. 2008;73:410–415. doi: 10.1016/j.ijrobp.2008.04.048. [DOI] [PubMed] [Google Scholar]
- Caudell J.J., Schaner P.E., Desmond R.A. Dosimetric factors associated with long-term dysphagia after definitive radiotherapy for squamous cell carcinoma of the head and neck. Int. J. Radiat. Oncol. Biol. Phys. 2010;76:403–409. doi: 10.1016/j.ijrobp.2009.02.017. [DOI] [PubMed] [Google Scholar]
- Chen A., Frankowski R., Bishop-Leone J. The development and validation of a dysphagia-specific quality-of-life questionnaire for patients with head and neck cancer. Archives of Otolaryngology Head and Neck. Surgery. 2001;127:870–876. [PubMed] [Google Scholar]
- Christensen H., Griffiths K.M., Farrer L. Adherence in internet interventions for anxiety and depression: systematic review. J. Med. Internet Res. 2009;11:e13. doi: 10.2196/jmir.1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cnossen I.C., van Uden-Kraan C.F., Witte B.I. Prophylactic exercises among head and neck cancer patients during and after swallowing sparing intensity modulated radiation: adherence and exercise performance levels of a 12-week guided home-based program. Eur. Arch. Otorhinolaryngol. 2017;274:1129–1138. doi: 10.1007/s00405-016-4367-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper J., Fu K., Marks J. Late effects of radiation therapy in the head and neck region. Int. J. Radiat. Oncol. Biol. Phys. 1995;31:1141–1164. doi: 10.1016/0360-3016(94)00421-G. [DOI] [PubMed] [Google Scholar]
- Cousins N., MacAulay F., Lang H. A systematic review of interventions for eating and drinking problems following treatment for head and neck cancer suggests a need to look beyond swallowing and trismus. Oral Oncol. 2013;49:387–400. doi: 10.1016/j.oraloncology.2012.12.002. [DOI] [PubMed] [Google Scholar]
- Daut R.L., Cleeland C.S., Flanery R.C. Development of the Wisconsin brief pain questionnaire to assess pain in cancer and other diseases. Pain. 1983;17:197–210. doi: 10.1016/0304-3959(83)90143-4. [DOI] [PubMed] [Google Scholar]
- Eisbruch A., Lyden T., Bradford C. Objective assessment of swallowing dysfunction and aspiration after radiation concurrent with chemotherapy for head and neck cancer. Int. J. Radiat. Oncol. Phys. 2002;53:23–28. doi: 10.1016/s0360-3016(02)02712-8. [DOI] [PubMed] [Google Scholar]
- Eisbruch A., Schwartz M., Rasch C. Dysphagia and aspiration after chemoradiotherapy for head and neck cancer: which anatomic structures are affected and can they be spared by IMRT? International Journal of Radiation. Oncol. Phys. 2004;60:1425–1439. doi: 10.1016/j.ijrobp.2004.05.050. [DOI] [PubMed] [Google Scholar]
- Fleming T., Bavin L., Lucassen M. Beyond the trial: systematic review of real-world uptake and engagement with digital self-help interventions for depression, low mood, or anxiety. J. Med. Internet Res. 2018;20:e199. doi: 10.2196/jmir.9275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Group MAHaNCSW, Dale T., Hutcheson K. Beyond mean pharyngeal constrictor dose for beam path toxicity in non-target swallowing muscles: dose-volume correlates of chronic radiation-associated dysphagia (RAD) after oropharyngeal intensity modulated radiotherapy. Radiother. Oncol. 2016;118:304–314. doi: 10.1016/j.radonc.2016.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoxbroe Michaelsen S., Gronhoj C., Hoxbroe Michaelsen J. Quality of life in survivors of oropharyngeal cancer: a systematic review and meta-analysis of 1366 patients. Eur. J. Cancer. 2017;78:91–102. doi: 10.1016/j.ejca.2017.03.006. [DOI] [PubMed] [Google Scholar]
- Hutcheson K.A., Lewin J.S. Functional assessment and rehabilitation – how to maximize outcomes. Otolaryngol. Clin. N. Am. 2013;46:657–670. doi: 10.1016/j.otc.2013.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutcheson K.A., Bhayani M.K., Beadle B.M. Eat and exercise during radiotherapy or chemoradiotherapy for pharyngeal cancers: use it or lose it. JAMA Otolaryngol. Head Neck Surg. 2013;139:1127–1134. doi: 10.1001/jamaoto.2013.4715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotz T., Federman A.D., Kao J. Prophylactic swallowing exercises in patients with head and neck cancer undergoing chemoradiation: a randomized trial. Arch Otolaryngol. Head Neck Surg. 2012;138:376–382. doi: 10.1001/archoto.2012.187. [DOI] [PubMed] [Google Scholar]
- Krekeler B.N., Broadfoot C.K., Johnson S. Patient adherence to dysphagia recommendations: a systematic review. Dysphagia. 2018;33:173–184. doi: 10.1007/s00455-017-9852-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulbersh B., Rosenthal E., McCrew B. Pretreatment preoperative swallowing exercises may improve dysphagia qualify of life. Laryngoscope. 2006;116:883–886. doi: 10.1097/01.mlg.0000217278.96901.fc. [DOI] [PubMed] [Google Scholar]
- Lazarus C.L., Husaini H., Falciglia D. Effects of exercise on swallowing and tongue strength in patients with oral and oropharyngeal cancer treated with primary radiotherapy with or without chemotherapy. Int. J. Oral Maxillofac. Surg. 2014;43:523–530. doi: 10.1016/j.ijom.2013.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logemann J.A., Pauloski B.R., Rademaker A.W. Swallowing disorders in the first year after radiation and chemoradiation. Head Neck. 2008;30:148–158. doi: 10.1002/hed.20672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin L.R., Williams S.L., Haskard K.B. The challenge of patient adherence. Ther. Clin. Risk Manag. 2005;1:189–199. [PMC free article] [PubMed] [Google Scholar]
- Martin-Harris B., McFarland D., Hill E.G. Respiratory-swallow training in patients with head and neck cancer. Arch. Phys. Med. Rehabil. 2015;96:885–893. doi: 10.1016/j.apmr.2014.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mashhour K., Abdelkader R., Abdelkader L. Swallowing exercises: will they really help head and neck cancer patients? Asian Pac. J. Cancer Prev. 2018;19:797–801. doi: 10.22034/APJCP.2018.19.3.797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendoza T.R., Wang X.S., Cleeland C.S. The rapid assessment of fatigue severity in cancer patients. Cancer. 1999;85:1186–1196. doi: 10.1002/(sici)1097-0142(19990301)85:5<1186::aid-cncr24>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- van der Molen L., van Rossum M., Burkhead L. Functional outcomes and rehabilitation strategies in patients treated with chemoradiotherapy for advanced head and neck cancer: a systematic review. Eur. Arch. Oto-Rhino Laryngol. 2009;266:889–900. doi: 10.1007/s00405-008-0817-3. [DOI] [PubMed] [Google Scholar]
- van der Molen L., van Rossum M.A., Burkhead L.M. A randomized preventive rehabilitation trial in advanced head and neck cancer patients treated with chemoradiotherapy: feasibility, compliance, and short-term effects. Dysphagia. 2011;26:155–170. doi: 10.1007/s00455-010-9288-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mortensen H., Jensen K., Aksglaede K. Late dysphagia after IMRT for head and neck cancer and correlation with dose-volume parameters. Radiother. Oncol. 2013;107:288–294. doi: 10.1016/j.radonc.2013.06.001. [DOI] [PubMed] [Google Scholar]
- Nguyen N., Moltz C., Frank C. Dysphagia following chemoradiation for locally advanced head and neck cancer. Ann. Oncol. 2004;15:383–388. doi: 10.1093/annonc/mdh101. [DOI] [PubMed] [Google Scholar]
- Nguyen N., Frank C., Moltz C. Aspiration rate following chemoradiation for head and neck cancer: an underreported occurrence. Radiother. Oncol. 2006;80:109–274. doi: 10.1016/j.radonc.2006.07.031. [DOI] [PubMed] [Google Scholar]
- Nguyen N., Moltz C., Frank C. Impact of swallowing therapy on aspiration rate following treatment for locally advanced head and neck cancer. Oral Oncol. 2007;43:352–357. doi: 10.1016/j.oraloncology.2006.04.002. [DOI] [PubMed] [Google Scholar]
- Roe J.W., Drinnan M.J., Carding P.N. Patient-reported outcomes following parotid-sparing intensity-modulated radiotherapy for head and neck cancer. How important is dysphagia? Oral Oncol. 2014;50:1182–1187. doi: 10.1016/j.oraloncology.2014.09.009. [DOI] [PubMed] [Google Scholar]
- Shinn E., Basen-Engquist K., Baum G. Adherence to preventive exercises and self-reported swallowing outcomes in post-radiation head and neck cancer patients. Head Neck. 2013 doi: 10.1002/hed.23255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegel R.L., Miller K.D., Jemal A. Cancer Statistics, 2019. CA Cancer J Clin. 2019;69:7–34. doi: 10.3322/caac.21551. [DOI] [PubMed] [Google Scholar]
- Sirur R., Richardson J., Wishart L. The role of theory in increasing adherence to prescribed practice. Physiother. Can. 2009;61:68–77. doi: 10.3138/physio.61.2.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Surveillance E, and End Results (SEER) Program Populations SEER*Stat Database: Cancer of the oral cavity and pharynx for selected subsites (invasive); SEER Relative survival (percent) by year of diagnosis (1975-2015); all races, males and females; in National Cancer Institute D, Surveillance Research Program (ed), 2015.
- USCB (2016): Educational Attainment 2012–2016 American Community Survey 5-year estimates. Washington D.C., U.S. Census Bureau, 2012–2016.
- Vainshtein J.M., Moon D.H., Feng F.Y. Long-term quality of life after swallowing and salivary-sparing chemo-intensity modulated radiation therapy in survivors of human papillomavirus-related oropharyngeal cancer. Int. J. Radiat. Oncol. Biol. Phys. 2015;91:925–933. doi: 10.1016/j.ijrobp.2014.12.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells M., King E., Toft K. Development and feasibility of a Swallowing intervention Package (SiP) for patients receiving radiotherapy treatment for head and neck cancer—the SiP study protocol. Pilot Feasibil. Stud. 2016;2(40) doi: 10.1186/s40814-016-0079-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson J., Carding P., Patterson J. Dysphagia after nonsurgical head and neck cancer treatment: Patients’ perspectives. Otolaryngology Head and Neck. Surgery. 2011;145:767–771. doi: 10.1177/0194599811414506. [DOI] [PubMed] [Google Scholar]
- Zhen Y., Wang J.G., Tao D. Efficacy survey of swallowing function and quality of life in response to therapeutic intervention following rehabilitation treatment in dysphagic tongue cancer patients. Eur. J. Oncol. Nurs. 2012;16:54–58. doi: 10.1016/j.ejon.2011.03.002. [DOI] [PubMed] [Google Scholar]