Images in pediatrics
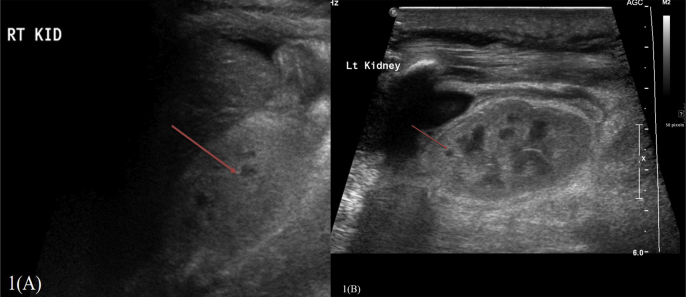
A five days old, full term baby boy transferred to our institution from private hospital diagnosed with hypertension and renal failure. The baby had no proper antenatal follow up. He was born at 39 weeks of gestation with uncomplicated, normal spontaneous vaginal delivery. The patient had abnormal Apgar score 5 and 7 in 1min and 5 min respectively. There is no history or risk of hypoxia recorded. The patient found to have dysmorphic features including hypertelorism, depressed nasal bridge and low-set ears. The baby was hypotonic and had seizure in the second day of life. The patient admitted to our hospital for investigation. Initial radiological exam was Ultrasound abdomen and pelvis, the scan showed normal size, echogenic kidneys with poor cortico-medullary differentiation and small cysts at corticomedullary junction consistent with medullary cystic disease of infancy (Nephronophthisis) (Fig. 1A and B).
Fig. 1.
Sagittal Ultrasound of the right (A) and left kidney (B) show normal-sized kidneys with parenchymal hyperechogenicity and loss of corticomedullary differentiation. Small cysts are present in the medulla bilaterally (arrow).
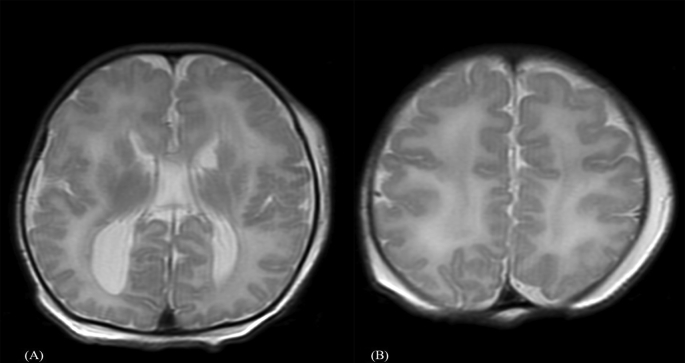
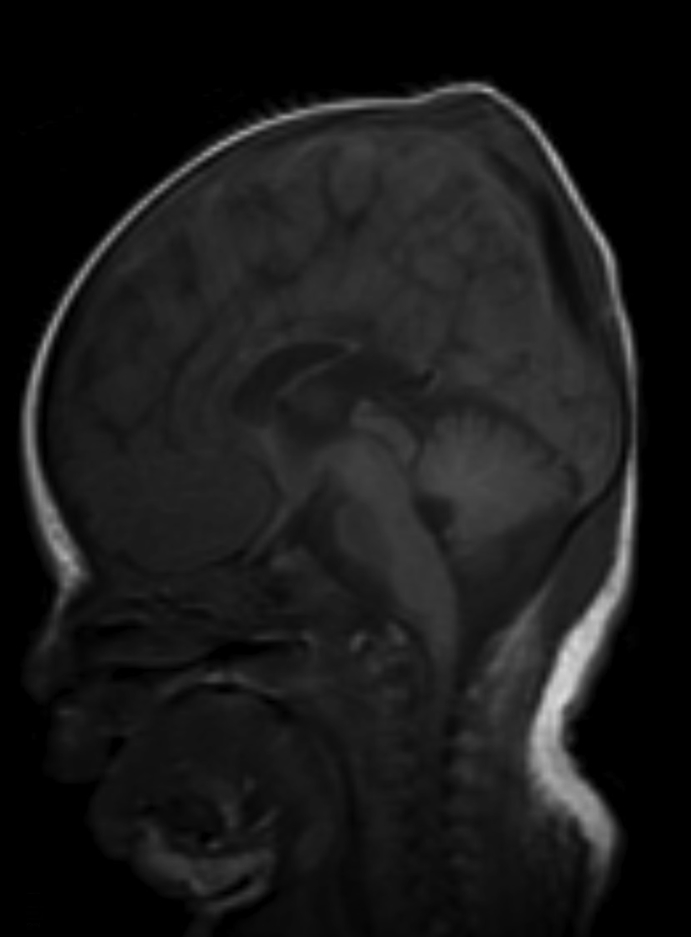
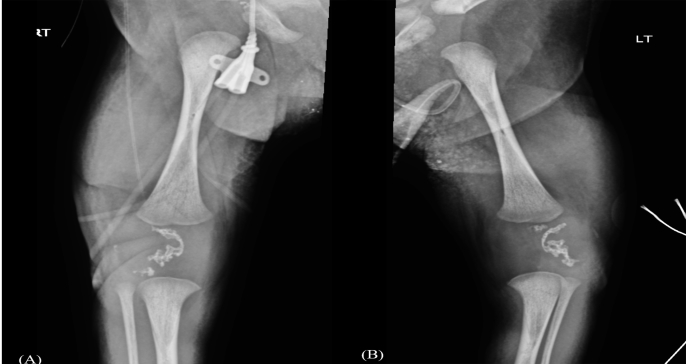
Subsequently MRI of the brain performed. It showed bilateral perisylvian polymicrogyria with bilateral caudothalmic groove cysts (Fig. 2A), Bilateral frontal and parietal pachygyria noted (Fig. 2B) also, delay myelination for the patient age noted [1,2] and hypoplastic corpus callosum (Fig. 3). The diagnosis of Zellweger syndrome suggested based on the MRI findings. The patient had skeletal survey that showed Scimitar-like ossification of patellae (Fig. 4A and B) classically described in Zellweger syndrome [3].
Fig. 2.
Brain MRI (A) Axial T2 WI image shows bilateral perisylvian polymicrogyria (white arrow) as well as caudothalamic germinolytic cysts. (B) Axial T2WI image show bilateral frontal pachygyria, delay myelination noted.
Fig. 3.
Brian MRI Sagittal T1WI image shows hypoplastic corpus callosum.
Fig. 4.
(A,B): AP view of the knees show scimitar-like patella bilatrally.
The patient diagnosis confirmed genetically with mutations in the PEX6 gene. The patient eventually died from renal failure and respiratory failure.
Zellweger syndrome known as the cerebrohepatorenal syndrome is an autosomal recessive disease caused by mutations in PEX genes [1,2]. It is the most severe form of peroxisomes abnormality. The incident is 1 in 50,000–100,000 live births. Peroxisomes are cellular organelles catalyzing a number of indispensable functions in cellular metabolism such as beta-oxidation of very-long-chain fatty acids (VLCFA).
ZW syndrome symptoms present soon after birth with facial dysmorphic features, hypotonia, difficult to suck and seizure [4].
Neuroimaging may lead the way to the diagnosis in ZW syndrome. MRI findings include delay myelination for the patient age, cortical malformations, and germinolytic cysts. The migration abnormality include polymicrogyria in the perisylvic region, pachygyria mainly in the frontoparietal regions and heterotopia.
Other radiological findings include hepatomegaly, echogenic kidney with medullary cystic disease secondary to ciliopathy [5]. Skeletal survey demonstrate scimitar patella secondary to stippled chondral ossification, known association with peroxisome disorder [3].
The laboratory diagnosis of Zellweger syndrome relies on abnormally elevated levels of very long chain fatty acids (VLCFA).
Zellweger syndrome has poor prognosis, most infants do not survive beyond their first year of life. The treatment mainly focuses on symptomatic and supportive care.
Footnotes
Peer review under responsibility of King Faisal Specialist Hospital & Research Centre (General Organization), Saudi Arabia.
References
- 1.Klouwer F., Berendse K., Ferdinandusse S., Wanders R., Engelen M., Tien Poll-The B. Zellweger spectrum disorders: clinical overview and management approach. Orphanet J Rare Dis. 2015;10:151. doi: 10.1186/s13023-015-0368-9. [online)] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.TienPoll-Thea B., Gärtnerb J. Linical diagnosis, biochemical findings and MRI spectrum of peroxisomal disorder. Biochim Biophys Acta (BBA) - Mol Basis Dis. 2012;1822(9):1421–1429. doi: 10.1016/j.bbadis.2012.03.011. Sept. [DOI] [PubMed] [Google Scholar]
- 3.Smitthimedhin A., Otero H.J. Scimitar-like ossification of patellae led to diagnosis of Zellweger syndrome in newborn: a case report. Clin Imaging. 2018;29:128–130. doi: 10.1016/j.clinimag.2018.01.008. May-June. [DOI] [PubMed] [Google Scholar]
- 4.Pfeifer C., Martinot C. Zellweger syndrome: depiction of MRI findings in early infancy at 3.0 Tesla. Neuroradiol J. 2017;30(5):442–444. doi: 10.1177/1971400917700670. Oct. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Salomon R., Saunier S., Niaudet P. Nephronophthisis. Pediatr Nephrol. 2009;24:2333–2344. doi: 10.1007/s00467-008-0840-z. [DOI] [PMC free article] [PubMed] [Google Scholar]