Abstract
Dematiaceous fungi can cause subcutaneous phaeohyphomycosis, an uncommon fungal infection of the dermis and subcutaneous tissues. Medicopsis romeroi is an emerging organism that can infect patients with subcutaneous phaeohyphomycosis, especially immunocompromised patients. The present case involved subcutaneous phaeohyphomycosis caused by Medicopsis romeroi in an 80-year-old Thai male with poorly controlled diabetes, for whom the lesion underwent spontaneous remission after his glycemic control was improved. Furthermore, cases of subcutaneous phaeohyphomycosis for the last 10 years were reviewed.
Keywords: Phaeohyphomycosis, Medicopsis romeroi, Pyrenochaeta romeroi, Diabetes
1. Introduction
Subcutaneous phaeohyphomycosis is not a common fungal infection of the dermis and subcutaneous tissues. It is caused by dematiaceous fungi, and it is believed to result from the traumatic implantation of the fungi into the subcutaneous tissue [1,2]. This form of infection is common in tropical countries and has been reported mainly in immunocompromised hosts. The common causative fungi are Exophiala jeanselmei, Exophiala dermatitidis, Phialophora spp. and Cladophialophora spp. [2,3]. The typical clinical presentation is an asymptomatic single nodule, or a cyst, or an abscess at the site of previous trauma, commonly on the extremities.
Medicopsis romeroi is allocated to phylum Ascomycota according to National Center for Biotechnology Information. It produces brown-colored, septate, hyphae without conidia [4]. These organisms are widely distributed in the soil and plants, and they are able to infect people by direct inoculation [4].
Medicopsis romeroi is an emerging fungus causing subcutaneous phaeohyphomycosis. Recent case reports have demonstrated that most patients with subcutaneous phaeohyphomycosis arising from Medicopsis romeroi have impaired immune systems [[4], [5], [6], [7], [8]], including patients with type 2 diabetes mellitus who have poor glycemic control [9,10]. Total surgical excision and debridement are the other options for eradicating the infection [1,2]. In this case, we demonstrated the case of subcutaneous phaeohyphomycosis caused by Medicopsis romeroi in a poorly controlled diabetic patient who achieved disease improvement through better glycemic control.
2. Case
An 80-year-old Thai male presented to the hospital (day 0) with 1-year of a single nodule on the medial aspect of his right foot (day −360). The lesion had gradually progressed to a size of around 1 cm. No pain or itching was found. He did not have fever, chronic cough, weight loss, or any other abnormal systemic symptoms. He denied having had previous trauma or working-contact with the soil or plants.
For 5 years (day −1800), the patient had had diabetes mellitus, which was poorly controlled (HbA1c 10%). However, he did not have retinopathy nor nephropathy. His current medications were metformin (1.5 g/day), glipizide (10 mg/day), and (aspirin 81 mg/day). He denied using any herbal drugs or other immunosuppressive drugs.
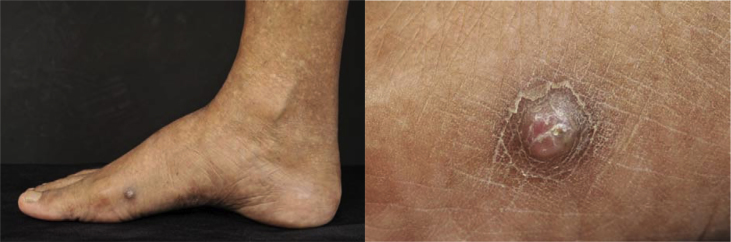
An examination revealed a single, firm, well-defined, erythematous nodule on the medial aspect of the right foot, but without lymphadenopathy (Fig. 1). All other physical examination findings were normal. A laboratory investigation showed normal blood cell counts and serum creatinine of 1.22 mg/dL (estimated glomerular filtration rate 41.0 ml/min/1.73 m2).
Fig. 1.
Clinical pictures of the patient demonstrated a single, firm, well-defined erythematous nodule on the medial aspect of the right foot.
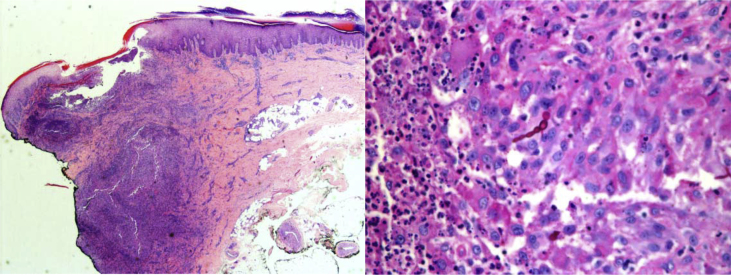
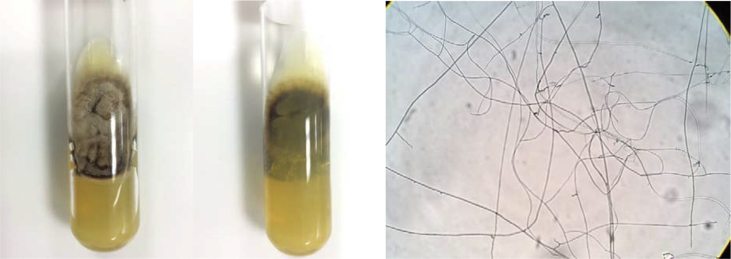
An incisional biopsy was undertaken (day 0) for histopathology, mycobacterium and fungal cultures, and fungal identification. The hematoxylin-and-eosin-stained histological sections revealed a nodular infiltrate of aggregates of epithelioid histiocytes with a mixed inflammatory infiltrate composed of numerous neutrophils, eosinophils, lymphocytes, and plasma cells. A Periodic acid–Schiff stain showed scattered multinucleated giant cells containing intracellular brownish septate hyphae, pseudohyphae and yeast-like organisms (Fig. 2). The fungal culture of the tissue biopsy demonstrated dematiaceous molds (day +90) (Fig. 3). A microscopic examination of the culture found broad, septate, branched, and dark brown hyphae. Molecular identification of the fungal species revealed Medicopsis romeroi (day +90). Molecular diagnosis is performed by sequencing of international transcribed spacer (ITS) region using primer sequence for ITS1 (5′-TCC GTA GGT GAA CCT GCG G-3′). The accession number of closest hit was JX088727.1 with 100% identification of maximal score of 852. The length of analyzed sequence was 477. The detail of polymerase chain reaction (PCR) protocol was demonstrated in Table 1. The bacterial and mycobacterial cultures of the tissue biopsy were negative (day +90). The diagnosis was subcutaneous phaeohyphomycosis caused by Medicopsis romeroi. After the histopathological diagnosis was established, an X-ray of the right foot was performed, but there was no evidence of an osteolytic lesion (day +50). A magnetic resonance imaging (MRI) study of the right foot was subsequently conducted (day +120). It found a small, diffuse, infiltrative region of abnormal signal intensity of the skin and subcutaneous tissues of the plantar surface of the foot, adjacent to the head of the first metatarsal bone and measuring about 2.4 x 0.9 × 2.5 cm (antero-posterior x width x height). No abnormality in signal intensity was observed in the bony structure or marrow. However, the imaging revealed that there were residual infiltrative lesions. While the patient was waiting for total excisional surgery, he succeeded in bringing his glycemic level under control, with his HbA1C value falling to below 7% (day +270). Because no mass was found on examination, a second MRI study of the right foot was performed (day +390). The MRI showed normal findings, with the disappearance of the small, diffuse, infiltrative region that had been found in the previous MRI study.
Fig. 2.
The Periodic acid–Schiff stain showed mixed-cell granulomas with intracellular, brownish, septate hyphae, pseudohyphae, and yeast-like organisms.
Fig. 3.
A fungal culture of the tissue biopsy demonstrated dematiaceous molds. Microscopic examination of the culture found broad, septate, branched, dark brown hyphae. (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
Table 1.
Polymerase chain reaction (PCR) protocol using sequencing of international transcribed spacer (ITS) region.
| Step | Temp.(°C) | Time (sec.) | Round |
|---|---|---|---|
| Pre-denature | 94 | 60 | 1 |
| Denature | 94 | 30 | 35 |
| Annealing | 48 | 30 | |
| Extension | 68 | 60 | |
| Final extension | 68 | 300 | 1 |
| Hold at | 4 | α |
In other words, the lesions of the subcutaneous phaeohyphomycosis were cured within 9 months (day +270), without the need for any systemic antifungal drug administration.
3. Discussion
Medicopsis romeroi is an emerging fungus causing subcutaneous phaeohyphomycosis. It has mostly been reported in immunocompromised patients receiving immunosuppressive drugs for hematologic malignancy [4], renal transplantation [5], rheumatoid arthritis [6], leprosy [7], and asthma [8]; however, there has been one report of a healthy, immunocompetent host [11], as shown in Table 2. Medicopsis romeroi has also reported in patients with type 2 diabetes mellitus who have poor glycemic control [9,10]. Since phagocytic activity is the main mechanism for anti-fungal infections [12], type 2 diabetes patients with hyperglycemic control have a significant decline in the phagocytic activity of peripheral blood mononuclear cells [13]. This could be why type 2 diabetes patients are susceptible to uncommon, cutaneous, fungal infections like Medicopsis romeroi.
Table 2.
Clinical settings and treatment outcomes of reviewed phaeohyphomycosis from Medicopsis romeroi patients.
| Report from | Age | Sex | Setting | Lesion | Site | Treatment and outcomes | Ref. |
|---|---|---|---|---|---|---|---|
| India | 45 | Female | Healthy | Subcutaneous nodule, cystic consistency | Right forearm | Surgical excision without oral anti-fungal treatment; then, completely cured, with no recurrence over 1 year | [11] |
| India | 47 | Female | ALL on prednisolone. methotrexate, vincristine, 6-MP | Subcutaneous nodule, cystic consistency | Right index finger | Aspirate pus and drainage; then, subsided gradually over 2 months without oral anti-fungal treatment | [4] |
| Taiwan | 78 | Male | Asthma on long-term prednisolone | Multiple papulopustular lesion | Right dorsum of hand and elbow | Amphotericin B for 3 weeks improved the lesion, with no recurrence over 6 months | [8] |
| Britain | 88 | Male | Leprosy and Bell's palsy on prednisolone | Discrete keratotic lesion | Dorsum of right hand | N/A | [7] |
| India | 61 | Female | RA on prednisolone, DMARD, methotrexate | Soft to firm mass | Proximal phalanx of right index finger | Itraconazole (200 mg/day) for 3 months; then, lesion improved, and no recurrence over 6 months | [6] |
| India | 43 | Male | KT on prednisolone, mycophenolate mofetil, tacrolimus | Multiple nodular lesion | Left thigh and calf | Itraconazole and then terbinafine; then, there were new lesions and were treated with excision and voriconazole | [5] |
| China | 55 | Male | KT on prednisolone, mycophenolate mofetil, cyclosporin | Nodule | Left posterior thigh | Surgical excision with long-term itraconazole | [15] |
| Africa | 66 | Male | KT on prednisolone, mycophenolate mofetil, tacrolimus | Hyperkeratotic nodule | Left heel | Surgical excision without oral anti-fungal treatment; then, completely cured, with no recurrence over 9 months | [14] |
| France | 47 | Female | DM type 2 for 3 years (BS 413 g/dL) | Firm mass | Radius of right foot | I&D without antifungal; then, clinical improvement | [9] |
| India | 48 | Male | DM type 2 (FBS 320 mg/dL), LL with ENL on dapsone, rifampicin | Subcutaneous nodule, cystic consistency | Lateral aspect of left foot | I&D plus itraconazole; then, lost to follow-up | [16] |
| India | 50 | Female | DM type 2 for 5 years with poor compliance (random BS 413 g/dl) | Soft to firm mass | Left foot | I&D plus itraconazole (200 mg/day) for 2 weeks; then, swelling resolved completely | [10] |
Abbreviations: 6-MP, 6-Mercaptopurine; ALL, acute myelocytic leukemia; BS, blood sugar; DM, diabetic mellitus; DMARD, disease-modifying anti-rheumatic drugs; ENL, erythema nodosum leprosum; FBS, fasting blood sugar; KT, kidney transplantation; LL, lepromatous leprosy; RA, rheumatoid arthritis.
In all previous case reports of Medicopsis romeroi causing subcutaneous phaeohyphomycosis, the fungus was identified as the causative organism through sequencing of the Internal Transcribe Spacer region and amplification. Fungal identification can guide treatment and inform the prognosis. Complete surgical excision is a curative treatment for phaeohyphomycosis. Systemic antifungal therapy is used in patients with refractory or recurrent infections due to incomplete excision. Information on the antifungal susceptibility of Medicopsis romeroi is limited. The few studies that have experimented with its in vitro susceptibilities demonstrated that the most potent drugs are itraconazole, isavuconazole, and posaconazole, each with very low minimum inhibitory concentrations of less than 1 μg/ml [4,11]. By contrast, amphotericin B, voriconazole, and especially fluconazole have been reported to have high minimum inhibitory concentrations [4,11].
Two earlier reports on type 2 diabetes patients had similar settings, namely, the two patients were females aged around 50 years, had a blood sugar level above 400 g/dL, and came to hospital with a firm mass on one side of a foot. In each case, molecular diagnosis identified Medicopsis romeroi [9,10]. Both cases demonstrated clinical improvement by surgical incisional and drainage. Although one patient was also prescribed itraconazole (200 mg/day) for 2 weeks, the other did not receive any antifungal drugs. The present patient represented the first case where a lesion regressed spontaneously, not through medical or surgical treatment, but instead by improving glycemic control. This may result from an enhancement of phagocytic activity (measured by using a modified flow cytometry procedure) in patients who have undergone metabolic optimization, as previously reported [13].
Recognition of subcutaneous infections caused by dematiaceous fungi remains challenging because identification is difficult via conventional cultures. The molecular method plays an important role in species identification, thereby aiding the diagnosis of phaeohyphomycosis and the determination of the most appropriate case management plan. Enhancing a patient's immune status may be a useful way to eliminate an infection.
Conflict of interest
There are none.
Acknowledgements
The authors gratefully acknowledge the technical assistance by Mrs. Nipa Tingtoy, under the supervision of Assoc. Prof. Dr. Popchai Ngamskulrungroj for providing the molecular diagnosis and information.
References
- 1.Hay R.J. Deep fungal infections. In: Kang S., Amagai M., Bruckner A.L., Enk A.H., Margolis D.J., McMichael A.J., Orringer J.S., editors. Fitzpatrick's Dermatology. ninth ed. McGraw-Hill; New York: 2019. p. 2972. [Google Scholar]
- 2.Elewski B.E., Hughey L.C., Hunt K.M., Hay R.J. Fungal disease. In: Bolognia J.L., Schaffer J.V., Cerroni L., editors. Dermatology. fourth ed. Elsevier; China: 2018. pp. 1361–1362. [Google Scholar]
- 3.Isa-Isa R., García C., Isa M., Arenas R. Subcutaneous phaeohyphomycosis (mycotic cyst) Clin. Dermatol. 2012;30(4):425–431. doi: 10.1016/j.clindermatol.2011.09.015. [DOI] [PubMed] [Google Scholar]
- 4.Khan Z., Ahmad S., Kapila K., Ramaswamy N.V., Alath P., Joseph L. Pyrenochaeta romeroi: a causative agent of phaeohyphomycotic cyst. J. Med. Microbiol. 2011;60:842–846. doi: 10.1099/jmm.0.029520-0. [DOI] [PubMed] [Google Scholar]
- 5.Kulkarni M., Jamale T., Hase N., Ubale M., Keskar V., Jagadish P.K. Subcutaneous phaeohyphomycosis caused by Pyrenochaeta romeroi in a kidney transplant recipient: a case report. Exp. Clin. Transplant. 2017;15(20):226–227. doi: 10.6002/ect.2014.0283. [DOI] [PubMed] [Google Scholar]
- 6.Sharma S., Capoor M.R., Singh M., Kiran D., Mandal A.K. Subcutaneous phaeohyphomycosis caused by Pyrenochaeta romeroi in a rheumatoid arthritis patient: a case report with review of the literature. Mycopathologia. 2016;181(9):735–743. doi: 10.1007/s11046-016-0022-7. [DOI] [PubMed] [Google Scholar]
- 7.Abdolrasouli A., Gonzalo X., Jatan A., McArthur G.J., Francis N., Azadian B.S. Subcutaneous phaeohyphomycosis cyst associated with Medicopsis romeroi in an immunocompromised host. Mycopathologia. 2016;181(9):717–721. doi: 10.1007/s11046-016-0017-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hsiao Y.W., Chia J.H., Lu C.F., Chung W.H. Molecular diagnosis and therapeutic experience of subcutaneous Pyrenochaeta romeroi infection: a case report and review of the literature. Int. J. Dermatol. 2013;52(10):1237–1240. doi: 10.1111/j.1365-4632.2011.05173.x. [DOI] [PubMed] [Google Scholar]
- 9.Dinh A., Levy B., Bouchand F., Davido B., Duran C., Cristi M. Subcutaneous phaeohyphomycosis due to Pyrenochaeta romeroi mimicking a synovial cyst. Front. Microbiol. 2016;7:1405. doi: 10.3389/fmicb.2016.01405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yadav S., Agarwal R., Singh S., Goel S. Pyrenochaeta romeroi causing subcutaneous phaeohyphomycosic cyst in a diabetic female. Med. Mycol. Case. Rep. 2015;8:47–49. doi: 10.1016/j.mmcr.2015.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Badali H., Chander J., Gulati N., Attri A., Chopra R., Najafzadeh M.J. Subcutaneous phaeohyphomycotic cyst caused by Pyrenochaeta romeroi. Med. Mycol. 2010;48(5):763–768. doi: 10.3109/13693780903440383. [DOI] [PubMed] [Google Scholar]
- 12.Romani L. Immunity to fungal infections. Nat. Rev. Immunol. 2011;11(4):275–278. doi: 10.1038/nri2939. [DOI] [PubMed] [Google Scholar]
- 13.Lecube A., Pachón G., Petriz J., Hernández C., Simó R. Phagocytic activity is impaired in type 2 diabetes mellitus and increases after metabolic improvement. PLoS One. 2011;6:e 23366. doi: 10.1371/journal.pone.0023366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ocampo M.A., Kanitakis J., Bienvenu A.L., Chauvet C., Euvrard S. Phaeohyphomycosis caused by Pyrenochaeta romeroi mimicking a plantar wart in a kidney transplant recipient. Transpl. Infect. Dis. 2012;14(6):e 173–174. doi: 10.1111/tid.12018. [DOI] [PubMed] [Google Scholar]
- 15.Chan Y.Y.C., Tan A.L., Tan B.H. Subcutaneous abscess due to Pyrenochaeta romeroi in a renal transplant recipient. Singap. Med. J. 2014;55(4):e 64–66. doi: 10.11622/smedj.2014063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sharma B., Singh P.K., Pandey K., Mittal G., Ramesh V., Deb M. Subcutaneous cyst due to Medicopsis romeroi in a diabetic lepromatous leprosy patient: an interesting case report and review from India. J. Clin. Diagn. Res. 2017;11(10):DD01–03. [Google Scholar]