Abstract
Background
There are a lack of clear guidelines for the dissemination of Internet-based cognitive behaviour therapy (ICBT) for childhood and adolescent anxiety in routine care. While self-guided ICBT has greater reach than therapist-guided ICBT, it is plagued by problems of low program adherence and many young people are not successfully treated. It is important that we identify models of ICBT that are accessible, but provide the right support, at the right time to those who need it. Stepped-care models of ICBT offer one potential solution.
Objective
This case study examined the application of stepped-care within an ICBT intervention for childhood and adolescent anxiety, in which young people were stepped up from self-guided to therapist-guided ICBT.
Methods
Three case studies are presented and include young males (aged 11–12 years) who participated in BRAVE Stepped-Care, a new ICBT program incorporating two treatment steps: Step 1 – five sessions of self-guided ICBT and Step 2 – five sessions of therapist-guided ICBT. Participants completed diagnostic assessments at pre- and post-treatment, along with a battery of self-report questionnaires. Step-up requirements were determined at a mid-treatment assessment. Treatment response was determined by change on diagnostic severity and presence of diagnosis and changes in self-reported anxiety symptoms (through T-scores and Reliable Change Indices).
Results
In-depth examination of the three case studies showed that decisions to step-up from Step 1 to Step 2 were complex and required consideration of program engagement and adherence, as well as changes on self-reported anxiety, behavioural indicators of anxiety and parent perspectives. Results showed that non-responders at mid-treatment who were stepped-up to therapist-guided ICBT after Step 1 were able to increase engagement and response to treatment in Step 2, such that they were free of their primary anxiety diagnosis at post-treatment.
Conclusions
The findings highlight the importance of early assessment of engagement and non-response within self-guided ICBT programs for youth anxiety and the positive changes that can subsequently occur when therapist-guidance is introduced mid-treatment for non-responders. The efficacy of stepped-care ICBT models needs to be confirmed in larger randomised controlled trials.
Keywords: Internet CBT, Child and adolescent, Anxiety disorders, Stepped-care, Self-help
Highlights
-
•
The cases presented here suggest problems with engagement and non-response to self-guided ICBT can be identified early.
-
•
Step-up decisions require consideration of engagement, improvements in anxiety and behaviour and multi-informant reports.
-
•
Stepping-up to minimal therapist-support was beneficial for the cases presented in this study.
1. Introduction
Childhood anxiety is a prevalent, chronic and disabling problem (Vigerland et al., 2017), with 6.5–7% of children and adolescents (here referred to as youth) internationally experiencing a clinical anxiety disorder (Lawrence et al., 2015; Polanczyk et al., 2015). Meta-analyses have shown that face-to-face cognitive-behavioural therapy (CBT) leads to full recovery in around 66% of anxious youth (Warwick et al., 2017), however, <50% of affected youth receive care (Costello et al., 2014). Internet-based CBT (ICBT) offers an acceptable alternative for today's digital natives (Merry et al., 2012) that can overcome shortages of CBT-trained therapists (Stallard et al., 2007), geographical restrictions limiting access, high therapy costs, and youth concerns regarding stigma and embarrassment (Lawrence et al., 2015; Sweeney et al., 2017; Sweeney et al., 2015). That is, ICBT presents a viable method for increasing the availability of evidence-based treatments to more young people (Andersson and Titov, 2014). The efficacy of ICBT interventions for youth anxiety has been demonstrated, with similar outcomes to face-to-face therapy, when delivered with therapist-guidance or support (Pennant et al., 2015; Spence et al., 2011; Podina et al., 2015). Further, there is now considerable evidence that ICBT is acceptable to clinicians, children, young people and their families (Sweeney et al., 2017; Sweeney et al., 2015; Topooco et al., 2017; Donovan et al., 2015).
1.1. Dissemination of ICBT in routine care
To date, ICBT or e-Mental Health interventions generally, have not been routinely adopted into healthcare services for children and young people (Wozney et al., 2018), nor are there formalised approaches to such dissemination (Hill et al., 2018). Preliminary support for routine implementation has been reported by Jolstedt et al. (2018) and March et al. (2018), though very different approaches were utilised. Jolstedt et al. (2018) distributed a therapist-supported ICBT program to twenty anxious children and their parents via outpatient clinics in Sweden. Although children reported moderate to high acceptability and demonstrated significant reductions in anxiety following the program, they completed on average, only half of the ICBT intervention (Jolstedt et al., 2018). The reliance on therapist support (20 min per week) also meant that widespread dissemination would be prohibitively expensive.
On the other hand, March et al. (2018) delivered their self-help ICBT program for anxiety (BRAVE Self-Help, with no therapist support), to 4425 young people across Australia. Children and adolescents who engaged with the program showed substantial reductions in anxiety, with a moderate to large effect size. Specifically, for those participants who completed the majority of the program, 57% achieved recovery into non-elevated levels of anxiety, and 54% achieved statistically reliable reductions (March et al., 2018), although these effects were not as strong as those found for the therapist-supported version of BRAVE (March et al., 2009; Spence et al., 2011). Similar to the findings of Jolstedt et al., adherence was problematic for the majority of users in this study, with only 30% completing three or more of the 10 sessions.
Thus, while efforts to disseminate ICBT interventions for child anxiety show promise, across both studies, engagement and adherence were clear issues. In addition, neither of the implementation studies provided detail regarding how individuals experience ICBT delivered in this way, or the precise challenges of integrating such interventions into routine care. Further work is also needed to determine optimal models of care or dissemination that have the capacity to capitalise on the reach and scale of self-guided ICBT interventions, as well as the clear benefits of therapist support that seem necessary for many young people.
1.2. Stepped-care
Stepped-care frameworks provide an opportunity to enhance the clinical and cost efficiency of ICBT and have been applied extensively in health care settings and adult mental health (Van Straten et al., 2015). This approach ‘steps up’ support or intervention intensity on an ‘as needs’ basis (following an assessment) to ensure optimal benefits are achieved from treatment, while minimising burden and cost (Salloum et al., 2014). Preliminary evidence supports the use of stepped-care in face-to-face CBT for childhood anxiety disorders, although very few studies exist and no empirically-supported model of stepped-care has been determined (Rapee et al., 2017, Tolin et al., 2011, Van Der Leeden et al., 2011). In one study, Van Der Leeden et al. (2011) delivered 10 sessions of manualised face-to-face CBT at Step 1, with 45% of children becoming free of any anxiety diagnosis after this step. Participants who failed to respond were stepped up to second and third treatment phases (additional 5 sessions and enhanced parent involvement) as necessary. A further 17% and 11% of children were free of any anxiety diagnosis following Steps 2 and 3 respectively showing that stepping up intensity/dose was helpful for some children who initially failed to respond.
More recently, Rapee et al. (2017) compared the efficacy of CBT delivered via a stepped-care model with a 12-week evidence-based CBT intervention. The stepped-care model included three possible steps differing in intensity and delivered over a 12-month period. Step 1 was a low-intensity intervention delivered via workbook (for parents of children) or CD ROM (for adolescents) plus four, 30-min telephone therapist sessions, Step 2 involved face-to-face manualised standard CBT, and Step 3 involved a face-to-face, individualised, formulation-based intervention. Each intervention phase stepped up in intensity and therapist skill level (qualifications). The stepped-care model and standard CBT intervention (12-weeks) did not differ in terms of outcomes reported at 12 months (post-treatment), however, total therapist time required to deliver treatment was lower in the stepped-care model. Importantly, the majority of gains were made in the first two steps. The findings of these studies highlight the feasibility of face-to-face or blended models of stepped-care for youth anxiety, and suggest that improved efficiency may primarily be observed through reduced therapist time and potential improvements in cost-efficiency.
The utility of stepped-care models in improving the clinical efficacy and efficiency of ICBT by incorporating a blend of self-help and guided steps is yet to be investigated. Given the positive effects and enormous reach of self-help ICBT, yet the noted superiority of guided ICBT for youth anxiety, there is an opportunity to enhance the overall efficiency of low-intensity ICBT programs before considering stepping up to higher intensity therapist-delivered services. If effective, a stepped-care model of ICBT would retain the benefits of low intensity interventions (lower cost, greater reach, wide geographic and temporal availability) and minimise the costs of ‘stepping up’ by utilising low-intensity therapist support (e.g. phone, email or videoconferencing support) instead of face-to-face support. Thus, it may present a viable model for ICBT dissemination and potential integration into routine care.
In the existing literature, decisions to step-up treatment intensity typically occur after delivery of a core course of CBT, typically involving 10 or more sessions. There are several reasons why ICBT stepped-care models might benefit from a different approach, where assessment and step-up decisions are made much earlier. First, difficulties with engagement and slow progress, especially in self-help ICBT, mean that a substantial proportion of young people do not complete ICBT programs (March et al., 2018). Thus, identifying early signs of non-adherence and response are crucial in ICBT, so that young people can be stepped-up before they disengage entirely. Second, there are some components of ICBT for youth anxiety that would be more likely to be effective when provided with therapist-support. The first half of ICBT programs for youth anxiety typically include the provision of psychoeducation, identification of cognitions, emotions and behaviours, with techniques becoming more complicated as young people progress through sessions. The second half of ICBT programs typically focus on skill rehearsal, and in particular, repeated implementation of key CBT techniques such as exposure hierarchies, which can be more difficult to develop and implement in the absence of a therapist. By including a step-up point immediately after knowledge acquisition, therapist support (if needed) can be provided to assist with the more complex intervention components and real-life skill rehearsal to prevent disengagement.
1.3. The present study
If we are to successfully disseminate ICBT interventions for youth anxiety, it is crucial that 1) we understand more about how individuals experience ICBT interventions clinically, and 2) that they are delivered in a way that allows young people to be connected to therapist support should they not respond to a self-help program. This study aims to conduct an in-depth examination of a stepped-care model of ICBT for youth anxiety disorders, in order to identify how they are experienced by young people and the potential challenges of this approach. Specifically, it utilises a case series design that allows an evaluation of the ICBT intervention as it is applied clinically (Kazdin, 2019). Case series designs are also particularly helpful when first implementing new models of care such as this one, in that they allow inferences to be drawn and outcomes examined in relation to the client's functioning, before, during and after the intervention (Kazdin, 2019) thus providing an initial test of intervention feasibility. In this study, using a methodology previously utilised by the authors (Spence et al., 2008; Cobham et al., 2012), we present three case studies of young people participating in BRAVE Stepped-Care (see Section 2.1 below for description) in order to provide an illustration of how stepped-care ICBT models might work in practice, the complexities and challenges involved, and to examine individual outcomes from this model.
In BRAVE Stepped-Care, young people first receive an initial five sessions of self-help ICBT, after which a decision is made to either ‘step them up’ to five sessions of therapist-supported ICBT or for them to receive five sessions of ongoing self-help, depending on their response. The cases presented in this study aim to highlight these two possible paths in BRAVE Stepped-Care, and are presented to examine the decision-making around the step-up assessment point, the challenges involved in determining whether a young person requires additional assistance, and the subsequent outcomes following completion of the ICBT program.
In addition, in the two cases who were stepped-up to therapist-support, this paper examines how therapist support can be delivered utilising different modalities and the unique challenges of each modality. Specifically, we highlight two different versions of the stepped-care ICBT model from two different clinical trials, one in which therapist support is delivered via email (the format used in early efficacy trials), and one in which therapist support is delivered via videoconferencing (new format currently being evaluated). Thus, this study also allows an examination of stepped-care delivered via different modalities, which can directly inform strategies for integrating ICBT into routine practice.
2. Method
2.1. Design and participants
A case series design was implemented to allow a preliminary examination of the feasibility of this new stepped-care ICBT program and clinical factors associated with its implementation. Three case studies were drawn from two current (at the time of writing) non-inferiority randomised controlled trials comparing stepped-care ICBT (new intervention) to therapist-supported ICBT (gold-standard comparator). In one trial, therapist-support (when needed) is delivered via email and phone support (ACTRN12618001415291) and in the other trial, support is provided via videoconferencing (ACTRN12618001418268). Case study evaluation occurred at the beginning of these trials to examine preliminary utility of the approach. In both trials, participants who self-referred to the BRAVE Self-Help open access program and presented with elevated anxiety were invited to participate in one of these two RCTs (randomly offered). Young people and their parents were informed of the stepped-care procedures, and told that a mid-point assessment would be conducted to help the Psychologist decide whether they might benefit from some extra support for the remainder of the program. Participants were not informed of the specific criteria for being stepped-up and were also not given a choice of whether they would like to step up or stay in self-help. Both trials hold ethical approval through The University of Southern Queensland.
The selection of cases occurred during the initial phases of the two RCTs so that we could provide an early examination of the feasibility of the stepped-care model and examine potential challenges with the step-up process, before the trial was rolled out. Thus, cases were selected from the initial pool of participants enrolled in the two RCTs. Participants were eligible to be included if they had completed the baseline, mid-point and post-treatment assessments, irrespective of the number of sessions completed. Subsequently, cases were selected from a pool of 8 participants who met inclusion criteria. Cases were chosen to be similar on age, gender and primary presenting problem, and to be representative of those who were ‘stepped-up’ or ‘not stepped-up’ (see Section 3).
Data was collected for all participants at baseline (full diagnostic and symptom assessment), through weekly sessions (brief anxiety scale), at mid-point assessment (full anxiety scale assessment to determine step-up requirement), and post-treatment (full diagnostic and symptom assessment). In all cases, the baseline and mid-point evaluation were conducted by the same therapist (author SB), who also delivered therapy to cases who were stepped-up and prepared the written case studies below. Post-treatment assessments were conducted by a blind diagnostic assessor. Data to accompany case studies was prepared by a research assistant (author MF). The measures administered at each time point are described below. Although all three cases experienced positive outcomes from the program, they are not presented as indicators of the effectiveness of the intervention. Rather, they are used to highlight the complexities and challenges involved with stepped-care ICBT, and the potential ways in which this approach might be useful in practice.
2.2. Interventions
2.2.1. BRAVE Self-Help
The BRAVE Self-Help program was adapted from the BRAVE Therapist-Assisted program, an online CBT program for child and adolescent anxiety (March et al., 2009; Spence et al., 2011; Spence et al., 2006). BRAVE Self-Help (March et al., 2018) was designed to be delivered in an open-access, self-help manner without any therapist contact. Similar to the therapist-assisted version of the program, the child-focused self-help program includes 10 sessions of CBT (approximately 45 min duration) covering evidence-based anxiety management strategies such as recognition of physiological symptoms, relaxation, coping self-talk, cognitive restructuring, graded exposure, and self-reinforcement (Rapee et al., 2000; Treffers and Silverman, 2000). The program also incorporates other personalisation and engagement enhancement strategies such as automatic personalised reminder emails (insertion of the participant's name), reinforcement pop-ups, interactive activities, quizzes to check and consolidate learning, practice (fill in) activities and use of visually appealing characters and stories to deliver material. Although there is an accompanying parent program, only the child-focused intervention was utilised in this study. Parents did have access to the parent self-help program, although in this study, none of the parents enrolled in this program.
The content and strategies of the Self-Help version are identical to those of the Therapist-Assisted version, with minor adaptations to material and presentation format in order to encourage learning in the absence of a therapist (see March et al., 2018 for description of translation). For example, the exposure hierarchy session was extended, and a specific hierarchy generation tool created, to assist the young person in developing their step-by-step hierarchy throughout the program. Structural changes were introduced to simplify navigation and enhance access to key resources, regular anxiety assessments and feedback of results via graphs were included, and alert and referral systems were introduced to manage participants who did not improve or who demonstrated very high levels of anxiety. In essence, the program was enhanced to minimise the potential impact of reducing therapist support. In BRAVE Self-Help, participants register for the program and may progress through sessions sequentially, similar to the therapist-assisted version of the program. Automated personalised emails are sent by the program to provide alerts regarding elevated anxiety and appropriate referral options. However, participant data is not monitored and responded to on an individual basis.
2.2.2. BRAVE Stepped-Care
BRAVE Stepped-Care is a combination of BRAVE Self-Help and the original BRAVE Therapist-Assisted program. BRAVE Stepped-Care incorporates 10-sessions, splitting them into two, 5-session treatment steps: Step 1 - self-help ICBT and Step 2 - continued self-help or therapist-assisted ICBT (depending on the results of a mid-point assessment). Step 1 is delivered first, and includes up to 5 sessions of BRAVE Self-Help (psychoeducation and skills acquisition) with a minimum of 5 days in between sessions. Following completion of Step 1 (or 6 weeks, whichever occurs first), young people are directed into an appropriate Step 2 determined by their mid-point assessment. It should be noted that the mid-point assessment occurred by the end of Week 6, irrespective of whether the young person had completed the entire first step of treatment (first five sessions of Self-Help). It was decided that this was more representative of routine care, which would step-up intensity, or change treatment if the young person did not show optimal engagement, rather than waiting for them to complete the first treatment component, which may never actually occur.
At the mid-point assessment, a full anxiety scale (see 2.2.3, 2.3.2) is used to determine whether young people receive more of Step 1 (treatment ‘responders’), or whether they need to be stepped-up into Step 2 for higher intensity treatment (treatment ‘non-responders’; see Section 2.2.3 for more details). Step 1 responders receive the remainder of the five BRAVE sessions through the self-help program (that is, they finish BRAVE Self-Help) and do not receive any additional therapist contact throughout their use of the program. Step 1 non-responders are stepped-up to a higher intensity treatment (Step 2) in the form of BRAVE-Therapist-Assisted and complete the remaining sessions (skill rehearsal and maintenance) with therapist support.
2.2.2.1. Type of therapist assistance
BRAVE Stepped-Care is currently offered using one of two forms of therapist support. In the Email and phone support version of BRAVE Stepped-Care, therapist support includes an initial phone call (30 min) following the mid-point assessment to review program usage and progress to date, establish goals, provide guidance on establishing the exposure hierarchy and to enhance motivation and engagement. Thereon, it includes weekly, email support by the therapist (approximately 15 min per session) that aims to assist with program engagement, provide reinforcement, and to assist in strategy rehearsal and implementation. Emails are sent by the therapist following review of session activities. In the videoconferencing version of BRAVE Stepped-Care, the support is identical with an initial call and weekly support, but is delivered entirely via brief videoconferencing (two-way) calls (audio and visual) instead of phone and Email. Videoconferencing can include discussion between therapist and participant or may also involve screen sharing so both parties can refer to program activities, review responses live, or complete program activities together during the call. Thus, while delivered via different modalities, in both versions of the program therapist support is designed to help overcome the obstacles of the self-help program, through regular, yet minimal contact.
2.2.3. Determining responder status
Responder status at the mid-point assessment was determined through responses to anxiety surveys, along with observed engagement with the program and other case information. First, and as the primary criteria, responder status was examined through improvements demonstrated on the Spence Children's Anxiety Scale Child and Parent report (Nauta et al., 2004; Spence, 1998). Gender-standardised and non-elevated percentile cut-offs have been calculated for these instruments based on normative and clinical youth samples (Spence, 1998; Spence et al., 2003) and are used for reference here. Scores above the 84th percentile (T > 60) are considered elevated, while scores below are considered non-elevated. These cut-offs were used to guide decisions around stepping-up. Upon completion of the mid-point assessment, surveys were scored and recommendations made regarding responder status. Evaluation of the mid-point assessment was conducted by a Clinical Psychologist who had conducted the initial assessment, and recommendations discussed with the lead investigator (SM). ‘Responders’ were identified as those young people who demonstrated a consistent reduction in anxiety into the non-elevated range on either their primary anxiety sub-scale or total scores on the SCAS Parent and Child Report. In contrast, ‘non-responders’ included those who had not demonstrated a reduction to within the ‘non-elevated’ range of anxiety for their primary anxiety and/or total score on the SCAS Parent and Child report by mid-treatment. Second, the number of sessions completed by the mid-point assessment and the way the young person engaged with activities were also taken into consideration when determining whether the young person was a responder. Completion of <3 sessions was deemed to be indicative of non-response at the mid-point. Finally, additional case information was considered to resolve any discrepancies between self-report data and program engagement. For example, answers to program activities that indicated little thought, insight or strategy implementation were deemed to be indicative of non-response.
2.3. Measures
2.3.1. Diagnostic status and functioning
Diagnostic status was assessed using the Anxiety Disorders Interview Schedule for Children–Child Version; ADIS-C (Albano and Silverman, 1996). This semi-structured diagnostic interview was administered via telephone to determine anxiety diagnostic status and associated clinician severity ratings (CSR) on a scale from 0 (absent)-8 (very severe). Administration of the ADIS-C via telephone has been successfully demonstrated in previous research (March et al., 2009; Spence et al., 2011). Assessors administering the ADIS-C were trained in the use of the ADIS-C and received supervision by an experienced Psychologist. The ADIS-C was administered at baseline and post-assessment and was delivered by assessors blind to experimental condition.
Information obtained through the ADIS-C was also used to inform a clinician rating of overall child functioning on the Children's Global Assessment Scale; CGAS (Shaffer et al., 1983). Assessors used information from the ADIS-C to provide a score on the CGAS ranging from 0 to 100. Scores in the 81–100 band represent normal levels of functioning, 61–80 represents slight disability, scores between 41 and 60 are indicative of moderate disability and scores from 1 to 40 indicate serious disability. The CGAS shows good inter-rater and test-retest reliability (Shaffer et al., 1983; Rey et al., 1995).
2.3.2. Anxiety symptoms
Anxiety symptoms were measured using two scales. The Children's Anxiety Scale (CAS-8; Spence et al., 2014) is an 8-item anxiety symptom scale completed by participants at program registration and at every session, to measure total anxiety severity. Items are responded to using a 4-point scale, where 0 = not at all, 1 = sometimes, 2 = often and 3 = always. Item scores are summed to provide a total anxiety score (maximum = 24). The CAS-8 is based on the Spence Children's Anxiety Scale (below) and demonstrates excellent reliability (Spence et al., 2014). Gender-standardised cut-off scores have been determined based on a large normative data set to indicate ‘elevated’ levels of anxiety. Scores ≥11 for females and ≥9 for males indicate elevated levels of anxiety and scores ≥15 for females and ≥12 for males indicate clinical levels of anxiety. The CAS-8 will be used to highlight changes in anxiety at each session.
The full Spence Children's Anxiety Scale-Child & Parent versions (SCAS-C&P; Nauta et al., 2004, Spence, 1998) were also administered at baseline, mid-point and post-assessments. The parent and child SCAS provide a comprehensive anxiety symptom assessment and demonstrate good psychometric properties (Nauta et al., 2004; Spence et al., 2003). Participants report how frequently symptoms occur on a 0 (never) to 3 (always) scale, with items summed to provide a total anxiety score, as well as sub-scales according to anxiety type (Separation anxiety, Generalised Anxiety, Specific Phobia, Panic Disorder, Social Anxiety). Gender-standardised cut-offs indicating elevated anxiety are available for the total and sub-scale scores. The SCAS-C/P scores were used as a secondary outcome measure and to determine ‘step-up’ decisions at mid-intervention.
2.3.3. Anxiety interference
The Child Anxiety Life Interference Scale (CALIS) provides an assessment of life interference and impairment experienced by the child (as reported by children and parents), as well as interference experienced by the parent themselves (parent report). Items are scored on 0 (not at all) to 4 (a great deal) scale to measure total impairment in child and parent lives. The CALIS shows good internal consistency, good convergent and divergent validity and is sensitive to treatment change (Lyneham et al., 2013). Interference in functioning is used as a secondary outcome measure in this study.
2.3.4. Satisfaction
Satisfaction was measured through a 5-item scale used in the evaluation of the Self-Help BRAVE program (March et al., 2018). This scale includes items that ask whether they would tell a friend about the program, how helpful the program was, how happy they were with the program, how much it helped to reduce their anxiety and their overall satisfaction with the program. Participants were asked to respond using a 5-point Likert scale from 1 (Definitely Not/Not at all/Very Bad) to 5 (Definitely Yes/Very Much/Very Good), depending on the question. Total satisfaction and mean item scores were calculated.
2.4. Assessment of change
Several methods were used to determine level of clinical improvement. First, changes in anxiety symptoms on the SCAS-C/P from pre- to mid- and pre- to post-treatment were examined, using two methods and in line with the procedure employed in March et al. (2018). Changes in raw scores were examined to determine whether or not the participant had shifted from elevated to non-elevated categories (using percentile and T-score cut-offs) and Reliable Change Indices (RCI; Jacobson and Truax, 1991) were calculated. The RCI allows determination of whether changes made by the individual are significantly greater than that due to measurement error, and is calculated based on a product of the scale's reliability and standard deviation (Jacobson and Truax, 1991). In this study, test-retest reliability and standard deviations were drawn from Arendt et al. (2014). For analyses examining RCIs at mid-treatment, 2-week test-retest reliability was used and at post-treatment, 3-month test-retest reliability was used. RCIs for each participant were then categorised as “reliable improvement”, “no improvement” or “reliable deterioration”. The use of T-score and RCI analyses allowed the determination of whether the changes made by individual participants in these case studies were both clinically (T-score change) and statistically (RCI score) significant. Second, changes in diagnostic status and clinician severity ratings from baseline to post-treatment assessment were examined. Third, changes in life interference as reported by the CALIS, using raw scores and RCIs were examined. Percentile and T-score cut-offs are not available for the CALIS, and therefore we were not able to conduct clinical improvement analyses on this measure.
3. Results: case illustrations
Case study descriptions (background, clinical diagnosis and treatment participation) were prepared by a Clinical Psychologist (author SB) who had completed the baseline assessment, mid-point evaluation and delivered therapy (where it was required) to the selected cases. Survey data was collated and prepared by a research assistant on the project (author MF). Case studies were prepared following previous templates utilised by the research team (Spence et al., 2008; Cobham et al., 2012).
3.1. Case study 1: 10-year old male, not stepped-up
3.1.1. Presenting problem and background
Will was a 10 year old boy who resided with his intact family (biological parents and two younger siblings). Will presented with worries and rumination about his academic performance and friendships. He also reported a specific fear of darkness and was unable to sleep without a nightlight and hallway light on, which had led to difficulties sleeping and occasional nightmares. Will's anxiety started in Grade 1 with Will becoming tearful and worried when making mistakes, and soon progressing to anxiety in anticipation of examinations, resulting in attempts of school refusal. These worries also extended to the home, with Will becoming anxious while completing homework and subsequently attempting to avoid these tasks. Will's Mother reported that Will's darkness fears also emerged around the same time. Will had not received any formal supports for his mental health, but had received some extra support to manage his difficulties with examination anxiety.
3.1.2. Baseline assessment
Table 1 outlines the diagnostic severity ratings and questionnaire results for Will at pre-, mid- and post-treatment. Fig. 1 depicts the weekly CAS-8 anxiety ratings obtained at the beginning of each session. At pre-treatment, the ADIS-C indicated that Will met DSM-5 criteria for GAD (primary diagnosis) and Specific Phobia of Darkness. The CSR ratings (see Table 1) placed him in the ‘Definitely Disabling’ range at pre-treatment and CGAS scores indicated he fell within the ‘Some Noticeable Problems’ band of overall functioning. Scores on the parent and child SCAS were consistent with the ADIS-C diagnoses, with both reporting multiple elevated scores. Scores on the CALIS indicated that Will's anxiety was interfering substantially with his life and that of his parents.
Table 1.
Case Study 1 (Will) – Pre- to post-treatment outcomes and diagnostic information
| Measure | Pre | Mid | Post | RCI Pre-Mid | RCI Pre-Post |
|---|---|---|---|---|---|
| Number of sessions completed | 0 | 5 | 10 | - | - |
| CSR GAD (Primary) | 5 | - | NIL | - | - |
| CSR Specific Phobia | 5 | - | NIL | - | - |
| CGAS | 58 (Some Noticeable Problems) |
- | 80 (Doing All Right) |
- | - |
| SCAS-C | |||||
| Social Phobia | 6 | 5 | 0 | -0.56 | -2.73b |
| Panic | 8a | 7a | 8a | -0.37 | 0.0 |
| Separation | 5 | 2 | 0 | -1.72 | -3.16b |
| Physical Injury | 5a | 2 | 2 | -2.11b | -1.91 |
| GAD | 12a | 6 | 2 | -3.56b | -5.14b |
| OCD | 5 | 5 | 4 | 0.0 | -0.44 |
| Total | 41a | 27 | 16 | -1.85 | -3.21b |
| SCAS-P | |||||
| Social Phobia | 8a | 4 | 5 | -2.43b | -1.92 |
| Panic | 8a | 4a | 5a | -2.87b | -1.60 |
| Separation | 6a | 3 | 3 | -2.1 3b | -1.92 |
| Physical Injury | 3 | 2 | 2 | -0.89 | -0.98 |
| GAD | 9a | 6a | 6a | -2.29b | -1.59 |
| OCD | 5a | 2a | 2a | -1.70 | -1.82 |
| Total | 39a | 21 | 23 | -3.55b | -2.51b |
| CALIS-C | 18 | - | 8 | - | - |
| CALIS-P Child Interference Parent Interference |
24 11 |
- - |
9 6 |
- - |
- - |
| Satisfaction Child | - | - | 3.2/5 | - | - |
RCI = Reliable Change Index score; CSR = Clinician Severity Rating; CGAS = Children’s Global Assessment Scale; SCAS-C = Spence Children’s Anxiety Scale – Child Version; SCAS-P = Spence Children’s Anxiety Scale – Parent Version; CALIS-C = Child Anxiety Life Interference Scale – Child Version; CALIS-P = Child Anxiety Life Interference Scale – Parent Version
elevated scores
RCI value indicates a reliable improvement
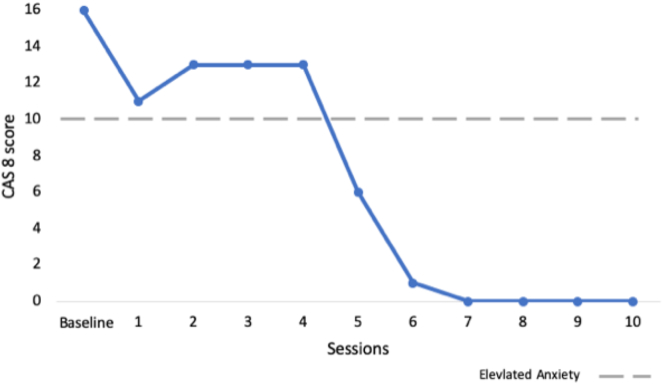
Fig. 1.
Case study 1 (Will) - session-by-session CAS-8 scores.
3.1.3. Treatment participation
3.1.3.1. Step 1 – self-help treatment
During Step 1, Will completed sessions on average every nine days, providing complete and thoughtful answers that indicated that he understood the content and was able to apply strategies to his own situations. Further, Will's responses to session activities provided evidence that he was practicing homework tasks and in particular, that he was making good use of relaxation strategies. Will's mother reported noticeable improvement in his worries during Step 1, noting that Will ruminated less about upcoming tests and examinations, and was more willing and confident when completing homework tasks.
3.1.3.2. Mid-point assessment
At the mid-point assessment, Will's scores on the SCAS-C indicated that his primary presenting problem (GAD sub-scale score), along with his Total Anxiety score, had reduced markedly and were no longer elevated. As can be seen in Table 1, reliable improvements on the RCI were noted for the GAD and Physical Injury sub-scales. Further, as indicated in Fig. 1, Will's CAS-8 scores showed a steady decline from baseline to Session 5 into the non-elevated range. Parent report on the SCAS indicated a decrease in Total Anxiety and all sub-scale scores, although the GAD sub-scale score remained slightly elevated at the mid-point assessment. Reliable improvements on the RCI were evident for all sub-scales except for OCD and Physical Injury. Further reports from Will's mother highlighted substantial behavioural changes with Will procrastinating much less on homework tasks, displaying less anxiety leading up to his final Grade examinations, and reporting fewer difficulties with sleep.
In Will's case, inconsistencies between parent and child report presented some challenges when making decisions about whether Will would benefit from additional support through the program. While Will's mother did not report substantial improvements in his primary diagnosis (GAD), in this case, the mid-point decision was made within the context of broad improvements demonstrated across other anxiety scales as well as meaningful engagement with program activities. The decision was therefore made for Will to continue with the Self-Help program at Step 2 and not be stepped-up.
3.1.3.3. Step 2 – continued self-help treatment
Throughout Step 2, Will completed all remaining ICBT sessions, on average 14 days apart. Will and his family travelled overseas during Step 2, resulting in some time off between sessions. However, the family arranged to continue with sessions and to implement the strategies as best they could while travelling. During Step 2, Will constructed an exposure hierarchy targeting his worries about doing homework and examinations, and reported some successful practice of these steps. However, he also provided responses to session activities that indicated success with, and a preference for, using relaxation and problem solving strategies to manage his worries. Will's scores on the CAS-8 remained at a score of 0 for the last four sessions of Step 2, indicating that he was not experiencing active anxiety during the last few weeks of the program.
3.1.4. Post-treatment assessment
At post-treatment, Will had completed all 10 BRAVE sessions, the clinical interview data indicated that he no longer met criteria for any anxiety diagnosis, and his scores on the CGAS had improved markedly. With respect to the anxiety questionnaires, Fig. 1 shows that Will's CAS-8 scores decreased slowly over the first half of the program (Step 1) but showed a dramatic decrease at the introduction of exposure and problem solving. Reports on the Child and Parent SCAS indicated a substantial reduction in Will's Total Anxiety score into the non-elevated range, with both reports also demonstrating reliable improvements on the RCI. In addition, Will reported reductions on the SCAS-C into the non-elevated range for GAD (primary problem) and Physical Injury (secondary problem) sub-scales, and statistically reliable improvements noted for the Social, Separation and GAD sub-scales. In contrast, Will's mother reported that Panic, GAD and OCD symptoms, while reduced from pre-treatment, remained in the elevated range and were not indicative of statistically reliable change. Following treatment, both Will and his mother reported substantial reductions in interference and Will reported moderate satisfaction with the program, noting the helpfulness of relaxation strategies.
3.2. Case study 2: 10-year old male, stepped-up to videoconferencing therapist support
3.2.1. Presenting problem and background
Matthew was a 10 year old boy who resided with his intact biological family (parents and 2 older brothers). Matthew's primary presenting problem was excessive worry and rumination about things he saw on the news, war, monsters and scary popular fiction. These worries impacted on Matthew's capacity to concentrate on his coursework at school and home, caused irritability and conflict, and fatigue at the end of the day due to constant rumination and hyper vigilance. Matthew also presented with a fear of darkness and separation, and slept with a nightlight on every night, often requesting that his mother stay with him until he fell asleep. Matthew had bad dreams about parental death, and worried about his parents being harmed while he was at school. Matthew was able to sleep over at close friends' or relative's houses, as long as he had previously spent time with them and trusted them.
Matthew's mother reported that his separation symptoms first appeared in grade 1, becoming tearful and requesting to stay home most mornings. Matthew's symptoms of anxiety re-emerged two years prior to presentation, when he became increasingly fearful of fictional characters and began fearing the dark. He had not received any formal professional mental health assistance for his difficulties previously.
3.2.2. Baseline assessment
Table 2 outlines the diagnostic severity ratings and questionnaire data for Matthew at pre-, mid- and post-treatment. Fig. 2 depicts the weekly CAS-8 anxiety ratings obtained at the beginning of each session. At pre-treatment, the ADIS-C indicated that Matthew met DSM-5 criteria for Generalised Anxiety Disorder (GAD; primary diagnosis), Specific Phobia of Darkness, and Separation Anxiety Disorder (SAD). The ADIS-C CSR ratings placed him in the ‘Definitely to Markedly Disturbing’ ranges of anxiety severity at pre-treatment. Matthew's overall functioning and impairment according to the CGAS fell within the 50–60 band at pre-treatment (Obvious Problems). Scores on the parent- and child-report SCAS were consistent with the ADIS-C diagnoses, with multiple elevated scales. Matthew's mother also reported that he experienced elevated levels of Panic and OCD, although these were not reported by Matthew at baseline. Finally, scores on the CALIS indicated that Matthew's anxiety was interfering substantially in his life, but impacted less on his parents' functioning.
Table 2.
Case Study 2 (Matthew) – Pre- to post-treatment outcomes and diagnostic information
| Measure | Pre | Mid | Post | RCI Pre-Mid | RCI Pre-Post |
|---|---|---|---|---|---|
| Number of sessions completed | 0 | 5 | 10 | - | - |
| CSR GAD (Primary) | 6 | - | NIL | - | - |
| CSR Specific Phobia | 5 | - | NIL | - | - |
| CSR Separation Anxiety | 5 | - | NIL | - | - |
| CGAS | 53 (Some noticeable Problems) |
- | 80 (Doing All Right) |
||
| SCAS-C | |||||
| Social Phobia | 2 | 3 | 1 | 0.56 | -0.45 |
| Panic | 0 | 0 | 10a | 0.0 | 4.61c |
| Separation | 10a | 11a | 4 | 0.57 | -3.79b |
| Physical Injury | 1 | 3 | 1 | 1.41 | 0.0 |
| GAD | 12a | 12a | 12a | 0.0 | 0.0 |
| OCD | 6 | 6 | 6 | 0.0 | 0.0 |
| Total | 31 | 35 | 34 | 0.53 | 0.39 |
| SCAS-P | |||||
| Social Phobia | 5 | 2 | 4 | -1.82 | -0.64 |
| Panic | 7a | 3a | 2a | -2.87b | -2.67b |
| Separation | 7a | 4 | 4 | -2.13b | -1.92 |
| Physical Injury | 4 | 2 | 3 | -1.78 | -0.98 |
| GAD | 11a | 10a | 8a | -0.76 | -1.59 |
| OCD | 2a | 2a | 2a | 0.0 | 0.0 |
| Total | 36a | 23 | 23 | -2.57b | -2.04b |
| CALIS-C | 18 | - | 23 | - | - |
| CALIS-P Child Interference Parent Interference |
20 9 |
- - |
17 8 |
- - |
- - |
| Satisfaction Child | - | - | 4.2/5 | - | - |
CSR = Clinician Severity Rating; CGAS = Children’s Global Assessment Scale; SCAS-C = Spence Children’s Anxiety Scale – Child Version; SCAS-P = Spence Children’s Anxiety Scale – Parent Version; CALIS-C = Child Anxiety Life Interference Scale – Child Version; CALIS-P = Child Anxiety Life Interference Scale – Parent Version
elevated scores
RCI value indicates a reliable improvement
RCI value indicates reliable deterioration
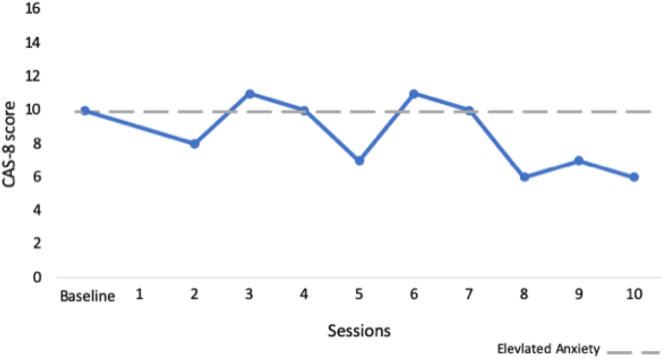
Fig. 2.
Case study 2 (Matthew) - session-by-session CAS-8 scores.
3.2.3. Treatment participation
3.2.3.1. Step 1 – self-help treatment
During Step 1 of treatment, Matthew completed five sessions of BRAVE approximately eight to nine days apart, although he skipped through sessions quite quickly as indicated by his short or incomplete answers to session activities. Matthew showed evidence of completing some homework tasks between sessions, although his responses showed an inability to flexibly apply strategies to home and school situations. During Step 1, Matthew's mother reported that he had developed a greater awareness of his anxious body signs, and was able to better articulate his anxiety to his parents and siblings. However, she reported that he continued to have difficulties with concentration and became irritable with small changes in his environment. Matthew's responses to session activities demonstrated strong evidence of black and white thinking patterns, which appeared to prevent him from thinking flexibly about the strategies learned and how he might apply them to his anxious experiences.
3.2.3.2. Mid-point assessment and step-up decision
By the mid-point assessment, Matthew had completed five sessions. As is evident from Table 2, there were some inconsistencies between parent and child report on the SCAS. Importantly, both Matthew and his mother reported that his primary anxiety problem had not reliably improved, nor shifted from the elevated range. Although the parent-reported SCAS indicated statistically reliable reductions in Total Anxiety score and separation anxiety into the non-elevated range, Matthew's report did not.
Thus, two distinct challenges in deciding whether or not to step-up were evident in Matthew's case. First, discrepancies in parent and child reports were once again apparent, with Matthew failing to report reductions in anxiety, despite improvements noted by his mother. This highlights the potential problem with relying on parent or child report alone. Second, although Matthew demonstrated reductions in anxiety symptoms by the midpoint (according to his Mother), notably, these improvements were not evident for his primary diagnosis, the focus of treatment. Thus, one challenge was whether or not improvement on secondary anxieties were sufficient to continue with the self-help program. In this case, given that Matthew's engagement with the program was not optimal through Step 1 (e.g. skipping through sessions), and his primary anxiety of GAD remained elevated, the decision was made for Matthew to step-up to the therapist-supported treatment at Step 2, in order to promote lasting change and change on the primary diagnosis.
3.2.3.3. Step 2 – therapist-assisted treatment
Upon commencing Step 2, the initial videoconferencing session focused on rapport building, skill acquisition and implementation. Matthew then continued to complete the remaining five ICBT sessions with brief videoconferencing support, approximately nine days apart. Following completion of Step 2, Matthew also went on to complete two additional Booster sessions. Videoconferencing calls were primarily used to reinforce Matthew's existing use of BRAVE strategies (i.e. he was particularly good at problem solving when worried) and to help Matthew apply the other BRAVE strategies to anxious situations. In total, the therapist provided 137 min of therapist support (including reviewing responses and videoconferencing sessions). Throughout Step 2, Matthew demonstrated autonomy in developing and implementing his exposure hierarchy, and the therapist phone call focused on ensuring that the steps of his hierarchy were more specific, evenly spaced and realistic. Given that Matthew was successfully using problem solving to manage his generalised worries, his exposure hierarchy targeted his fear of darkness in the first instance, which was interfering with his sleep and making him cognitively vulnerable to anxiety during the day.
By Session 8, Matthew spoke about facing his anxieties with more confidence and reported often engaging in deliberate exposure whenever a chance arose. By Session 9, Matthew had successfully attempted the last step on exposure hierarchy, and by Session 10 he was sleeping by himself in the dark six out of seven days of the week. Matthew noted some difficulties sleeping when he was tired, which he attributed to having less cognitive energy to reframe his anxious cognitions. Matthew was encouraged to problem solve these barriers to intervention and came up with several solutions to manage his fatigue, including using relaxation strategies before he went to bed.
At the end of Step 2, Matthew was encouraged to develop further exposure hierarchies to reduce patterns of rumination related to more general worries. However, at this time, Matthew reported a noticeable decrease in rumination which he attributed to elimination of his darkness phobia and improved sleep. Matthew also indicated a preference for use of problem solving strategies to face general worries given his previous success with this strategy.
3.2.4. Post-treatment assessment
At post-treatment, the clinical interview and questionnaire data indicated that Matthew no longer met DSM 5 criteria for any anxiety diagnoses and that his scores on the CGAS had improved substantially, with only slight impairment in functioning at home and with peers. Matthew reported a significant improvement in his ability to regulate his emotions, and a subsequent improvement in his relationships with family and teachers. Matthew's mother corroborated Matthew's behavioural improvements and noted that Matthew was more equipped to manage unexpected changes in his environment (i.e. when parents were delayed in picking him up from school) and required fewer prompts to redirect his concentration back to his schoolwork.
With respect to questionnaire results, Fig. 2 demonstrates that Matthew's CAS-8 scores remained elevated during Step 1, but decreased steadily once videoconferencing therapist-assistance was introduced. Parent report indicated reductions on the Total Anxiety score, and Separation Anxiety sub-scale score into the non-elevated range. Matthew's reports also indicated substantial reductions in Separation Anxiety (the target of his exposure hierarchy). However, both Matthew and his mother continued to report elevated levels on the GAD sub-scale, and Matthew also reported elevated levels of Panic not present at baseline. This 10-point increase in the Panic sub-scale also meant that his Total Anxiety score on the SCAS-C report did not reduce over time. Elevations on the Panic subscale may reflect either improved ability to identify Panic symptoms, or, an increase in Panic or environmental stressors immediately before completion of the post-treatment questionnaires. RCI scores demonstrated that Matthew showed statistically reliable reductions in parent-reported Total Anxiety and Panic, and child-reported Separation scores. Despite diagnostic and behavioural improvements, Matthew's anxiety continued to interfere somewhat with his functioning according to the CALIS.
Matthew reported high satisfaction with the program, particularly noting the exposure hierarchy and videoconferencing calls which provided him with someone to talk to, and problem solve with, about his everyday difficulties. From the therapist's perspective, videoconferencing supported Matthew to develop greater insight and awareness of how he could utilise BRAVE strategies to manage his difficulties. The use of the videoconferencing platform also allowed for the inclusion of Matthew's mother in the intervention to share progress, encourage positive parental response, and manage the practicalities associated with the exposure hierarchy.
3.3. Case study 3 (12-year old male, stepped-up to email support)
3.3.1. Presenting problem and background
Edward was a 12-year-old boy who resided with his intact biological family (both parents and younger sister). Edward's primary presenting problem was excessive worry about school, health, interpersonal relationships and new or unfamiliar situations. He reported being anxious about attending school, and had started to isolate himself from his peers in an effort to avoid any potential bullying or judgement. He had subsequently developed concerns about speaking to others, and speaking out in class, for fear that his peers would perceive him to be “different”.
Edward also reported feelings of loneliness, helplessness and low mood as a result of spending less quality time with his peers. He reported feeling helpless in his capacity to manage his anxiety, and occasional thoughts that life would be “easier” if he was not present, or if he ran away. Edward denied any current or historical intent to deliberately harm himself and attributed his low mood to his symptoms of anxiety. He noted periods of feeling “down” after anxiety-provoking events.
Edward's mother reported that his symptoms of anxiety and depression had emerged two years prior when he was bullied at school. During this period, Edward attempted to avoid school and became upset and tearful each morning. Since transitioning to Year 7, Edward's mother noted that his school avoidance had become less problematic, and he appeared to have a good group of friends. However, in the last few months prior to presentation, Edward had become more withdrawn at home and school and experienced increased anxiety.
3.3.2. Baseline assessment
Table 3 outlines the diagnostic and questionnaire results for Edward at pre-, mid- and post-treatment, and Fig. 3 depicts the weekly CAS-8 anxiety ratings. At pre-treatment, results from the ADIS-C indicated that Edward met DSM-5 criteria for GAD (primary diagnosis), Social Anxiety Disorder and Major Depressive Disorder. The CSR ratings placed him in the ‘Definitely to Markedly Disturbing’ range of anxiety severity. Scores on the parent and child SCAS indicated elevated levels of Total anxiety, Social Phobia, Panic, GAD and OCD. Edward also reported elevated Separation anxiety, although this was not reported by his mother. Scores on the CALIS indicated that Edward's anxiety was interfering substantially in his life, although it was causing greater problems according to his parent's report.
Table 3.
Case Study 3 (Edward) – Pre- to post-treatment outcomes and diagnostic information
| Measure | Pre | Mid | Post | RCI Pre-Mid | RCI Pre-Post |
|---|---|---|---|---|---|
| Number of sessions completed | 0 | 3 | 6 | - | - |
| CSR GAD (Primary) | 6 | - | NIL | - | - |
| CSR Social Phobia | 5 | - | NIL | - | - |
| CSR Major Depressive | 5 | - | NIL | - | - |
| CGAS | 53 (Some noticeable Problems) |
- | 78 (Doing All Right) |
||
| SCAS-C | |||||
| Social Phobia | 12a | 11a | 5 | -0.56 | -3.18b |
| Panic | 9a | 7a | 1 | -0.74 | -3.69b |
| Separation | 7a | 5a | 3 | -1.15 | -2.52b |
| Physical Injury | 2 | 4a | 3 | 1.41 | 0.64 |
| GAD | 11a | 8a | 4 | -1.78 | -3.60b |
| OCD | 8a | 6 | 1 | -0.84 | -3.09b |
| Total | 49a | 41a | 17 | -1.06 | -4.11b |
| SCAS-P | |||||
| Social Phobia | 12a | 12a | 9a | 0.0 | -1.92 |
| Panic | 3a | 5a | 0 | 1.44 | -1.60 |
| Separation | 4 | 5a | 3 | 0.71 | -0.64 |
| Physical Injury | 2 | 1 | 0 | -0.89 | -1.95 |
| GAD | 8a | 9a | 5a | 0.76 | -1.59 |
| OCD | 2a | 3a | 2a | 0.57 | 0.0 |
| Total | 31a | 35a | 19 | 0.79 | -1.88 |
| CALIS-C | 18 | - | 9 |
- |
- |
| CALIS-P Child Interference Parent Interference |
23 11 |
- - |
16 14 |
- - |
- - |
| Satisfaction Child | - | - | 3.4/5 | - | - |
CSR = Clinician Severity Rating; CGAS = Children’s Global Assessment Scale; SCAS-C = Spence Children’s Anxiety Scale – Child Version; SCAS-P = Spence Children’s Anxiety Scale – Parent Version; CALIS-C = Child Anxiety Life Interference Scale – Child Version; CALIS-P = Child Anxiety Life Interference Scale – Parent Version
elevated scores
RCI value indicates a reliable improvement
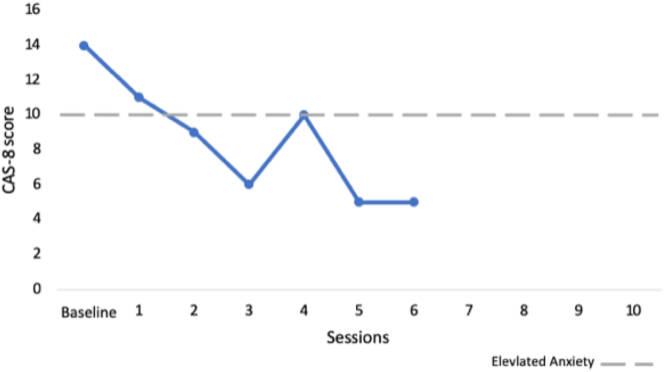
Fig. 3.
Case study 3 (Edward) - session-by-session CAS-8 scores.
3.3.3. Treatment participation
3.3.3.1. Step 1 – self-help treatment
During Step 1 of treatment, Edward progressed slowly through the program, completing only three of the five sessions 10 to 11 days apart. His responses to initial sessions were brief and lacked detail, indicating that he was speeding through activities. In addition, he often failed to report on homework tasks. Edward's mother reported some improvement in his anxiety symptoms through the first five weeks of the program, noting that he had become slightly less withdrawn in the home context, and was spending less time in his room by himself. She also noted that Edward exhibited fewer anxiety symptoms prior to attending school, and appeared brighter (“less drained”) when he came home from school.
3.3.3.2. Mid-point assessment and step-up decision
By the mid-point assessment, Edward had completed only three sessions. As is evident from Table 3, Edward's anxiety had reduced but remained elevated. Although Edward's CAS-8 scores had reduced into the non-elevated range by mid-treatment, both child and parent SCAS report indicated that his Total Anxiety score, GAD, social, separation, physical injury, OCD and panic sub-scale scores all remained elevated. Importantly no statistically reliable change was made on the RCI calculations, on both parent and child reports. Further, completion of only three ICBT sessions within Step 1 suggested sub-optimal engagement with the program. Given the consistency across reports and poor engagement, the decision was therefore made for Edward to step-up to the therapist-supported treatment at Step 2, and he received therapist-assistance via weekly emails plus one phone call to support development of the exposure hierarchy.
3.3.3.3. Step 2 – therapist-assisted treatment
The initial telephone call in Step 2 focused on building rapport, exploring Edwards' engagement in the strategies so far and helping him to structure his goals for the program. Following this call, Edward continued with the ICBT sessions (starting with Session 4) and received email support following completion of each session. Throughout Step 2 (and up to the post-treatment assessment point), Edward completed a further three sessions (six out of 10 in total). His engagement with the program improved, completing sessions approximately nine to ten days apart and engaging more with activities. Specifically, he was observed to be more thoughtful in his completion of session activities (i.e. writing longer responses to questions) and appeared to apply the strategies more frequently between sessions, as indicated by homework practice.
Throughout Step 2, emails primarily focused on reinforcing Edward's engagement and completion of sessions, implementation of skills, and supporting the development of the exposure hierarchy. For example, Edward had reported some reluctance to engage in relaxation exercises because he was conscious of others knowing that he was using these strategies. Problem solving was used to encourage the use of more subtle techniques at school (i.e. muscle tension and relaxing - of toes, leg muscles or clenched fists under the table).
Edward identified wanting to focus on his general social and performance worries as a goal for his exposure hierarchy as this would target both his primary GAD and social anxiety. However, he had difficulty brainstorming incremental steps, with the majority he put forward being highly anxiety provoking (i.e. giving a speech in class; performing in a play). Therapist support was directed at helping Edward to develop less anxiety-provoking steps on his ladder, and he subsequently reported greater efficacy in managing smaller, less threatening social interactions. Therapist support was also directed towards helping Edward recognise and reinforce the everyday social interactions he was managing without any anxiety, in order to encourage and build upon his sense of control and mastery. Edward was somewhat meticulous in working through his exposure hierarchy, and on occasion, he appeared frustrated with his slow progress. Weekly emails encouraged him to review his steps, and to consider whether he needed to adapt them to make them more achievable. In total, the therapist provided 45 min of therapist support during Step 2, including reviewing responses and drafting emails, and the mid-point phone call.
Sessions were interrupted after Session 5, when Edward and his family travelled overseas unexpectedly to support his Grandfather who had fallen unwell. On return home, Edward and his Mother have reported difficulties getting back into the routine of the program and subsequently completed only one additional session. Edward's Mother reported that Edward became disengaged from the program primarily because he was no longer experiencing anxiety.
3.3.4. Post-treatment assessment
By post-treatment, Edward had completed six sessions, and the clinical interview data indicated that he no longer met criteria for any anxiety diagnosis. Further, his overall functioning on the CGAS had improved, with only slight impairment in functioning at home and with peers. Fig. 3 reveals that Edward's CAS-8 scores remained elevated over the first few sessions of the program (Step 1) but began to decrease during Step 2, finishing within the non-elevated range. His weekly anxiety ratings showed a slight peak around the time that therapist support commenced and cognitive restructuring was introduced. Edward's responses on the SCAS-C indicated that his Total Anxiety score and all sub-scale scores had reduced into the non-elevated range, with RCI scores indicating reliable improvement for all sub-scales except Physical Injury. Although parent-report also showed a substantial reduction in Total Anxiety into the non-elevated range, Edward's social anxiety and GAD sub-scale scores, while reduced, were still in the elevated range according to parent report. No statistically reliable changes were noted on the Parent report, although RCIs were close to the 1.96 cut-off for significance. Similarly, although Edward reported a reduction in overall life interference, his mother did not, a result that is somewhat inconsistent with the other findings. Edward reported moderate satisfaction with the program, particularly enjoying the phone calls from the BRAVE Team (initial ADIS-C phone interview and Exposure phone call) and the online format and emails, noting that these were less intimidating then speaking with someone face-to-face.
4. Discussion
The outcomes of these case studies were generally positive and highlight the ways in which stepped-care models of ICBT can be successfully applied in the treatment of child and adolescent anxiety. Importantly, each of the cases experienced multiple presenting problems and a long history of anxiety. Though they engaged in, and responded differently to the stepped-care ICBT intervention, all demonstrated substantial improvements over the course of the program. Improvements were observed with respect to both the primary and secondary anxiety diagnoses, indicating that effects of the overall program generalised to other anxiety problems. The program was rated positively by the young people and several helpful features of the stepped-care model were reported. The positive response noted in these cases will need to be confirmed in randomised controlled trials and it will be particularly important to determine overall patterns of response at mid- and post-treatment, common reasons for stepping-up, and response to the different steps of treatment. The following section highlights some of the challenges and successes of the stepped-care approach.
4.1. Participation in treatment step 1: self-help sessions
In terms of participation with the first step (first five sessions of BRAVE Self-Help), the three cases demonstrated varying patterns of engagement and adherence, not dissimilar to those reported by March et al. (2018). Importantly, in addition to the number of sessions completed (3–5 sessions), each case showed distinct differences in how they engaged with the program and its activities, with some engaging thoughtfully, setting appropriate goals and proactively implementing treatment techniques, and others struggling to apply knowledge and techniques to their own personal contexts. The cases also progressed at different speeds, and this certainly restricted the progress made by Edward who completed sessions 10–11 days apart during Step 1. This variation in engagement and slow speed of session completion is consistent with our previous trials that have demonstrated young people are slower to complete ICBT sessions than traditional face-to-face therapy (March et al., 2009; Spence et al., 2011). These patterns of engagement highlight the challenges of undertaking CBT without therapist support, and ultimately shaped the step-up requirements of each case, discussed in more detail below.
4.2. Reasons for stepping-up or continuing with self-help
The results of this case study highlight that decisions to step-up (or not) need to be grounded in consideration of multiple factors, including anxiety improvement (particularly on comprehensive assessment scales), adherence, engagement, acquisition of skills and a combination of parent and child reports of symptoms and behavioural improvement.
4.2.1. Improvements in anxiety
In all three cases, the full SCAS provided more valuable information than the brief CAS-8 when determining step-up requirements. Generally speaking, all cases showed reductions on the brief scale. However, two cases (Edward and Matthew) failed to show substantial gains in their primary anxiety diagnosis (as reported on the full scale) following the knowledge acquisition phase of treatment and thus, failed to respond adequately to Step 1. The lack of improvement on their primary anxiety were consistent with their noted engagement problems with the program (see Section 4.2.2). For Matthew, although he may have sensibly chosen to focus on less severe anxieties in order to gain confidence, this may also represent avoidance of his primary anxiety disorder (GAD), or, avoidance due to increased anxiety when being asked to confront these worries. In contrast, Will showed reductions on the brief and full scales, including Total and specific sub-scale scores, indicating greater gains made through treatment Step 1, especially on his primary anxiety problem.
While brief symptom measures may provide a good overview of anxiety level, given the lack of corresponding change on the full SCAS-C and SCAS-P, they are insufficient as a single indicator to base step-up decisions on. Using a comprehensive measure of anxiety that is able to capture improvements on primary and secondary anxiety problems will be of greatest use in determining step-up requirements, especially when it is not feasible to incorporate diagnostic assessments at the step-up point.
4.2.2. Adherence and engagement
It was apparent through the three cases presented that improvements on anxiety were not the only indicator of response and non-response. Engagement and adherence to the program emerged as key factors that should be examined when considering whether or not to step-up treatment. Importantly, simple measures of adherence such as the number of sessions completed were not necessarily consistent with reductions in anxiety symptoms. Rather, in-depth examination of participation was required to more accurately determine whether a young person had made progress through the program, acquired new knowledge and skills, and applied the new skills to their own personal situation. This was achieved through examination of the young person's completion of session activities (number and timing), types of responses provided (brief, thoughtful, comprehensive), homework participation (frequency and insights), acquisition of knowledge (accuracy) and application of techniques to their personal context (examples of practice).
It was interesting to note the diversity in patterns of engagement across the cases. For example, Matthew (non-responder), despite showing good adherence to the program on the surface (completion of all sessions, timely progression), failed to engage deeply with activities, providing only very brief answers and commentary of his practice. Through examination of his responses in the first treatment step, it was apparent that Matthew was unable to take the techniques acquired and apply them to his own situations, a skill crucial in achieving positive outcomes and generalisation beyond the program. In the case of Edward, he completed only three sessions during the first step of treatment, at a slow pace and with additional signs of non-engagement with treatment content. Specifically, he provided vague treatment goals, brief answers to treatment activities, failed to complete homework, and actively reported not using relaxation strategies in anxiety-provoking situations as they further exacerbated his anxiety. Thus, there were multiple and clear indicators of non-response through examination of his participation in treatment, yet they were very different to those of Matthew, who on the surface adhered to treatment. For Will (responder) on the other hand, there was clear evidence of engagement and treatment adherence, as evidenced by completion of all sessions approximately 9 days apart, thoughtful engagement with activities, completion of homework activities, and subsequent improvements in anxiety.
The three cases highlight different ways in which young people choose to engage in self-help ICBT interventions and demonstrate that simple measures of adherence such as number of sessions completed may not accurately capture a young person's engagement with the program or their acquisition of skills. Rather, consideration of how the young person responds to treatment activities, is crucial. Further, these cases point to the importance of regular or earlier assessment (of responses and outcomes) within ICBT to ensure that children and adolescents who struggle to engage or have difficulty in applying strategies can be identified and assisted.
4.2.3. Parent and child report
The cases highlighted here also demonstrate the benefit and challenges of incorporating reports from both the young person and their parent in assessments. There were some occasions where discrepancies between parent and child report were substantial, especially on specific subscales of the SCAS. In all three cases GAD was the primary diagnosis, and it may be that the young person is better able to report on such internalised worries, and that parents are less aware due to the less behavioural nature of the disorder. On the other hand, in all three cases, parents were better able to provide indications of whether key behavioural targets (e.g. sleep, avoidance of fears) had improved after Step 1. For example, Will's mother was able to note that he showed less avoidance in completing homework, that his sleep had improved, and that he was able to complete his final examinations without experiencing anxiety. Thus, consideration of the parents' perspective may allow greater insight into the improvements (or lack thereof) made after Step 1. However, reflection on parental capacity to comment accurately on some (internalising) types of anxiety is also required. Interestingly, despite parent-child agreement at pre-treatment, there was disagreement between the child reported ADIS and parent reported SCAS at post-treatment. Again, this tended to be related to parent reports of specific anxiety types such as GAD and Panic. This may also be a result of the young person's enhanced ability to accurately recognise and understand signs of anxiety, which is a core focus of treatment.
Outcomes from the three mid-point assessments highlight the challenges of determining clear cut-offs or criteria for stepping-up within ICBT interventions. Early identification of non-engagement is important, given the relationship between adherence and positive outcome (March et al., 2018). It is also clear from these cases that decisions regarding the need to step up to therapist-support should be based on a combination of child and parent report of outcomes, as well as an inspection of program responses to estimate engagement with, and understanding of, material.
4.3. The benefits of stepping-up to videoconferencing or email support
For the two cases that were stepped up to receive therapist support, clear benefits and gains were noted during the second treatment step. In both cases, a key feature of therapist support involved the tailoring of strategies to encourage the implementation of techniques into real-life examples. In the case of Edward, the therapist was able to address his previous avoidance of anxiety management strategies (e.g. avoidance of relaxation when anxious in social situations due to fear of anxiety being noticed by peers) and create alternative approaches that were more acceptable to him. For Matthew, videoconferencing support was used to assist him in the application of techniques to anxiety-provoking situations that came up on a weekly basis, and to encourage the rehearsal of key CBT strategies, an area in which he struggled during the self-help sessions. Further, videoconferencing sessions allowed the inclusion and involvement of Matthew's mother at times to assist in the implementation of techniques and to manage difficulties that arose during the week.
Therapist support was also used to assist both Edward and Matthew in refining and applying their exposure hierarchies, breaking down their fears down into smaller realistic and achievable steps, so that exposure practice could be effectively implemented. In the case of Matthew, videoconferencing allowed the therapist to work collaboratively with Matthew and his mother through screen sharing in real-time, to amend the exposure hierarchy and problem solve implementation challenges. Thus, videoconferencing more closely mimicked face-to-face therapy for this key therapeutic technique. Importantly, the fact that neither of these cases experienced substantial change in anxiety until exposure was implemented highlights the importance of moving skill acquisition and rehearsal to earlier stages of treatment as a strategy for improving adherence. Finally, therapist support in both cases was also utilised to provide reinforcement and to enhance motivation following session completion. In the case of Edward, email therapist support was able to successfully reinforce the strategies Edward was applying well but that he had not recognised as treatment successes (e.g. problem solving). In both cases, email and videoconferencing support was also successful in reinforcing the progress made during exposure and problem solving practice to encourage a sense of mastery, as well as to redirect unhelpful cognitions related to progress.
The ways in which therapist support shaped treatment engagement during Step 2 differed between the cases. With one phone call and three email contacts, Edward was able to go on and complete three more sessions during Step 2. Although this adherence was not ideal as he did not finish the program, Edward engaged more with the strategies during these sessions than in the initial self-help sessions, and was able to change his behaviours considerably more during this time. Given that only minimal therapist support was provided to Edward (brief email after each completed session +1 exposure/mid-point call; 45 min in total), these results are encouraging and support a stepped-care model. The positive changes noted by Edward after six sessions, and the decision to stop sessions, are also consistent with the results from the large dissemination study that suggested effects of ICBT may begin to plateau after six sessions. It is possible that a brief 6-session intervention may be a viable treatment option for some young people.
In the case of Matthew, the therapist was able to book in weekly videoconferencing sessions (weekly videoconferencing sessions + exposure call; 137 min in total), and Matthew was able to complete all 10 sessions, as well as two booster (revision) sessions. However, it also demanded greater therapist time compared to email support and self-help. The inclusion of Matthew's mother in some videoconferencing sessions provided additional support and transferral of skills into daily activities. Encouraging parents to simultaneously complete the parent version of the program, or providing parent-focused therapist-support may be another strategy for enhancing effects in young people struggling to engage in the program.
Interestingly, both Matthew and Edward rated the treatment as satisfactory, and both reported benefits associated with their modality of therapist support. The videoconferencing sessions were noted by Matthew as his favourite part of the program, while Edward also reported the phone call as being important and highlighted the non-confronting nature of support via email.
4.4. Strengths and limitations
The present study utilised a case study design that allowed an interpretation of how an ICBT stepped-care program could be implemented clinically in real-world practice. Such case illustrations can inform strategies for the dissemination of evidence-based ICBT interventions. The case study methodology was rigorous, with repeated assessment points, multiple measures for assessing anxiety and associated functioning, and multiple informants. Further, the use of reliable change indices provides statistical rigour to the examination of effects. Nonetheless, there are several limitations. Follow-up data beyond the post-treatment assessment is required to provide an indication of maintenance of change. Further, the lack of a baseline monitoring phase for participants, or inclusion of randomisation in the case study design means that we cannot be sure the observed results are due to the stepped-care ICBT model. The effects noted here need to be confirmed in large randomised controlled trials and compared to the existing evidence-base. Finally, this study did not incorporate the personal choice of the young person in determining whether or not they should be stepped-up to receive therapist assistance, a factor which may be important in promoting program adherence. Future studies should examine the impacts when the family's preferences are incorporated into the mid-point assessment.
5. Conclusions
Stepped-care models of ICBT show promise in the treatment of child and adolescent anxiety. Young people face clear challenges when participating in self-help ICBT programs, yet a proportion are able to show meaningful change after completing such programs on their own. Early assessment of engagement and response conducted within ICBT programs shows potential in identifying young people at-risk of disengagement and non-response, and can facilitate redirection into higher intensity ICBT where therapist support can be employed to assist the young person. The cases presented in this study highlight the complexities involved in determining response mid-treatment, and highlight the positive changes that can occur with the introduction of therapist support at this time.
Funding sources
This work was supported by the Children's Financial Markets Trust (Children's Foundation) Australia [2017-070]; and Australian Rotary Health.
Declaration of competing interest
Authors SM, SS and CD declare that although the intellectual property for BRAVE-ONLINE is owned by UniQuest/the University of Queensland, they may potentially benefit from royalties related to the program.
Acknowledgements
The authors would like to acknowledge the families who participated in this project and gave up their time to complete assessments and the treatment program. We also thank Ms. Arlen Rowe for her assistance in preparing the data for this study.
Contributor Information
Sonja March, Email: Sonja.March@usq.edu.au.
Caroline L. Donovan, Email: c.donovan@griffith.edu.au.
Sarah Baldwin, Email: Sarah.Baldwin@usq.edu.au.
Martelle Ford, Email: Martelle.Ford@usq.edu.au.
Susan H. Spence, Email: s.spence@griffith.edu.au.
References
- Albano A.M., Silverman W.K. Psychological Corporation; San Antonio, TX: 1996. The Anxiety Disorders Interview Schedule for Children for DSM-IV: Clinician Manual (Child and Parent Versions) [Google Scholar]
- Andersson G., Titov N. Advantages and limitations of internet-based interventions for common mental disorders. World Psychiatry. 2014;13:4–11. doi: 10.1002/wps.20083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arendt K., Hougaard E., Thastum M. Psychometric properties of the child and parent versions of SpenceChildren’s Anxiety Scale in a Danish community and clinical sample. Journal of Anxiety Disorders. 2014:947–956. doi: 10.1016/j.janxdis.2014.09.021. [DOI] [PubMed] [Google Scholar]
- Cobham V., March S., De Young A., Leeson F., Nixon R., McDermott B., Kenardy J. Involving parents in indicated early intervention for childhood PTSD following accidental injury. Clin. Child. Fam. Psychol. Rev. 2012;15:345–363. doi: 10.1007/s10567-012-0124-9. [DOI] [PubMed] [Google Scholar]
- Costello J.E., He J., Sampson N., Kessler R., Merikangas K. Services for adolescents with psychiatric disorders: 12-month data from the National Comorbidity Survey–Adolescent. Psychiatric Services. 2014;65:359–366. doi: 10.1176/appi.ps.201100518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donovan C.L., March S., Poole C., Boyes N., Redgate J. Australian mental health worker attitudes towards cCBT: what is the role of knowledge? Are there differences? Can we change them? Internet Interv. 2015;2(4):372–381. [Google Scholar]
- Hill C., Creswell C., Vigerland S., Nauta M.H., March S., Donovan C., Wolters L., Spence S.H., Martin J.L., Wozney L., Mclellan L., Kreuze L., Gould K., Jolstedt M., Nord M., Hudson J.L., Utens E., Ruwaard J., Albers C., Khanna M., Albano A.M., Serlachius E., Hrastinski S., Kendall P.C. Navigating the development and dissemination of internet cognitive behavioral therapy (iCBT) for anxiety disorders in children and young people: a consensus statement with recommendations from the #iCBTLorentz Workshop Group. Internet Interv. 2018;12:1–10. doi: 10.1016/j.invent.2018.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson N.S., Truax P. Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. J. Consult. Clin. Psychol. 1991;59:12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- Jolstedt M., Wahlund T., Lenhard F., Ljótsson B., Mataix-Cols D., Nord M., Öst L.-G., Högström J., Serlachius E., Vigerland S. Efficacy and cost-effectiveness of therapist-guided internet cognitive behavioural therapy for paediatric anxiety disorders: a single-centre, single-blind, randomised controlled trial. The Lancet Child & Adolescent Health. 2018;2:792–801. doi: 10.1016/S2352-4642(18)30275-X. [DOI] [PubMed] [Google Scholar]
- Kazdin A.E. Single-case experimental designs. Evaluating interventions in research and clinical practice. Behav. Res. Ther. 2019;117:3–17. doi: 10.1016/j.brat.2018.11.015. [DOI] [PubMed] [Google Scholar]
- Lawrence D., Johnson S., Hafekost J., Boterhoven De Haan K., Sawyer M., Ainley J., Zubrick S.R. Department of Health; Cabverra: 2015. The Mental Health of Children and Adolescents. Report on the Second Australian Child and Adolescent Survey of Mental Health and Wellbeing. [Google Scholar]
- Lyneham H.J., Sburlati E.S., Abbott M.J., Rapee R.M., Hudson J.L., Tolin D.F., Carlson S.E. Psychometric properties of the Child Anxiety Life Interference Scale (CALIS) Journal of Anxiety Disorders. 2013;27:711–719. doi: 10.1016/j.janxdis.2013.09.008. [DOI] [PubMed] [Google Scholar]
- March S., Spence S.H., Donovan C.L. The efficacy of an internet-based cognitive-behavioral therapy intervention for child anxiety disorders. J. Pediatr. Psychol. 2009;34:474–487. doi: 10.1093/jpepsy/jsn099. [DOI] [PubMed] [Google Scholar]
- March S., Spence S.H., Donovan C.L., Kenardy J.A. Large-scale dissemination of internet-based cognitive behavioral therapy for youth anxiety: feasibility and acceptability study. J. Med. Internet Res. 2018;20:e234. doi: 10.2196/jmir.9211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merry S.N., Stasiak K., Shepherd M., Frampton C., Fleming T., Lucassen M.F. The effectiveness of SPARX, a computerised self help intervention for adolescents seeking help for depression: randomised controlled non-inferiority trial. BMJ. 2012;344:e2598. doi: 10.1136/bmj.e2598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nauta M.H., Scholing A., Rapee R.M., Abbott M., Spence S.H., Waters A. A parent-report measure of children’s anxiety: psychometric properties and comparison with child-report in a clinic and normal sample. Behav. Res. Ther. 2004;42:813–839. doi: 10.1016/S0005-7967(03)00200-6. [DOI] [PubMed] [Google Scholar]
- Pennant M.E., Loucas C.E., Whittington C., Creswell C., Fonagy P., Fuggle P., Kelvin R., Naqvi S., Stockton S., Kendall T. Computerised therapies for anxiety and depression in children and young people: a systematic review and meta-analysis. Behav. Res. Ther. 2015;67:1–18. doi: 10.1016/j.brat.2015.01.009. [DOI] [PubMed] [Google Scholar]
- Podina I.R., Mogoase C., David D., Szentagotai A., Dobrean A. A meta-analysis on the efficacy of technology mediated CBT for anxious children and adolescents. J. Ration. Emot. Cogn. Behav. Ther. 2015;34:31–50. [Google Scholar]
- Polanczyk G.V., Salum G.A., Sugaya L.S., Caye A., Rohde L.A. Annual research review: a meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J. Child Psychol. Psychiatry. 2015;56:345–365. doi: 10.1111/jcpp.12381. [DOI] [PubMed] [Google Scholar]
- Rapee R.M., Wignall A., Hudson J.L., Schniering C.A. New Harbinger Publications; Oakland, CA, US: 2000. Treating Anxious Children and Adolescents: An Evidence-based Approach. [Google Scholar]
- Rapee R.M., Lyneham H.J., Wuthrich V., Chatterton M.L., Hudson J.L., Kangas M., Mihalopoulos C. Comparison of stepped care delivery against a single, empirically validated cognitive-behavioral therapy program for youth with anxiety: a randomized clinical trial. J. Am. Acad. Child Adolesc. Psychiatry. 2017;56:841–848. doi: 10.1016/j.jaac.2017.08.001. [DOI] [PubMed] [Google Scholar]
- Rey J.M., Starling J., Wever C., Dossetor D.R., Plapp J.M. Inter-rater reliability of global assessment of functioning in a clinical setting. J. Child Psychol. Psychiatry. 1995;36:787–792. doi: 10.1111/j.1469-7610.1995.tb01329.x. [DOI] [PubMed] [Google Scholar]
- Salloum A., Scheeringa M.S., Cohen J.A., Storch E.A. Development of stepped care trauma-focused cognitive-behavioral therapy for Young children. Cognitive Behaviour Practice. 2014;21:97–108. doi: 10.1016/j.cbpra.2013.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaffer D., Gould M.S., Brasic J., Ambrosini P., Fisher P., Bird H., Aluwahlia S. A children’s global assessment scale (CGAS) Arch. Gen. Psychiatry. 1983;40:1228–1231. doi: 10.1001/archpsyc.1983.01790100074010. [DOI] [PubMed] [Google Scholar]
- Spence S.H. A measure of anxiety symptoms among children. Behav. Res. Ther. 1998;36:545–566. doi: 10.1016/s0005-7967(98)00034-5. [DOI] [PubMed] [Google Scholar]
- Spence S.H., Barrett P.M., Turner C.M. Psychometric properties of the Spence Children’s Anxiety Scale with young adolescents. Journal of Anxiety Disorders. 2003;17:605–625. doi: 10.1016/s0887-6185(02)00236-0. [DOI] [PubMed] [Google Scholar]
- Spence S.H., Holmes J.M., March S., Lipp O.V. The feasibility and outcome of clinic plus internet delivery of cognitive-behavior therapy for childhood anxiety. J. Consult. Clin. Psychol. 2006;74:614–621. doi: 10.1037/0022-006X.74.3.614. [DOI] [PubMed] [Google Scholar]
- Spence S.H., Donovan C.L., March S., Gamble A., Anderson R.E., Prosser S., Kercher A., Kenardy J. Online CBT in the treatment of child and adolescent anxiety disorders: issues in the development of BRAVE-ONLINE and two case illustrations. Behavioural and Cognitive Psychoterhapy. 2008;36:411–430. [Google Scholar]
- Spence S.H., Donovan C.L., March S., Gamble A., Anderson R.E., Prosser S., Kenardy J. A randomized controlled trial of online versus clinic-based CBT for adolescent anxiety. J. Consult. Clin. Psychol. 2011;79:629–642. doi: 10.1037/a0024512. [DOI] [PubMed] [Google Scholar]
- Spence S.H., Sawyer M.G., Sheffield J., Patton G., Bond L., Graetz B., Kay D. Does the absence of a supportive family environment influence the outcome of a universal intervention for the prevention of depression? Int. J. Environ. Res. Public Health. 2014;11:5113–5132. doi: 10.3390/ijerph110505113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stallard P., Udwin O., Goddard M., Hibbert S. The availability of cognitive behaviour therapy within specialist child and adolescent mental health services (CAMHS): a national survey. Behav. Cogn. Psychother. 2007;35:501–505. [Google Scholar]
- Sweeney G.M., Donovan C.L., March S., Laurenson S.D. Logging into therapy: parent attitudes and intentions to use computer-based therapies for youth mental health. Internet Interv. 2015;2:437–445. [Google Scholar]
- Sweeney G.M., Donovan C.L., March S., Forbes Y. Internet Interventions. 2017. Logging into therapy: adolescent perceptions of computer-based therapies for mental health problems. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolin D.F., Diefenbach G.J., Gilliam C.M. Stepped care versus standard Cognitive-Behavioral Therapy for obsessive-compulsive disorder: a preliminary study of efficacy and costs. Depression & Anxiety. 2011;28:314–323. doi: 10.1002/da.20804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Topooco N., Riper H., Araya R., Berking M., Brunn M., Chevreul K., Cieslak R., Ebert D.D., Etchmendy E., Herrero R., Kleiboer A., Krieger T., García-Palacios A., Cerga-Pashoja A., Smoktunowicz E., Urech A., Vis C., Andersson G. Attitudes towards digital treatment for depression: a European stakeholder survey. Internet Interv. 2017;8:1–9. doi: 10.1016/j.invent.2017.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Treffers P.D.A., Silverman W.K. Anxiety and its disorders in children and adolescents before the twentieth century. In: Treffers P.D.A., Silverman W.K., editors. Anxiety Disorders in Children and Adolescents: Research, Assessment and Intervention. Cambridge University Press; Cambridge: 2000. [Google Scholar]
- Van Der Leeden A.J.M., Van Der Leeden R., Liber J.M., Utens E.M.W.J., Treffers P.D.A. Stepped care cognitive behavioural therapy for children with anxiety disorders: a new treatment approach. Behav. Cogn. Psychother. 2011;39:55–75. doi: 10.1017/S1352465810000500. [DOI] [PubMed] [Google Scholar]
- Van Straten A., Hill J., Richards D.A., Cuijpers P. Stepped care treatment delivery for depression: a systematic review and meta-analysis. Psychol. Med. 2015;45:231–246. doi: 10.1017/S0033291714000701. [DOI] [PubMed] [Google Scholar]
- Vigerland S., Serlachius E., Thulin U., Andersson G., Larsson J., Ljótsson B. Long-term outcomes and predictors of internet-delivered cognitive behavioral therapy for childhood anxiety disorders. Behaviour Research & Therapy. 2017;90:67–75. doi: 10.1016/j.brat.2016.12.008. [DOI] [PubMed] [Google Scholar]
- Warwick H., Reardon T., Cooper P., Murayama K., Reynolds S., Wilson C., Creswell C. Complete recovery from anxiety disorders following Cognitive Behavior Therapy in children and adolescents: a meta-analysis. Clin. Psychol. Rev. 2017;52:77–91. doi: 10.1016/j.cpr.2016.12.002. [DOI] [PubMed] [Google Scholar]
- Wozney L., Mcgrath P.J., Gehring N.D., Bennett K., Huguet A., Hartling L., Dyson M.P., Soleimani A., Newton A.S. eMental healthcare technologies for anxiety and depression in childhood and adolescence: systematic review of studies reporting implementation outcomes. JMIR Ment. Health. 2018;5:e48. doi: 10.2196/mental.9655. [DOI] [PMC free article] [PubMed] [Google Scholar]