Abstract
Medial epicondylitis, also known as “golfer's elbow,” is a common orthopaedic condition that typically results from overuse of the flexor pronator mass. Repetitive eccentric loading of the muscles responsible for wrist flexion and forearm pronation leads to microtrauma and subsequent degeneration of the flexor pronator tendon. Patients with medial epicondylitis typically present in the fourth to sixth decade of life and have an insidious onset of medial elbow pain. Occasionally, medial epicondylitis may result from an acute traumatic event, such as an acute avulsion of the common flexor tendon. Patients should be examined for concomitant elbow pathologies, including ulnar neuritis and ulnar collateral ligament injury. T2-weighted magnetic resonance imaging can show increased signal intensity in the common flexor tendon or a complete rupture. Nonsurgical management is the mainstay of treatment; however, surgical treatment may be indicated in elite athletes and patients with persistent symptoms after conservative treatment. This technique article with accompanying video describes open debridement and repair of the flexor pronator tendon, with an emphasis on restoration of the anatomic footprint and compression across the repair site to promote biological healing.
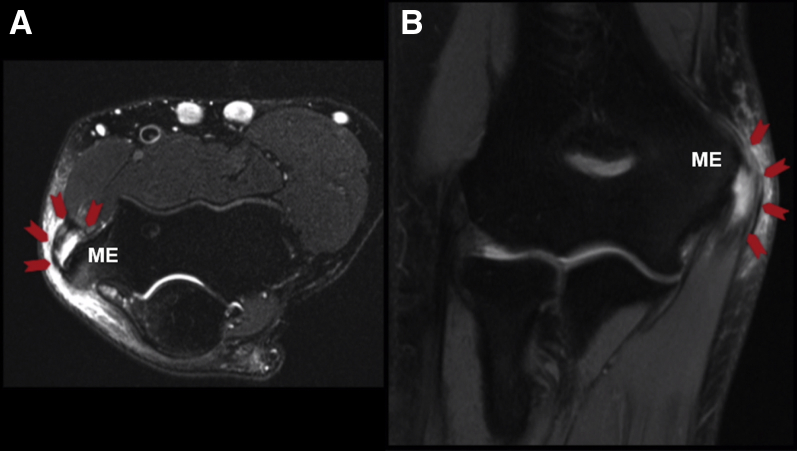
Medial epicondylitis, also commonly referred to as “golfer's elbow,” is typically seen in patients in the fourth to sixth decade of life. The condition equally affects men and women and occurs more commonly in certain occupational settings, and recent reports have shown an increasing incidence in the general population.1, 2, 3, 4 The common flexor tendon is the convergence of 5 muscles: pronator teres, flexor carpi radialis, palmaris longus, flexor digitorum superficialis, and flexor carpi ulnaris.4 This common tendon is about 2.5 cm in length, attaches to the humeral medial epicondyle just proximal to the anterior bundle of the ulnar collateral ligament (UCL), and provides dynamic stability to the elbow.5, 6, 7 Patients with medial epicondylitis typically present with pain over the medial epicondyle radiating down the proximal medial forearm. In overhead athletes or certain manual laborers, this pain is exacerbated by the sport or occupation. Repetitive stress on the elbow especially with activities involving wrist flexion, forearm pronation, or valgus stress results in microtrauma and degeneration. Overhead-throwing athletes who are eccentrically loading the common flexor tendon by such a mechanism can also present with acute avulsion or rupture of the common flexor tendon. However, most cases are degenerative, characterized by a gradual onset. Physical examination will reveal tenderness at the medial epicondyle and pain or weakness with resisted wrist flexion, forearm pronation, or a forceful grip. Other pathologies common to this area should also be elicited on examination because concomitant injuries could be present, including ulnar neuritis and UCL injuries, particularly in the overhead-throwing athlete. Noncontrast magnetic resonance imaging (MRI) remains the gold standard for imaging of medial epicondylitis. T2-weighted sequences will show high-intensity signal at the common flexor tendon significant for edema and tendinitis or frank rupture. The MRI scan of the patient in this case example shows significant tendinitis with rupture (Fig 1). The integrity of the UCL can also be assessed with MRI.
Fig 1.
Axial (A) and coronal (B) T2-weighted magnetic resonance images of the right elbow showing edema and disruption of the common flexor tendon at the level of the medial epicondyle (ME) as indicated by the arrows.
Most cases of medial epicondylitis are treated successfully with conservative management including nonsteroidal anti-inflammatory drugs and physical therapy. Night-time splinting or orthoses can also be used especially in patients with concomitant ulnar neuritis symptoms. Other nonsurgical management options include extracorporeal shockwave therapy and corticosteroid injections, with several case series showing successful treatment with these modalities.8, 9 Surgical management is considered for patients with persistent symptoms after several months of conservative therapy or for young athletes with evidence of acute tendon avulsion.10 The purpose of this article is provide a detailed technique for surgical debridement and anatomic repair of the common flexor tendon for medial epicondylitis or flexor pronator mass avulsion using transosseous suture fixation.
Surgical Technique
Patient Positioning
After anesthesia is administered, the patient is positioned supine with the operative extremity on a hand table. A nonsterile tourniquet is placed on the proximal arm, and the extremity is prepared and draped in standard sterile fashion (Video 1).
Exposure
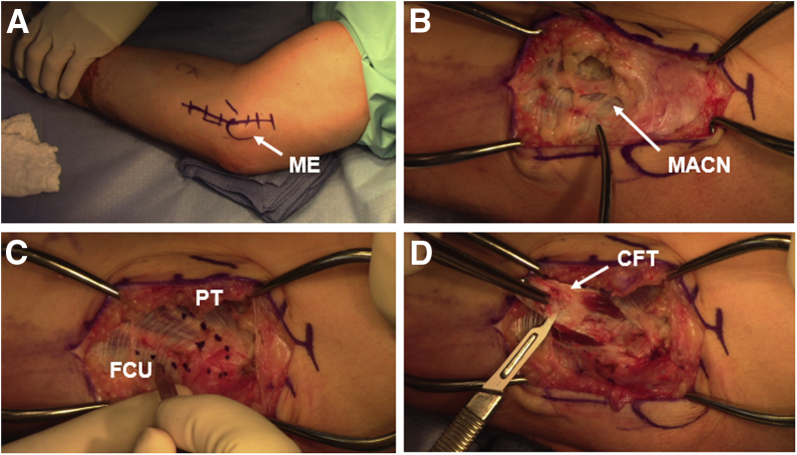
The medial epicondyle and the proposed skin incision centered just anterior to the medial epicondyle are outlined (Fig 2A). After limb exsanguination with an Esmarch bandage, a 4- to 6-cm curvilinear incision is made centered over the medial epicondyle. Dissection is carried down the subcutaneous tissue with particular attention to identify the medial antebrachial cutaneous nerve branches, which are mobilized and protected (Fig 2B). Next, the common flexor tendon is outlined between the flexor carpi ulnaris and the pronator teres (Fig 2C). The tendon is incised along this U-shaped incision and elevated from its origin onto the medial epicondyle while avoiding injury to the UCL. The common flexor tendon is reflected, revealing the degenerative tissue and tendinosis (Fig 2D). The tendinotic tissue is sharply excised.
Fig 2.
The patient is positioned supine with the right upper extremity on a hand table. (A) The medial epicondyle (ME) is outlined, as well as the proposed incision, which is just anterior to the ME. (B) The medial antebrachial cutaneous nerve (MACN) is identified and protected during subcutaneous dissection. (C) The fascial incision for the common flexor tendon is outlined between the pronator teres (PT) and flexor carpi ulnaris (FCU). (D) The degenerative tissue just deep to the tendon is sharply excised. (CFT, common flexor tendon.)
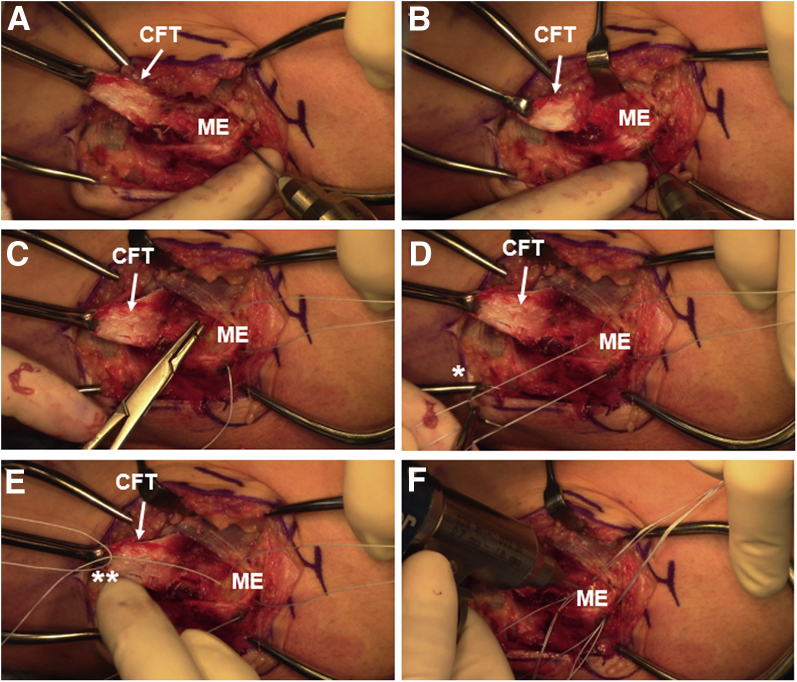
Bony Preparation and Tendon Repair
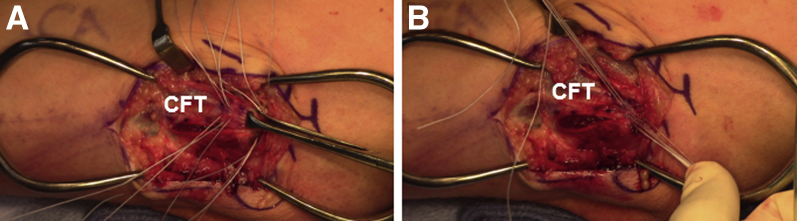
Once the tendon is elevated, the medial epicondyle is abraded with a curette to prepare for healing of the tissue to the bone. Two bone tunnels are then made with a 0.045-mm Kirschner wire (K-wire) while care is taken to protect and avoid the ulnar nerve (Fig 3 A and B). The bone tunnels are created with a 5-mm bone bridge, with 1 tunnel more superior and another more posterior in the orientation of the common flexor tendon. A No. 0 nonabsorbable suture (Arthrex FiberWire suture in this case) is passed from posterior to anterior through each bone tunnel (Fig 3C). A separate suture is then sewn through the substance of each suture limb that was passed through the bone tunnels (Fig 3D). This effectively creates 3 suture limbs available to be shuttled for each both tunnel (Fig 3E), yielding a total of 6 suture limbs available for the repair. Small perforations are then made in the bone with a K-wire to create a vascular bed for tendon healing (Fig 3F). All 6 sutures are passed in simple fashion through the common flexor tendon to repair and compress it to its footprint (Fig 4A). The 3 suture limbs from the posterior tunnel are passed more posteriorly and the 3 suture limbs from the anterior tunnel are passed more anteriorly through the tunnel. Once all the sutures are passed, the sutures from each limb are tied to themselves and then to the adjacent suture limbs to create a crossing pattern to compress the tendon down to bone (Fig 4B).
Fig 3.
In a right elbow, 2 bone tunnels are created through the medial epicondyle (ME) with a 0.045-mm Kirschner wire, 1 more posteriorly (A) and the other more anteriorly (B). (C) A No. 0 nonabsorbable suture is passed from posterior to anterior through each bone tunnel. A new No. 0 nonabsorbable suture (asterisk) is sewn through the substance of each suture that was passed through the bone tunnel (D), therefore creating 3 suture strands (asterisks) arising from each bone tunnel (E). (F) Small perforations in the ME are made with a Kirschner wire to prepare the footprint for healing. (CFT, common flexor tendon.)
Fig 4.
A right elbow is shown. (A) The 3 posterior limbs are passed posteriorly in the tendon and the other 3 limbs are passed anteriorly in simple fashion to restore the tendon to its footprint. (B) The limb strands are first tied to themselves and then to the adjacent limbs in a crisscrossing pattern to compress the tendon into the medial epicondyle. (CFT, common flexor tendon.)
Closure and Immobilization
The fascial incision is closed with absorbable suture (No. 3-0 Vicryl suture [Ethicon] in this case) in simple fashion. The dermal layer is closed with absorbable suture (No. 3-0 Vicryl) in buried simple fashion, followed by a running subcuticular layer for the skin (No. 4-0 Monocryl; Ethicon). The patient is immobilized in a posterior plaster splint at 70° of flexion for 10 days.
Postoperative Rehabilitation
The patient is initially placed in a posterior plaster splint postoperatively that is removed at the first postoperative visit in 10 to 14 days; the patient is then transitioned to a hinged elbow brace that allows for range of motion as tolerated. Strengthening exercises are started at 6 to 8 weeks postoperatively, with no restrictions at 3 to 4 months.
Discussion
The prevalence of medial epicondylitis or a common flexor tendon injury is less than 1%, but cases can be found with higher frequency in particular athletes and individuals in certain occupational settings.1, 2, 4 Most cases are successfully treated with conservative measures including activity modification, physical therapy, oral analgesics, or various injections. Surgical intervention is considered for recalcitrant symptoms despite conservative management or for elite athletes with evidence of tendon disruption on imaging or acute avulsion of the common flexor tendon.11
The described surgical techniques usually consist of open debridement of the common tendon, with or without microfracture of the medial epicondyle, and either side-to-side tendon repair or reattachment of the common tendon to the medial epicondyle.10 Vangsness and Jobe12 retrospectively reviewed surgical cases of medial epicondylitis and found good to excellent outcomes in 34 of 35 elbows treated with open debridement and repair. Recent techniques have included debridement of the common flexor tendon and repair to the medial epicondyle using suture anchors with satisfactory pain relief and patient-reported outcome measures.11, 13 Another described technique involved a mini-open muscle resection of the common flexor mass and microfracture of the medial epicondyle without reattachment of the tendon, followed by closure of the fascia, therefore creating an enclosed hematoma for healing.14 This technique, however, involved a very small incision, which does not allow identification of the ulnar nerve in cases in which it needs to be decompressed or transposed. In addition, Kwon et al.15 reported on a fascial elevation and tendon origin resection technique, with 18 of 20 patients in their cohort reporting satisfaction with surgical outcomes.
We prefer our technique of debridement followed by anatomic repair using transosseous sutures and compression back to the footprint (Table 1). Pearls and pitfalls of our procedure are outlined in Table 2. This open technique, as described in this article, allows the surgeon to identify and protect the ulnar nerve, as well as perform concomitant procedures when necessary, specifically when addressing ulnar neuritis or UCL injuries. Our technique also describes a method of suture shuttling through bone tunnels with 3 suture limbs through each tunnel and sequential tying of the limbs to each other to provide robust fixation and compression of the tendon to the medial epicondyle.
Table 1.
Advantages and Disadvantages of Elbow Common Flexor Tendon Repair
| Advantages |
| The common flexor tendon is repaired to its origin; this allows tendon restoration and has been observed to offer clinical improvement in pronation strength.11 |
| Tendon release procedures alone may subsequently make the elbow vulnerable to valgus instability compared with debridement and repair. |
| The need for and potential complications with suture anchor implants are avoided because no special implants are required for this procedure. |
| The open technique allows for safe identification and protection of the ulnar nerve and allows for concomitant procedures such as ulnar nerve transposition. |
| Disadvantages |
| Transosseous sutures have the potential to cause ulnar nerve irritation compared with suture anchor fixation, given the location of the sutures. |
| Limited literature exists comparing repair and fixation techniques for elbow common flexor tendons. |
Table 2.
Surgical Pearls and Potential Pitfalls of Elbow Common Flexor Tendon Repair
| Pearls |
| If an ulnar nerve transposition is anticipated, consider making a slightly more posterior incision so that it lies more posterior to the final destination of the anteriorly transposed ulnar nerve. |
| Ensure most of the degenerative or tendinotic tissue is excised and debrided to promote the healthier tissue to heal to the medial epicondyle. |
| Pitfalls |
| Avoid injury to the ulnar collateral ligament, which is just deep to the common flexor mass, when elevating and debriding the degenerative tissue from the medial epicondyle. |
| Beware of the ulnar nerve posterior to the medial epicondyle when drilling bone tunnels in the medial epicondyle; identify and protect the ulnar nerve during drilling. |
Footnotes
The authors report the following potential conflicts of interest or sources of funding: C.A. receives grant support and personal fees from Arthrex; grant support from Major League Baseball and Stryker; and personal fees from At Peak and Lead Player. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Step-by-step demonstration of common flexor tendon repair in right elbow. The patient is positioned supine with the operative extremity prepared and draped on a hand table over a nonsterile tourniquet. After limb exsanguination with a bandage, a 6-cm curved incision is made centered just anterior to the medial epicondyle. Dissection is completed through the subcutaneous tissues with particular attention to identify and preserve the medial antebrachial cutaneous nerve. Once at the level of the fascia, a U-shaped incision is made between the flexor carpi ulnaris and the pronator teres, and the common flexor tendon is elevated off of the medial epicondyle. Care is taken to avoid injury to the deeper ulnar collateral ligament. The tendon is reflected, and the degenerative tissue is excised. After the medial epicondyle is exposed, curettes are used to abrade the bone to prepare it for healing. By use of a 0.045-mm Kirschner wire (K-wire), 2 bone tunnels are created in the epicondyle with a 5-mm bone bridge between them along the orientation of the common flexor tendon. A heavy nonabsorbable suture is passed through each bone tunnel. A separate suture is then sewn through the substance of each suture limb that was passed through the bone tunnels. This creates 3 suture limbs available for each bone tunnel, therefore creating 6 limbs total for the repair. Small perforations are then made in the bone with a K-wire to create a vascular bed for tendon healing. All 6 sutures are passed in simple fashion through the common flexor tendon to repair and compress it to its footprint. Once all the sutures are passed, the sutures from each limb are tied to themselves and then to the adjacent suture limbs to create a crossing pattern to provide a compression effect. The fascial incision is closed with absorbable suture in interrupted fashion. The dermal layer is closed with interrupted buried absorbable suture, and the skin is closed with a running subcuticular suture.
References
- 1.Descatha A., Leclerc A., Chastang J.F., Roquelaure Y., Study Group on Repetitive Work Medial epicondylitis in occupational settings: Prevalence, incidence and associated risk factors. J Occup Environ Med. 2003;45:993–1001. doi: 10.1097/01.jom.0000085888.37273.d9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ritz B.R. Humeral epicondylitis among gas- and waterworks employees. Scand J Work Environ Health. 1995;21:478–486. doi: 10.5271/sjweh.64. [DOI] [PubMed] [Google Scholar]
- 3.Wiggins A.J., Cancienne J.M., Camp C.L. Disease burden of medial epicondylitis in the USA is increasing: An analysis of 19,856 patients from 2007 to 2014. HSS J. 2018;14:233–237. doi: 10.1007/s11420-018-9617-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Amin N.H., Kumar N.S., Schickendantz M.S. Medial epicondylitis: Evaluation and management. J Am Acad Orthop Surg. 2015;23:348–355. doi: 10.5435/JAAOS-D-14-00145. [DOI] [PubMed] [Google Scholar]
- 5.Otoshi K., Kikuchi S., Shishido H., Konno S. The proximal origins of the flexor-pronator muscles and their role in the dynamic stabilization of the elbow joint: An anatomical study. Surg Radiol Anat. 2014;36:289–294. doi: 10.1007/s00276-013-1168-3. [DOI] [PubMed] [Google Scholar]
- 6.Park M.C., Ahmad C.S. Dynamic contributions of the flexor-pronator mass to elbow valgus stability. J Bone Joint Surg Am. 2004;86:2268–2274. doi: 10.2106/00004623-200410000-00020. [DOI] [PubMed] [Google Scholar]
- 7.Lin F., Kohli N., Perlmutter S., Lim D., Nuber G.W., Makhsous M. Muscle contribution to elbow joint valgus stability. J Shoulder Elbow Surg. 2007;16:795–802. doi: 10.1016/j.jse.2007.03.024. [DOI] [PubMed] [Google Scholar]
- 8.Lee S.S., Kang S., Park N.K. Effectiveness of initial extracorporeal shock wave therapy on the newly diagnosed lateral or medial epicondylitis. Ann Rehabil Med. 2012;36:681–687. doi: 10.5535/arm.2012.36.5.681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stahl S., Kaufman T. The efficacy of an injection of steroids for medial epicondylitis. A prospective study of sixty elbows. J Bone Joint Surg Am. 1997;79:1648–1652. doi: 10.2106/00004623-199711000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Ciccotti M.G., Ramani M.N. Medial epicondylitis. Tech Hand Up Extrem Surg. 2003;7:190–196. doi: 10.1097/00130911-200312000-00010. [DOI] [PubMed] [Google Scholar]
- 11.Vinod A.V., Ross G. An effective approach to diagnosis and surgical repair of refractory medial epicondylitis. J Shoulder Elbow Surg. 2015;24:1172–1177. doi: 10.1016/j.jse.2015.03.017. [DOI] [PubMed] [Google Scholar]
- 12.Vangsness C.T., Jr., Jobe F.W. Surgical treatment of medial epicondylitis. Results in 35 elbows. J Bone Joint Surg Br. 1991;73:409–411. doi: 10.1302/0301-620X.73B3.1670439. [DOI] [PubMed] [Google Scholar]
- 13.Grawe B.M., Fabricant P.D., Chin C.S. Clinical outcomes after suture anchor repair of recalcitrant medial epicondylitis. Orthopedics. 2016;39:e104–e107. doi: 10.3928/01477447-20151222-09. [DOI] [PubMed] [Google Scholar]
- 14.Cho B.K., Kim Y.M., Kim D.S. Mini-open muscle resection procedure under local anesthesia for lateral and medial epicondylitis. Clin Orthop Surg. 2009;1:123–127. doi: 10.4055/cios.2009.1.3.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kwon B.C., Kwon Y.S., Bae K.J. The fascial elevation and tendon origin resection technique for the treatment of chronic recalcitrant medial epicondylitis. Am J Sports Med. 2014;42:1731–1737. doi: 10.1177/0363546514530664. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Step-by-step demonstration of common flexor tendon repair in right elbow. The patient is positioned supine with the operative extremity prepared and draped on a hand table over a nonsterile tourniquet. After limb exsanguination with a bandage, a 6-cm curved incision is made centered just anterior to the medial epicondyle. Dissection is completed through the subcutaneous tissues with particular attention to identify and preserve the medial antebrachial cutaneous nerve. Once at the level of the fascia, a U-shaped incision is made between the flexor carpi ulnaris and the pronator teres, and the common flexor tendon is elevated off of the medial epicondyle. Care is taken to avoid injury to the deeper ulnar collateral ligament. The tendon is reflected, and the degenerative tissue is excised. After the medial epicondyle is exposed, curettes are used to abrade the bone to prepare it for healing. By use of a 0.045-mm Kirschner wire (K-wire), 2 bone tunnels are created in the epicondyle with a 5-mm bone bridge between them along the orientation of the common flexor tendon. A heavy nonabsorbable suture is passed through each bone tunnel. A separate suture is then sewn through the substance of each suture limb that was passed through the bone tunnels. This creates 3 suture limbs available for each bone tunnel, therefore creating 6 limbs total for the repair. Small perforations are then made in the bone with a K-wire to create a vascular bed for tendon healing. All 6 sutures are passed in simple fashion through the common flexor tendon to repair and compress it to its footprint. Once all the sutures are passed, the sutures from each limb are tied to themselves and then to the adjacent suture limbs to create a crossing pattern to provide a compression effect. The fascial incision is closed with absorbable suture in interrupted fashion. The dermal layer is closed with interrupted buried absorbable suture, and the skin is closed with a running subcuticular suture.