Abstract
Introduction:
The management of multiple sclerosis (MS) has become more complicated after the introduction of new diagnostic and treatment options. Despite the abundance of guidelines, the experience of physicians still plays a major role in the management of patients. This study aimed to define differences in behavior patterns between general neurologists (GNs) and MS specialists (MSSs).
Methods:
We conducted a survey of 36 questions to 318 neurologists, including 33 MSSs. The survey covered topics including laboratory investigations, pregnancy, and treatment.
Results:
Our study found many differences between GNs and MSSs in terms of management, the most important being treatment initiation and switching. GNs had a tendency to initiate treatment later than MSSs however, they tended to switch treatment faster. Our study also showed that GNs ordered magnetic resonance imaging (MRI) more frequently than MSSs, even if patients were clinically stable. Moreover, although GNs more frequently relied on MRI, they did not consider brain atrophy as an important measure in the follow-up of their patients. Furthermore, GNs considered replacement therapy less often than MSSs, even in patients with vitamin D deficiency.
Discussion:
Our study revealed important discrepancies between the management patterns of GNs and MSSs in MS patients. These findings suggest the need for a national education program for GNs on MSSs.
Keywords: Multiple sclerosis, general neurologists, multiple sclerosis specialists, management differences
INTRODUCTION
More progress has been made in the past decade in multiple sclerosis (MS) than in most of the other neurologic disorders. The management of the disease is growing in complexity by the year, particularly due to the number of new therapies growing in breathtaking speed. Further complicated by individual differences of patients, this situation is making decision making more and more challenging for clinicians.
The complexity of processes is also leading to potential differences of approaches by clinicians (1). In certain cases, clinicians may be even compelled to make their decision based on experience, rather than evidence-based medicine due to inadequacy of the scientific evidence available. The situation has made decision-making particularly challenging for neurologists who lack sufficient experience in MS.
The experience of the clinician is a key factor in the diagnosis and treatment of MS. However, the number of studies seeking to estimate the required degree of such experience is inadequate. In one such study, surveying German neurologists on pregnancy among MS patients, only 54% of the responding general neurologists (GNs) could accurately answer the questions (2). Borisow et al. noted that the rate of accuracy was higher among neurologists who saw more than 400 MS patients per year (2). In Turkey, it can be estimated that only those neurologists who work at an MS clinic could see that number of patients.
In this study we aimed at revealing the experience levels of neurologists in Turkey and the differences in how they approach their patients with MS using a questionnaire consisting of 36 questions. The questionnaire consisted a variety of topics, ranging from preferred diagnostic tests used by physicians, factors affecting pregnancy decisions, the criteria for starting disease-modifying therapies (DMTs), and how neurologists use laboratory test results. The method aimed to disclose the differences, if any, between general neurologists (NGs) and neurologists experienced in MS (NEMS), in their approaches to treating MS patients.
METHOD
For our study, 285 GNs and 33 NEMS, for a total of 318 physicians, across 22 provinces were asked to answer a questionnaire specifically developed for this study. The study complied with the requirements of the Declaration of Helsinki, and was conducted after receiving signed informed consent of the respondents. The NEMS were selected among neurologists who are members of the MS Study Group of Turkey, and who treat and follow-up more than 100 MS patients in a year. The questionnaire comprised 36 questions, inquiring neurologists on factors that have a bearing on their diagnosis and treatment of MS, including pregnancy, use of vitamin D therapy and presence of cerebral atrophy. For example, the questions, “In your clinical practice, do you believe that vitamin D affects the course of MS?” “In your opinion, which of the following statements is more accurate as regards the relationship between MS and vitamin D levels?” and “Would you start an MS patient on vitamin D therapy if you find their vitamin D levels to be low?” questions 16, 17 and 18, respectively, were aimed at exploring the physicians’ approaches to vitamin D use, whereas the questions “In your opinion, is cerebral atrophy a measurable parameter?” and “In your clinical practice, is cerebral atrophy a decisive parameter in your selection of a therapy?” questions 28 and 29, respectively, sought to reveal whether cerebral atrophy affected their choice of treatment.
Statistical Analysis
An online software, Qualrate® (GfK; Istanbul, Turkey), was used for collecting the study data. The software enabled the data entered by the physicians to be captured in real-time into the database, allowing viewing of graphical depictions of data in real-time, by use of a macro script. Statistical Package for the Social Sciences, version 21.0 (IBM Corp.; Armonk, NY, USA) was used for statistical analysis of the data collected. Chi-square testing was used for categorical comparison of data. Student’s t test was used for comparison of numerical data and parametric analyses, and Mann-Whitney U test for analysis of non-parametric data. A p-value of 0.05 or lower on the two-tailed independent t-test was considered statistically significant.
RESULTS
Differences in Approaches to Pregnancy in Patients with Multiple Sclerosis
In both groups, the key factors prior to the pregnancy decision were the course of disease and disability (GNs: 45%, NEMS: 85%; p<0.01). It was also notable, although not statistically significant, that the number of children was a more important consideration for GNs than for NEMS, in the decision to conceive (31.2% vs 18.1%, respectively; p>0.05) (Table 1).
Table 1.
The responses received to the question “What would be your approach, if your patient was planning to conceive?”
| General neurologists (n: 285) % | Neurologists experienced in multiple sclerosis (n: 33) % | p* | |
|---|---|---|---|
| Supports it depending on the degree of progression and disability | 46 | 85 | <0.01 |
| Supports it in only those patients who have no children | 31 | 18 | NS |
| Supports it in those patients with 1 child | 15 | 18 | NS |
| Supports it in those patients 2 or more children | 12 | 6 | NS |
| Does not support conception | 1 | - | - |
Chi-square test; NS: non-significant
Differences in Approaches to Cerebrospinal Fluid Examination and Vitamin D Levels
When asked “Do you request CSF examination for assessing the MS risk in patients with clinically isolated syndrome?” 72.1% of GNs responded in saying “Yes,” compared to 75.0% of NEMS. This result showed that the percentages of those having a preference for requesting CSF examination were similar between GNs and NEMS, with almost three fourths of all neurologists requesting CSF analysis (p<0.05).
Less than 50% of all neurologists believed there was a relationship between vitamin D levels and MS prognosis, with 42.4% of NEMS and as high as 48.8% of GNs answering in “Yes” to the question “In your clinical practice, do you believe that vitamin D affects the course of MS?”. However, 27.0% of GNs did not start the patient on vitamin D replacement therapy even when the vitamin D levels were low (Table 2), whereas only 6.0% of NEMS did not prescribe a therapy in the same situation; the difference was statistically significant (p<0.001).
Table 2.
The answers given by general neurologists to the question “Would you start an MS patient on vitamin D therapy if you find their vitamin D levels to be low?”
| General neurologists % | Neurologists experienced in multiple sclerosis % | p* | |
|---|---|---|---|
| Yes | 49 | 42 | NS |
| Occasionally | 24 | 52 | <0.01 |
| No | 27 | 6 | <0.01 |
Chi-square test; NS: non-significant
Differences in Radiological Examinations
There were significant differences in the answers given by GNs and NEMS to the question “What is the frequency of your follow-up MRIs in MS patients with a stable clinical picture?” 4.6% of GNs, and none of the NEMS, performed follow-up by magnetic resonance imaging (MRI) once every three months. Additionally, 34.7% of GNs, and only 9.1% of NEMS requested follow-up once every six months. The percentages of GNs and NEMS requesting MRI follow-up once a year were 48.4% and 12.3%; and once every two years 78.8% and 12.1%, respectively (Figure 1). In conclusion, GNs followed up their patients by MRI more frequently compared to NEMS (chi-square test; p<0.05).
Figure 1.
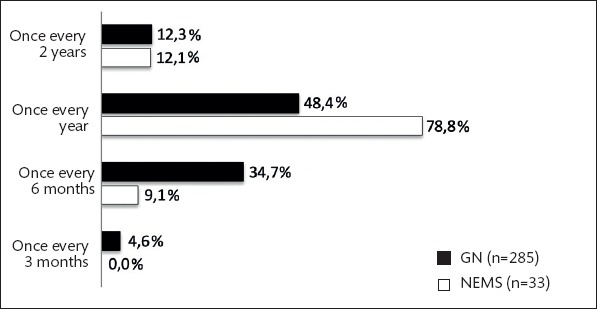
The answers given by GNs and NEMS to the question “What is the frequency of your follow-up MRIs in MS patients with a stable clinical picture?” (%) (p<0.05, Chi-square test)
Moreover, access to MRI was fairly effortless for NEMS, whereas GNs had access problems; 2.5% of GNs stated no MRI devices were available in the region where they worked, and 13.0% confirmed they could occasionally access an MRI device. All of the NEMS had an access to an MRI device, and only 3% stated they had occasional access (p<0.05).
Our survey also sought to explore the clinicians’ attitudes to MRI reports (Figure 2). Accordingly, NEMS had a greater preference compared to GNs for interpreting the radiologists’ reports themselves (p<0.05). In response to the question “Which of the following statement(s) best describe(s) your behavior with respect to a magnetic resonance imaging report you had asked for?” 91.6% of GNs answered “I would consider the radiology report, but definitely make my own assessment,” whereas 2.1% confirmed they would “completely trust the radiology report.” The percentage of GNs, answering the question in saying “I would disregard the radiology report, and make my own assessment” was 9.1%, compared to 21.2% for NEMS. Additionally, NEMS followed up their patients who had radiological activity more frequently (94.2% vs 80.3%; chi-square; p<0.05) (Table 3).
Figure 2.
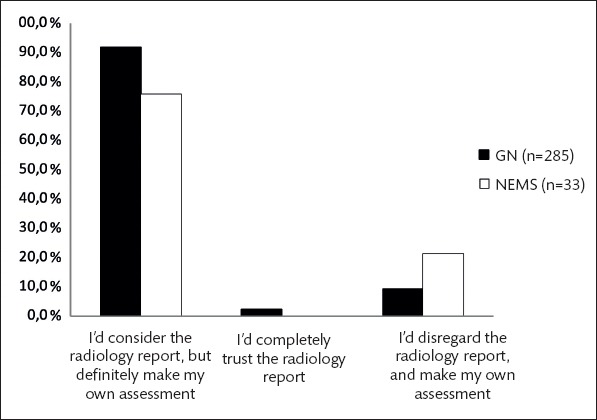
The answers given by GNs and NEMS to the question “Which of the following statement(s) best describe(s) your behavior with respect to a magnetic resonance imaging report you had asked for?” (p<0.05, Chi-square test)
Table 3.
Treatment approach to clinically stable patients who have a new lesion detected on magnetic resonance imaging
| General neurologists % | Neurologists experienced in multiple sclerosis % | p* | |
|---|---|---|---|
| Follows up patient more frequently and in shorter intervals* | 80 | 94 | <0.01 |
| Continues with the current therapy | 27 | 21 | NS |
| Modifies therapy | 12 | 12 | NS |
Chi-square test; NS: non-significant
For determining disability progression, monitoring cerebral atrophy (49.4%) and detecting black holes in MRI (42.1%) were the most important findings for NEMS, compared to 12.2% and 14.3% for GNs, respectively (p<0.01) (Table 4).
Table 4.
Important parameters for disability progression in MS
| General neurologists % | Neurologists experienced in multiple sclerosis % | p* | |
|---|---|---|---|
| Frequency of attacks and MRI activity | 69 | 73 | NS |
| Frequency of attacks | 17 | 9 | NS |
| Presence of cerebral atrophy | 14 | 42 | <0.01 |
| Presence of black holes on MRI | 12 | 49 | <0.01 |
| Presence of activity on MRI | 4 | 9 | NS |
Chi-square test; MRI: magnetic resonance imaging; NS: non-significant
Differences in Treatment
The top challenge for NEMS in following up their patients with MS was deciding on switching treatments of clinically active patients. The second most challenging issues were selecting a treatment at disease onset with diagnostic difficulties. Nearly a half of all respondents believed that efficacy was the most important factor for deciding on a long-term treatment. Interestingly, even when they made a diagnosis based on the McDonald criteria, 27.2% of GNs did not start the patient on a disease-modifying therapy (DMT) but waited for the next attack for starting treatment. In their routine clinical practice, 25% of GNs and 27% of NEMS considered cerebral atrophy on MRI as a factor for choosing a treatment (p>0.05).
Besides, 14.3% of the physicians started patients with radiologically isolated syndrome (RIS) on a DMT. Although not statistically significant, GNs were more inclined toward treating patients with RIS (15.1% vs 6.0%; p=0.17). While both GNs and those who are experienced in MS considered the same factors for the decision to switch treatments, GNs, notably, acted more quickly in the event of no response to treatment (p=0.02). Overall, 31.2% of the neurologists switched treatments only because their patients asked for it, and 12.0% when they detected a lesion on MRI.
Similarities Between the Two Groups
There were no differences between GNs and NEMS in terms of access to MRI (93% vs 95%), the rate of requesting CSF examination in patients with clinically isolated syndrome (72% vs 76%), the circumstances for requesting CSF test and evoked potential tests, the distribution of criteria considered for treatment selection, considering cerebral atrophy to be a non-measurable parameter, timing of the second visit for newly-diagnosed patients, the distribution of factors considered for switching treatments, and the rate of switching treatments solely on the patient’s request (33% vs 21%).
DISCUSSION
Many international surveys are available which assess physicians’ approaches to treating MS patients (3,4,5). However, very few of those surveys were designed to question the differences due to physicians’ varying levels of experience. In this respect, our study was the first study in Turkey to compare the behavior of general neurologists with that of neurologists specialized in any disease.
A comparison of the physicians’ attitudes toward radiological examination results showed that GNs used MRI more frequently than NEMS for diagnosis and treatment. The fact that MRI is frequently requested even for clinically stable patients suggests that too much is spent on radiological examination for the follow-up MS patients in Turkey. In fact, according to OECD data, 119 examinations per 1000 patients were performed in 2013, putting Turkey at the top of the list in terms of requesting MRI examinations (6). It is also a remarkable paradox that GNs request MRI more frequently, although they have less access to these devices.
Our study has also found that GNs regarded radiologist reports more than NEMS. The main reason for this behavior could be the inclination of specialized physicians to interpret laboratory examination results themselves, or the fact that GNs in Turkey spend less time per patient compared to NEMS. In that case, it can be concluded that flawed MRI reports by radiologists who have not been specifically trained in neuroradiology could lead to misdiagnosis.
Based on other findings of our survey, we had the impression that GNs did not follow up patients with radiological activity in sufficient frequency. Moreover, GNs did not regard radiological parameters, such as black holes and cerebral atrophy, as important considerations in patients with clinical progression. These finding suggest that GNs did not attribute sufficient value to the radiological findings in MS patients.
The data collected by the study on treatment were also interesting: overall, the top challenges for neurologists were the criteria for starting and switching treatments. This finding is consistent with previous studies (1). Surprisingly, although GNs started patients on DMTs later, they were inclined to switch treatments earlier and treat more RIS patients. This suggests that the GNs put too much value in MRI lesions in clinically normal patients. Interestingly, similar findings were observed in a study of Scottish neurologists (7). Lumley et al. reported (7) that, although 53% of neurologists stated they were adequately knowledgeable in diagnostic criteria for MS, only 9% were able to correctly diagnose MS in an inquiry using case examples (8). A similar situation may be applicable to neurologists in Turkey, or it may be caused by the physicians, having very short time for evaluating patients, incorrectly associating MRI findings with clinical observations. Moreover, another reason why the percentage of neurologists starting RIS patients on DMTs is so high could be the inadequacy of GNs in correctly interpreting MRI findings.
We also noted that GNs lacked sufficient regard for cerebral atrophy and low vitamin D levels. This might be due to difficulties in accessing and interpreting both of these laboratory examinations.
In conclusion, we have found that GNs differed significantly from NEMS in the management of patients with MS. There is a risk of MS patients being adversely affected by these differences in behavior of GNs who see far greater numbers of MS patients than NEMS do. Considering the possibility of flawed decision-making by GNs, who are under a heavy workload, it might be suggested that it is better for MS patients to be followed up by NEMS. It has been concluded, therefore, that there is need for a nationwide educational effort aimed at GNs, on the management of MS patients.
Study Limitations
The study was designed as a survey and respondents were expected to give their answers based on recollection of their experiences during the past year. This may have led to some questions having been answered incorrectly or inadequately.
Footnotes
Ethics Committee Approval: Authors declared that the research was conducted according to the principles of the World Medical Association Declaration of Helsinki “Ethical Principles for Medical Research Involving Human Subjects” (amended in October 2013)
Informed Consent: Written informed consent was obtained from patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - M.K., A.T., U.U.; Design - M.K., A.T., U.U., Z.Ç., A.K.P.; Supervision - R.A., A.A.; Resource - Z.Ç., A.K.P.; Materials - H.P., A.S.K., C.Ö., M.T., Ö.F.K.; Data Collection and/or Processing - M.K., A.T., U.U., H.P., A.S.K., C.Ö., M.T., Ö.F.K.; Analysis and/or Interpretation - M.K., A.T., U.U., Z.Ç., A.K.P., R.A., A.A.; Literature Search - M.K., A.T., U.U.; Writing - M.K., A.T., U.U.; Critical Reviews - R.A., A.A.
Conflict of Interest: Z.K. and A.K.P. are fulltime employees of Novartis, Turkey. Other authors do not have a conflict of interest relevant to the study.
Financial Disclosure: This study was sponsored by Novartis, Turkey.
REFERENCES
- 1.Ng P, Murray S, Hayes SM. Clinical decision-making in multiple sclerosis:Challenges reported internationally with emerging treatment complexity. Mult Scler Relat Disord. 2015;4:320–328. doi: 10.1016/j.msard.2015.05.008. [DOI] [PubMed] [Google Scholar]
- 2.Borisow N, Paul F, Ohlraun S, Pach D, Fischer F, Dörr J. Pregnancy in multiple sclerosis:a questionnaire study. PLoS One. 2014;9:e99106. doi: 10.1371/journal.pone.0099106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hanson KA, Agashivala N, Wyrwich KW, Raimundo K, Kim E, Brandes DW. Treatment selection and experience in multiple sclerosis:survey of neurologists. Patient Prefer Adherence. 2014;8:415–422. doi: 10.2147/PPA.S53140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Decoo D, Vokaer M. Treatment adherence in multiple sclerosis:a survey of Belgian neurologists. Patient Prefer Adherence. 2015;9:1669–1676. doi: 10.2147/PPA.S91973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fragoso YD. Survey of Latin American Neuroimmunologists on the Treatment of Multiple Sclerosis with Monoclonal Antibodies. Curr Drug Saf. 2015;10:217–220. doi: 10.2174/1574886310666150421113154. [DOI] [PubMed] [Google Scholar]
- 6.OECD Data. Magnetic resonance imaging (MRI) exams. Available at: https://data.oecd.org/healthcare/magnetic-resonance-imaging-mri-exams.htm .
- 7.Lumley R, Davenport R, Williams A. Most Scottish neurologists do not apply the 2010 McDonald criteria when diagnosing multiple sclerosis. J R Coll Physicians Edinb. 2015;45:23–26. doi: 10.4997/JRCPE.2015.106. [DOI] [PubMed] [Google Scholar]
- 8.Polman CH, Reingold SC, Banwell B, Clanet M, Cohen JA, Filippi M, Fujihara K, Havrdova E, Hutchinson M, Kappos L, Lublin FD, Montalban X, O'Connor P, Sandberg-Wollheim M, Thompson AJ, Waubant E, Weinshenker B, Wolinsky JS. Diagnostic criteria for multiple sclerosis:2010 revisions to the McDonald criteria. Ann Neurol. 2011;69:292–302. doi: 10.1002/ana.22366. [DOI] [PMC free article] [PubMed] [Google Scholar]


