Abstract
Background:
Surgical repair of rotator cuff (RC) tears is an effective treatment option. However, the prevalence of recurrent ruptures is high.
Hypothesis:
Recurrent tears are a frequent complication of surgical repair of RC tears. Their incidence might be influenced by factors such as the patient’s age and size of the initial tear.
Study Design:
Case series; Level of evidence, 4.
Methods:
Data from 90 adult patients who underwent arthroscopic RC repair between 2014 and 2017 and underwent an ultrasound examination 6 to 12 months after surgery were analyzed retrospectively. Massive tears were repaired using a double-row technique, and nonmassive tears were repaired with a single-row technique. Clinical records were reviewed for demographic information.
Results:
All patients (57.8% women; 42.2% men) were older than 18 years (mean, 58.9 years). Of these patients, 30.0% (27/90) had massive tears, which were primarily found in patients ≥60 years (74.1%; 20/27). Complete healing was seen in 74.5% of all repairs during follow-up. A total of 23 patients (25.5%) had retears (13 complete; 10 partial), which were diagnosed by ultrasound imaging 6 to 12 months after the initial surgery. The occurrence of retears was more prevalent in patients with massive tears than in patients with nonmassive tears (40.7% vs 19.0%, respectively); the difference was statistically significant (P = .03). Reruptures occurred in 50.0% of patients older than 60 years with massive tears. Although patients older than 60 years had more recurrent tears (32.6%) compared with younger patients (18.2%), the difference was not statistically significant (P = .12).
Conclusion:
One-quarter of the patients who had undergone surgical repair of an RC tear had recurrent ruptures. There was a statistically significant association between the initial massive tear and a retear. Patients older than 60 years showed a higher recurrence rate, but this difference lacked statistical significance. Reruptures occurred in 50.0% of patients older than 60 years with massive tears.
Keywords: massive tear, rotator cuff, rotator cuff tear, retear
Shoulder pain is one of the most common reasons for consultation, and a rotator cuff (RC) injury is the most frequent cause of this pain.46 Surgical repair of the RC is an effective treatment option with good clinical outcomes but with high social and financial costs27,28,31 as well as unacceptably high rates of structural failure, reaching up to 80% in massive tears.25 A rerupture of the RC is the most frequent complication of repair surgery.29 Failure rates of surgical repair between 20% and 94% have been reported in the literature.8,13,18 Factors predisposing patients to a recurrent tear include age,2,5,10 diabetes,39 smoking,9,34 size of the original tear,10,13,42 tissue quality, tendon delamination, and fat infiltration and muscular atrophy30 in addition to genetic,14,43–45 technical,39 and traumatic factors.32,41
RC retears occur primarily within 3 months after surgery, with a minority of cases occurring between 3 and 12 months.1,16,17 Once this period passes, the structural results appear to persist over time, as observed in 10-year follow-ups.6 Magnetic resonance imaging (MRI) and ultrasonography are the preferred tools for diagnosing RC tears and reruptures. Evidence shows similar sensitivity and specificity between the 2 techniques.3,23,36,40 Ultrasound has shown high sensitivity and specificity in demonstrating recurrent ruptures when compared with arthroscopic revision.12
Despite the high prevalence and economic impact of RC tears, many questions remain to be answered, especially regarding the postoperative healing capacity and causes of failure. The purpose of this study was to assess the frequency of recurrent tears in patients treated for RC tears at a university hospital in Colombia and to evaluate how this frequency could be affected by factors such as age and initial tear size.
Methods
Patients
We performed a retrospective review of the clinical records of 90 adult patients who underwent arthroscopic RC repair between 2014 and 2017 and underwent an ultrasound examination 6 to 12 months after surgery. Nonprobability sampling was performed. The personal medical history and information on the presurgical shoulder’s range of motion, supraspinatus and infraspinatus muscle strength, the American Shoulder and Elbow Surgeons score, and the visual analog scale for pain score were collected from the clinical records. Patients with a history of shoulder trauma, infections, humeral head avascular necrosis, augmentation of repair with the proximal biceps tendon,47 irreparable massive injuries, and previous shoulder surgery were excluded from the study. The protocol for this study was approved by an institutional review board.
The RC tears were classified as massive if they met at least 2 of the following 3 criteria: involvement of ≥2 tendons (footprint exposure >2.5 cm, as measured during surgery), Patte grade 2 or 3,35 and modified Goutallier grade 3 or 4 on MRI7 (Table 1).
TABLE 1.
Classification of Massive Versus Nonmassive Rotator Cuff Tears
| Patte Grade | Goutallier Grade | Arthroscopic Surgery | |
|---|---|---|---|
| Nonmassive | 1 | 1-2 | Footprint ≤2.5 cm in anteroposterior plane |
| Massive | 2-3 | 3-4 | Footprint >2.5 cm in anteroposterior plane |
Surgical Procedure
All procedures were performed by the same surgeon (P.J.L.), with the patient in the beach-chair position. Anesthesia consisted of an interscalene regional block and general anesthesia. An initial approach through a posterior portal was used for the assessment of glenohumeral structures. Surgical findings including cartilage quality and details on the biceps, subscapularis tendon, and labrum were noted in the clinical record.
According to age, all patients underwent either biceps tenotomy (patients ≥50 years of age) or suprapectoral tenodesis with titanium anchors (patients <50 years of age). Subscapularis tears of types III and IV20 were sutured through a glenohumeral portal with titanium anchors (4.5-mm HEALIX TI Dual Threaded Suture Anchor; DePuy Synthes). The subacromial space was assessed through the same posterior portal. Limited anterior arthroscopic acromioplasty was performed if coracoacromial ligament fraying was observed. The greater tuberosity was prepared with a shaver to leave a bleeding area for enhancing repair biology.
To evaluate the involvement of the supraspinatus and infraspinatus insertions, we changed the arthroscope to the lateral portal to obtain a frontal view of the tear and measure the anteroposterior distance of the footprint exposure using a probe calibrated every 5 mm (Figure 1). For lesions of the supraspinatus that involved the anterior pillar (“L” for left shoulders or “L” inverted for right shoulders), the most anterior reference point was the posterior lip of the bicipital groove.
Figure 1.
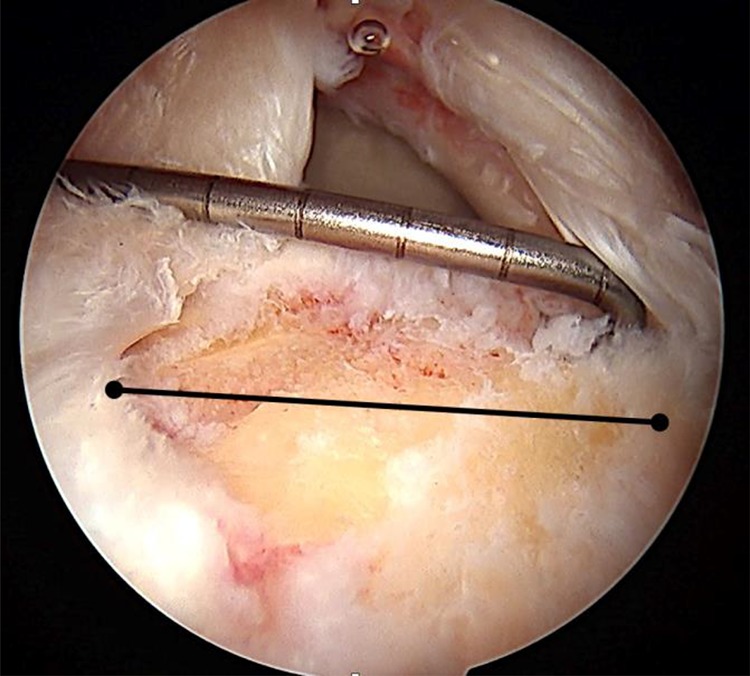
Measurement of footprint exposure in the anteroposterior plane.
For massive tears, the double-row technique with the transosseous-equivalent technique was preferred (HEALIX ADVANCE Knotless Anchor; DePuy Synthes), using the working portals as needed. For nonmassive tears, the single row with simple stitches technique was chosen (4.5-mm HEALIX TI Dual Threaded Suture Anchor).
Postoperative Rehabilitation
Postoperative management included shoulder immobilization with a 40° abductor pillow for 4 weeks, with free elbow and wrist mobility from day 1 after surgery. Active assisted exercises were started after the fourth week postoperatively for regaining range of motion. Muscle strength and proprioception were gradually rehabilitated. Sports activities were not allowed until 6 months postoperatively.
Ultrasonographic Diagnosis
All patients underwent a postoperative assessment with routine ultrasound imaging between 6 and 12 months after surgery, regardless of whether they had any symptoms. The ultrasound examination was performed by an expert radiologist certified in musculoskeletal injuries. Findings were classified as complete healing (no recurrent tear), complete retear, or partial retear, depending on the coverage of the footprint: total coverage, no coverage, or partial coverage, respectively15 (Figure 2).
Figure 2.
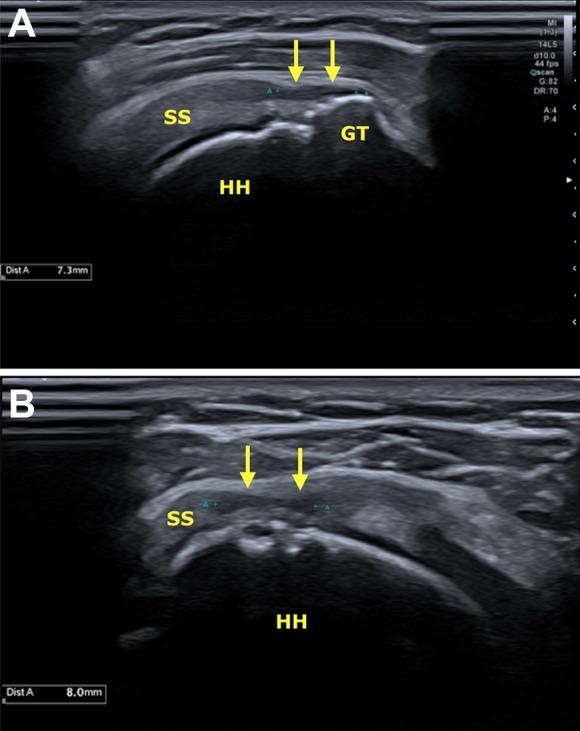
Ultrasound with a high-frequency (18 MHz) linear transducer: (A) longitudinal and (B) transverse planes of the supraspinatus tendon. Partial-thickness retear of the bursal fibers (yellow arrows), compromising 50% of the tendon. GT, greater tuberosity; HH, humeral head; SS, supraspinatus tendon.
Statistical Analysis
Data of interest (age, initial tear size, and presence or absence of retear) were registered in an Excel file (Microsoft). Once the database was completed, the quality of the data was evaluated by a random sample of 10% of the data. No inconsistencies were found. The distribution of continuous variables was determined by the Shapiro-Wilk test. Given that the distribution was normal, means and standard deviations were calculated. Categorical variables are reported as percentages. Comparisons of these variables were carried out with the chi-square test. P < .05 was considered statistically significant.
Results
Of the 90 patients included in this study, 57.8% (n = 52) were women. The mean age was 58.9 years. Moreover, 30.0% of the participants (27/90) had massive tears, and 74.1% of massive tears were in patients 60 years and older (20/27). A total of 23 patients (25.5%) had retears: 13 complete and 10 partial (Table 2). Patients with complete healing had a mean age of 57.4 years, whereas those with recurrent tears (either partial or complete) had a mean age of 62.8 years, and this difference was statistically significant (P = .04).
TABLE 2.
Patient and Tear Characteristics (N = 90)a
| Age, mean ± SD, y | 58.9 ± 11.9 |
| Sex | |
| Male | 38 (42.2) |
| Female | 52 (57.8) |
| Initial tear | |
| Massive | 27 (30.0) |
| Nonmassive | 63 (70.0) |
| Ultrasound result | |
| Complete healing | 67 (74.5) |
| Partial retear | 10 (11.1) |
| Complete retear | 13 (14.4) |
aData are reported as n (%) unless otherwise specified.
Regarding the influence of initial tear size, 40.7% (11/27) of the patients with massive tears had a recurrent rupture, whereas 19.0% (12/63) of the patients with nonmassive tears presented with a rerupture. This difference was statistically significant (P = .03) (Table 3).
TABLE 3.
Influence of Initial Tear Size on the Presence of Rerupturesa
| Retear (n = 23) | Complete Healing (n = 67) | P Value | |
|---|---|---|---|
| Initial tear size | .03 | ||
| Massive (n = 27) | 11 (40.7) | 16 (59.3) | |
| Nonmassive (n = 63) | 12 (19.0) | 51 (81.0) |
aData are reported as n (%).
Recurring ruptures occurred in 32.6% (15/46) of the patients 60 years and older, whereas 18.2% (8/44) of the patients younger than 60 years experienced reruptures. However, this difference was not statistically significant (P = .12) (Table 4).
TABLE 4.
Influence of Age on the Presence of Rerupturesa
| Retear (n = 23) | Complete Healing (n = 67) | P Value | |
|---|---|---|---|
| Age | .12 | ||
| ≥60 y (n = 46) | 15 (32.6) | 31 (67.4) | |
| <60 y (n = 44) | 8 (18.2) | 36 (81.8) |
aData are reported as n (%).
Patients 60 years and older with massive tears had a recurrent tear in 50.0% of the cases, whereas those 60 years and older with nonmassive tears had recurrence in 19.2% of the cases. This difference was statistically significant (P = .03) (Table 5).
TABLE 5.
Influence of Older Age and Initial Tear Size on the Presence of Rerupturesa
| Retear | Complete Healing | P Value | |
|---|---|---|---|
| Age and initial tear size | .03 | ||
| ≥60 y with massive tears (n = 20) | 10 (50.0) | 10 (50.0) | |
| ≥60 y with nonmassive tears (n = 26) | 5 (19.2) | 21 (80.8) |
aData are reported as n (%).
Discussion
In our retrospective case series, the rerupture rate was 25.5%, which is consistent with that reported in the literature (20%-94%).8,13,18 We found that the involvement of ≥2 tendons in the initial rupture (footprint exposure >2.5 cm from the greater tuberosity, measured during surgery), Patte grade 2 or 3, and modified Goutallier grade 3 or 4 were statistically significant factors that negatively affected healing. Patients with massive ruptures developed a retear in 40.7% of the cases versus 19.0% of the patients with nonmassive ruptures. Many researchers have identified RC tear size as a variable that affects the healing process.21,22,33
There is significant confusion regarding the term “massive” in the literature. Gerber et al11 defined “massive” as the presence of ≥2 ruptured tendons. By this definition, based on anatomic insertions of the supraspinatus and infraspinatus muscles, all tears more than 1.5 cm from the greater tuberosity would be massive. This classification differs from that of DeOrio and Cofield,4 who defined “massive” as tears measuring more than 5 cm. The elastic properties of tendons make this measurement vulnerable to variables such as the degree of shoulder traction, tear configuration, size of the patient, and surgical position. Therefore, neither classification is clear for defining such involvement, which leads to interpretations that do not aid in concept standardization.
Footprint measurement after preparation for RC reinsertion in the greater tuberosity is a more reliable value that is unaffected by the age, sex, height, size, or position of the patient.26 Measurements exceeding footprint exposure by 2.5 cm indicate that the supraspinatus is fully involved as well as at least 50% of the infraspinatus. On the other hand, despite moderate reliability in terms of interobserver assessments of retraction and fat degeneration on MRI (Patte and Goutallier),24 there is a consensus regarding a poorer prognosis in patients with Patte grade 2 or 3 and Goutallier grade 3 or 4 during midterm clinical and structural follow-up.
Kwon et al19 used a multivariate analysis of independent factors that affect RC healing. They proposed a 15-point scoring system that included age >70 years at the time of surgery, size of the tear in the anteroposterior dimension and retraction, fatty infiltration of the infraspinatus grade >2, low bone mineral density, and high level of work activity. As found in our study, a footprint exposure of >2.5 cm was considered to have a negative effect on tendon healing. However, we consider it difficult to apply this scoring system to all patients. If the term “massive” is to be taken as indicative of a poor prognosis, we propose that the definition of “massive” should be based on MRI7,35 and arthroscopic findings, which are more consistent with clinical results (Table 1).
Our results were not as conclusive regarding age. In our series, there was a statistically significant difference in the mean age of patients with healed tears compared with patients with unhealed tears (57.4 vs 62.8 years, respectively). Structural failures occurred in 40.7% of the patients with a massive tear. This proportion increased up to 50.0% in patients who had a massive tear and were 60 years and older. In contrast, when the injury size was not considered, our recurrence rate in patients 60 and older was 32.6% and, with the numbers available for this study, was not statistically significant compared with patients younger than 60 (18.2%). Furthermore, the recurrence rate was similar in patients 60 and older with nonmassive tears and patients younger than 60 (19.2% and 18.2%, respectively). It is important to mention that the small sample size might have weakened the statistical power of our findings; thus, further studies with more participants should be conducted to clarify them.
Boileau et al2 concluded that RC healing is markedly influenced by age, with a 57% failure risk in patients older than 65 years. In a series, Diebold et al5 found that age is a factor that conditions the presence of RC reruptures, with rates increasing by 5% each decade from the age of 50 years and scaling upward substantially after the age of 70 years. In a study including 693 patients, Lee et al22 concluded that the patient’s age, initial rupture size, and fat degeneration of the supraspinatus are independent risk factors for an RC rerupture. Other studies38 agree with our findings regarding proper healing in patients older than 70 years, concluding that a rerupture is more affected by the initial size than by age. In a 238-patient series, Rhee et al37 concluded that the retear rate increased significantly with increasing intraoperative tear size but not with increasing age.
In our series, the tear size increased with age. The mean age of the patients with nonmassive tears was 58.1 years compared with 64.7 years among patients with massive tears. In addition, 74.1% of massive tears occurred in patients older than 60 years. Moreover, the percentage of massive tears was higher in patients 60 years and older (20/46; 43.5%) compared with patients younger than 60 years (7/44; 15.9%); the risk ratio was 2.73 (95% CI, 1.29-5.81; P = .004). Thus, it is unclear whether age is really a factor associated with recurrent ruptures or only a confounding factor because of its association with larger initial tears. Additional studies with larger sample sizes should be conducted with multivariate analysis, which will clarify this doubt.
Ultrasonography was chosen as the follow-up technique because its sensitivity and specificity are both similar to those of MRI in addition to its greater availability, lower cost, and relative harmlessness; in addition, it is not affected by the presence of metal anchors. Furthermore, the radiologist at our institution has wide experience in musculoskeletal injuries. There is evidence confirming that most retears occur in the first 3 months after surgery.32,41 Consequently, ultrasound follow-up after 6 to 12 months is an effective technique for obtaining patients’ structural results.
Last, this case series was retrospective; therefore, one of its limitations is that it did not allow us to calculate measures of association such as risk ratios. Further studies in which risk ratios could be estimated, and thus risk factors for RC tear recurrence could be established, are warranted. Another limitation is that we had no strict protocol indicating the specific times at which ultrasound should be performed after surgery. Moreover, because of the small sample size, the risk of a type II error is increased.
Conclusion
The retear rate after RC repair was 25.5% in the current study. There was a statistically significant difference in complete healing between patients with nonmassive tears and patients with massive tears (81.0% vs 59.3%, respectively). Patients older than 60 years with RC ruptures developed retears more frequently than those younger than 60 years; however, with the numbers available for this study, the difference was not statistically significant.
Acknowledgment
The authors thank Laura Zamudio Castilla, MD, for helping with the statistical analysis.
Footnotes
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Comité de Etica en Investigación Biomédica de la Fundación Valle del Lili (protocol No. 1180).
References
- 1. Barth J, Andrieu K, Fotiadis E, Hannink G, Barthelemy R, Saffarini M. Critical period and risk factors for retear following arthroscopic repair of the rotator cuff. Knee Surg Sports Traumatol Arthrosc. 2017;25(7):2196–2204. [DOI] [PubMed] [Google Scholar]
- 2. Boileau P, Brassart N, Watkinson DJ, Carles M, Hatzidakis AM, Krishnan SG. Arthroscopic repair of full-thickness tears of the supraspinatus: does the tendon really heal? J Bone Joint Surg Am. 2005;87(6):1229–1240. [DOI] [PubMed] [Google Scholar]
- 3. Codsi MJ, Rodeo SA, Scalise JJ, Moorehead TM, Ma CB. Assessment of rotator cuff repair integrity using ultrasound and magnetic resonance imaging in a multicenter study. J Shoulder Elbow Surg. 2014;23(10):1468–1472. [DOI] [PubMed] [Google Scholar]
- 4. DeOrio JK, Cofield RH. Results of a second attempt at surgical repair of a failed initial rotator-cuff repair. J Bone Joint Surg Am. 1984;66(4):563–567. [PubMed] [Google Scholar]
- 5. Diebold G, Lam P, Walton J, Murrell GAC. Relationship between age and rotator cuff retear. J Bone Joint Surg Am. 2017;99(14):1198–1205. [DOI] [PubMed] [Google Scholar]
- 6. Elia F, Azoulay V, Lebon J, Faraud A, Bonnevialle N, Mansat P. Clinical and anatomic results of surgical repair of chronic rotator cuff tears at ten-year minimum follow-up. Int Orthop. 2017;41(6):1219–1226. [DOI] [PubMed] [Google Scholar]
- 7. Fuchs B, Weishaupt D, Zanetti M, Hodler J, Gerber C. Fatty degeneration of the muscles of the rotator cuff: assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elbow Surg. 1999;8(6):599–605. [DOI] [PubMed] [Google Scholar]
- 8. Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am. 2004;86(2):219–224. [DOI] [PubMed] [Google Scholar]
- 9. Galatz LM, Silva MJ, Rothermich SY, Zaegel MA, Havlioglu N, Thomopoulos S. Nicotine delays tendon-to-bone healing in a rat shoulder model. J Bone Joint Surg Am. 2006;88(9):2027–2034. [DOI] [PubMed] [Google Scholar]
- 10. Gazielly DF, Gleyze P, Montagnon C. Functional and anatomical results after rotator cuff repair. Clin Orthop Relat Res. 1994;304:43–53. [PubMed] [Google Scholar]
- 11. Gerber C, Fuchs B, Hodler J. The results of repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 2000;82(4):505–515. [DOI] [PubMed] [Google Scholar]
- 12. Gilat R, Atoun E, Cohen O, et al. Recurrent rotator cuff tear: is ultrasound imaging reliable? J Shoulder Elbow Surg. 2018;27(7):1263–1267. [DOI] [PubMed] [Google Scholar]
- 13. Harrymanm DT, 2nd, Mack LA, Wang KY, Jackins SE, Richardson ML, Matsen FA., 3rd Repairs of the rotator cuff: correlation of functional results with integrity of the cuff. J Bone Joint Surg Am. 1991;73(7):982–989. [PubMed] [Google Scholar]
- 14. Harvie P, Ostlere SJ, Teh J, et al. Genetic influences in the aetiology of tears of the rotator cuff: sibling risk of a full-thickness tear. J Bone Joint Surg Br. 2004;86(5):696–700. [DOI] [PubMed] [Google Scholar]
- 15. Kamath G, Galatz LM, Keener JD, Teefey S, Middleton W, Yamaguchi K. Tendon integrity and functional outcome after arthroscopic repair of high-grade partial-thickness supraspinatus tears. J Bone Joint Surg Am. 2009;91(5):1055–1062. [DOI] [PubMed] [Google Scholar]
- 16. Kim JH, Hong IT, Ryu KJ, Bong ST, Lee YS, Kim JH. Retear rate in the late postoperative period after arthroscopic rotator cuff repair. Am J Sports Med. 2014;42(11):2606–2613. [DOI] [PubMed] [Google Scholar]
- 17. Kluger R, Bock P, Mittlbock M, Krampla W, Engel A. Repairs using ultrasound and magnetic resonance imaging analysis: long-term survivorship of rotator cuff. Am J Sports Med. 2011;39(10):2071–2081. [DOI] [PubMed] [Google Scholar]
- 18. Knudsen HB, Gelineck J, Søjbjerg JO, Olsen BS, Johannsen HV, Sneppen O. Functional and magnetic resonance imaging evaluation after single-tendon rotator cuff reconstruction. J Shoulder Elbow Surg. 1999;8(3):242–246. [DOI] [PubMed] [Google Scholar]
- 19. Kwon J, Kim SH, Lee YH, Kim TI, Oh JH. The rotator cuff healing index: a new scoring system to predict rotator cuff healing after surgical repair. Am J Sports Med. 2019;47(1):173–180. [DOI] [PubMed] [Google Scholar]
- 20. Lafosse L, Jost B, Reiland Y, Audebert S, Toussaint B, Gobezie R. Structural integrity and clinical outcomes after arthroscopic repair of isolated subscapularis tears. J Bone Joint Surg Am. 2007;89(6):1184–1193. [DOI] [PubMed] [Google Scholar]
- 21. Le BT, Wu XL, Lam PH, Murrell GA. Factors predicting rotator cuff retears: an analysis of 1000 consecutive rotator cuff repairs. Am J Sports Med. 2014;42(5):1134–1142. [DOI] [PubMed] [Google Scholar]
- 22. Lee YS, Jeong JY, Park CD, Kang SG, Yoo JC. Evaluation of the risk factors for a rotator cuff retear after repair surgery. Am J Sports Med. 2017;45(8):1755–1761. [DOI] [PubMed] [Google Scholar]
- 23. Lenza M, Buchbinder R, Takwoingi Y, Johnston RV, Hanchard NC, Faloppa F. Magnetic resonance imaging, magnetic resonance arthrography and ultrasonography for assessing rotator cuff tears in people with shoulder pain for whom surgery is being considered. Cochrane Database Syst Rev. 2013;24(9):CD009020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lippe J, Spang JT, Leger RR, Arciero RA, Mazzocca AD, Shea KP. Inter-rater agreement of the Goutallier, Patte, and Warner classification scores using preoperative magnetic resonance imaging in patients with rotator cuff tears. Arthroscopy. 2012;28(2):154–159. [DOI] [PubMed] [Google Scholar]
- 25. Lo IKY, Burkhart SS. Arthroscopic revision of failed rotator cuff repairs: technique and results. Arthroscopy. 2004;20(3):250–267. [DOI] [PubMed] [Google Scholar]
- 26. Lumsdaine W, Smith A, Walker RG, Benz D, Mohammed KD, Stewart F. Morphology of the humeral insertion of the supraspinatus and infraspinatus tendons: application to rotator cuff repair. Clin Anat. 2015;28(6):767–773. [DOI] [PubMed] [Google Scholar]
- 27. Makhni EC, Swart E, Steinhaus ME, et al. Cost-effectiveness of reverse total shoulder arthroplasty versus arthroscopic rotator cuff repair for symptomatic large and massive rotator cuff tears. Arthroscopy. 2016;32(9):1771–1780. [DOI] [PubMed] [Google Scholar]
- 28. Mather RC, Koenig L, Acevedo D, et al. The societal and economic value of rotator cuff repair. J Bone Joint Surg Am. 2013;95(22):1993–2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Mazzocca AD, Millett PJ, Guanche CA, Santangelo SA, Arciero RA. Arthroscopic single-row versus double-row suture anchor rotator cuff repair. Am J Sports Med. 2005;33(12):1861–1868. [DOI] [PubMed] [Google Scholar]
- 30. Melis B, DeFranco MJ, Chuinard C, Walch G. Natural history of fatty infiltration and atrophy of the supraspinatus muscle in rotator cuff tears. Clin Orthop Relat Res. 2010;468(6):1498–1505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Narvy SJ, Ahluwalia A, Vangsness CTJ. Analysis of direct costs of outpatient arthroscopic rotator cuff repair. Am J Orthop (Belle Mead NJ). 2016;45(1):E7–E11. [PubMed] [Google Scholar]
- 32. Neviaser RJ. Evaluation and management of failed rotator cuff repairs. Orthop Clin North Am. 1997;28(2):215–224. [DOI] [PubMed] [Google Scholar]
- 33. Nho SJ, Brown BS, Lyman S, Adler RS, Altchek DW, MacGillivray JD. Prospective analysis of arthroscopic rotator cuff repair: prognostic factors affecting clinical and ultrasound outcome. J Shoulder Elbow Surg. 2009;18(1):13–20. [DOI] [PubMed] [Google Scholar]
- 34. Park JH, Oh KS, Kim TM, et al. Effect of smoking on healing failure after rotator cuff repair. Am J Sports Med. 2018;46(12):2960–2968. [DOI] [PubMed] [Google Scholar]
- 35. Patte D. Classification of rotator cuff lesions. Clin Orthop Relat Res. 1990;254:81–86. [PubMed] [Google Scholar]
- 36. Prickett WD, Teefey SA, Galatz LM, et al. Accuracy of ultrasound imaging of the rotator cuff in shoulders that are painful postoperatively. J Bone Joint Surg Am. 2003;85(6):1084–1089. [DOI] [PubMed] [Google Scholar]
- 37. Rhee YG, Cho NS, Yoo JH. Clinical outcome and repair integrity after rotator cuff repair in patients older than 70 years versus patients younger than 70 years. Arthroscopy. 2014;30(5):546–554. [DOI] [PubMed] [Google Scholar]
- 38. Robinson PM, Wilson J, Dalal S, Parker RA, Norburn P, Roy BR. Rotator cuff repair in patients over 70 years of age. Bone Joint J. 2013;95(2):199–205. [DOI] [PubMed] [Google Scholar]
- 39. Sherman SL, Lyman S, Koulouvaris P, Willis A, Marx RG. Risk factors for readmission and revision surgery following rotator cuff repair. Clin Orthop Relat Res. 2008;466(3):608–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Smith TO, Back T, Toms AP, Hing CB. Diagnostic accuracy of ultrasound for rotator cuff tears in adults: a systematic review and meta-analysis. Clin Radiol. 2011;66(11):1036–1048. [DOI] [PubMed] [Google Scholar]
- 41. Sonnabend DH, Howlett CR, Young AA. Histological evaluation of repair of the rotator cuff in a primate model. J Bone Joint Surg Br. 2010;92(4):586–594. [DOI] [PubMed] [Google Scholar]
- 42. Sugaya H, Maeda K, Matsuki K, Moriishi J. Repair integrity and functional outcome after arthroscopic double-row rotator cuff repair: a prospective outcome study. J Bone Joint Surg Am. 2007;89(5):953–960. [DOI] [PubMed] [Google Scholar]
- 43. Tashjian RZ. Evidence for an inherited predisposition contributing to the risk for rotator cuff disease. J Bone Joint Surg Am. 2009;91(5):1136–1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Tashjian RZ, Granger EK, Farnham JM, Cannon-Albright LA, Teerlink CC. Genome-wide association study for rotator cuff tears identifies two significant single-nucleotide polymorphisms. J Shoulder Elbow Surg. 2016;25(2):174–179. [DOI] [PubMed] [Google Scholar]
- 45. Tashjian RZ, Granger EK, Zhang Y, Teerlink CC, Cannon-Albright LA. Identification of a genetic variant associated with rotator cuff repair healing. J Shoulder Elbow Surg. 2016;25(6):865–872. [DOI] [PubMed] [Google Scholar]
- 46. Teefey SA, Middleton WD, Payne WT, Yamaguchi K. Detection and measurement of rotator cuff tears with sonography: analysis of diagnostic errors. AJR Am J Roentgenol. 2005;184(6):1768–1773. [DOI] [PubMed] [Google Scholar]
- 47. Veen EJD, Stevens M, Diercks RL. Biceps autograft augmentation for rotator cuff repair: a systematic review. Arthroscopy. 2018;34(4):1297–1305. [DOI] [PubMed] [Google Scholar]


