PRACTICAL IMPLICATIONS
Consider seizures in the differential diagnosis of atypical or unusual behaviors in patients with genetic neurologic syndromes such as Angelman syndrome. Focal frontal lobe seizures can be mistaken for stereotyped behaviors, particularly when there is bilateral motor activity with preserved awareness, and are difficult to diagnose without video-EEG.
Reflex epilepsies are a rare entity, occurring when seizures are triggered by specific well-defined sensory or cognitive stimuli.1 Among reflex seizures, those triggered by micturition or defecation are rarely described.2 Angelman syndrome is a rare neurologic genetic disorder caused by abnormalities involving chromosome 15q11–13, leading to severe neurodevelopmental delay, microcephaly, hypotonia, ataxia, hyperreflexia, and commonly drug-resistant epilepsy.3 Although multiple seizure types are seen in Angelman syndrome, reflex seizures are uncommon. We report a case of a patient with Angelman syndrome and micturition and defecation reflex seizures, initially unrecognized due to having an uncommon semiology characterized by bilateral clonic activity with preserved awareness.
Case
A 9-year-old boy with Angelman syndrome presented for evaluation of ongoing paroxysmal events of unclear etiology over the past year. His parents described these as bilateral hand and feet shaking without loss of awareness, which were consistently triggered by micturition with or without concomitant bowel movements. Sometimes, they also occurred spontaneously or while his parents were helping him put on clothing. Before the onset of these events, he had undergone screening encephalography (EEG) and was found to have epileptiform discharges. For this reason, he was started on valproic acid (VPA). Although the dose was titrated up to 750 mg twice daily (33 mg/kg/d), achieving a trough serum level of 93 μg/mL (therapeutic range 50–125 μg/mL), he continued experiencing events according to his parents. Previous pertinent diagnostic studies included normal MRI of the brain at ages 3 and 6 years and a methylation study that was consistent with Angelman syndrome.
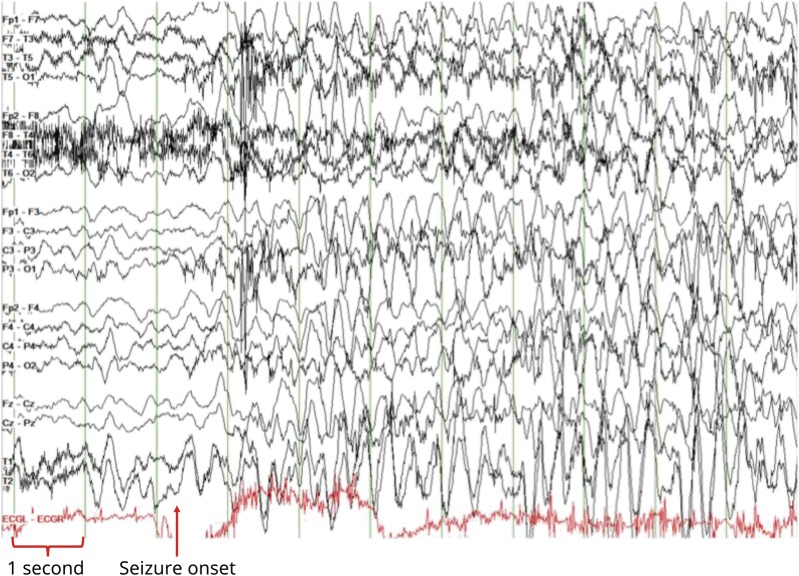
During video-EEG monitoring, the patient used the restroom 5 times, accompanied by his parents, who pressed the event button at the onset of his typical event triggered by micturition with or without defecation. These were found to be electroclinical seizures lasting up to 40 seconds, corresponding to the electrographic pattern shown in the figure Less frequently, the patient also experienced these spontaneously or triggered by tactile stimuli involving his parents dressing him (specifically putting on a shirt or jacket). The clinical seizure semiology consisted of hypermotor and clonic movements of bilateral arms and legs with preserved awareness. The EEG seizure pattern was characterized by rapid evolution of diffuse rhythmic high voltage delta activity with admixed spikes, which was not seen interictally (figure). Given the poor efficacy of VPA monotherapy, clobazam was initiated, decreasing seizure frequency by 60%–70% over the following 2 weeks according to the parents.
Figure. EEG.
EEG of electroclinical seizure onset (arrow), viewed in a longitudinal bipolar montage (double banana), with a low-frequency filter set at 1 Hz and high-frequency filter set at 70 Hz, a notch filter set at 60 Hz, and at a sensitivity of 10 μV/mm, with a timebase of 30 mm/s. At onset, there is diffuse and rapid evolution of high-amplitude rhythmic “notched” delta activity (delta with admixed spikes). The patient's clinical seizure onset was characterized by bilateral hypermotor and clonic activity with preserved awareness triggered by micturition and correlated with the EEG onset. EEG = encephalography.
Discussion
Reflex epilepsies comprise a small portion of seizures in patients with epilepsy. They are most common in idiopathic generalized epilepsies (IGEs)—e.g., photosensitive seizures in juvenile myoclonic epilepsy. In IGEs, they are primarily related to network function, whereas in focal epilepsies, they are related to the specific location of the epileptogenic focus.1 Epilepsy occurs in up to 80% of children with Angelman syndrome, typically with an onset before age 3 years.4 Multiple seizure types occur, and sometimes multiple in the same individual. The most frequent are atypical absence, atonic, myoclonic, or generalized tonic-clonic seizures.5
Reflex epilepsies are uncommon and even more rarely observed in Angelman syndrome. A case of reflex seizures has been described in a patient with both Angelman syndrome and trisomy 21. This patient experienced multiple seizure types, including reflex seizures triggered by taking shirts on or off, drinking water, or eating food—though, not in response to micturition or defecation.6 Among reported cases of patients with reflex micturition seizures, there have been rare reports of these occurring with both preserved awareness and bilateral motor activity including clonic activity. This is possibly due to excess activation of frontal cortical midline regions involved in micturition, which could generate a focal seizure in this region.2 This is concordant with the seizure semiology in our patient, who maintained awareness while experiencing bilateral clonic activity. In addition to reflex seizures, our patient had characteristic EEG findings described in patients with Angelman syndrome, including intermittent delta frequency (2–4 Hz) slow waves.4,5,7
Hyperkinetic and stereotyped behaviors are common in Angelman syndrome and other neurodevelopmental disorders. Our case highlights the importance of characterizing suspicious stereotyped behaviors using video-EEG. This is particularly important in disorders known to portend a higher risk of epilepsy, as behavioral events are at risk of being misinterpreted based on clinical semiology alone, which may lead to either over- or under-treatment.
Author contributions
J. Pellinen: primary author, writing and editing for content. H. Hasan, N. Ortiz, J. Bluvstein, and D. Miles: writing and editing for content.
Study funding
No targeted funding reported.
Disclosure
The authors report no disclosures relevant to the manuscript. Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/cp.
References
- 1.Wolf P. Reflex epileptic mechanisms in humans: lessons about natural ictogenesis. Epilepsy Behav 2017;71:118–123. [DOI] [PubMed] [Google Scholar]
- 2.Jang HJ, Kwon MJ, Cho KO. Central regulation of micturition and its association with epilepsy. Int Neurourol J 2018;22:2–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Buiting K, Williams C, Horsthemke B. Angelman syndrome—insights into a rare neurogenetic disorder. Nat Rev Neurol 2016;12:584–593. [DOI] [PubMed] [Google Scholar]
- 4.Vendrame M, Loddenkemper T, Zarowski M, et al. Analysis of EEG patterns and genotypes in patients with Angelman syndrome. Epilepsy Behav 2012;23:261–265. [DOI] [PubMed] [Google Scholar]
- 5.Fiumara A, Pittalà A, Cocuzza M, Sorge G. Epilepsy in patients with Angelman syndrome. Ital J Pediatr 2010;36:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ferlazzo E, Sueri C, Elia M, D'Agostino T, Aguglia U. Reflex seizures in a patient with Angelman syndrome and trisomy 21. Neurol Sci 2016;37:1373–1374. [DOI] [PubMed] [Google Scholar]
- 7.Laan LA, Vein AA. Angelman syndrome: is there a characteristic EEG? Brain Dev 2005;27:80–87. [DOI] [PubMed] [Google Scholar]