PRACTICAL IMPLICATIONS
Vessel wall MR imaging may be helpful in diagnosing and monitoring the treatment of vasculitic complications from CNS infections.
The World Health Organization reports tuberculosis (TB) as the ninth leading cause of death globally.1 CNS TB has a higher mortality and morbidity than pulmonary TB with tuberculous meningitis (TBM) being the most common manifestation.2 Vasculitis from thick exudates is a common vascular complication of TBM. Imaging is critically important to diagnose CNS TB as laboratory diagnosis carries low sensitivity and specificity.3,4 We present a case of pediatric CNS TB complicated by cerebral vasculitis. We show the radiologic evolution of the disease and infectious vasculitis by serial vessel wall imaging (VWI), which uses black blood T1-weighted sequences acquired before and after the administration of gadolinium. This case shows the utility of VWI in diagnosing and monitoring an infectious vasculitis.
Case
A 6-year-old immunocompetent girl presented with left facial and left arm weakness following a generalized tonic-clonic seizure. Her mother reported fevers ranging up to 102°F and headaches. Her immunizations were up-to-date. Her physical examination was negative for neck pain or stiffness, vision changes, rashes, or oral ulcers. Her laboratory test results showed a normal white blood cell (WBC) count. A lumbar puncture (LP) showed a lymphocytic pleocytosis, borderline low glucose (59 mg/dL, normal 60–80), and normal protein (30 mg/dL, normal 15–45). A brain MRI showed hypoperfusion in the right middle cerebral artery (MCA) territory without infarction. Magnetic resonance angiogram showed mildly decreased caliber of the right MCA branches. She was treated with IV vancomycin, ceftriaxone, and acyclovir until herpes simplex virus encephalitis was excluded by a negative CSF PCR, and bacterial meningitis was excluded by negative CSF cultures at 48 hours. She was discharged home with clinical improvement and a working diagnosis of postictal changes.
Ten days later, she re-presented to the emergency department with persistent fevers, headaches, and left upper extremity weakness. Serology showed leukocytosis (9,200 cells/μL; 70% polymorphonuclear leukocytes, 13% eosinophils), and an erythrocyte sedimentation rate of 46. A LP showed worsening pleocytosis (WBC 252/mm3, 63% lymphocytes, 29% polymorphonuclear leukocytes), elevated protein (87 mg/dL), and decreased glucose (39 mg/dL). A chest radiograph was negative. Brain and spine MRIs showed new acute infarctions and craniospinal leptomeningeal enhancement. She was started on aspirin and restarted on acyclovir, ceftriaxone, and vancomycin for a possible infectious meningitis. An expanded bacterial, viral, and fungal work-up, including a purified protein derivative skin test and CSF acid-fast bacillus stain, returned negative. A T-SPOT test was run given her history of travel to a TB-endemic region 2 years prior but returned as borderline.
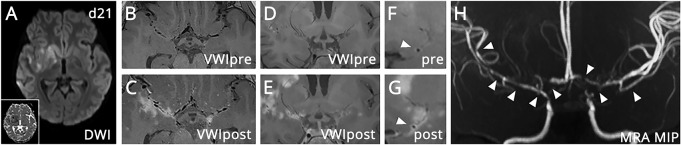
Two days later, a new left facial droop prompted another brain MRI, which showed infarction extension into the right basal ganglia and multiple new right MCA territory punctate cortical infarctions. VWI showed circumferential vessel wall thickening and enhancement consistent with vasculitis. The imaging findings, travel history, and the borderline T-SPOT test led to a working diagnosis of TBM with vasculitis. Isoniazid, pyrazinamide, rifampin, and ethionamide was started. Due to a drug interaction between Plavix and isoniazid, 81 mg of aspirin followed by enoxaparin for stroke prevention was initiated. An intravenous steroid pulse and 2-month course of oral steroids for vasculitis were completed. A brain MRI during initial treatment (day 21) showed expected evolution of the infarctions (figure 1A) and persistent vessel wall thickening and enhancement (figure 1, B–H). A repeat positive T-SPOT test and the constellation of imaging findings led to a clinical diagnosis of vasculitis and probable TBM, according to published criteria.2
Figure 1. Brain MRI with VWI (day 21).
(A) Diffusion-weighted imaging shows an evolving right MCA infarction in the right basal ganglia, insula, and frontotemporal cortex. Inset shows corresponding hypointensity on the ADC map. (B and C) Axial VWI pre- and postcontrast images show parenchymal and multifocal vessel wall thickening and enhancement predominantly involving the proximal right MCA. (D and E) Coronal VWI pre- and postcontrast images show enhancement centered around the origins of the medial lenticulostriate arteries of the M1 MCA. (F and G) Orthogonal views (sagittal oblique plane) of the right M1 MCA shows vessel wall thickening and enhancement of the right M1 MCA (arrowheads) on pre- and postcontrast imaging. (H) 3D time-of-flight MRA of the anterior circulation shows loss of flow–related enhancement in the supraclinoid internal carotid arteries and multisegmental beading and irregularity of the bilateral internal carotid artery termini and proximal ACAs and MCAs (arrowheads). ACA = anterior cerebral artery; ADC = apparent diffusion coefficient; MCA = middle cerebral artery; MRA = magnetic resonance angiogram; VWI = vessel wall MR imaging.
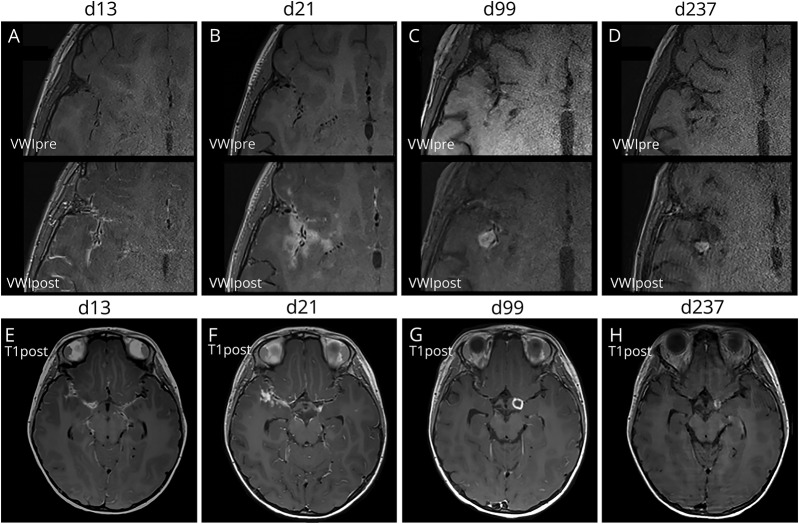
Serial brain MRI with VWI (figure 2, A–H) during the treatment course showed gradual radiographic improvement. At day 99, tuberculomas developed (figure 2, C and G). By day 164, leptomeningeal and vessel wall enhancement decreased (figure 2, C, D, G, and H). Treatment with a 4-drug regimen was continued for 1 year followed by a 2-drug maintenance phase (isoniazid and rifampin). She was successfully weaned from steroids. Following discontinuation of enoxaparin at 7 months, she continued with aspirin therapy for stroke prophylaxis. She showed improved cerebral artery vessel caliber by day 237 and has not had a clinical or a radiographic infarct since day 172.
Figure 2. Serial vessel wall MR and T1 SPACE images.
Pre- and postcontrast VWI images of the right frontotemporal sulci at the level of the right sylvian fissure are shown at (A) 13, (B) 21, (C) 99, and (D) 237 days from initial presentation. (A) At 13 days, leptomeningeal and vessel wall enhancement is present. (B) At 21 days, parenchymal enhancement consistent with cerebritis and evolving infarctions centered around the infected vessels were present. (C) At 99 days, an enhancing tuberculoma in the right sylvian fissure developed. Concurrently, there was resolution of the parenchymal enhancement and decreased vessel wall enhancement. (D) By 237 days, there was complete resolution of the vessel wall enhancement leaving only residual wall thickening and a contracting tuberculoma. (E–F) At days 13 and 21, imaging shows thick enhancing basilar exudates in the sylvian fissures bilaterally. (G–H) By day 99, a ring-enhancing tuberculoma in the left suprasellar cistern developed, which gradually contracted by day 237. VWI = vessel wall MR imaging.
Discussion
Diagnosis of TBM and cerebral vasculitis is challenging and relies heavily on a combination of clinical, laboratory, and radiologic findings. However, many laboratory tests have low sensitivity for TBM and imaging plays a critical role in supporting a diagnosis of TBM and its complications. Secondary complications of TBM include hydrocephalus, infarction, arachnoiditis, abscesses, tuberculomas and vasculitis.5 This case showed rapidly progressive CNS vasculitis as a complication of TBM. Through serial brain MRI examinations with VWI, the treatment was monitored and showed subsequent radiographic resolution of the vessel wall enhancement.
Author contributions
J. Song contributed to the conceptualization of the study, acquisition of data, analysis of the data, and drafting of the manuscript for intellectual context. L. Lehman contributed to the conceptualization of the study, acquisition of data, analysis of the data, and drafting of the manuscript for intellectual context. M. Rivkin contributed to the conceptualization of the study, acquisition of data, analysis of the data, and drafting of the manuscript for intellectual context. M. Gorman contributed to the conceptualization of the study, acquisition of data, analysis of the data, and drafting of the manuscript for intellectual context. E. Yang contributed to the conceptualization of the study, acquisition of data, analysis of the data, and drafting of the manuscript for intellectual context.
Study funding
No targeted funding reported.
Disclosure
The authors report no disclosures relevant to the manuscript. Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/cp.
References
- 1.World Health Organization. Global Tuberculosis Report 2017. World Health Organization; 2017. Available at: who.int/tb/publications/global_report/en/. Accessed May 1, 2018. [Google Scholar]
- 2.Marais S, Thwaites G, Schoeman JF, et al. . Tuberculous meningitis: a uniform case definition for use in clinical research. Lancet Infect Dis 2010;10:803–812. [DOI] [PubMed] [Google Scholar]
- 3.van Well GT, Paes BF, Terwee CB, et al. . Twenty years of pediatric tuberculous meningitis: a retrospective cohort study in the western cape of South Africa. Pediatrics 2009;123:e1–8. [DOI] [PubMed] [Google Scholar]
- 4.Yaramus A, Gurkan F, Elevli M, et al. . Central nervous system tuberculosis in children: a review of 214 cases. Pediatrics 1998;102:e49. [DOI] [PubMed] [Google Scholar]
- 5.Cag Y, Ozturk-Engin D, Gencer S, et al. . Hydrocephalus and vasculitis delay therapeutic responses in tuberculous meninigitis: results of haydarpasa-III study. Neurol India 2016;64:896–905. [DOI] [PubMed] [Google Scholar]