Abstract
OBJECTIVE:
Determine if two self-regulation interventions that reduced 3-year weight gain in young adults remain effective at 6 years.
METHODS:
Randomized trial in 2 academic settings in 599 young adults, age 18–35, normal weight or overweight; 504 (84%) re-consented for 6-year extension (SNAP-E) with ongoing intervention and assessments. Weight gain over 6 years was compared for all assigned to Control (C); Large Changes (LC; lose 5–10 pounds initially), and Small Changes (SC; make small daily changes in intake and activity).
RESULTS:
Weight change baseline to 6 years did not differ significantly among the 3 groups (C=3.9 kg, SC= 4.1 kg, and LC=2.8 kg). However, there was a significant age by treatment interaction, p=0.002. Among those <25 years, weight gain from baseline to 6 years averaged 7.3 kg and was reduced by almost 50% in LC and SC. LC also significantly reduced mean weight gain (area under the curve) over 6 years compared to C or SC.
CONCLUSIONS:
Although the interventions did not reduce weight gain at 6 years for the full cohort, they were effective in those age <25. Future efforts should focus on young adults age 18–24.9 and test more intensive interventions with more diverse participants.
Keywords: Weight gain, prevention, young adults, self-regulation
INTRODUCTION
Recently there has been increased attention to prevention of weight gain in young adults.1 This derives from the difficulties of producing sustained weight loss in individuals with obesity and recognition that the rate of weight gain is greatest at this time in life.2–4 Individuals aged 20–35 years experience weight gains of 1–2 pounds per year, with worsening cardiovascular risk factors in those who gain the most weight.5 There have been several studies designed to identify predictors of weight gain6–8 and to test interventions to reduce or prevent this weight gain.9 Frequently, these interventions have yielded positive short-term effects, but there are few studies with longer follow-up10–14 and most have been unsuccessful.15
We recently reported positive results from the Study of Novel Approaches to Weight Gain Prevention (SNAP), a randomized clinical trial in 599 young adults comparing two self-regulation interventions and a control on weight gain prevention over a mean follow-up of 3 years.16 Both self-regulation approaches involved frequent self-weighing; the Large Changes approach focused on losing 5–10 pounds during the first 4 months to provide a buffer against expected weight gains and the Small Changes approach taught participants to make small daily changes (approximately 100 calories) in both intake and activity. As previously reported,16 mean weight gains averaged across the 3 years of follow-up were 0.26 kg, −0.56 kg, and −2.37 kg in Control, Small Changes, and Large Changes, respectively, with significant differences among all three groups.
Given these positive results, SNAP was extended (SNAP-E) to test the hypothesis that there would be less weight gain from baseline to 6 years in both interventions than in the control group. To our knowledge, 6 years is the longest follow-up to date of a weight gain prevention intervention trial.
METHODS
Participants
SNAP was conducted at two clinical sites (University of North Carolina, Chapel Hill, NC; Miriam Hospital, Providence RI) with Wake Forest as the Coordinating Center. Eligibility criteria for SNAP have been described in detail16,17 and included aged 18–35 years with a BMI of 21.0 to 30.9. SNAP recruitment was via mailings and emails from August 2010-February 2012. After completing 4 years in SNAP, all participants (N=599) were invited to re-enroll in SNAP-E; 504 (84%) consented for SNAP-E. All three IRBs approved the initial study and extension.
Interventions
At the start of SNAP, subjects were randomly assigned to one of three treatment groups. Randomization was implemented through a web-based data management system, using variable block lengths, stratified by clinical site, sex, and race/ethnicity.16,17 The interventions have been described in detail elsewhere,16 and are briefly described here. Both interventions, Large and Small Changes, attended 10 meetings over the first 4 months (weekly for 8 weeks, then monthly). Using a self-regulation framework,18,19 both intervention groups were taught to weigh themselves frequently (daily weighing was recommended) and to use these weights to know when changes in diet and physical activity were needed. The Small Changes (SC) approach involved making daily changes of approximately 100 calories in intake. The Large Changes (LC) group was given calorie, fat, and activity goals to produce a 5–10-pound initial weight loss during the first 4 months to act as a buffer against expected weight gains. After the initial 4 months, participants in the intervention groups were instructed to report their weight weekly and to either reinforce themselves for remaining below baseline weight, be cautious if small weight gains occurred, or return to the Large or Small Change approaches if weight gains were > 5 lbs. The Control group (C) (referred to as the Self-guided group) attended 1 group session and was introduced to the two different approaches and encouraged to follow whichever seemed most appropriate.
After the first 4 months, all groups received quarterly newsletters, and the two intervention groups were sent monthly feedback related to their current color zone. Twice a year, participants in the two interventions groups were invited to participate in optional 4-week refresher programs, offered on-line, which encouraged return to the core principles of the Small or Large Changes approach.
Those who enrolled in SNAP-E were provided with Smart Scales (Body Trace eScales; BT-003) and Fit-Bits to encourage participation and allow remote data collection. In addition, all groups continued to receive newsletters and the two interventions were provided with quarterly feedback regarding their color zones and invited to two 4-week on-line refreshers each year similar to those during SNAP.16
Assessments
In SNAP, weights were measured by blinded assessors at in-clinic visits at 4 months and annually thereafter during years 1–4. Participants who had moved or were unwilling to come in to the clinic were sent a Smart Scale which automatically transmitted data to the clinic. During the extension (SNAP-E), weights were collected via Smart Scales at 4.5, 5.0, and 5.5 years and in the clinic at 6 years (or remotely for those who were not willing or had moved out-of-state). Because of the timing of the start of funding for the extension, only some participants could be approached for the 4.5 and 5-year assessments, whereas all could be approached for 5.5-year and 6-years. Height was assessed with a stadiometer at baseline and 6 years and used to calculate BMI.
Statistical Analysis
We examined whether there were differences in the characteristics at SNAP enrollment between participants who re-consented to extended follow-up compared with those who did not using chi-squared tests.
Analyses were guided by the statistical plan pre-specified in the SNAP-E protocol (Supplement 1). The primary outcome for SNAP-E was weight change from the SNAP baseline to Year 6, as estimated with a linear contrast from mixed effects models applied to weights at times corresponding to clinic visits: at 4 months and years 1, 2, 3, 4, and 6. Intent-to-treat analysis, including all initially-randomized participants, was used. Covariate adjustment was made for whether weights were obtained at clinics or via Smart Scales and for the stratification factors used in randomization: clinic site, gender, and race /ethnicity (Non-Hispanic White vs. others). Overall differences among the three treatment groups were assessed with two-tailed type 1 error set at 0.05; three linear contrasts comparing pairwise group differences (LC vs. C, SC vs. C, LC vs. SC) in the mean weight change from baseline to 6 years were used to compute 98.3% confidence intervals (Bonferroni-adjustment for the 3 comparisons) for mean differences. Sensitivity analyses were conducted including only those who consented to SNAP-E and using inverse probability weighting to gauge the impact of missing data. The N of 504, observed standard error, and Bonferroni adjustments provided 80% post-hoc power to detect mean pairwise differences of 1.6 kg for the primary outcome.
Pre-specified secondary analyses included weight gain averaged over the 6 years (referred to as “weight gain exposure”). This outcome was calculated using linear contrasts from a mixed effects model across all time points and summing the areas (both positive and negative) traced by the trajectory of means from 0 (or area under the curve; see Figure S1); positive values represented the accumulated exposure to weight gains over time. Area under the curve was used in preference to simply averaging across time-points in order to account for the difference in time intervals between the assessments (4 months, 1, 2, 3, 4, 4.5, 5.0, 5.5, 6.0 years). We conducted parallel analyses in which all SNAP participants were included and, separately, limited to SNAP-E participants. An additional pre-specified secondary outcome was the odds that participants transitioned to a greater weight class from baseline to 6 years, i.e. from normal weight to overweight or obesity or from overweight to obesity and an exploratory analysis of transitions to obesity. These analyses were limited to participants who had a BMI <30.0 kg/m2 at baseline, with BMI calculated at year 6 using the most recent measured height, and were based on logistic regression.
Three subgroup comparisons were pre-specified, based on gender, age (18–24.9; ≥25.0 −35), and BMI at SNAP enrollment. Interaction terms were used to assess whether intervention effects varied among subgroups.
RESULTS
Study Participants
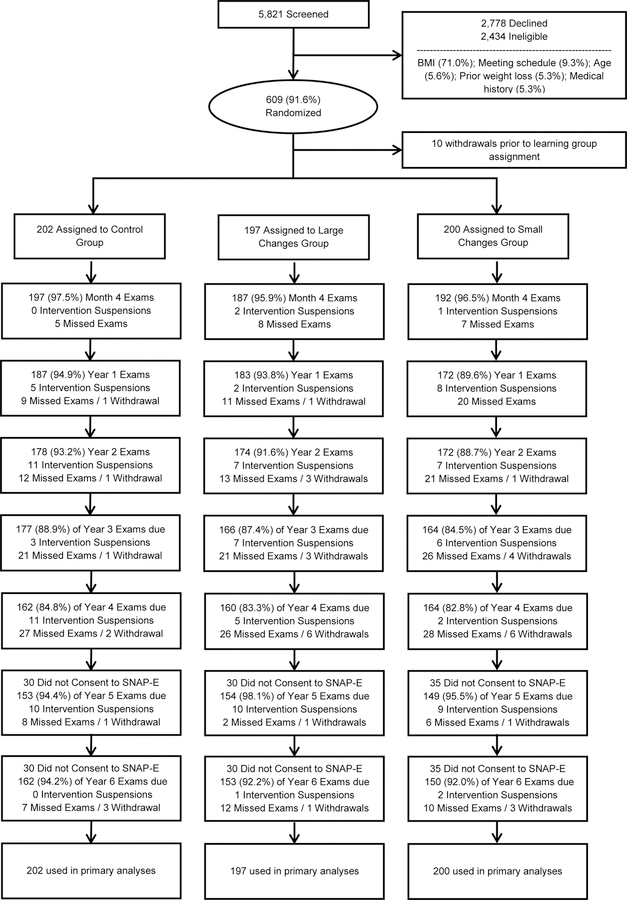
Table 1 shows that the 599 original SNAP participants and the 504 (84%) who re-consented for extended follow-up were similar at baseline (Table 1). Of note, the proportion of participants in the three conditions did not differ in SNAP-E vs SNAP. Figure 1 indicates the number who completed each of the clinic visits. Retention at 6 years was comparable across the 3 groups (92–94%), as were the proportion of weights collected remotely (24.1%, 24.2% and 27.2 % of C, LC, and SC; p=0.77).
Table 1:
Characteristics of the SNAP cohort at enrollment and at SNAP-E enrollment: N (%).
| Baseline Characteristic |
SNAP Enrollment N=599 |
SNAP-E Enrollment N=504 |
Differential Follow-up p-value |
|---|---|---|---|
| Age group, years 18.0 to 24.9 ≥ 25.0 to 35.0 |
169 (28.2%) 430 (71.8%) |
135 (26.8%) 369 (73.2%) |
0.07 |
| Body mass index 21 to < 25.0 ≥ 25.0 to 30 |
277 (46.2%) 322 (53.8%) |
229 (45.4%) 275 (54.6%) |
0.36 |
| Sex Females Males |
469 (78.3%) 130 (21.7%) |
390 (77.4%) 114 (22.6%) |
0.21 |
| Clinic site Chapel Hill, NC Providence, RI |
307 (51.2%) 292 (48.8%) |
264 (52.4%) 240 (47.6%) |
0.20 |
| Race/ethnicity African-American Non-Hispanic White Other |
66 (11.0%) 438 (73.1%) 95 (15.9%) |
51 (10.1%) 372 (73.8%) 81 (16.1%) |
0.27 |
| Intervention assignment Control (C) Large changes (LC) Small changes (SC) |
202 (33.7%) 197 (32.9%) 200 (33.4%) |
172 (34.1%) 167 (33.1%) 165 (32.7%) |
0.73 |
Figure 1:
Consort Diagram
Weight Changes
As seen in Table 2, differences among the intervention groups for the primary outcome of weight change from baseline to Year 6 were not statistically significant (p=0.11). Participants in the C group gained a mean (standard error) 3.92 (0.49) kg over the 6 years, whereas those in LC gained 2.80 (0.50) kg and SC participants gained 4.16 (0.49) kg. None of the pairwise comparisons were significant. Analyses including only those who consented to the extension and using inverse probability weighting provided similar results as did analyses using percent weight change (5.57% [0.67], 4.18 [0.69], 5.65% [0.68] for C, LC and SC, respectively; p=0.23).
Table 2:
Mean weight outcomes for participants in Control, Large Changes, and Small Changes with covariate adjustment for gender, race/ethnicity, clinic site, and mode of weight measurement (clinic-based or Smart Scale).
| Outcome | Intervention Assignment Mean (SE) |
Overall p-value |
Bonferroni-adjusted 95% confidence Interval | ||||
|---|---|---|---|---|---|---|---|
| Control | Large Changes |
Small Changes |
Large Changes minus/vs Control |
Small Changes minus/vs Control |
Large Changes minus/vs Small Changes |
||
| Primary Outcome: Weight changes from Baseline to 6 Years, kgs |
3.92 (0.49) | 2.80 (0.50) | 4.16 (0.49) | 0.11 | −1.12 (0.69) [−2.78,0.54] |
0.24 (0.69) [−1.41,1.90] |
−1.36 (0.69) [−3.03,0.305] |
| Primary Outcome (sensitivity) Weight changes Baseline to 6 Years, kgs: SNAP-E ppts. only |
3.78 (0.50) | 2.65 (0.51) | 4.32 (0.50) | 0.06 | −1.14 (0.71) [−2.84,0.57] |
0.54 (0.71) [−1.16,2.24] |
−1.67 (0.71) [−3.39,0.04] |
| Primary Outcome (sensitivity) Inverse probability weighting |
3.68 (0.48) | 2.69 (0.50) | 4.25 (0.49) | 0.08 | −0.99 (0.69) [−2.65,0.67 |
0.57 (0.69) [−1.09,2.23] |
−1.56 (0.70) [−3.23,0.11] |
| Secondary Outcome: Difference in weight exposure (AUC) over follow-up1 |
8.06 (2.12) | −0.53 (2.10) | 4.08 (2.10) | 0.003 | −8.59 (2.51) [−14.61,−2.57]* |
−3.98 (2.50) [−9.98,2.02] |
−4.61 (2.51) [−10.64,1.41] |
| Secondary Outcome: Difference in weight exposure (AUC) over follow-up1: SNAP-E ppts. only |
7.05 (2.24) | −1.54 (2.25) | 4.90 (2.25) | 0.004 | −8.59 (2.67) [−14.99,−2.19]* |
−2.15 (2.66) [−8.55,4.24] |
−6.44 (2.68) [−12.86,−0.01]* |
| Secondary Outcome: Transition to overweight or obesity at 6 yrs.2 |
31.0% | 26.5% | 27.7% | 0.66 | OR=0.80 [0.44,1.48] |
OR=0.84 [0.46,1.55] |
OR=0.95 [0.51,1.79] |
| Exploratory Outcome: Transition to obesity at 6 yrs |
19.0% | 14.6% | 27.7% | 0.46 | OR=0.73 [0.35,1.52] |
OR=1.04 [0.52,2.08] |
0.70 [0.33,1.47] |
Includes weight changes at 4 months, years 1, 2, 3, 4, 4.5, 5, 5.5, and 6 years; the metric for the outcome is kg-years.
Based on current height for in-clinic measures and most recent measured height for Smart Scale weights. Limited to non-obese participants at baseline
Bonferroni-adjusted 95% confidence interval excludes 0.
However, groups differed significantly for the secondary outcome of weight gain exposure (p=0.003) (Figure 2A). In analyses including all SNAP participants, this was largely driven by less weight gain exposure in LC vs C -- a mean difference of 8.59 kg-years of exposure; the Bonferroni-adjusted confidence interval for this difference excluded 0. In analyses limited to SNAP-E participants, differences among groups were also statistically significant (p=0.004), and in this analysis LC differed significantly from both SC and C. The secondary outcome of transition to a greater weight class at 6 years did not differ among groups (p=0.66) nor did the proportion who became obese ( p=0.46).
Figure 2:
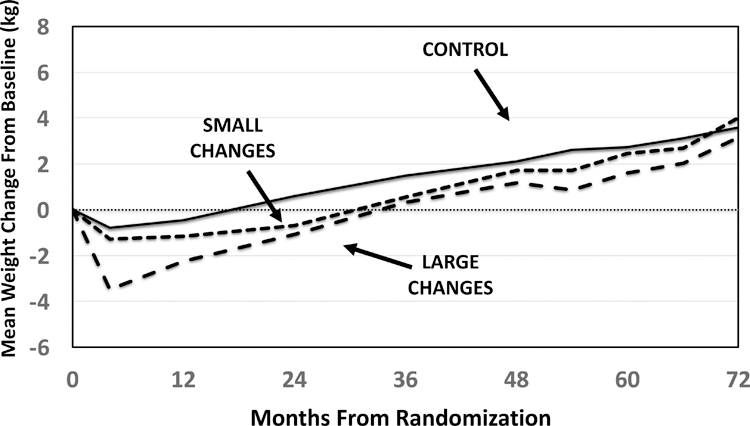
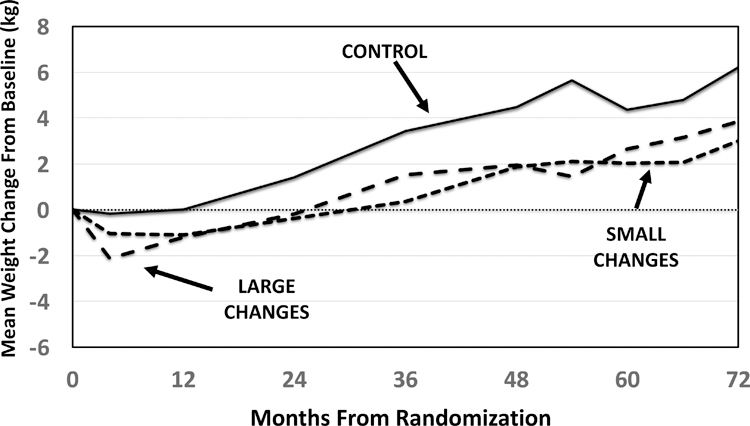
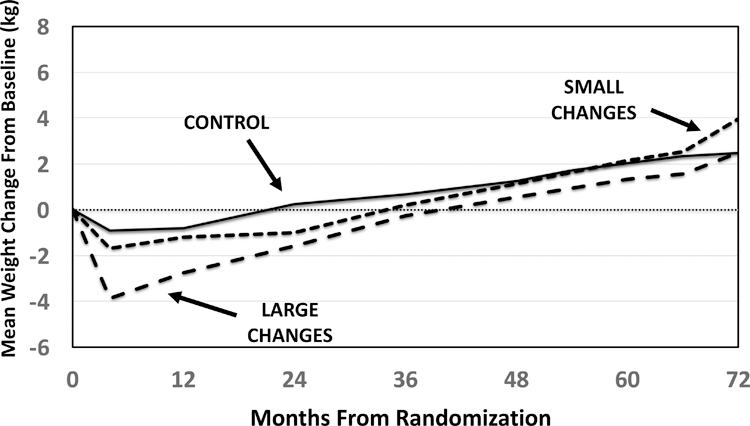
Mean changes in weight (kg) from baseline, adjusted for gender, race/ethnicity, clinic, and protocol. Primary Aim is based on changes from baseline to 6 years using assessments conducted at baseline, 4 months, 1,2,3,4 and 6 years. Secondary analysis of weight exposure (AUC) was calculated using all time points.
2A. Full Sample of participants
2B. Subgroup of participants ages 18–24.9 at baseline
2C. Subgroup of participants ages ≥25.0–35 at baseline
Subgroup analyses
We observed a significant interaction (p= 0.002) between participants’ age and treatment group for the primary outcome of weight change from baseline to Year 6 (Table 3). Figures 2B and 2C depict the weight at each assessment for participants grouped by age. Individuals aged 18–24.9 (Fig 2B) assigned to C (N=41) gained on average 7.30 kg over the 6 years, which differed significantly from similarly aged individuals in LC (N=48) or SC (n=46), who gained 3.86 and 3.18 kg respectively (p=0.008). Within older individuals (Fig 2C, the differences among treatment groups were also significant (p=0.026) with greater weight gain in SC (4.52 kg) than in LC or C (2.44 and 2.97 respectively).
Table 3:
Subgroup comparisons for the primary outcome (weight changes (kg) from baseline to 6 years) and the secondary outcome (weight exposure or AUC) for participants in Control, Large Changes and Small Changes with covariate adjustment for gender, race/ethnicity, clinic site, and mode of weight measurement (clinic-based or Smart Scale).
| Subgroup | Intervention Assignment Mean (SE) |
Overall p-value |
||
|---|---|---|---|---|
| Control | Large Changes | Small Changes | ||
|
Primary Outcome 18 – 24.9 years of age ≥ 25.0 −35 years of age Difference [95% CI] Females Males Difference [95% CI] Non-overweight Overweight Difference [95% CI] |
7.30 (1.02) 2.97 (0.55) 4.32 [1.55,7.09]* 3.79 (0.54) 4.66 (1.15) −0.87 [−3.92,2.19] 3.46 (0.71) 4.34 (0.67) −0.88 [−3.22,1.46] |
3.86 (1.01) 2.44 (0.57) 1.42 [−1.35,4.21] 3.14 (0.56) 1.63 (1.08) 1.51 [−1.40,4.43] 2.27 (0.71) 3.29 (0.69) −1.02 [−3.40,1.35] |
3.18 (0.95) 4.52 (0.57) −1.34 [−3.99,1.32] 3.79 (0.56) 5.39 (1.00) −1.60 [−4.35,1.15] 2.54 (0.76) 5.29 (0.64) −2.75 [−5.13,−0.37]* |
0.008 0.026 0.002** 0.631 0.029 0.156** 0.46 0.10 0.33** |
|
Secondary Outcome1 18–24.9 years of age ≥ 25.0 −35 years of age Difference [95% CI] Females Males Difference [95% CI] Non-overweight Overweight Difference [95% CI] |
15.47 (3.79) 5.43 (2.30) 10.04 [2.06,18.02]* 8.88 (2.17) 9.72 (4.08) −0.84 [−9.52,7.83] 4.98 (2.91) 11.11 (2.65) −6.14 [−13.20,0.92] |
6.95 (3.45) −3.68 (2.42) 10.64 [2.88,18.40]* 1.77 (2.19) −3.76 (3.90) 5.53 [−2.85,13.91] 0.07 (2.85) −0.87 (2.70) 0.95 [−6.15,8.05] |
4.71 (3.47) 3.63 (2.37) 1.08 [−6.51,8.68] 5.91 (2.18) 1.36 (3.99) 4.55 [−3.99,13.09] 3.84 (2.98) 4.40 (2.58) −0.56 [−7.65,6.53] |
0.06 0.005 0.15** 0.04 0.04 0.54** 0.37 0.003 0.33** |
Change in kilogram years over follow-up including weight changes at 4 months, years 1, 2, 3, 4, 4.5, 5, 5.5, and 6 years
95% confidence interval excludes 0
Interaction p-value
The interaction between age and treatment arm was not statistically significant for the secondary outcome of weight gain exposure (p=0.15) but the pattern paralleled that seen for the primary outcome (Table 3). Younger individuals had the greatest weight gain exposure when assigned to C (15.5, 6.9 and 4.7 kg years for C, LC, and SC respectively, p=0.06). Among older individuals, those assigned to the LC condition averaged below their baseline across the 6 years (−3.68 kg years), whereas those in SC or C averaged above their baseline weights (3.63, and 5.43, respectively), with the difference among the three significant at p=0.005. The interaction between age and treatment condition was not significant for the proportion that transitioned to a higher BMI category.
Although formal tests for interactions of treatment group with gender and baseline weight did not reach statistical significance, weight gain exposure for males and participants who were overweight at baseline was greatest in C and lowest in LC.
DISCUSSION
In contrast to our primary hypothesis, we found no significant differences in weight gain from baseline to 6 years among the three groups. However, the secondary outcome of weight gain exposure differed significantly among the three groups: the Large Changes approach, which taught young adults to lose 5–10 pounds to buffer the expected subsequent weight gains, was effective in reducing weight gain exposure over the 6 years relative to the Control group. Moreover, for those who entered SNAP-E, the Large Changes approach reduced weight gain exposure relative to both the Control and the Small Changes intervention.
Second, there was a significant age by treatment group interaction for the primary outcome of 6-year weight change from baseline. This resulted primarily from differences within the younger participants (age 18–24.9): those in the Control group gained 7.3 kg over the 6 years, or more than 1kg/year and both the Large Changes and Small Changes self-regulation interventions were effective in reducing the average weight gained over 6 years by over 50% relative to the Control group. In the older participants, weight changes from baseline to 6 years were greatest in Small Changes.
Weight gain is an important health problem for young adults, with 98% of men and 92% of women experiencing upward sloping weight trajectories over an 18-year follow-up.20 Weight gain in this age group has stronger associations with critical outcomes such as cancer risk and mortality than weight gain at other ages.21,22 Moreover, young adults who experience early or rapid weight gain are most likely to be on a steeper long-term weight gain trajectory;20 which is associated with greater likelihood of reporting hypertension, diabetes, and arthritis in middle age. Thus, the finding that those in the Control group who are age 18–24.9 gained more than 1 kg per year is of concern and strengthens the argument for weight gain prevention approaches in this age group. Moreover, evidence that the Large Changes intervention delayed weight gain initially and reduced weight gain exposure over 6 years suggests that this approach may yield positive health benefits longer term. Weight gain exposure, like pack years in smoking or obese-years23 provides a measure of cumulative exposure to the risk factor. Such measures are used frequently in long-term observational studies such as Framingham Heart Health Study and the Bogalusa Heart Study 24,25 because they can capture the cumulative damage of these conditions on health outcomes.
The results presented here extend prior findings from SNAP. The primary outcome in SNAP was weight gain exposure over an average of three years, which differed significantly among the three treatment groups as did the secondary outcomes of weight change from baseline to 2 years (the last time point reached by all cohorts) and the proportion that transitioned to obesity.16 At 6 years in the current analyses, weight gain from baseline no longer differs significantly among groups, suggesting that the intensity of the intervention may not have been sufficient to prevent weight gain in later years. In contrast, weight gain exposure continued to differ significantly. Over the 6 years of follow-up, Large Changes had a negative exposure to obesity, indicating that their trajectory of weight changes over the 6 years averaged below their baseline level. The beneficial effects of Large Changes on weight gain exposure occurred as the result of the 3.5 kg weight loss at 1 year; subsequently all three groups gained weight, and the difference among groups narrowed. Given the long-term effects of creating the initial buffer in Large Changes, future efforts at weight gain prevention should consider the possibility of periodically (e.g. on an annual basis) encouraging participants to lose 5–10 pounds to reinstate the buffer. Thus far in SNAP we have found no negative effects of creating an initial weight loss buffer,26,27 although future studies should continue to evaluate positive and potential negative effects of this strategy.
As noted above, we found evidence of important differences among subgroups. For both the primary and secondary outcomes, younger individuals who were assigned to the Control group, and thus received very limited intervention, gained the greatest amount of weight and had the greatest exposure to weight gain over the 6 years. Previous studies focusing on emerging adults (i.e. those age 18–25) confirm their large weight gains over time and note their poor outcomes in weight loss trials.28–31 Only 25% of the participants entering SNAP were in the younger age group and there was a trend (p=0.07) for poorer retention rates in this age group. In addition, among those who were older or heavier at baseline, and among males, the Large Changes intervention led to negative levels of weight gain exposure (i.e., the average weight for these subgroups over 6 years was below their baseline weight). In all other subgroups, weight gain exposure was greater than zero. These results suggest that those who were already overweight at baseline or older may particularly benefit from an approach focused on modest weight losses.
Strengths of this study include the large sample size, excellent retention, and extended follow-up. Given the mobility of this population, our intervention was delivered primarily via on-line methods in out-years. Smart Scales allowed us to capture frequent weight data and maintain high levels of retention. We and others have demonstrated the validity of Smart Scale weights in intervention trials.32,33 This study is limited, however, by concerns about the generalizability of findings. All participants had joined SNAP, a trial which specifically focused on weight gain prevention; moreover, the sample had limited diversity (73% were nonHispanic white and 78% were female) and was recruited at only two geographic areas. Future studies should include more men, racial/ethnic minorities, and more geographic diversity. In addition, the provision of scales and activity trackers (i.e. self-monitoring tools) could have affected the weight changes seen in SNAP-E.
In conclusion, there were no significant effects of the interventions on weight gain from baseline to 6 years. However, relative to Control, the Large Changes approach, in which participants are encouraged to lose weight initially to buffer expected weight gain, was effective in reducing weight gain exposure over 6 years. Future studies should consider this approach particularly for those who are already overweight and examine the efficacy of intermittently encouraging participants to lose small amounts of weight to create this buffer. In addition, our findings strengthen the imperative to develop weight gain prevention interventions for young adults, aged 18–25. Without such interventions, this group is at high risk of weight gain and future weight-related health problems. The two interventions tested here were both effective in reducing the amount of weight gained over 6 years in this subgroup and should receive further study.
Supplementary Material
Supplementary Figure 1: Example of Approach Used to Calculate Area-Under-the-Curve (AUC)
What is already known about this subject:
Young adults are the age group at greatest risk of significant weight gain.
Interventions to prevent weight gain are often effective initially, but few have documented benefits at 2 years or longer.
We previously tested two self-regulation interventions: Large Changes, which taught participants to lose 5–10 pounds initially to create a weight gain buffer, and Small Changes, which stressed small daily changes in intake and activity, and reported that both interventions significantly reduced weight gain in young adults, relative to a control condition, over a mean follow-up of 3 years.
What does this study add:
This study examined whether the effects of the two self-regulation interventions on weight gain prevention in young adults were still seen at 6 years.
Weight changes from baseline to 6 years did not differ significantly among groups. However, relative to the control condition, both interventions significantly decreased weight gain in the subgroup of participants age 18 to 24.9 at baseline.
This study suggests that those age 18 to 24.9 are especially vulnerable to weight gain, but this weight gain can be significantly reduced through self-regulation interventions.
Acknowledgements:
Data Sharing Plan
All de-identified data collected during the trial will be available from the NHLBI Data Repository (https://biolincc.nhlbi.nih.gov/home/) by January 2020. This will include the data, data dictionary, and informed consent documents. Data will be made available to others according to NHLBI policies which will determine the types of analyses and with whom the data will be shared.
The Study of Novel Approaches to Weight Gain Prevention (SNAP) Research Group members (listed alphabetically by site unless otherwise specified):
Miriam Hospital/Brown Medical School: Rena R. Wing, PhD (principal investigator); Elissa Jelalian, PhD (co-investigator); Erica Ferguson Robichaud, MSW, RD (program coordinator); Jose DaCruz; Kaitlyn Dahlborg, BS; Caitlin Egan, MS; Denise Fernandes Pierre, BS; Chelsea Pimentel, BA; Wilza Rodrigues, BS; Samantha Williams, MSc.
University of North Carolina at Chapel Hill: Deborah Tate, PhD (principal investigator); Kristen Polzien, PhD (program coordinator); Candice Alick, MS; Loneke Blackman, MS, RD; Molly Diamond, MPH; Karen E. Hatley, MPH; Brett Meager; Julianne Power, MS; Brooke Tompkins Nezami, MA; Paige Trexler; Carmina Valle, PhD, MPH.
Wake Forest School of Medicine: Mark A. Espeland, PhD (principal investigator); Judy L. Bahnson, BA, CCRP (co-investigator); Letitia H. Perdue, MS (program coordinator); Cheryl Bentley; Patty Davis, BS; Katelyn Garcia, MS; Rebecca H. Neiberg, MS; Julia Robertson, BS; Greg Russell, MS.
Consultant co-investigators were Cora E. Lewis, MD, MSPH, University of Alabama at Birmingham; Amy Gorin, PhD, University of Connecticut; Jessica G. LaRose, PhD, Virginia Commonwealth University School of Medicine.
Funding: National Institutes of Health grants U01HL090864, U01HL090875 and 5R01HL127341.
Disclosures: Dr. Tate serves on the Scientific Advisory board and receives grant funding from WW.
Footnotes
Trial Registration: clinicaltrials.gov Identifier:
REFERENCES
- 1.Lytle LA, Svetkey LP, Patrick K, et al. The EARLY trials: a consortium of studies targeting weight control in young adults. Transl Behav Med. 2014;4(3):304–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Williamson DF, Kahn HS, Remington PL, Anda RF. The 10-year incidence of overweight and major weight gain in US adults. Arch Intern Med. 1990;150(3):665–672. [PubMed] [Google Scholar]
- 3.Ball K, Crawford D, Ireland P, Hodge A. Patterns and demographic predictors of 5-year weight change in a multi-ethnic cohort of men and women in Australia. Public Health Nutr. 2003;6(3):269–281. [DOI] [PubMed] [Google Scholar]
- 4.Reas DL, Nygard JF, Svensson E, Sorensen T, Sandanger I. Changes in body mass index by age, gender, and socio-economic status among a cohort of Norwegian men and women (1990–2001). BMC Public Health. 2007;7:269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Truesdale KP, Stevens J, Lewis CE, Schreiner PJ, Loria CM, Cai J. Changes in risk factors for cardiovascular disease by baseline weight status in young adults who maintain or gain weight over 15 years: the CARDIA study. Int J Obes (Lond). 2006;30(9):1397–1407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ball K, Crawford D. An investigation of psychological, social and environmental correlates of obesity and weight gain in young women. Int J Obes (Lond). 2006;30(8):1240–1249. [DOI] [PubMed] [Google Scholar]
- 7.Viner RM, Cole TJ. Who changes body mass between adolescence and adulthood? Factors predicting change in BMI between 16 year and 30 years in the 1970 British Birth Cohort. Int J Obes (Lond). 2006;30(9):1368–1374. [DOI] [PubMed] [Google Scholar]
- 8.Pereira MA, Kartashov AI, Ebbeling CB, et al. Fast-food habits, weight gain, and insulin resistance (the CARDIA study): 15-year prospective analysis. Lancet. 2005;365(9453):36–42. [DOI] [PubMed] [Google Scholar]
- 9.Hebden L, Chey T, Allman-Farinelli M. Lifestyle intervention for preventing weight gain in young adults: a systematic review and meta-analysis of RCTs. Obes Rev. 2012;13(8):692–710. [DOI] [PubMed] [Google Scholar]
- 10.Hivert MF, Langlois MF, Berard P, Cuerrier JP, Carpentier AC. Prevention of weight gain in young adults through a seminar-based intervention program. Int J Obes (Lond). 2007;31(8):1262–1269. [DOI] [PubMed] [Google Scholar]
- 11.Jeffery RW, French SA. Preventing weight gain in adults: the pound of prevention study. Am J Public Health. 1999;89(5):747–751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Levine MD, Klem ML, Kalarchian MA, et al. Weight gain prevention among women. Obesity (Silver Spring). 2007;15(5):1267–1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lytle LA, Laska MN, Linde JA, et al. Weight-Gain Reduction Among 2-Year College Students: The CHOICES RCT. Am J Prev Med. 2017;52(2):183–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stice E, Marti CN, Spoor S, Presnell K, Shaw H. Dissonance and healthy weight eating disorder prevention programs: long-term effects from a randomized efficacy trial. J Consult Clin Psychol. 2008;76(2):329–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Partridge SR, Juan SJ, McGeechan K, Bauman A, Allman-Farinelli M. Poor quality of external validity reporting limits generalizability of overweight and/or obesity lifestyle prevention interventions in young adults: a systematic review. Obes Rev. 2015;16(1):13–31. [DOI] [PubMed] [Google Scholar]
- 16.Wing RR, Tate DF, Espeland MA, et al. Innovative self-regulation strategies to reduce weight gain in young adults: the study of novel appproaches to weight gain prevention (SNAP) randomized clinical trial. JAMA Intern Med. 2016;176(6):755–762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wing RR, Tate D, Espeland M, et al. Weight gain prevention in young adults: design of the study of novel approaches to weight gain prevention (SNAP) randomized controlled trial. BMC Public Health. 2013;13(1):300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.FH K. Self-management methods In: Kanfer FH, Goldstein AP, eds. Helping People Change: A Textbook of Methods. 1991;4th ed. New York, NY: Allyn & Bacon;:309–355. [Google Scholar]
- 19.Carver CS, Scheier MF. Principles of Feedback Control In: Carver CS, Scheier MF, eds. On the Self-Regulation of Behavior. Cambridge: Cambridge University Press; 1998:10–28. [Google Scholar]
- 20.Malhotra R, Østbye T, Riley CM, Finkelstein EA. Young adult weight trajectories through midlife by body mass category. Obesity. 2013;21(9):1923–1934. [DOI] [PubMed] [Google Scholar]
- 21.Renehan AG, Flood A, Adams KF, et al. Body mass index at different adult ages, weight change, and colorectal cancer risk in the National Institutes of Health-AARP Cohort. Am J Epidemiol. 2012;176(12):1130–1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Adams KF, Leitzmann MF, Ballard-Barbash R, et al. Body mass and weight change in adults in relation to mortality risk. Am J Epidemiol. 2014;179(2):135–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Abdullah A, Amin FA, Stoelwinder J, et al. Estimating the risk of cardiovascular disease using an obese-years metric. BMJ open. 2014;4(9):e005629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Felson DT, Anderson JJ, Naimark A, Walker AM, Meenan RF. Obesity and knee osteoarthritis: the Framingham Study. Annals of internal medicine. 1988;109(1):18–24. [DOI] [PubMed] [Google Scholar]
- 25.Lai C-C, Sun D, Cen R, et al. Impact of long-term burden of excessive adiposity and elevated blood pressure from childhood on adulthood left ventricular remodeling patterns: the Bogalusa Heart Study. Journal of the American College of Cardiology. 2014;64(15):1580–1587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wing RR, Tate DF, Garcia KR, Bahnson J, Lewis CE, Espeland MA. Improvements in cardiovascular risk factors in young adults in a randomized trial of approaches to weight gain prevention. Obesity (Silver Spring). 2017. [DOI] [PMC free article] [PubMed]
- 27.Gorin AA, Gokee LaRose J, Espeland MA, et al. Eating pathology and psychological outcomes in young adults in self-regulation interventions using daily self-weighing. Health Psychology. 2019;38(2):143–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Burke GL, Bild DE, Hilner JE, Folsom AR, Wagenknecht LE, Sidney S. Differences in weight gain in relation to race, gender, age and education in young adults: the CARDIA Study. Coronary Artery Risk Development in Young Adults. Ethn Health. 1996;1(4):327–335. [DOI] [PubMed] [Google Scholar]
- 29.Nelson MC, Story M, Larson NI, Neumark-Sztainer D, Lytle LA. Emerging adulthood and college-aged youth: an overlooked age for weight-related behavior change. Obesity (Silver Spring). 2008;16(10):2205–2211. [DOI] [PubMed] [Google Scholar]
- 30.Gokee-LaRose J, Gorin AA, Raynor HA, et al. Are standard behavioral weight loss programs effective for young adults? Int J Obes (Lond). 2009;33(12):1374–1380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.LaRose JG, Tate DF, Lanoye A, et al. Adapting evidence-based behavioral weight loss programs for emerging adults: A pilot randomized controlled trial. J Health Psychol. 2017:1359105316688951. [DOI] [PMC free article] [PubMed]
- 32.Ross KM, Eastman A, Wing RR. Accuracy of self-report versus objective smart-scale weights during 12-week weight management intervention. Obesity. 2019. [DOI] [PMC free article] [PubMed]
- 33.Ross KM, Wing RR. Concordance of in-home ‘smart’scale measurement with body weight measured in-person. Obesity science & practice. 2016;2(2):224–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Figure 1: Example of Approach Used to Calculate Area-Under-the-Curve (AUC)