Abstract
Despite high cure rates in children, acute lymphoblastic leukemia (ALL) remains a leading cause of cancer death in the young, and the likelihood of treatment failure increases with age. With the exception of tyrosine kinase inhibitors, there have been few advances in repurposing or developing new therapeutic approaches tailored to vulnerabilities of ALL subtypes or individual cases. Large-scale genome profiling studies conducted over the last decade promise to improve ALL outcomes by refining risk stratification and modulation of therapeutic intensity, and by identifying new targets and pathways for immunotherapy. Many of these approaches have been validated in preclinical models and now merit testing in clinical trials. This review discusses the advances in our understanding of the genomic taxonomy and ontogeny of B-progenitor ALL, with an emphasis on those discoveries of clinical importance.
Keywords: acute lymphoblastic leukemia, ALL, ALL subtype, B-progenitor ALL, B-ALL, DUX4, ETV6-RUNX1, genome profiling, hypodiploid, IGH, IKZF1, MEF2D, NUTM1, PAX5, Ph-like, taxonomy, ZNF384
Introduction
Cure rates for B-precursor acute lymphoblastic leukemia (B-ALL) now exceed 90% in children treated with optimal, risk-adapted therapy [1]. This contrasts with the prognosis in older children and adults, where cure rates decline sharply to less than 50% in adults over the age of 40 [2]. Previously, genetic alterations identified by chromosomal karyotyping, fluorescence in situ hybridization, and identification of common fusion gene transcripts have been used to identify good-risk (eg, high hyperdiploidy and ETV6-RUNX1 rearrangement) and poor-risk (KMT2A rearrangement, BCR-ABL1, and hypodiploidy) subsets of childhood ALL [3]. The repertoire of leukemia-driving and subtype-defining genetic alterations in adult ALL has been far less well understood, and treatment typically determined by the presence or absence of BCR-ABL1.
The last decade has witnessed major advances in the use of genomic approaches to identify leukemia subtypes and the constellations of inherited and somatic genomic alterations that characterize each, as well as the nature of genetic variegation that underlies clonal heterogeneity and disease progression in the setting of treatment failure and relapse [4–6]. These studies have been notable for (1) initial characterization of ALL in children, but with an increasing focus on the disease in adults; (2) progressively increased comprehensiveness of analysis, initially using single nucleotide polymorphism (SNP) microarrays to characterize DNA copy number alterations (CNAs) and copy-neutral loss of heterozygosity (LOH) [7, 8] to whole exome (WES), transcriptome (WTS), and genome (WGS) sequencing approaches; and (3) analysis of large cohorts of cases across the age spectrum. These studies have been performed in both B-progenitor and T-lineage ALL [9], but it is in B-ALL, where a greater proportion of cases have previously lacked known drivers, that these studies have been most informative.
A revised taxonomy of B-ALL
Previously established subtypes of B-ALL include aneuploidy (high hyperdiploidy, low hypodiploidy, and near haploidy), complex chromosomal rearrangements (intrachromsomal amplification of chromosome 21, iAMP21), and rearrangements that deregulate oncogenes or result in the expression of chimeric fusion oncoproteins (eg, ETV6-RUNX1, KMT2A rearrangement, TCF3-PBX1, and BCR-ABL1) [3]. Conventional cytogenetic and molecular analyses fail to identify clonal driver alterations in approximately 25% of ALL in children and the majority of cases in adults. These clonal, subtype-defining chromosomal alterations are typically associated with distinct leukemic gene expression profiles upon microarray or WTS-based gene expression profiling. As WTS may characterize both gene rearrangements and gene expression, this platform has been increasingly used to profile ALL in children and adults to identify new subtypes and their drivers.
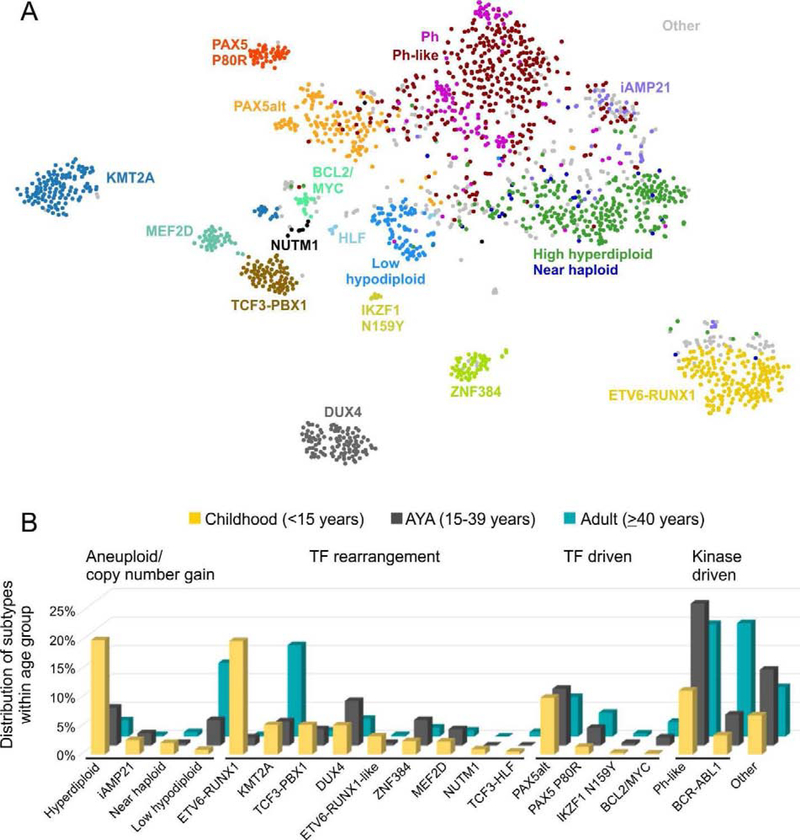
In an analysis of 1988 ALL cases, approximately two thirds from children (enrolled on St Jude Total Therapy and Children’s Oncology Group studies) and one third from adults (treated on protocols of the Alliance-CALGB, ACRIN - Eastern Cooperative Oncology Group, MD Anderson Cancer Center, and Southwest Oncology Group), WTS was used in all cases to identify gene expression profiles, aneuploidy, sequence mutations and chromosomal rearrangements [10]. Multiple algorithms were used to cluster cases according to leukemia gene expression profile. This confirmed and expanded recent studies identifying new subtypes: 23 were identified with significant variation in prevalence according to age stratum (children <16, adolescent and young adult (16–39), and older adult (>39 years of age at diagnosis) (Table 1 and Figure 1). These new subtypes were not identified by prior chromosomal analysis for several reasons: (1) rearrangements were cryptic on karyotyping; (2) some subtypes were defined by diverse rearrangements to a single partner gene (eg, MEF2D, ZNF384, and NUTM1-rearranged ALL); (3) several subtypes are driven by sequence mutations of transcription factors (eg, PAX5 P80R and IKZF1 N159Y), or (4) subtypes may have diverse alterations within a single group (eg, PAX5alt, or “PAX5 altered” that comprises PAX5 rearrangements, sequence mutations, and structural variants; and Ph-like ALL).
Table 1.
Prevalence and prognosis of subtypes in B-ALL
| ALL subtype | Category | Median age (yrs) | Peak prevalence | Genomic alterations | Clinical features | Therapy | References |
|---|---|---|---|---|---|---|---|
| Hyperdiploid (>50 chromosomes) | Aneuploid | 4 | Children (25%) | Ras pathway Epigenetic modifiers | Excellent prognosis | Reduce intensity | [60] |
| Low hypodiploid (31–39 chromosomes) | Aneuploid | 47 | Adults (10–15%) | IKZF2 del, TP53 mut (commonly inherited) | Poor prognosis | BCL2 inhibitors | [61] |
| Near haploid (24–30 chromosomes) | Aneuploid | 5.4 | <3% in all ages | Ras pathway, IKZF3 del | Intermediate prognosis | BCL2 inhibitors | [61] |
| iAMP21 | Copy number gain | 10 | ∼3% in children and AYA | Complex structural alterations of chromosome 21 | Good prognosis with intensive therapy, low WBC | [62] | |
| ETV6-RUNX1 t(12;21)(p13;q22) | TF rearrangement | 4 | Children (25%) | PAX5 del, WHSC1 mut | Excellent prognosis | Reduce intensity | [7, 63] |
| ETV6-RUNX1-like | TF rearrangement | 3 | Children (3%) | ETV6 fusions and del, IKZF1 fusions and del | Unknown | Reduce intensity | [42, 43] |
| DUX4-rearranged | TF rearrangement | 14.3 | AYA (∼8%) | ERG del, IKZF1 del, Ras pathway | Excellent prognosis | Reduce intensity | [18, 42, 44] |
| KMT2A-rearranged | TF rearrangement | 40 | Infants (∼90%) and adults (∼15%) | Ras pathway (commonly subclonal) | Poor prognosis | Bortezomib, DOT1L, Menin inhibition | [64] |
| TCF3-PBX1 t(1;19)(q23;p13) | TF rearrangement | 8 | Children (5%) | Good prognosis, CNS relapse | [65, 66] | ||
| ZNF384-rearranged | TF rearrangement | 15 | AYA (∼5%) | Epigenetic modifiers, Ras pathway | Intermediate prognosis | FLT3 inhibition | [12, 17, 18] |
| MEF2D-rearranged | TF rearrangement | 14 | AYA (∼7%) | Ras pathway | Intermediate prognosis, | HDAC inhibition | [11, 13] |
| NUTM1-rearranged | TF rearrangement | 3 | Children (1%) | Unknown | Excellent prognosis | Bromodomain inhibitors | [10, 22] |
| TCF3-HLF t(17;19)(q22;p13) | TF rearrangement | 15 | Rare rare in all ages (<1%) | TCF3 mut, PAX5 del, | Very poor prognosis, Ras pathway | BCL2 inhibitors | [67] |
| PAX5alt | Other TF driven | 10 | Children (∼11%) | PAX5 fusion, mut, amp | Intermediate prognosis | [10, 22] | |
| PAX5 P80R | Other TF driven | 22 | Adults (∼4%) | Ras pathway | Intermediate prognosis | [10, 22] | |
| IKZF1 N159Y | Other TF driven | Rare in all ages (<1%) | Unknown | Unknown | FAK inhibitors, rexinoids | [10, 22] | |
| BCL2/MYC-rearranged | Other TF driven | 48 | AYA and adults (∼3%) | Unknown | Poor prognosis | [10] | |
| Ph-like | Kinase driven | 21 | AYA (25–30%) | Multiple kinase alterations, IKZF1 del and mut, CDKN2A/B del | Poor prognosis, amenable to TKI therapy | TKI, PI3Ki, BCL2 inhibitors | [15, 26] |
| BCR-ABL1 t(9;22)(q34;q11.2) | Kinase driven | 40–45 | Adults (40–50%) | IKZF1 del and mut, CDKN2A/B del | Prognosis improved with TKI | TKI, FAK inhibitors, rexinoids | [15, 26, 68] |
| Other | 16 | ∼5% children, ∼10% AYA and adults | Unknown | Intermediate prognosis |
AYA, adolescent and young adult; amp, amplification; B-ALL, B-progenitor acute lymphoblastic leukemia; del, deletion; mut, sequence mutation; TF, transcription factor; TKI, tyrosine kinase inhibitor.
Figure 1.
(A) Major B-ALL subtypes based on gene expression profiling of 1988 cases. (B) Distribution of B-ALL subtypes within each age group. Subtypes are grouped as gross chromosomal abnormalities (aneuploidy or copy number gain), transcription factor (TF) rearrangement, other TF-driven, kinase-driven, and all others [10].
Although it is well established that several subtypes are associated with age (eg, high hyperdiploid and ETV6-RUNX1 ALL in children, and BCR-ABL1 and Ph-like ALL in the adolescent-young adult [AYA] and older adult population), this analysis also demonstrated additional associations with age: older adult ALL has a more restricted range of subtypes, the most common being low hypodiploid ALL, KMT2A-rearranged and kinase driven (BCR-ABL1+ and Ph-like ALL). In addition, many cases previously categorized as “B-other” harbored founding PAX5 alterations, more commonly PAX5alt in children and older adults, and PAX5 P80R in older adults. An additional group was identified with double or triple hit alterations in BCL2, MYC, and/or BCL6, lesions also observed in a subset of aggressive diffuse large cell lymphoma.
Many of these subtypes showed significant associations with event-free or overall survival in both children and adults. These associations were particularly striking in adults, where few alterations associated with favorable prognosis have previously been identified. Rearrangement of the double homeobox gene DUX4 was associated with the most favorable outcome in both children and adults, PAX5 P80R with intermediate outcome, PAX5alt with unfavorable outcome, and kinase-driven leukemia, KMT2A-rearrangemed and BCL2/MYC-rearranged leukemia with dismal outcome in adults. Thus, these data indicate the importance of accurate identification of ALL subtype at diagnosis to guide therapeutic intensification and, for good-risk subtypes, potential avoidance of intensive, toxic regimens such as allogeneic stem cell transplantation. A comprehensive review of the genetics and biology of each subtype is beyond the scope of this manuscript, but newly described entities with therapeutic implications are described below.
MEF2D-rearranged ALL
Recurrent rearrangements of MEF2D occur in approximately 4% of children and 7% of AYA patients, and is associated with older age of onset (median 14 years) and intermediate to poor outcome [11–13]. The rearrangements result in expression of chimeric fusion oncoproteins with MEF2D (myocyte enhancer factor 2D) at the N-terminus fused to BCL9 (most commonly), CSF1R, DAZAP1, FOXJ2, HNRNPUL1, HNRNPH1, and SS18 [11, 13, 14]. MEF2D-CSF1R is exceptional for being observed in Ph-like ALL rather than the other MEF2D fusions that have a distinct gene expression profile [15]. The immunophenotype of MEF2D ALL is notable for CD10 negativity and CD38 positivity. The fusions retain the DNA binding of MEF2D, and in vitro, result in transcriptional activation of known MEF2D targets such as HDAC9 and hematopoietic cell transformation [11]. The deregulation of HDAC9 results in a therapeutic vulnerability, as patient-derived leukemic cells are exquisitely sensitive to histone deacetylase inhibitors such as panobinostat [11].
ZNF384-rearranged leukemia
Rearrangements of ZNF384 (zinc finger 384) define a subtype of leukemia that may be diagnosed as pre-B ALL (with or without aberrant expression of myeloid antigens) or B/myeloid mixed phenotype acute leukemia [16]. The secondary genomic alterations and gene expression profiles of ZNF384-rearranged B-ALL and B/myeloid mixed phenotype acute leukemia (MPAL) are essentially indistinguishable, suggesting that the presence of the ZNF384 should be considered the hallmark, and diagnostic criterion, for this form of leukemia rather than initially stratifying patients by immunophenotype into B-ALL or MPAL. In B-ALL, ZNF384 rearrangements are observed in 5% of childhood and 10% of AYA cases and are associated with intermediate outcome. The fusions involve a range of N-terminal fusion partners, often transcriptional regulators or chromatin modifying genes fused to ZNF384 (ARIDIB, BMP2K, CLTC, CREBBP, EP300, EWSR1, NIPBL, SMARCA2, SYNRG, TAF15, and TCF3) [12, 17–19]. The majority of the fusions involve rearrangement of the entire coding region of ZNF384, resulting in the expression of both the wild-type protein and fusion chimera. Several observations suggest that the immunophenotypic aberrancy and frequent immunophenotypic multiclonality arises from inherent lineage plasticity: (1) the lack of variability of secondary mutations between immunophenotypic subclones; (2) the ability of flow-sorted immunophenotypic subpopulations to reconstitute the diversity of the primary tumor in immunocompromised mice; and (3) detection of founding lesions in MPAL such as ZNF384 rearrangement or WT1 mutation in a subset of hematopoietic stem cells [16]. Detection of this fusion has several clinical and therapeutic implications. There is a compelling genomic rationale that all ZNF384-rearranged cases should be managed in a uniform fashion, rather than using myeloid or lymphoid leukemia-directed therapy according to predominant lineage. ZNF384-rearranged leukemia is characterized by overexpression of (non-mutated) FLT3, and anecdotal reports have shown remarkable responsiveness of refractory EP300-ZNF384 leukemia to the kinase inhibitor sunitinib [20]. Finally, the inherent lineage plasticity of ZNF384-rearranged leukemia is evident under selective pressure of conventional therapy, in which lymphoid disease may recur as myeloid disease and vice versa, with preservation of the founding fusions, and thus should not be mistaken for secondary leukemia. Similarly, chimeric antigen receptor (CAR) T-cell therapy may result in lineage drift or switch to myeloid disease [21].
Recent studies have identified ALL cases with alternate fusions that result in a similar gene expression profile: rearrangement of the zinc finger ZNF362 to SMARCA2 and TAF15 [22]. It is not yet known if such cases also result in lineage aberrancy or potential vulnerability to FLT3 inhibition.
Ph-like ALL
Ph-like, or BCR-ABL1-like ALL is characterized by a leukemic cell transcriptional profile similar to Ph+ ALL but lack the BCR-ABL1 fusion gene [23, 24], and is one of the few recently described subtypes of ALL now incorporated into the 2016 revision of the World Health Classification of acute leukemia [25]. The incidence of Ph-like ALL increases with age, from 10%−15% of ALL in children, rising to 30% in young adults [15, 26–31]. Ph-like ALL is consistently associated with unfavorable outcomes, including elevated measurable residual disease (MRD) levels and/or higher rates of treatment failure compared to non Ph-like ALL patients [15, 26, 32, 33].
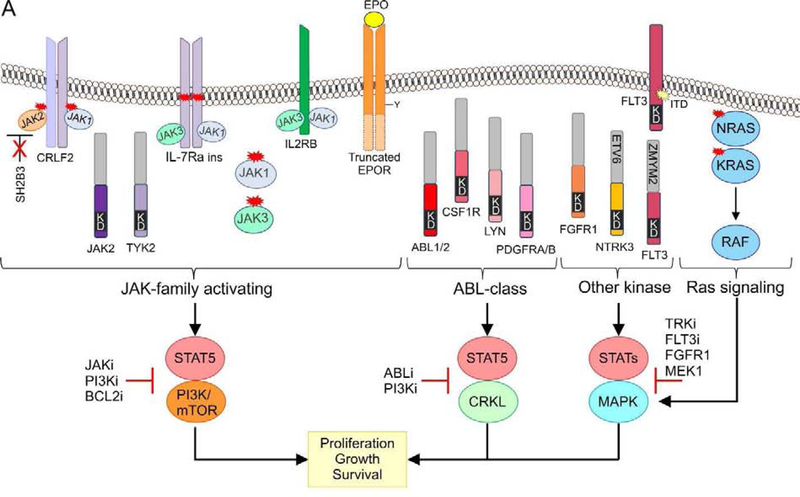
Ph-like ALL is extremely heterogeneous in the genes altered and the nature (rearrangements, mutations, or deletions) of alterations that result in the activated tyrosine kinase or cytokine receptor signaling characteristic of this subtype of ALL (Figure 2). However, these fall into four main groups: (1) Alterations driving JAK-STAT signaling, most commonly rearrangements of CRLF2 (IGH-CRLF2, P2RY8-CRLF2, CRLF2 F232C), and less commonly, rearrangements of JAK2, EPOR, or TYK2, and mutations/deletions of IL7R, SH2B3, JAK1, JAK3, TYK2, IL2RB); (2) fusions involving ABL-class genes (ABL1, ABL2, CSF1R, LYN, PDGFRA, PDGFRB); (3) mutations activating Ras signaling (NRAS, KRAS, PTPN11); and (4) less common fusions (FLT3, FGFR1, NTRK3) [15, 26, 27] (Figure 2A). IGH-CRLF2 is particularly common in adolescent/adult ALL but is less common in children. ABL-class fusions are most prevalent in children with high-risk ALL. A small subset of children harboring rearrangement of CRLF2, most commonly P2RY8-CRLF2, lack the Ph-like ALL gene expression signature [10].
Figure 2.
Kinase alterations and signaling pathways dysregulated in Ph-like ALL. The majority of kinase and cytokine receptor alterations converge on two pathways that activate JAK-family member signaling or ABL-signaling. Alterations that activate JAK-STAT signaling can be targeted with JAK and PI3K inhibitors. ABL-class alterations can be targeted with ABL-inhibitors such as dasatinib. Other kinase alterations and those that activate Ras signaling can be targeted with specific inhibitors including those that inactivate TRK, FLT3, FGFR1, and MEK for the MAPK pathway.
Preclinical and anecdotal patient data have been reported to support evaluation of TKIs in trials of Ph-like ALL [34–37], but it is likely that responses will be variable and dependent on treatment regimen. For example, preclinical leukemia models driven by chimeric ABL-class or Janus kinase fusions are potently inhibited by imatinib/dasatinib or ruxolitinib, respectively, although with notable synergism with chemotherapy [38]. ETV6-NTRK3 fusions are a potent monogenic driver of Ph-like ALL and such cells are eradicated by NTRK inhibitors such as larotrectinib [39]. In contrast, CRLF2-rearranged leukemias show variable JAK-STAT activation and response to type I JAK inhibitors such as ruxolitinib. Thus, it is critical that TKI efficacy is formally evaluated in clinical trials, and this is being pursued by St. Jude Children’s Research Hospital (Total XVII, ) [40] and Children’s Oncology Group (COG) protocols (AALL1131, ; AALL1521, ) [32]. However, it is likely that alternative or adjunct treatment approaches will be required, particularly for CRLF2-rearranged ALL. Such approaches include combinatorial therapy with PI3K inhibitors [41] or BCL2 inhibitors [38].
ETV6-RUNX1-like ALL
Transcriptome sequencing studies incorporating analysis of gene expression profiles have shown that the majority of subtypes of ALL are notable for “phenocopies,” in which cases with similar gene expression profile to a well characterized fusion are identified that are driven by alternative, or unknown drivers. The most striking of these is Ph-like ALL, in which the prevalence of phenocopies (Ph-like) greatly outnumbers that of the index alteration (BCR-ABL1). The next most prevalent is ETV6-RUNX1-like ALL, which exhibits a gene expression profile and immunophenotype (CD27 positive, CD44 low to negative) similar to ETV6-RUNX1 ALL [42, 43]. As with ETV6-RUNX1 ALL, ETV6-RUNX1-like ALL is almost exclusively identified in children (~3%) and confers a favorable prognosis, emphasizing the importance of detecting this subtype to potentially treat such cases with less intensive therapies. This subtype is associated with alternate lesions (gene fusions or copy number alterations) in ETV6, IKZF1, or TCF3, suggesting global deregulation of lymphoid development is a hallmark of this transcriptional signature [10].
DUX4-rearranged ALL
DUX4-rearranged ALL is particularly important in view of its favorable outcome in both children and adults. Such cases have a very distinctive gene expression profile and immunophenotype (CD2 and CD371 positive) [18, 42, 44–47]. This form of leukemia is driven by two transcription factor gene alterations. The initiating alteration is rearrangement of the homeobox transcription factor DUX4 (double homeobox 4) that results in expression of a C-terminal truncated DUX4 protein. DUX4 then binds to an intragenic region of the ETS family transcription factor gene ERG (ETS-related gene). This results in multiple alterations of ERG: gross transcriptional deregulation with expression of multiple coding, non-coding, and antisense transcripts, and commonly, expression of a C-terminal truncated isoform of ERG, ERGalt, that is encoded by a non-canonical first exon induced by DUX4 binding. ERGalt retains the DNA-binding and transactivating domain of ERG, inhibits the transcriptional activity of wild-type ERG, and is transforming in mouse models of B-ALL [44]. Many DUX4-rearranged cases also exhibit ERG deletions induced by RAG-mediated recombination. This is widely, but inappropriately used as a biomarker of this subtype, as almost half of DUX4 rearranged cases have no clonal ERG deletion. This is clinically important: IKZF1 (Ikaros) alterations are common in DUX4 rearranged ALL, but in contrast to BCR-ABL1 and Ph-like ALL are not associated with poor outcome—in contrast, DUX4-rearranged ALL is associated with an excellent prognosis in both children and adults [10, 44]. Thus, approaches to selectively genotype ERG and IKZF1 alterations to refine treatment intensification are inadequate as many IKZF1-altered cases are DUX4-rearranged but ERG wild type, and without identification of DUX4 rearrangement may be directed to inappropriately intensive therapy. Identification of DUX4 rearrangements by genomic approaches, DUX4 expression or flow cytometry is needed.
NUTM1 rearrangements
Fusion of almost all the coding region of NUTM1 (nuclear protein in testis midline carcinoma family 1) to six different 5′ partners is observed in 1%−2% of childhood ALL: ACIN1, BRD9, CUX1, IKZF1, SLC12A6, and ZNF618, resulting in increased expression of NUTM1 [10, 22]. NUTM1 is a chromatin modifier in the testis by recruiting EP300 to increase local histone acetylation [48]. BRD4-NUTM1 is a hallmark of NUT midline carcinoma (NMC) [49]. BRD4-NUTM1 acts to repress differentiation in NMC by recruiting histone acetyltransferases and other transcriptional cofactors to regions of chromatin that are actively transcribing pro-proliferative and anti-differentiation genes, including MYC [49]. The mechanistic basis of NUTM1 rearrangements in leukemogenesis is unknown, but in view of the common involvement of BRD9, bromodomain or HDAC inhibitors merit investigation.
PAX5-driven subtypes
The B-cell transcription factor gene PAX5 is commonly mutated in ALL, and with the exception of rearrangements, PAX5 alterations were previously considered to be important, but secondary, cooperating lesions in leukemogenesis [7, 8, 50]. Large RNA-seq studies have now shown that PAX5 alterations also define two distinct subtypes of ALL [10, 22]. PAX5-altered (PAX5alt), comprises cases with diverse PAX5 rearrangements (most commonly to ETV6 or NOL4L), sequence mutations, or intragenic amplification [51], with the highest prevalence observed in children and AYA (10% each vs. 7% in adults) [10]. The second subtype is characterized by the presence of the PAX5 P80R mutation with inactivation of the wild-type PAX5 allele from deletion of frameshift mutation, indicating loss of both PAX5 alleles drives the unique unique gene expression profile of this subtype [10, 22, 52]. PAX5 P80R increases with age, accounting for almost 5% of adults, and is associated with intermediate to favorable prognosis [10, 52]. PAX5 P80R cases have a high frequency of signaling mutations, particularly in the Ras pathway. The notion that specific sequence mutations define B-ALL subtypes is provocative, but confirmed by the observation that mice harboring constitutive PAX5 P80R mutations develop highly penetrant B-progenitor ALL, with inactivation of the wild-type Pax5 allele as observed in human ALL [10]. The identification of PAX5 subtypes as distinct entities highlights the importance of this gene in regulating B-cell differentiation and confirms PAX5 alterations as founding lesions in B-lymphoid leukemogenesis as opposed to secondary cooperating events as previously thought.
IKZF1 N159Y
A second example of mutation-initiated ALL is a subtype with heterozygous IKZF1 N159Y mutations [10, 22]. Like PAX5, IKZF1 mutations are common in ALL, however IKZF1 N159Y defines this subtype. The mutation is located at a critical DNA-binding residue of the N-terminal zinc fingers of IKZF1 and results in misregulation of IKZF1 transcriptional activation, in part through subcellular mislocalization [53]. As with PAX5 P80R, the reason why this specific mutation, but not similarly deleterious mutations, drives a distinct subtype is unclear, but is important as IKZF1 alterations result in aberrant leukemic cell adhesion and drug resistance that is reversible with rexinoids and focal adhesion kinase inhibitors [53, 54].
IGH rearrangements
The IGH locus is rearranged to multiple partner genes in ALL across the age spectrum including CRLF2, CEBP family members (CCAAT/enhancer binding protein) and ID4 and generally confer a poor prognosis [55, 56]. Transcriptomic sequencing has identified a subset of cases with pre-B immunophenotype and a unique transcriptional signature characterized by rearrangement of IGH to BCL2, MYC, and/or BCL6 (BCL2/MYC) [10] that resemble those observed in “double-hit” lymphoma, and are rarely identified in ALL [55, 57–59]. This subtype is predominantly identified in adults (median age 48.5 years) and is associated with an extremely unfavorable outcome.
Hypodiploid ALL
Hypodiploid ALL comprises two main subtypes of generally unfavorable prognosis: near haploid ALL with a modal chromosome number of 24–31, and low hypodiploid ALL with 32–39 chromosomes. These subtypes have distinct gene expression profiles and genetic alterations; high hypodiploid cases (40–44 chromosomes) are heterogeneous and not a distinct entity. Near haploid ALL is characterized by a high frequency of Ras pathway alterations (particularly NF1) and IKZF2 (Helios) alterations, and low hypodiploid ALL IKZF3 (Aiolos) and TP53 mutations. Near hypodiploid ALL is mostly observed in children, while low hypodiploid ALL is more common in adults. In children, many low hypodiploid ALL cases harbor germline TP53 alterations, whereas in adults, these alterations are somatic. Hypodiploid ALL cells are exquisitely sensitive to BCL2 inhibitors such as venetoclax, and these agents (venetoclax and navitoclax) are now being tested in clinical trials.
Conclusions
A decade of intensive effort has now resolved the genetic drivers of the majority of B-ALL cases across the age spectrum. This has had several major implications for clinical management. First, in view of the striking associations with outcome in both children and adults, accurate identification of both classical subtype-defining lesions, drivers of phenocopies, and submicroscopic lesions (PAX5 P80R, IZKF N159Y) is required. This required careful genomic analysis, ideally with sequencing-based approaches, but such approaches are increasingly widely utilized. Secondly, while there are attractive therapeutic options for several subtypes, much work is needed. The majority of subtypes are driven by transcription factor alterations that are not intuitively directly druggable; and some subtypes with dismal prognosis have no immediately attractive therapy. Thus, while the ALL field has enthusiastically pursued genotype-agnostic approaches such as antibody and cellular immunotherapy, much work is needed to define the tumor-intrinsic and -extrinsic determinants of response, as well as systematically investigating the vulnerabilities of each subtype to new therapeutic approaches. Ideally, each new agent will be tested in clinical trials of newly diagnosed ALL rather than at relapse, but this will pose major challenges for trial design and accrual. However, these challenges have been met for Ph+ ALL.
Acknowledgements
The authors thank colleagues at St. Jude, the Children’s Oncology Group, and the multiple centers and leukemia cooperative study groups that have contributed samples and expertise to many of the studies described in this review. The authors are supported by a National Cancer Institute R35 CA197695 Outstanding Investigator Award, a St Baldrick’s Foundation Robert J. Arceci Innovation Award, and the Henry Schueler 41&9 Foundation.
Footnotes
Disclosure:
Consulting fees: Amgen, Pfizer; Speakers Bureau: Amgen, Pfizer; Contracted research: Loxo Oncology
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- [1].Hunger SP, Mullighan CG. Acute Lymphoblastic Leukemia in Children. N Engl J Med 2015;373:1541–1552. [DOI] [PubMed] [Google Scholar]
- [2].Frey NV, Luger SM. How I treat adults with relapsed or refractory Philadelphia chromosome-negative acute lymphoblastic leukemia. Blood 2015;126:589–596. [DOI] [PubMed] [Google Scholar]
- [3].Harrison CJ, Moorman AV, Schwab C, Iacobucci I, Mullighan C. Cytogenetics and Molecular Genetics In: Vora A, editor. Childhood Acute Lymphoblastic Leukemia. Cham: Springer International Publishing; 2017. p. 61–98. [Google Scholar]
- [4].Tzoneva G, Dieck CL, Oshima K, Ambesi-Impiombato A, Sanchez-Martin M, Madubata CJ, et al. Clonal evolution mechanisms in NT5C2 mutant-relapsed acute lymphoblastic leukaemia. Nature 2018;553:511–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Ma X, Edmonson M, Yergeau D, Muzny DM, Hampton OA, Rusch M, et al. Rise and fall of subclones from diagnosis to relapse in pediatric B-acute lymphoblastic leukaemia. Nat Commun 2015;6:6604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Mullighan CG, Phillips LA, Su X, Ma J, Miller CB, Shurtleff SA, et al. Genomic analysis of the clonal origins of relapsed acute lymphoblastic leukemia. Science 2008;322:1377–1380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Mullighan CG, Goorha S, Radtke I, Miller CB, Coustan-Smith E, Dalton JD, et al. Genome-wide analysis of genetic alterations in acute lymphoblastic leukaemia. Nature 2007;446:758–764. [DOI] [PubMed] [Google Scholar]
- [8].Kuiper RP, Schoenmakers EF, van Reijmersdal SV, Hehir-Kwa JY, van Kessel AG, van Leeuwen FN, et al. High-resolution genomic profiling of childhood ALL reveals novel recurrent genetic lesions affecting pathways involved in lymphocyte differentiation and cell cycle progression. Leukemia 2007;21:1258–1266. [DOI] [PubMed] [Google Scholar]
- [9].Liu Y, Easton J, Shao Y, Maciaszek J, Wang Z, Wilkinson MR, et al. The genomic landscape of pediatric and young adult T-lineage acute lymphoblastic leukemia. Nat Genet 2017;49:1211–1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Gu Z, Churchman ML, Roberts KG, Moore I, Zhou X, Nakitandwe J, et al. PAX5-driven subtypes of B-progenitor acute lymphoblastic leukemia. Nat Genet 2019;51:296–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Gu Z, Churchman M, Roberts K, Li Y, Liu Y, Harvey RC, et al. Genomic analyses identify recurrent MEF2D fusions in acute lymphoblastic leukaemia. Nat Commun 2016;7:13331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Liu YF, Wang BY, Zhang WN, Huang JY, Li BS, Zhang M, et al. Genomic profiling of adult and pediatric B-cell acute lymphoblastic leukemia. EBioMedicine 2016;8:173–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Suzuki K, Okuno Y, Kawashima N, Muramatsu H, Okuno T, Wang X, et al. MEF2D-BCL9 fusion gene is associated with high-risk acute B-cell precursor lymphoblastic leukemia in adolescents. J Clin Oncol 2016;34:3451–3459. [DOI] [PubMed] [Google Scholar]
- [14].Ohki K, Kiyokawa N, Saito Y, Hirabayashi S, Nakabayashi K, Ichikawa H, et al. Clinical and molecular characteristics of MEF2D fusion-positive B-cell precursor acute lymphoblastic leukemia in childhood, including a novel translocation resulting in MEF2D-HNRNPH1 gene fusion. Haematologica 2019;104:128–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Roberts KG, Li Y, Payne-Turner D, Harvey RC, Yang YL, Pei D, et al. Targetable kinase-activating lesions in Ph-like acute lymphoblastic leukemia. N Engl J Med 2014;371:1005–1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Alexander TB, Gu Z, Iacobucci I, Dickerson K, Choi JK, Xu B, et al. The genetic basis and cell of origin of mixed phenotype acute leukaemia. Nature 2018;562:373–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Shago M, Abla O, Hitzler J, Weitzman S, Abdelhaleem M. Frequency and outcome of pediatric acute lymphoblastic leukemia with ZNF384 gene rearrangements including a novel translocation resulting in an ARID1B/ZNF384 gene fusion. Pediatr Blood Cancer 2016;63:1915–1921. [DOI] [PubMed] [Google Scholar]
- [18].Yasuda T, Tsuzuki S, Kawazu M, Hayakawa F, Kojima S, Ueno T, et al. Recurrent DUX4 fusions in B cell acute lymphoblastic leukemia of adolescents and young adults. Nat Genet 2016;48:569–574. [DOI] [PubMed] [Google Scholar]
- [19].Hirabayashi S, Ohki K, Nakabayashi K, Ichikawa H, Momozawa Y, Okamura K, et al. ZNF384-related fusion genes define a subgroup of childhood B-cell precursor acute lymphoblastic leukemia with a characteristic immunotype. Haematologica 2017;102:118–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Griffith M, Griffith OL, Krysiak K, Skidmore ZL, Christopher MJ, Klco JM, et al. Comprehensive genomic analysis reveals FLT3 activation and a therapeutic strategy for a patient with relapsed adult B-lymphoblastic leukemia. Exp Hematol 2016;44:603–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Oberley MJ, Gaynon PS, Bhojwani D, Pulsipher MA, Gardner RA, Hiemenz MC, et al. Myeloid lineage switch following chimeric antigen receptor T-cell therapy in a patient with TCF3-ZNF384 fusion-positive B-lymphoblastic leukemia. Pediatr Blood Cancer 2018;65:e27265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Li JF, Dai YT, Lilljebjorn H, Shen SH, Cui BW, Bai L, et al. Transcriptional landscape of B cell precursor acute lymphoblastic leukemia based on an international study of 1,223 cases. Proc Natl Acad Sci U S A 2018;115:E11711–e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Den Boer ML, van Slegtenhorst M, De Menezes RX, Cheok MH, Buijs-Gladdines JG, Peters ST, et al. A subtype of childhood acute lymphoblastic leukaemia with poor treatment outcome: a genome-wide classification study. Lancet Oncol 2009;10:125–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Mullighan CG, Su X, Zhang J, Radtke I, Phillips LA, Miller CB, et al. Deletion of IKZF1 and prognosis in acute lymphoblastic leukemia. N Engl J Med 2009;360:470–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Arber DA, Orazi A, Hasserjian R, Thiele J, Borowitz MJ, Le Beau MM, et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood 2016;127:2391–2405. [DOI] [PubMed] [Google Scholar]
- [26].Roberts KG, Gu Z, Payne-Turner D, McCastlain K, Harvey RC, Chen IM, et al. High frequency and poor outcome of Philadelphia chromosome-like acute lymphoblastic leukemia in adults. J Clin Oncol 2017;35:394–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Reshmi SC, Harvey RC, Roberts KG, Stonerock E, Smith A, Jenkins H, et al. Targetable kinase gene fusions in high-risk B-ALL: a study from the Children’s Oncology Group. Blood 2017;129:3352–3361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Jain N, Roberts KG, Jabbour E, Patel K, Eterovic AK, Chen K, et al. Ph-like acute lymphoblastic leukemia: a high-risk subtype in adults. Blood 2017;129:572–581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Tasian SK, Hurtz C, Wertheim GB, Bailey NG, Lim MS, Harvey RC, et al. High incidence of Philadelphia chromosome-like acute lymphoblastic leukemia in older adults with B-ALL. Leukemia 2017;31:981–984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Roberts KG, Reshmi SC, Harvey RC, Chen IM, Patel K, Stonerock E, et al. Genomic and outcome analyses of Ph-like ALL in NCI standard-risk patients: a report from the Children’s Oncology Group. Blood 2018;132:815–824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Loh ML, Zhang J, Harvey RC, Roberts K, Payne-Turner D, Kang H, et al. Tyrosine kinome sequencing of pediatric acute lymphoblastic leukemia: a report from the Children’s Oncology Group TARGET Project. Blood 2013;121:485–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Tasian SK, Loh ML, Hunger SP. Philadelphia chromosome-like acute lymphoblastic leukemia. Blood 2017;130:2064–2072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Roberts KG, Pei D, Campana D, Payne-Turner D, Li Y, Cheng C, et al. Outcomes of children With BCR-ABL1-like acute lymphoblastic leukemia treated with risk-directed therapy based on the levels of minimal residual disease. J Clin Oncol 2014;32:3012–3020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Kobayashi K, Miyagawa N, Mitsui K, Matsuoka M, Kojima Y, Takahashi H, et al. TKI dasatinib monotherapy for a patient with Ph-like ALL bearing ATF7IP/PDGFRB translocation. Pediatr Blood Cancer 2015;62:1058–1060. [DOI] [PubMed] [Google Scholar]
- [35].Lengline E, Beldjord K, Dombret H, Soulier J, Boissel N, Clappier E. Successful tyrosine kinase inhibitor therapy in a refractory B-cell precursor acute lymphoblastic leukemia with EBF1-PDGFRB fusion. Haematologica 2013;98:e146–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Schwab C, Ryan SL, Chilton L, Elliott A, Murray J, Richardson S, et al. EBF1-PDGFRB fusion in pediatric B-cell precursor acute lymphoblastic leukemia (BCP-ALL): genetic profile and clinical implications. Blood 2016;127:2214–2218. [DOI] [PubMed] [Google Scholar]
- [37].Weston BW, Hayden MA, Roberts KG, Bowyer S, Hsu J, Fedoriw G, et al. Tyrosine kinase inhibitor therapy induces remission in a patient with refractory EBF1-PDGFRB-positive acute lymphoblastic leukemia. J Clin Oncol 2013;31:e413–416. [DOI] [PubMed] [Google Scholar]
- [38].Roberts KG, Yang Y-L, Payne-Turner D, Lin W, Files JK, Dickerson K, et al. Oncogenic role and therapeutic targeting of ABL-class and JAK-STAT activating kinase alterations in Ph-like ALL. Blood Adv 2017;1:1657–1671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Roberts KG, Janke LJ, Zhao Y, Seth A, Ma J, Finkelstein D, et al. ETV6-NTRK3 induces aggressive acute lymphoblastic leukemia highly sensitive to selective TRK inhibition. Blood 2018;132:861–865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Inaba H, Azzato EM, Mullighan CG. Integration of next-generation sequencing to treat acute lymphoblastic leukemia with targetable lesions: The St. Jude Children’s Research Hospital approach. Front Pediatr 2017;5:258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Tasian SK, Teachey DT, Li Y, Shen F, Harvey RC, Chen IM, et al. Potent efficacy of combined PI3K/mTOR and JAK or ABL inhibition in murine xenograft models of Ph-like acute lymphoblastic leukemia. Blood 2017;129:177–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Lilljebjorn H, Henningsson R, Hyrenius-Wittsten A, Olsson L, Orsmark-Pietras C, von Palffy S, et al. Identification of ETV6-RUNX1-like and DUX4-rearranged subtypes in paediatric B-cell precursor acute lymphoblastic leukaemia. Nat Commun 2016;7:11790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Zaliova M, Kotrova M, Bresolin S, Stuchly J, Stary J, Hrusak O, et al. ETV6/RUNX1-like acute lymphoblastic leukemia: A novel B-cell precursor leukemia subtype associated with the CD27/CD44 immunophenotype. Genes Chromosomes Cancer 2017;56:608–616. [DOI] [PubMed] [Google Scholar]
- [44].Zhang J, McCastlain K, Yoshihara H, Xu B, Chang Y, Churchman ML, et al. Deregulation of DUX4 and ERG in acute lymphoblastic leukemia. Nat Genet 2016;48:1481–1489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Schinnerl D, Mejstrikova E, Schumich A, Zaliova M, Fortschegger K, Nebral K, et al. CD371 cell surface expression: A unique feature of DUX4-rearranged acute lymphoblastic leukemia. Haematologica 2019; 104:e352–e355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Harvey RC, Mullighan CG, Wang X, Dobbin KK, Davidson GS, Bedrick EJ, et al. Identification of novel cluster groups in pediatric high-risk B-precursor acute lymphoblastic leukemia with gene expression profiling: correlation with genome-wide DNA copy number alterations, clinical characteristics, and outcome. Blood 2010;116:4874–4884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Yeoh EJ, Ross ME, Shurtleff SA, Williams WK, Patel D, Mahfouz R, et al. Classification, subtype discovery, and prediction of outcome in pediatric acute lymphoblastic leukemia by gene expression profiling. Cancer Cell 2002;1:133–143. [DOI] [PubMed] [Google Scholar]
- [48].Alekseyenko AA, Walsh EM, Wang X, Grayson AR, Hsi PT, Kharchenko PV, et al. The oncogenic BRD4-NUT chromatin regulator drives aberrant transcription within large topological domains. Genes Dev 2015;29:1507–1523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].French C NUT midline carcinoma. Nat Rev Cancer. 2014;14:149–150. [DOI] [PubMed] [Google Scholar]
- [50].Dang J, Wei L, de Ridder J, Su X, Rust AG, Roberts KG, et al. Pax5 is a tumor suppressor in mouse mutagenesis models of acute lymphoblastic leukemia. Blood 2015;125:3609–3617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Schwab C, Nebral K, Chilton L, Leschi C, Waanders E, Boer JM, et al. Intragenic amplification of PAX5: a novel subgroup in B-cell precursor acute lymphoblastic leukemia? Blood Adv 2017;1:1473–1477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Passet M, Boissel N, Sigaux F, Saillard C, Bargetzi M, Ba I, et al. PAX5 P80R mutation identifies a novel subtype of B-cell precursor acute lymphoblastic leukemia with favorable outcome. Blood 2019;133:280–284. [DOI] [PubMed] [Google Scholar]
- [53].Churchman ML, Low J, Qu C, Paietta EM, Kasper LH, Chang Y, et al. Efficacy of retinoids in IKZF1-mutated BCR-ABL1 acute lymphoblastic leukemia. Cancer Cell 2015;28:343–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Churchman ML, Evans K, Richmond J, Robbins A, Jones L, Shapiro IM, et al. Synergism of FAK and tyrosine kinase inhibition in Ph+ B-ALL. JCI Insight 2016;1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Russell LJ, Enshaei A, Jones L, Erhorn A, Masic D, Bentley H, et al. IGH@ translocations are prevalent in teenagers and young adults with acute lymphoblastic leukemia and are associated with a poor outcome. J Clin Oncol 2014;32:1453–1462. [DOI] [PubMed] [Google Scholar]
- [56].Dyer MJ, Akasaka T, Capasso M, Dusanjh P, Lee YF, Karran EL, et al. Immunoglobulin heavy chain (IGH) locus chromosomal translocations in B-cell precursor acute lymphoblastic leukemia (BCP-ALL): rare clinical curios or potent genetic drivers? Blood 2010; 115:1490–1499. [DOI] [PubMed] [Google Scholar]
- [57].Moorman AV, Schwab C, Ensor HM, Russell LJ, Morrison H, Jones L, et al. IGH2 translocations, CRLF2 deregulation, and microdeletions in adolescents and adults with acute lymphoblastic leukemia. J Clin Oncol 2012;30:3100–3108. [DOI] [PubMed] [Google Scholar]
- [58].Uchida A, Isobe Y, Uemura Y, Nishio Y, Sakai H, Kato M, et al. De novo acute lymphoblastic leukemia-like disease of high grade B-cell lymphoma with MYC and BCL2 and/or BCL6 rearrangements: a case report and literature review. BMC Clin Pathol 2017;17:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Wagener R, Lopez C, Kleinheinz K, Bausinger J, Aukema SM, Nagel I, et al. IG-MYC (+) neoplasms with precursor B-cell phenotype are molecularly distinct from Burkitt lymphomas. Blood. 2018;132:2280–2285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Paulsson K, Lilljebjorn H, Biloglav A, Olsson L, Rissler M, Castor A, et al. The genomic landscape of high hyperdiploid childhood acute lymphoblastic leukemia. Nat Genet 2015;47:672–676. [DOI] [PubMed] [Google Scholar]
- [61].Holmfeldt L, Wei L, Diaz-Flores E, Walsh M, Zhang J, Ding L, et al. The genomic landscape of hypodiploid acute lymphoblastic leukemia. Nat Genet 2013;45:242–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Harrison CJ. Blood Spotlight on iAMP21 acute lymphoblastic leukemia (ALL), a high-risk pediatric disease. Blood 2015;125:1383–1386. [DOI] [PubMed] [Google Scholar]
- [63].Jaffe JD, Wang Y, Chan HM, Zhang J, Huether R, Kryukov GV, et al. Global chromatin profiling reveals NSD2 mutations in pediatric acute lymphoblastic leukemia. Nat Genet 2013;45:1386–1391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Andersson AK, Ma J, Wang J, Chen X, Gedman AL, Dang J, et al. The landscape of somatic mutations in infant MLL-rearranged acute lymphoblastic leukemias. Nat Genet 2015;47:330–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Barber KE, Harrison CJ, Broadfield ZJ, Stewart AR, Wright SL, Martineau M, et al. Molecular cytogenetic characterization of TCF3 (E2A)/19p13.3 rearrangements in B-cell precursor acute lymphoblastic leukemia. Genes Chromosomes Cancer 2007;46:478–486. [DOI] [PubMed] [Google Scholar]
- [66].Burmeister T, Gokbuget N, Schwartz S, Fischer L, Hubert D, Sindram A, et al. Clinical features and prognostic implications of TCF3-PBX1 and ETV6-RUNX1 in adult acute lymphoblastic leukemia. Haematologica 2010;95:241–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Fischer U, Forster M, Rinaldi A, Risch T, Sungalee S, Warnatz HJ, et al. Genomics and drug profiling of fatal TCF3-HLF-positive acute lymphoblastic leukemia identifies recurrent mutation patterns and therapeutic options. Nat Genet 2015;47:1020–1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [68].Mullighan CG, Miller CB, Radtke I, Phillips LA, Dalton J, Ma J, et al. BCR-ABL1 lymphoblastic leukaemia is characterized by the deletion of Ikaros. Nature 2008;453:110–114. [DOI] [PubMed] [Google Scholar]