Abstract
Background
With increasing efforts to scrutinize and reduce opioid prescribing, limited data exist on the recent trend in receipt of prescription pain medications before diagnosis of opioid use disorder (OUD) or opioid-related overdose (OD).
Methods
Using 2005–2016 Truven MarketScan Commercial Claims databases, we assessed trends in annual 1) incidence of OUD or OD and 2) prevalence of receipt of prescription opioids or four commonly-prescribed adjuvant analgesics among patients newly diagnosed with OUD/OD. Trends were examined in the overall sample and by 3 age groups, including youths (≤18 years), adults (19–64 years), and older adults (≥65 years).
Results
The incidence of diagnosed OUD or OD increased more than 3-fold from 4.99 to 23.81 per 10,000 persons from 2006 to 2016, with the highest increase (14.18-fold) seen in older adults, followed by adults (3.53-fold), and youths (0.16-fold). Between 2006 and 2016, the proportion of patients with incident OUD/OD who received anticonvulsant adjuvant analgesics in the year before diagnosis increased (from 23.4% to 34.3% [P-trend = .005]) whereas the proportion receiving high-dose prescriptions opioids decreased (from 45.5% to 34.8% [P-trend =< .001]). A decreasing trend was observed in general for tricyclic antidepressants and serotonin and norepinephrine reuptake inhibitors.
Discussion
In US commercially insured patients newly diagnosed with OUD/OD, receipt of high-dose opioid prescriptions preceding the diagnosis decreased over time, paralleled by increased use of anticonvulsants commonly prescribed for pain conditions. Further investigations are warranted to understand how prescribed and anticonvulsants contribute to the development of OUD/OD.
Keywords: Opioid Use Disorders, Incidence Of OUD Or Opioid-Related Overdose, Prescription Opioid And Adjuvant Analgesics
1. Introduction
Opioid use disorder (OUD) is the main contributor to opioid-related morbidity and mortality in the United States (U.S.) (Rudd et al., 2016). The Diagnostic and Statistical Manual of Mental Disorders (Fifth Edition) characterizes OUD as problematic use of opioids leading to significant impairment or distress characterized by the presence of at least 2 of 11 symptoms in a 12-month period (Hasin et al., 2013). National survey data suggest that 1.9 million adults (0.8%) had OUD in 2015, with a higher prevalence (2.1%) observed among adults who use prescription opioids (Han et al., 2017). Both US survey and administrative claims data have shown a consistent upward trend in the prevalence of OUD, at the magnitude of a 3-fold increase from 2003 to 2013 (Dufour et al., 2014; Kirson et al., 2015). Of note, this upward trend has continued despite noted decreases in opioid prescribing.
Although there is evidence of a declining use of prescription opioids over time (Guy et al., 2017), trends in use patterns have not been examined among patients who develop OUD or opioid-related overdose (OD) (Madras 2017; Dowell et al., 2016; Soelberg et al., 2017). With increasing efforts by state and federal authorities, health plans, and professional associations to reduce access to prescription opioids (Schuchat et al., 2017), there is increasing concern that patients may supplement the restricted amount of prescription opioids with alternative prescription medications or illicit substances to achieve pain control or to enhance euphoric effects (Throckmorton et al., 2018). For instance, gabapentinoids (including both pregabalin and gabapentin), used as adjuvant nonopioid treatment of neuropathic pain, carry the risk of abuse potential, especially among patients with a history of opioid abuse (Evoy et al., 2017). Pregabalin, classified as a US Drug Enforcement Administration schedule V controlled substance, was recently discovered in more than one-fifth of fatal OD (Slavova et al., 2018). Although this number appears alarming, no study has examined trends of gabapentinoid use to explore whether changes in use patterns may help explain the continuing growth of ODs in light of decreasing opioid prescribing.
The present study aimed to first examine the secular trend in the incidence of individuals who were newly diagnosed as having OUD/OD to understand the recent change in background incidence of the diagnosis. We then examined the trend in the receipt of prescription opioids and 4 commonly U.S. prescribed classes of adjuvant analgesics (including anticonvulsants) for treatment of pain conditions in the year before the diagnosed incident OUD/OD. We assessed both aims in the overall sample as well as in 3 distinct age groups, namely youths (aged ≤18 years), adults (aged 19–64 years), and older adults (aged ≥65 years) to understand whether the secular trend varied by age.
2. Methods
2.1. Study Design and Source
We used the 2005–2016 Truven MarketScan databases of Commercial and Medicare supplement claims to conduct a cross-sectional study of individuals across the age spectrum to assess 11-year trends of OUD/OD incidence and prescription opioids and adjuvant analgesics among the patients with OUD/OD. The Truven database consists of more than 350 self-insured employers and health plans, including approximately 46.9 million youths and 135.9 million adults in the commercial claims datasets, and 21.5 million older adults participating in Medicare supplemental insurance programs in the US between 2005 and 2016. The Truven database has been widely used to evaluate trends in incidence or prevalence of diseases (including OUD and OD) and prescription drug use among different age groups (Hadland et al., 2017; Roland et al., 2013). The files contain enrollee billing records for inpatient and outpatient encounters and pharmacy filled prescriptions, as well as enrollee demographics and enrollment status. The inpatient and outpatient records include details on procedures and diagnoses, coded using the International Classification of Disease, Ninth or Tenth Revision, Clinical Modification (ICD-9-CM or ICD-10-CM). This cross-sectional study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline. The University of Florida at Gainesville institutional review and privacy boards exempted this study from review because the data were deidentified.
2.1.2. Study Sample
To assess annual incidence of OUD or OD, we include individuals who had continuous enrollment with health and drug benefits for any 2 consecutive years between 2005 and 2016 and who had no OUD or OD diagnosis during the initial year of the 2-year observation period. Patients could contribute to multiple 2-year observation period if they met enrollment requirements. OUD or OD was defined as having at least 1 inpatient or outpatient billing record with a diagnosis code for opioid dependence (ICD-9-CM codes, 304.0× 304.7x, and 305.5x; and ICD-10 codes, F11.xx) or opioid-related overdose (965.0x, E850.0-E850.2; and ICD-10-CM codes, T40.0xx to T40.4xx, where the “xx” placeholders contained X1 or X4 or T40.601, T40.604, T40.691, or T40.694) in any diagnostic position (Green et al., 2017). When identifying patients with incident OUD or OD, we excluded ICD-10-CM codes that indicated “in remission” (eg, F11.x1) or “subsequent encounter” (eg, F40.xxxD) of OUD or OD.
2.1.3. Incidence of OUD or OD
Annual incidence proportions were calculated as the number of eligible patients who were newly diagnosed as having OUD/OD (numerator) in a given year (e.g., 2006) divided by the total number of individuals who were at risk but had not yet been diagnosed with OUD/OD in the year (e.g., 2005) prior to the corresponding year (denominator). Annual incidence was reported as the number of cases per 10,000 persons.
2.1.4. Prescription Pain Medications
Prescription pain medications of interest included prescription opioids approved for management of pain and adjuvant medications used for pain conditions in the United States (U.S.). FDA-approved or guideline-recommended adjuvant analgesics for treatment of pain conditions in the U.S. include tricyclic antidepressants (TCAs), serotonin and norepinephrine reuptake inhibitor (SNRI) antidepressants, anticonvulsants, and muscle relaxants (Supplementary eTable 1). We did not include nonopioid analgesic pain medications (eg, acetaminophen or acetylsalicylic acid) because 1) these drugs are also available over the counter and are therefore not fully captured in pharmacy claims records; and 2) they are have no evident abuse potential and thus rarely increases the risk of OUD/OD when administrated with prescription opioids (Brune et al., 2015). We assessed prescription pain medications dispensed in the year before the incident OUD/OD.
2.1.5. Statistical Analysis
We reported annual crude incidences of OUD/OD from 2006 to 2016 in the overall eligible population sample and in 3 age groups: youths (≤18 years), adults (19–64 years), and older adults (≥ 65 years) according to the age at the beginning of the corresponding year. For each age group, we further analyzed the incidence trend in males and females and in predefined age strata within youths (≤6, 7–12, and 13–18 years), adults (19–30, 31–40, 41–50, and 51–64 years), and older adults (65–74, 75–84, 85+), as well as by both sex and age strata. Across the study years, there were changes in health plans contributing to Truven data, resulting in changes in the number of enrollees in the database (ie, a gradual increase in enrollee number through 2013 was followed by a decrease between 2014 and 2016; see Supplementary eTable 2. To reduce potential bias resulting from changes in the denominator population, we conducted a sensitivity analysis by estimating the age-standardized overall and age-specific incidence trends in a subset of individuals who were continuously enrolled from 2005 through 2016.
Across study years, we reported the proportion of patients with newly diagnosed OUD or OD who had received prescription opioids or each of 4 adjuvant analgesic classes during the year before the incident diagnosis. The proportions were calculated for the overall patients with OUD/OD as well as in youth, adult, and older adult groups with the diagnosis. For prescription opioids, we further analyzed the proportion of patients with high-dose use, defined as a mean daily morphine equivalent dosage of 90 mg or greater during a 30-day period (Dowell et al., 2016).
To describe trends in incidence of OUD/OD and in the receipt of prescription pain medications among patients with incident OUD/OD, we calculated a percentage change for each outcome of interest from 2006 to 2016. To test temporal trends, we used linear regression, a commonly-used approach to determine whether a trend follows a linear or non-linear pattern and to estimate the magnitude of the trend (Helsel et al., 2002). We fitted separate linear regression models with each outcome (measured as a proportion) as the dependent variable and year as the main independent variable. We reported P values for linear trends. For outcomes whose trends did not follow a linear pattern, we further fitted nonlinear regression with a quadratic polynomial function of the outcome of interest, and we did not observe any significant nonlinear pattern for these outcomes. All analyses were performed using SAS, version 9.4 (SAS Institute Inc). Statistical significance was set at P < .05, and all tests were 2-tailed.
3. Results
This study included data from 204,401,990 eligible individuals, consisting of 46,921,461 youths, 135,921,758 adults, and 21,558,771 older adults from 2005 through 2016. Information about sample sizes by year and age groups are given in Supplementary eTable 2. Among the eligible individuals, 268,918 patients were identified as having received a new diagnosis of OUD or OD, with 52.1% of the patients being male. Of this overall sample, 19,646 (7.3%) were 18 years old or younger, 227,126 (84.5%) were 19 to 64 years old, and 22,146 (8.2%) were 65 years or older. Information on sex, census region, pain diagnosis, selected health conditions, and substance use disorders among individuals who had received a diagnosis of OUD/OD in the overall population and stratified by age group is provided in Table 1.
Table 1.
Characteristics of Commercially Insured Individuals Who Received a New Diagnosis of OUD or Opioid-Related Overdose Between 2006 And 2016, Overall and by Age Group
| Characteristic | Individuals, No. (%) | |||
|---|---|---|---|---|
| Overall Incident OUD or Opioid-Related Overdose | Age Group | |||
| ≤18 Years | 19–64 Years | ≥65 Years | ||
| Sample size | 268,918 (100) | 19,646 (100) | 227,126 (100) | 22,146 (100) |
| Male sex | 140,074 (52.1) | 11,623 (59.2) | 119,735 (52.7) | 8,716 (39.4) |
| Census region | ||||
| South | 106,756 (39.7) | 6,305 (32.1) | 93,128 (41.0) | 7,323 (33.1) |
| Northeast | 51,654 (19.2) | 4,328 (22.0) | 44,496 (19.6) | 2,830 (12.8) |
| Northcentral | 56,731 (21.1) | 4,805 (24.5) | 45,657 (20.1) | 6,269 (28.3) |
| West | 53,777 (20.0) | 4,208 (21.4) | 43,845 (19.3) | 5,724 (25.8) |
| Pain diagnosis | ||||
| Chronic | 141,390 (52.6) | 2,126 (10.8) | 122,180 (53.8) | 17,084 (77.1) |
| Neuropathic | 64,405 (23.9) | 401 (2.0) | 55,401 (24.4) | 8,603 (38.8) |
| Musculoskeletal | 178,908 (66.5) | 5,994 (30.5) | 153,224 (67.5) | 19,690 (88.9) |
| Selected health condition | ||||
| Anxiety disorder | 53,803 (20.0) | 3,769 (19.2) | 46,445 (20.4) | 3,589 (16.2) |
| Depression | 88,972 (33.1) | 6,733 (34.3) | 75,389 (33.2) | 6,850 (30.9) |
| Seizure | 5620 (2.1) | 265 (1.3) | 4,816 (2.1) | 539 (2.4) |
| Substance use disorder | ||||
| Tobacco use disorder | 23,780 (8.8) | 1,044 (5.3) | 21,362 (9.4) | 1,374 (6.2) |
| Alcohol use disorder | 24,031 (8.8) | 2,396 (12.0) | 20,694 (9.0) | 941 (4.0) |
Abbreviation: OUD, opioid use disorder.
3.1. Incidence and Trends of OUD or OD
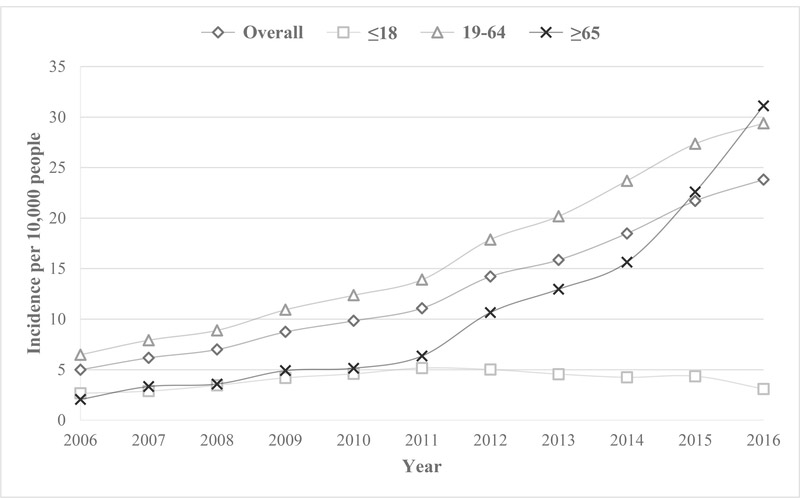
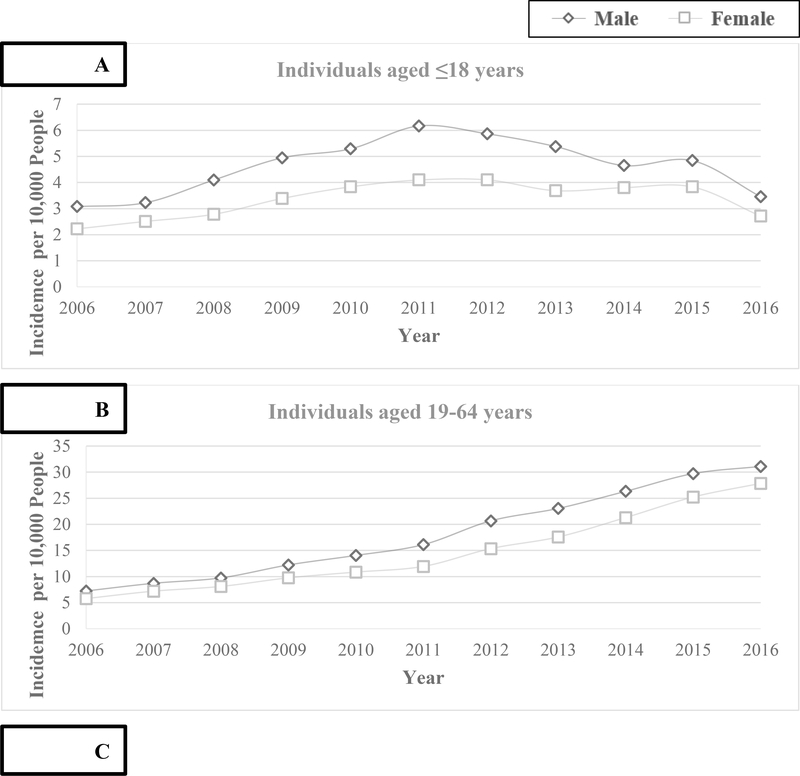
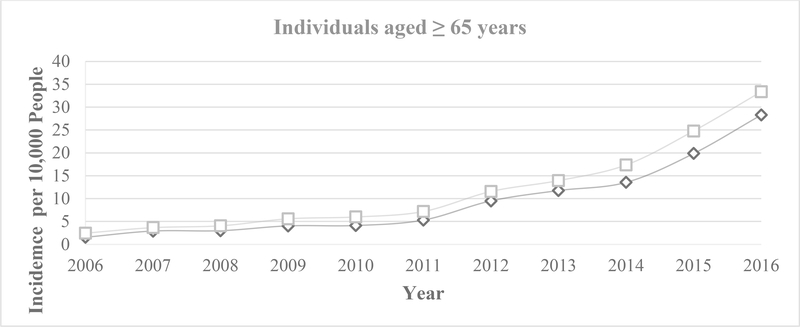
The overall crude incidence of OUD/OD increased by more than 3-fold, from 4.99 to 23.81 per 10,000 persons, between 2006 and 2016 (Figure 1). Age-specific incidence proportions revealed a 14.18-fold increase among older adults (from 2.05 to 31.12 per 10,000 persons), a 3.53-fold increase among adults (from 6.48 to 29.38 per 10,000 persons), and a 0.16-fold increase among youths (from 2.66 to 3.09 per 10,000 persons) between 2006 and 2016 (Figure 1). When analyzing the incidence trend of each age group stratified by predefined age-specific strata, teenagers aged 13 to 18 years, adults aged 19 to 30 years, and older adults aged 65 to 74 years had the highest incidence of OUD/OD across time in each corresponding age group (See Supplementary eFigure 1).We observed a sex difference in the incidence of OUD or OD across age groups. The incidence was significantly higher among males than among females in the youth and adult populations, whereas the opposite pattern, that is, a higher incidence among females than among males, was observed in the older adult population (Figure 2). The similar pattern of a sex difference in OUD/OD incidence was also observed in most of the age-predefined age strata in the youths, adults and older adults. (Supplementary eFigure 2) The sensitivity analysis among individuals with continuous enrollment throughout the 12-year study period showed similar upward trends in the incidence of OUD/OD in the overall study sample as well as in each of the 3 age groups (Supplementary eFigure 3).
Figure 1.
Annual Crude Incidence of Diagnosed Opioid Use Disorder or Opioid-Related Overdose in a Commercially Insured Population, Overall and by Age Group. Lines represent incidence trends, overall and within age groups, and for each line, each point represents annual incidence of OUD or OD.
Figures 2.
A-C. Annual Crude Incidence of Diagnosed Opioid Use Disorder or Opioid-Related Overdose in 3 Age Groups by Sex. In each sub-figure, lines represent incidence trends for males and females, and for each line, each point represents annual incidence of OUD or OD.
3.2. Prior Receipt of Prescription Opioids and Adjuvant Analgesics Before OUD or OD
Tables 2 gives the trends in prescription opioid receipt in the 12 months before diagnosed incident OUD/OD in the overall sample of patients and by age group. Between 2006 and 2016, the proportion of patients with OUD/OD who had received any prescription opioid before the diagnosis was unchanged with time in the overall patient population (from 70.7% to 70.8% [P-trend=.14]). However, this proportion decreased in youths (from 29.4% to 22.6% [P-trend=.001]) and in adults (from 75.6% to 70.8% [P-trend=.004] patients. In addition, we observed a more pronounced decreasing trend in the proportion of patients with high-dose prescription opioid use in the overall population (from 45.5% to 34.8% [P-trend=<.001]) and in all 3 age groups (from 8.4% to 3.1% in youths; 49.4% to 34.8% in adults; 67.3% to 41.6% in older adults; P-trend < .001 in all age groups) with incident OUD/OD.
Table 2.
Receipt of Prescription Opioids in the Year before Diagnosed Incident OUD or Opioid-Related Overdose in the Overall Patient Population and by Age Group From 2006 to 2016
| Percentage of Population | P Value for Trend | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Opioid Prescription | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | |
| Any | ||||||||||||
| Overall | 70.7 | 71.0 | 72.9 | 71.1 | 68.6 | 66.9 | 65.4 | 65.8 | 66.9 | 69.0 | 70.8 | .14 |
| Youth | 29.4 | 32.3 | 34.1 | 32.0 | 30.7 | 30.4 | 28.5 | 27.8 | 25.3 | 26.5 | 22.6 | .001 |
| Adult | 75.6 | 74.9 | 77.2 | 75.3 | 72.6 | 70.2 | 67.7 | 66.8 | 67.4 | 69.5 | 70.8 | .004 |
| Older adult | 87.1 | 85.5 | 87.8 | 87.7 | 86.4 | 86.6 | 78.7 | 83.7 | 86.9 | 84.9 | 81.6 | .11 |
| High dose | ||||||||||||
| Overall | 45.5 | 45.4 | 47.0 | 43.8 | 41.0 | 39.2 | 35.5 | 35.3 | 35.2 | 34.0 | 34.8 | <.001 |
| Youth | 8.4 | 8.9 | 7.4 | 7.1 | 6.6 | 5.3 | 4.0 | 5.2 | 4.9 | 3.7 | 3.1 | <.001 |
| Adult | 49.4 | 48.8 | 51.2 | 47.9 | 44.5 | 42.3 | 37.6 | 36.4 | 35.8 | 34.6 | 34.8 | <.001 |
| Older adult | 67.3 | 62.3 | 63.6 | 58.8 | 59.1 | 57.5 | 46.1 | 47.0 | 47.1 | 42.7 | 41.6 | <.001 |
Abbreviation: OUD, opioid use disorder.
Tables 3 gives the trends in the receipt of each of the 4 classes of adjuvant analgesics prescribed in the year before incident OUD/OD for the overall population and by age group. In the overall patient population, the proportion receiving tricyclic antidepressants (TCAs) (from 10.0% to 8.2% [P-trend < .001]), norepinephrine reuptake inhibitor antidepressants (SNRIs) (from 17.6% to 17.0% [P-trend = .03]) decreased from 2006 to 2016, and the proportion receiving muscle relaxants was unchanged (from 39.8% to 39.4% [P-trend = .28]) between 2006 and 2016. Conversely, the proportion of patients receiving the studied anticonvulsant analgesics increased with time in the overall patient population (from 23.4% to 34.3% [P-trend = .005]). When analyzed by age group, a contrasting pattern emerged only in adult patients for a significant increasing trend in the studied anticonvulsant fills concurrent with a significant decreasing trend in TCA, SNRI, or muscle relaxant adjuvant analgesic fills.
Table 3.
Receipt of Adjuvant Analgesic Treatment of Pain in the Year Before Diagnosed Incident OUD or Opioid-Related Overdose in the Overall Patient Population and by Age Group from 2006 to 2016
| Percentage of Population | P Value for Trend | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | ||
| Any TCA | ||||||||||||
| Overall | 10.0 | 9.7 | 9.2 | 8.6 | 8.0 | 7.9 | 7.8 | 7.6 | 8.0 | 7.7 | 8.2 | .002 |
| Youth | 2.2 | 2.4 | 2.7 | 3.1 | 2.7 | 3.0 | 2.1 | 2.1 | 2.4 | 3.5 | 1.9 | .92 |
| Adult | 10.8 | 10.2 | 9.7 | 9.1 | 8.5 | 8.3 | 8.1 | 7.8 | 8.2 | 8.0 | 8.4 | <.001 |
| Older adult | 14.1 | 13.9 | 15.6 | 12.6 | 11.3 | 10.6 | 10.2 | 9.9 | 9.5 | 7.8 | 7.9 | <.001 |
| Any SNRI | ||||||||||||
| Overall | 17.6 | 19.1 | 18.9 | 18.3 | 16.8 | 15.8 | 15.3 | 15.1 | 15.5 | 16.6 | 17.0 | .03 |
| Youth | 4.1 | 6.1 | 4.0 | 4.7 | 3.9 | 4.1 | 4.1 | 3.7 | 4.4 | 5.3 | 6.0 | .55 |
| Adult | 19.8 | 20.7 | 20.9 | 19.9 | 18.2 | 17.0 | 16.1 | 15.6 | 15.9 | 16.8 | 17.1 | .002 |
| Older adult | 13.2 | 21.2 | 20.4 | 22.7 | 21.3 | 19.8 | 18.1 | 18.8 | 19.2 | 19.7 | 19.2 | .73 |
| Any anticonvulsant | ||||||||||||
| Overall | 23.4 | 25.2 | 27.0 | 26.2 | 24.3 | 23.9 | 24.5 | 26.9 | 29.4 | 32.2 | 34.3 | .005 |
| Youth | 8.5 | 8.7 | 7.5 | 8.4 | 8.6 | 8.0 | 9.4 | 9.5 | 10.2 | 12.5 | 12.6 | .002 |
| Adult | 24.7 | 26.2 | 28.7 | 27.7 | 25.7 | 24.9 | 25.1 | 27.0 | 29.4 | 32.2 | 33.7 | .02 |
| Older adult | 36.0 | 38.9 | 40.1 | 39.3 | 35.9 | 38.5 | 34.1 | 39.0 | 41.3 | 41.9 | 43.3 | .08 |
| Any muscle relaxant | ||||||||||||
| Overall | 39.8 | 38.5 | 40.1 | 38.1 | 36.5 | 34.9 | 34.6 | 34.8 | 36.4 | 37.8 | 39.4 | .28 |
| Youth | 12.0 | 9.0 | 10.2 | 7.9 | 7.7 | 8.1 | 7.9 | 6.8 | 7.4 | 7.5 | 7.1 | .90 |
| Adult | 44.6 | 42.4 | 44.7 | 42.5 | 40.4 | 38.5 | 37.5 | 37.1 | 38.4 | 40.0 | 41.7 | .04 |
| Older adult | 29.1 | 37.5 | 35.2 | 32.8 | 33.6 | 33.5 | 30.5 | 33.3 | 33.5 | 32.3 | 31.5 | .52 |
Abbreviations: OUD, opioid use disorder; SNRI, serotonin and norepinephrine reuptake inhibitor; TCA, tricyclic antidepressant.
4. Discussion
The present study is among the first that examined secular trends in receipt of prescription opioids and 4 commonly prescribed classes of adjuvant analgesics in the year before the incident OUD/OD diagnosis over a decade. Within our population of commercially insured patients, we found a significantly decreasing trend in prescription opioid fills preceding an OUD/OD diagnosis for youth and adult patients. Moreover, our data showed a pronounced decrease in the proportion of patients who received mean doses above the recommended morphine equivalent threshold of 90 mg prior to their OUD/OD diagnosis (Dowell et al., 2016). Our findings are consistent with a recent national survey reporting a decline in opioid prescribing rates in the general adult population (Schuchat et al., 2017).
Although the decreases we observed in opioid prescription fills in youths and adults patients with OUD/OD may appear encouraging at first glance, our findings raise concern as to whether non-prescription source of opioids is the main contributor to OUD/OD. This concern is supported by a recent national survey indicating that the majority of individuals with OUD/OD reportedly obtained their opioids from friends or relatives for free or buying opioids from friends/relatives/drug dealers (Han et al., 2017). Among patients with OUD/OD who received opioids as part of medical pain management, the decrease in the number of those who received high-risk opioid doses also raise questions whether this patient population might also increasingly supplement their pain regimen with other prescription drugs with abuse potential or non-prescription opioids that contribute to OUD or OD.
The observed increasing trend in the receipt of the studied anticonvulsant analgesics preceded by incident OUD or OD raises some concern in this context. The mechanisms underlying development of OUD/OD after prescription anticonvulsant analgesics for treatment of pain conditions are not completely understood but two have been postulated. First, gabapentinoids—commonly prescribed anticonvulsant class for neuropathic pain— can produce euphoric effects that are reminiscent of, but not as strong as, opioids (Evoy et al., 2017; Satish et al., 2015). High doses (ie, 1.5–12 g) of gabapentinoids alone can induce euphoria that increases its potential for abuse and addiction (Smith et al., 2016). These drugs are reportedly being used among heroin and opioid abusers to enhance opioid high (Lyndon et al., 2017; Smith et al., 2015). Indeed, in a postmortem toxicology analysis conducted in a US state, more than one-fifth of fatal opioid-related overdoses were reported to have concomitant exposure to pregabalin (Slavova et al., 2018). Second, anticonvulsant analgesics when administrated with opioids appear to reinforce the activation of dopaminergic rewarding system in the brain, enforcing opioid adverse effects, such OUD/OD (Vashchinkina et al., 2018; Baird et al., 2014). Adding to prior research (Evoy et al., 2017; Gomes et al., 2018), our study found increasing receipt of anticonvulsant analgesics prior to OUD/OD diagnosis. Whether this association is an artifact of increasing pain regimen augmentation with gabapentinoids to supplement reduced opioid doses or whether gabapentinoids are indeed preferentially used by patients who develop OUD or OD needs to be examined in future studies that include individuals with or without the diagnosis. Importantly, building on these findings, compartmentalized efforts that either focus on comprehensive assessment of prescription pattern using healthcare data or employ patient interview to capture misuse ought to be joined to fully understand the rapidly evolving interplay between clinically-guided and illicit opioid use resulting in OUD/OD.
During the same 11-year period, we also observed a decreasing trend in receipt of TCAs, SNRIs, and muscle relaxants, especially among adult patients with OUD or OD. Although decreases in the use of muscle relaxants may be attributable to similar concerns about abuse potential, which has resulted in the rescheduling of carisoprodol (Reeves et al., 2012), the reasons for decreases in TCA and SNRI prescriptions are unclear. Again, further research should examine whether the same trends apply to patients with chronic pain who do not develop adverse opioid-related outcomes.
The present study also examined the incidence of diagnosed OUD/OD in inpatient or outpatient settings and found an overall increase by more than 3-fold during the examined years. The observed increasing incidence may be partly attributable to increasing opioid prescriptions (Dowell et al., 2016), although the prescribing rates have dropped since 2011 (Guy et al., 2017). Other analyses have suggested increasing contributions of the growing supply of cheap and potent illicit opioids (including heroin and synthetic fentanyl) (Compton et al., 2016; Unick et al., 2014), which have been responsible for 40% of opioid-related overdose deaths in recent years (O’Donnell et al., 2017). Alternatively, the increase in the incidence of diagnosed OUD/OD may reflect greater clinical awareness and readiness to diagnose (and then treat) patients with OUD, which have been greatly promoted by national policies and guidelines in recent years (Madras 2017; Dowell et al., 2016; Soelberg et al., 2017).
Of note in the present study is the finding of a significant increase in OUD or OD incidence among older adults who purchased Medicare supplemental insurance, representing appropriately 23% of the Medicare fee-for-service population (The Henry J. Kaiser Family Foundation 2017). Our observation is supported by 2006 to 2014 data from US poisoning centers that have indicated an increasing misuse of prescription opioids and associated fatal and nonfatal overdoses among adults aged 60 or older (West et al., 2015; West et al., 2016). Older adults are the largest consumers of prescription opioids, in part due to the high prevalence of chronic pain reported in this age group (Reid et al., 2015). Physiological and psychosocial changes contribute additional risk factors to this vulnerable population (Reid et al., 2015; Park et al., 2010), although opioid use trajectories and risk factors for OUD/OD in older populations are relatively understudied. Our findings of both the steep rise and peak incidence of OUD/OD in older adults as compared with younger adults underscores the importance of understanding mechanisms and risk factors unique to this population, especially among women aged 65 to 74 years, who presented the highest incidence in this study.
Using a large population of commercially insured patients, this study evaluated trends of OUD or OD over the last decade in the context of clinical pain management. Our findings raise important concerns about future trends in adverse opioid-related outcomes that may not be addressable with increasing restrictions in opioid prescribing.
Several limitations of this study should be noted. First, assessment of OUD and opioid-related overdose relied on billing records. During the study period, the number of opioid-related diagnosis codes increased from 20 ICD-9-CM codes to 100 ICD-10-CM codes, resulting in an accompanying surge of OUD/OD diagnoses following the newer coding system in October 2015 (Heslin et al., 2017). This notwithstanding, our incidence data showed a steady upward trend throughout the study period and differential increases in older adults, which are unlikely attributable to changes in the coding system. Second, we did not examine types of pain, which may affect the composition of pain regimens, including adjuvant therapy (eg, gabapentinoids are recommended for treatment of neuropathic pain). Third, our data did not capture individuals with OUD who did not seek medical care or individuals with fatal overdoses; thus, underestimation of both outcomes is likely. Our data also did not include prescription drugs paid for by sources other than the Commercial and Medicare supplemental insurance that patients purchased. Finally, our findings are generalizable only to the US privately insured population and need to be confirmed in other populations.
6. Conclusions
In a US commercially insured population, incidence of diagnosed OUD/OD increased by more than 3-fold between 2006 and 2016, with the greatest increase observed among older adults. The proportion of patients with incident OUD/OD receiving high-dose prescription opioids before the diagnosis decreased overtime time, while the proportion of patients receiving anticonvulsant analgesics increased. These contrasting trends warrant further investigation to understand how the use of prescribed opioids and anticonvulsants for treatment of pain conditions among high-risk patients is shifting.
Supplementary Material
Highlights.
Reducing opioid prescribing may alter pain medication use for OUD/OD patients.
Decreasing OUD/OD patients had prescription opioids in the year before diagnosis.
Increasing OUD/OD patients had anticonvulsants in the year before diagnosis.
Discerning how prescribed opioids and anticonvulsants may cause OUD/OD is needed.
Acknowledgments
Role of Funding Source
Funding/Support: This project had no direct funding. Dr. Wei is supported in part by a National Institutes of Health/National Institute on Aging (NIH/NIA) Mentored Research Scientist Award (K01AG054764).
Role of the Funder/Sponsor: The National Institute on Aging had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication.
Footnotes
Conflict of Interest
No conflict declared.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication, As a service to our customers we are providing this early version of the manuscript, The manuscript will undergo copyediting, typesetting, and review of the resulting proof, before it is published in its final form. Please note that during the production process, errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Baird CR, Fox P, and Colvin LA 2014. ‘Gabapentinoid abuse in order to potentiate the effect of methadone: a survey among substance misusers’, Eur Addict Res, 20: 115–8. [DOI] [PubMed] [Google Scholar]
- Brune K, and Patrignani P 2015. ‘New insights into the use of currently available non-steroidal anti-inflammatory drugs’, J Pain Res, 8: 105–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton WM, Jones CM, and Baldwin GT 2016. ‘Relationship between Nonmedical Prescription-Opioid Use and Heroin Use’, N Engl J Med, 374: 154–63. [DOI] [PubMed] [Google Scholar]
- Dowell D, Haegerich TM, and Chou R 2016. ‘CDC Guideline for Prescribing Opioids for Chronic Pain - United States, 2016’, MMWR Recomm Rep, 65: 1–49. [DOI] [PubMed] [Google Scholar]
- Dufour R, Joshi AV, Pasquale MK, Schaaf D, Mardekian J, Andrews GA, and Patel NC 2014. ‘The prevalence of diagnosed opioid abuse in commercial and Medicare managed care populations’, Pain Pract, 14: E106–15. [DOI] [PubMed] [Google Scholar]
- Evoy KE, Morrison MD, and Saklad SR 2017. ‘Abuse and Misuse of Pregabalin and Gabapentin’, Drugs, 77: 403–26. [DOI] [PubMed] [Google Scholar]
- Gomes T, Greaves S, van den Brink W, Antoniou T, Mamdani MM, Paterson JM, Martins D, and Juurlink DN 2018. ‘Pregabalin and the Risk for Opioid-Related Death: A Nested Case-Control Study’, Annals of internal medicine. [DOI] [PubMed] [Google Scholar]
- Green CA, Perrin NA, Janoff SL, Campbell CI, Chilcoat HD, and Coplan PM 2017. ‘Assessing the accuracy of opioid overdose and poisoning codes in diagnostic information from electronic health records, claims data, and death records’, Pharmacoepidemiology and drug safety, 26: 509–17. [DOI] [PubMed] [Google Scholar]
- Guy GP Jr., Zhang K, Bohm MK, Losby J, Lewis B, Young R, Murphy LB, and Dowell D 2017. ‘Vital Signs: Changes in Opioid Prescribing in the United States, 2006–2015’, MMWR. Morbidity and mortality weekly report, 66: 697–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadland SE, Wharam JF, Schuster MA, Zhang F, Samet JH, and Larochelle MR 2017. ‘Trends in Receipt of Buprenorphine and Naltrexone for Opioid Use Disorder Among Adolescents and Young Adults, 2001–2014’, JAMA Pediatr, 171: 747–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han B, Compton WM, Blanco C, Crane E, Lee J, and Jones CM 2017. ‘Prescription Opioid Use, Misuse, and Use Disorders in U.S. Adults: 2015 National Survey on Drug Use and Health’, Annals of internal medicine, 167: 293–301. [DOI] [PubMed] [Google Scholar]
- Hasin DS, O’Brien CP, Auriacombe M, Borges G, Bucholz K, Budney A, Compton WM, Crowley T, Ling W, Petry NM, Schuckit M, and Grant BF 2013. ‘DSM-5 criteria for substance use disorders: recommendations and rationale’, Am J Psychiatry, 170: 834–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helsel DR, and Hirsch RM. 2002. ‘Chapter 12: Trend Analysis’ in, Statistical Methods in Water Resources. [Google Scholar]
- Heslin KC, Owens PL, Karaca Z, Barrett ML, Moore BJ, and Elixhauser A 2017. ‘Trends in Opioid-related Inpatient Stays Shifted After the US Transitioned to ICD-10-CM Diagnosis Coding in 2015’, Med Care, 55: 918–23. [DOI] [PubMed] [Google Scholar]
- Kirson NY, Shei A, Rice JB, Enloe CJ, Bodnar K, Birnbaum HG, Holly P, and Ben-Joseph R 2015. ‘The Burden of Undiagnosed Opioid Abuse Among Commercially Insured Individuals’, Pain medicine, 16: 1325–32. [DOI] [PubMed] [Google Scholar]
- Lyndon A, Audrey S, Wells C, Burnell ES, Ingle S, Hill R, Hickman M, and Henderson G 2017. ‘Risk to heroin users of polydrug use of pregabalin or gabapentin’, Addiction, 112: 1580–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madras BK 2017. ‘The Surge of Opioid Use, Addiction, and Overdoses: Responsibility and Response of the US Health Care System’, JAMA Psychiatry, 74: 441–42. [DOI] [PubMed] [Google Scholar]
- O’Donnell JK, Gladden RM, and Seth P 2017. ‘Trends in Deaths Involving Heroin and Synthetic Opioids Excluding Methadone, and Law Enforcement Drug Product Reports, by Census Region - United States, 2006–2015’, MMWR. Morbidity and mortality weekly report, 66: 897–903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park J, and Lavin R 2010. ‘Risk factors associated with opioid medication misuse in community-dwelling older adults with chronic pain’, The Clinical journal of pain, 26: 647–55. [DOI] [PubMed] [Google Scholar]
- Reeves RR, Burke RS, and Kose S 2012. ‘Carisoprodol: update on abuse potential and legal status’, South Med J, 105: 619–23. [DOI] [PubMed] [Google Scholar]
- Reid MC, Eccleston C, and Pillemer K 2015. ‘Management of chronic pain in older adults’, BMJ, 350: h532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roland CL, Joshi AV, Mardekian J, Walden SC, and Harnett J 2013. ‘Prevalence and cost of diagnosed opioid abuse in a privately insured population in the United States’, J Opioid Manag, 9: 161–75. [DOI] [PubMed] [Google Scholar]
- Rudd RA, Aleshire N, Zibbell JE, and Gladden RM 2016. ‘Increases in drug and opioid overdose deaths--united states, 2000–2014’, MMWR. Morbidity and mortality weekly report, 64: 1378–82. [DOI] [PubMed] [Google Scholar]
- Satish R, Kandasamy A, Jayarajan D, and Benegal V 2015. ‘Gabapentin dependence in a patient with opioid dependence syndrome’, J Neuropsychiatry Clin Neurosci, 27: e64. [DOI] [PubMed] [Google Scholar]
- Schuchat A, Houry D, and Guy GP Jr. 2017. ‘New Data on Opioid Use and Prescribing in the United States’, Jama, 318: 425–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavova S, Miller A, Bunn TL, White JR, Kirschke D, Light T, Christy D, Thompson G, and Winecker R 2018. ‘Prevalence of gabapentin in drug overdose postmortem toxicology testing results’, Drug and alcohol dependence, 186: 80–85. [DOI] [PubMed] [Google Scholar]
- Smith RV, Havens JR, and Walsh SL 2016. ‘Gabapentin misuse, abuse and diversion: a systematic review’, Addiction, 111: 1160–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith RV, Lofwall MR, and Havens JR 2015. ‘Abuse and diversion of gabapentin among nonmedical prescription opioid users in Appalachian Kentucky’, Am J Psychiatry, 172: 487–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soelberg CD, Brown RE Jr., Du Vivier D, Meyer JE, and Ramachandran BK 2017. ‘The US Opioid Crisis: Current Federal and State Legal Issues’, Anesth Analg, 125: 1675–81. [DOI] [PubMed] [Google Scholar]
- The Henry J Kaiser Family Foundation. 2017. ‘An Overview of Medicare’, Accessed on July 23 https://www.kff.org/medicare/issue-brief/an-overview-of-medicare/.
- Throckmorton DC, Gottlieb S, and Woodcock J 2018. ‘The FDA and the Next Wave of Drug Abuse - Proactive Pharmacovigilance’, N Engl J Med, 379: 205–07. [DOI] [PubMed] [Google Scholar]
- Unick G, Rosenblum D, Mars S, and Ciccarone D 2014. ‘The relationship between US heroin market dynamics and heroin-related overdose, 1992–2008’, Addiction, 109: 1889–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vashchinkina E, Piippo O, Vekovischeva O, Krupitsky E, Ilyuk R, Neznanov N, Kazankov K, Zaplatkin I, and Korpi ER 2018. ‘Addiction-related interactions of pregabalin with morphine in mice and humans: reinforcing and inhibiting effects’, Addict Biol, 23: 945–58. [DOI] [PubMed] [Google Scholar]
- West NA, and Dart RC 2016. ‘Prescription opioid exposures and adverse outcomes among older adults’, Pharmacoepidemiology and drug safety, 25: 539–44. [DOI] [PubMed] [Google Scholar]
- West NA, Severtson SG, Green JL, and Dart RC 2015. ‘Trends in abuse and misuse of prescription opioids among older adults’, Drug and alcohol dependence, 149: 117–21. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.