Objectives:
Burnout tends to be high in ICU settings. Stressors include serious patient illness, round-the-clock acute events, and end-of-life (nonbeneficial) care. We report on an ICU with very low burnout scores. We sought to understand factors that might be responsible for these favorable outcomes.
Design:
We compared ICU scores on burnout and its predictors with scores in non-ICU providers, merging scores in four ICUs (burn, medical, surgical, and pediatrics). Analyses included descriptive statistics, as well as general estimating equations to assess odds of burnout in ICU clinicians versus non-ICU clinicians.
Setting:
Annual wellness survey performed in October 2017 at Hennepin Healthcare System, an integrated system of care that includes an urban safety net hospital in Minneapolis, MN.
Subjects:
Six-hundred seventy-nine providers (physicians and advanced practice providers).
Interventions:
None.
Measurements and Main Results:
Annual surveys are performed using the validated Mini-Z 10 item wellness instrument. The Mini-Z assesses stress, satisfaction, and burnout, as well as known predictors including work control, chaos, teamwork, values alignment, and electronic medical record-related stress. Response rate in ICUs was 70% (64% elsewhere). Ten percentage of ICU clinicians reported burnout versus 37% of other providers (p = 0.015). ICUs were characterized as having lower chaos, less stress, and very high teamwork and values alignment between clinicians and leaders. Odds of burnout were four times lower in ICU clinicians (odds ratio, 0.24; 95% CI, 0.06–0.96; p = 0.043). Of all Hennepin Healthcare System providers, those with values not aligned with leaders had 3.28 times the odds of burnout (95% CI, 1.92–5.59; p < 0.001).
Conclusions:
Low burnout can be present in a busy, safety net ICU. Explicitly aligning values between clinicians and leaders may hold promise as a remediable worklife factor for producing these favorable results.
Keywords: chaos, intensive care, physician burnout, teamwork, values, work conditions
The ICU setting is described as one where providers have a very high prevalence of burnout (recent reported rates 6–47%) with the largest studies demonstrating a prevalence of 28–61% (1). Although defining burnout still lacks uniformity, it is clear that burnout is a threat to both quality care for patients and provider wellness. It has become the fourth element of the quadruple aim due to its interrelatedness with patient experience, value, and population health.
Risk factors contributing to provider burnout have included individual and organizational factors. Generally, lack of control over workload, chaos, time pressure related to documentation burden, and insufficient support have been noted to contribute to burnout (2). The ICU literature describes younger age, female gender, single marital status/no children, and fewer years’ experience as risk factors for stress and burnout (1). Excessive night shifts and working hours and longer periods of time between days off are associated with higher burnout scores (3). Conflict with colleagues, nurses, or patient families is also associated with higher burnout (3, 4). Ethical issues and end-of-life decision-making have been described as risk factors for providers and are also associated with higher intent to leave the job (3–5). A common phenomenon of end-of-life decision-making, moral distress, is experienced by a provider when he/she knows the ethical and appropriate action to take but feels constrained from enacting the specific action. Typically, moral distress in providers arises from providing nonbeneficial care near the end of life and this is highly associated with severe burnout (6). In one study, inappropriate care (usually “too much” care that is perceived as nonbeneficial) was described by 32% of physicians and was associated with intent to leave the job (7). Activities such as participating in an ICU research group and maintaining professional activities outside the ICU have been described to be protective (3, 4). The presence of efficient teamwork and values alignment may be important as protective factors (2).
Hennepin Healthcare System (HHS) conducts an annual wellness survey of all providers to help inform action at the departmental and divisional levels. Critical care providers cross departments that made the assessment of burnout in ICUs difficult to ascertain. This study was designed to evaluate predictors and overall burnout rates in ICU providers and compare to non-ICU providers at HHS and Hennepin County Medical Center (HCMC), a safety net hospital system in Minneapolis, MN.
MATERIALS AND METHODS
All 679 HHS providers (physicians, psychologists, dentists, and advanced practice providers, including nurse practitioners and physician assistants) were surveyed in October 2017. Critical care providers in the surgical ICU (SICU), burn ICU, medical ICU (MICU), and PICU were evaluated. At the time of the survey, there were 7 MICU providers and 17 SICU/burn ICU providers. There are 72 ICU beds with flexibility for overflow. HHS is a level 1 trauma center and teaching hospital with both closed (MICU and PICU) and open ICU structures (SICU). Closed ICU structures have a single team as the primary team, and open units may have multiple teams comanaging the patient; an example would be a neurosurgical patient with a critical care consultant. The SICU providers surveyed included trauma surgery, neurosurgery, and cardiothoracic surgery. There is 24-hour in-hospital coverage for the ICUs.
Assessment was conducted using the validated Mini-Z 10 item worklife questionnaire assessing stress, satisfaction, burnout, control over workload, time for documentation, chaos in work atmosphere, values alignment with leadership, and teamwork efficiency (2). These stressors in the Mini-Z have been shown to correlate with burnout as defined by the Maslach Burnout Inventory (8). A question on nonbeneficial care was added for ICU providers to assess for possible moral distress. Burnout was measured with a validated single-item metric, which is a 5-point scale question. It has been highly correlated with the emotional exhaustion scale on the Maslach Burnout Inventory (9). chi-square and Fisher exact tests were used to test for independence among responses in ICU versus non-ICU providers, general estimating equations with robust ses assessed the odds of burnout in each location (ICU vs hospital), adjusted for teamwork (poor/marginal vs satisfactory/optimal), and values alignment (not aligned vs aligned). Further consideration was put on also adjusting the model for gender, but based on the extensive subject matter expertise; we concluded that there is no enough evidence that gender is confounding the relationship between burnout and location.
Upon completion of the survey, the authors met with providers to discuss the results of the survey including commentary about risks for burnout and protective factors. Field notes were transcribed from those conversations and then evaluated for themes or common sentiments by two reviewing authors. If the factor was mentioned by more than one group, it was noted.
RESULTS
Of 30 providers in the SICU, MICU, burn ICU, and PICU, 21 providers responded (70% response rate). Response rate for the other 649 HCMC providers surveyed was 64%. In non-ICU providers, there were 59% of women and 40% of men versus 23% of women and 76% of men in the ICU respondents.
Burnout in ICUs was low (10%) compared with a 36% overall provider burnout rate (p < 0.05). ICU job satisfaction was high (95% were satisfied). Teamwork efficiency and values alignment were also high, each endorsed by 95% of ICU respondents. Chaotic environments were noted by a minority of ICU providers (40%), and control of workload in the ICU was reasonable (satisfactory or positive) in 70%. Full results are shown in Table 1.
TABLE 1.
Burnout Predictors and Clinician Outcomes in Hennepin Healthcare ICUs Versus Overall Provider Group
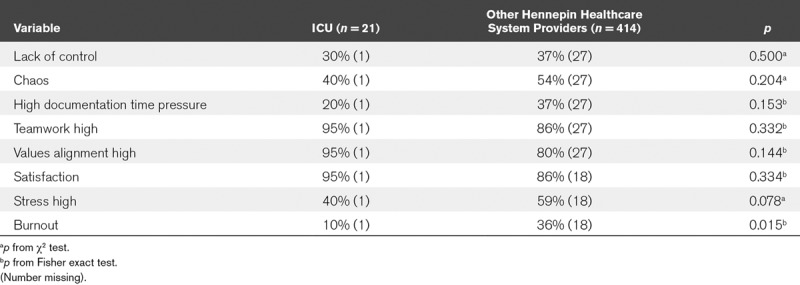
Odds of burnout were four times lower for those working in ICUs (odds ratio [OR], 0.24; 95% CI, 0.06–0.96; p = 0.043). Values alignment with departmental leadership was strongly associated with burnout in all providers; odds of burnout for those with values not aligned were 3.28 times that of the odds if values were aligned (95% CI, 1.92–5.59; p < 0.001), holding other variables constant. Teamwork did not have a significant effect on odds of burnout (OR of burnout with poor or marginal teamwork 1.36; 95% CI, 0.75–2.47; p = 0.31).
Ten percentage of ICU providers reported providing frequent nonbeneficial care, with 30% of providers in the MICU endorsing “often” or “always” providing nonbeneficial care. Qualitative information gathered from field notes included a recurring theme that none of the ICU physicians practiced exclusively in the ICU and that variety of clinical activities was helpful in avoiding burnout. Teamwork and collegiality were also described as burnout mediators.
DISCUSSION
In this study of four ICUs in a safety net hospital, we found a surprisingly low rate of overall burnout, despite a moderately high rate of providing nonbeneficial care in one of the ICUs. Odds of burnout in HHS ICU providers were four times lower than in non-ICU providers. Many stressors, again somewhat surprisingly, appeared to be more favorable in the ICUs, with less chaos, more work control, and less concerns about time pressure due to documentation. Variety in work was also endorsed as a moderator of ICU burnout. Values alignment was strongly protective from burnout in all HHS settings.
Values alignment, the one predictor that emerged from the multivariate analysis as associated with burnout in all providers, may speak to collegiality and clarity of purpose among leaders. Values alignment can be defined as the degree to which providers feel that their purpose or the mission that drives their work is reflected in their leaders. Examples of this alignment may include collaborative decision-making among providers and leadership, and leadership being responsive to changes desired by providers. The literature supports the association of high values alignment and low burnout. In a 2016 study, a unit described as the “best practices site” reported satisfaction in 95% of providers and high values alignment in 90% of providers (2). Additionally, high values alignment has been shown to correlate with improved patient outcomes. A 2009 study found fewer total, prevention, and diabetes care errors in clinics with high values alignment (10). A collegial culture in HHS ICUs where providers feel bonded by strong organizational values can therefore be linked to their high values alignment and low burnout scores.
Teamwork, work control, and chaos seemed more favorable in ICUs, although these differences were not statistically significant, perhaps due to small sample sizes of ICU providers. The importance of teamwork is reflected in the qualitative data, which indicates an organizational culture of collegiality and open communication in the ICUs. The literature supports that conflict among providers, ineffective communication, and a lack of teamwork, especially in ICU settings, are correlated with high burnout. A 2007 study of 978F intensivists found a 46.5% rate of burnout, with one of the determinants being impaired relationships between the providers. In this study, high-quality relationships between providers were associated with decreased burnout (3). Another study demonstrated that up to 70% of intensivists reported conflict in the ICU. The majority of that conflict was related to communication and teamwork, with about one-third of the conflicts being between ICU staff and patients/relatives. This conflict was associated with greater job strain (11). Teamwork with leadership for interdisciplinary decision-making is also thought to promote a superior ethical climate, which may be associated with less perception of excessive care (12).
Qualitative comments collected from field notes during debriefing added a finding that all ICU providers at HHS maintained clinical activities outside the ICU such as clinic, non-ICU hospital care, administrative work, teaching, and research. This was mentioned as a “protective factor” by multiple providers. The concept of working in another capacity outside of the ICU as being protective was first described in a multicenter Brazilian study (4). This finding warrants further study.
The perception of having to provide frequent nonbeneficial care among providers in all four ICUs was relatively low overall (10%) but was more prevalent (30%) in the MICU. Nonbeneficial treatment and moral distress are related but not equivalent concepts; both are known to be associated with burnout. Providing nonbeneficial treatment is strongly associated with emotional exhaustion and intent to leave the job (7). In another study, burnout was two times that in providers who perceived moral distress from providing more interventions than were thought clinically appropriate (6).
Conclusions of our work are limited by the small number of ICU providers and the single setting of the survey. The survey is anonymous, so demographics and analysis of potential confounding factors is limited. The observational and cross-sectional nature of the survey does not allow establishing causality. In addition, burnout is not static and is subject to change over time. Survey data are notoriously biased with participation bias, recall bias, and participation bias. Strengths of the study include the use of validated measures. The single-item burnout question correlates highly with the emotional exhaustion domain on the Maslach Burnout Inventory (9). If anything, it underestimates burnout but would be symmetric for all respondents. The use of the Mini-Z for wellness monitoring at HHS is a mature program with a well-established infrastructure for survey administration, data analysis, and interpretation and subsequent action plan for burnout reduction. The high response rates for the survey may have been due to several factors. First, there is a diligent effort to assure anonymity and privacy for respondents, which is appreciated by the faculty. Second, surveyed providers are reminded by email, thanked for participation, and updated on survey completion rates. Third, there is departmental support for the survey with reminders for providers to perform the survey. Fourth, and most importantly, the overall information is shared through the organization with all faculty; each department chair and division chief also receive reports about burnout in their areas and collaborate with the Office of Professional Worklife to form an action plan to address burnout.
CONCLUSIONS
We conclude that burnout can, in spite of a stressful environment, be low in ICUs. Protective factors may include values alignment, a more collegial and reasonably paced environment, and more variety in work activities. We propose larger studies in multiple ICU settings to explore the role of these predictors in promoting professional satisfaction and preventing ICU-related burnout. Additionally, we would advocate for collecting enriched data including more demographics detail about previously described risk factors and objective indicators of burnout such as days away from work, quality and safety, and departures from the clinical setting.
Footnotes
This research was supported by the National Institutes of Health’s National Center for Advancing Translational Sciences, grant UL1TR002494.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health’s National Center for Advancing Translational Sciences.
The authors have disclosed that they do not have any potential conflicts of interest.
REFERENCES
- 1.Chuang CH, Tseng PC, Lin CY, et al. Burnout in the intensive care unit professionals: A systematic review. Medicine (Baltimore) 2016; 95:e5629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Linzer M, Poplau S, Babbott S, et al. Worklife and wellness in academic general internal medicine: Results from a national survey. J Gen Intern Med 2016; 31:1004–1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Embriaco N, Papazian L, Kentish-Barnes N, et al. Burnout syndrome among critical care healthcare workers. Curr Opin Crit Care 2007; 13:482–488. [DOI] [PubMed] [Google Scholar]
- 4.Teixeira C, Ribeiro O, Fonseca AM, et al. Burnout in intensive care units - a consideration of the possible prevalence and frequency of new risk factors: A descriptive correlational multicentre study. BMC Anesthesiol 2013; 13:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Galván ME, Vassallo JC, Rodríguez SP, et al. ; Members of Clinical and Epidemiological Research Group in Pediatric Intensive Care Units - Sociedad Argentina de Pediatría Professional burnout in pediatric intensive care units in argentina. Arch Argent Pediatr 2012; 110:466–473. [DOI] [PubMed] [Google Scholar]
- 6.Fumis RRL, Junqueira Amarante GA, de Fátima Nascimento A, et al. Moral distress and its contribution to the development of burnout syndrome among critical care providers. Ann Intensive Care 2017; 7:71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schwarzkopf D, Rüddel H, Thomas-Rüddel DO, et al. Perceived nonbeneficial treatment of patients, burnout, and intention to leave the job among ICU nurses and junior and senior physicians. Crit Care Med 2017; 45:e265–e273. [DOI] [PubMed] [Google Scholar]
- 8.Olson K, Sinsky C, Rinne, et al. Cross-sectional survey of workplace stressors associated with physician burnout measured by the Mini-Z and the Maslach Burnout Inventory. Stress Health 2019; 35:157–175. [DOI] [PubMed] [Google Scholar]
- 9.Rohland BM, Kruse GR, Rohrer JE.Validation of a single-item measure of burnout against the Maslach Burnout Inventory among physicians. Stress Health 2004; 20:75–79. [Google Scholar]
- 10.Linzer M.Working conditions in primary care: Physician reactions and care quality. Ann Intern Med 2009; 151:28. [DOI] [PubMed] [Google Scholar]
- 11.Azoulay E, Timsit JF, Sprung CL, et al. ; Conflicus Study Investigators and for the Ethics Section of the European Society of Intensive Care Medicine Prevalence and factors of intensive care unit conflicts: The conflicus study. Am J Respir Crit Care Med 2009; 180:853–860. [DOI] [PubMed] [Google Scholar]
- 12.Benoit DD, Jensen HI, Malmgren J, et al. ; DISPROPRICUS study group of the Ethics Section of the European Society of Intensive Care Medicine Outcome in patients perceived as receiving excessive care across different ethical climates: A prospective study in 68 intensive care units in Europe and the USA. Intensive Care Med 2018; 44:1039–1049. [DOI] [PMC free article] [PubMed] [Google Scholar]


