Abstract
Niemann-Pick C1 (NPC1), a host receptor involved in the envelope glycoprotein (GP)–mediated entry of filoviruses into cells, is believed to be a major determinant of cell susceptibility to filovirus infection. It is known that proteolytically digested Ebola virus (EBOV) GP interacts with 2 protruding loops in domain C of NPC1. Using previously published structural data and the National Center for Biotechnology Information Single-Nucleotide Polymorphism (SNP) database, we identified 10 naturally occurring missense SNPs in human NPC1. To investigate whether these SNPs affect cell susceptibility to filovirus infection, we generated Vero E6 cell lines stably expressing NPC1 with SNP substitutions and compared their susceptibility to vesicular stomatitis virus pseudotyped with filovirus GPs and infectious EBOV. We found that some of the substitutions resulted in reduced susceptibility to filoviruses, as indicated by the lower titers and smaller plaque/focus sizes of the viruses. Our data suggest that human NPC1 SNPs may likely affect host susceptibility to filoviruses.
Keywords: Ebolavirus, Marburgvirus, Niemann-Pick C1 (NPC1), single-nucleotide polymorphism (SNP), NPC1-knockout Vero E6 (Vero E6/NPC1-KO)
Viruses in the Ebolavirus and Marburgvirus genera are members of the family Filoviridae and cause severe hemorrhagic fever in humans and nonhuman primates. Filoviridae consists of 3 genera, encompassing 7 species (5, 1, and 1 species in the genera Ebolavirus, Marburgvirus, and Cuevavirus, respectively) [1]. Currently, 8 distinct viruses are assigned to these 7 species: Ebola virus (EBOV), Bundibugyo virus (BDBV), Taï Forest virus (TAFV), Sudan virus (SUDV), and Reston virus (RESTV) in the genus Ebolavirus; Marburg virus (MARV) and Ravn virus (RAVV) in the genus Marburgvirus; and Lloviu virus (LLOV) in the genus Cuevavirus. The biological properties of LLOV are uncharacterized since infectious LLOV has not been isolated yet. Filoviruses have continuously produced sporadic outbreaks, with an increased frequency in Central and West Africa, and are considered a significant public health concern.
The envelope glycoprotein (GP) is the only viral surface protein of filoviruses and mediates viral entry into cells [2]. After binding to attachment factors such as C-type lectins [3, 4], virus particles are internalized into host cells via macropinocytosis [5–7]. Late endosomal low pH leads to cysteine protease-mediated proteolysis of the viral GP [8, 9]. This digested GP (dGP) can then interact with the host endosomal fusion receptor, Niemann-Pick C1 (NPC1), allowing fusion between the viral envelope and the host endosomal membrane [10–12]. Thus, NPC1 represents a major determinant of cell susceptibility to filovirus infection [13, 14].
The recently published costructures of EBOV dGP in complex with NPC1 revealed that 2 surface-exposed loops on NPC1 mediate the interaction with dGP [15, 16]. Biochemical analysis of purified NPC1 and dGP has further shown that amino acid substitutions (eg, P424A, F503G, and F504G) in these 2 loops reduce the binding to dGP [15]. This finding led us to hypothesize that single-nucleotide polymorphisms (SNPs) in human NPC1 might influence host susceptibility to filovirus infection. Mutations tested in previous studies [13–15] were not linked to human NPC1 SNPs and are unregistered in the National Center for Biotechnology Information (NCBI) SNP database (available at: https://www.ncbi.nlm.nih.gov/snp/); thus, it remains unknown whether naturally occurring SNPs found in human NPC1 can affect the efficiency of filovirus infection.
Using a structural-guided approach to the SNP database, we identified 10 missense SNPs in the GP-interacting loop regions of NPC1. To investigate the potential effects of these substitutions on filovirus infection in vitro, we generated an NPC1-knockout Vero E6 cell line and established stable cell lines expressing the NPC1 SNP mutants. Cell susceptibility was examined using vesicular stomatitis virus (VSV) pseudotyped with filovirus GPs [2, 17], as well as a replication-competent EBOV expressing green fluorescent protein (GFP) [18]. Here, we report human NPC1 SNPs that influence the susceptibility of cells to filovirus entry and infection.
MATERIALS AND METHODS
Viruses
VSVs containing the GFP gene instead of the receptor-binding VSV G protein gene (VSV∆G) and pseudotyped viruses with GPs of EBOV (Mayinga), BDBV (Butalya), TAFV (Pauléoula), SUDV (Boniface), RESTV (Pennsylvania), MARV (Angola), RAVV (Kitum Cave), and LLOV (Asturias), designated by VSV∆G-EBOV, -BDBV, -TAFV, -SUDV, -RESTV, -MARV, -RAVV, and -LLOV, respectively, were generated as described previously [2, 19]. Infectious units (IUs) of these pseudotyped VSVs were determined in Vero E6 cells as previously described [2, 20]. Replication-competent recombinant VSVs (rVSV-EBOV [Mayinga] and rVSV-MARV [Angola]) were generated as described previously [17]. rVSV-EBOV, rVSV-MARV, and recombinant EBOV expressing GFP (EBOV-GFP) [18] were propagated in Vero E6 cells and stored at −80°C. Infectivity of rVSV-EBOV, rVSV-MARV, and EBOV-GFP in each cell line was determined by plaque- and focus-forming assays, respectively, as described previously [21, 22]. Relative infectivity in each cell line was calculated by setting IUs, plaque-forming units, or focus-forming units given by Vero E6 cells expressing 293T-NPC1 to 100%.
Biosafety
All infectious work with EBOV-GFP was performed in the biosafety level 4 laboratory at the Integrated Research Facility of the Rocky Mountain Laboratories, Division of Intramural Research, National Institute of Allergy and Infectious Diseases, National Institutes of Health (NIH; Hamilton, MT). All standard operating procedures were approved by the NIH Institutional Biosafety Committee.
Cell Lines
Vero E6, NPC1-knockout Vero E6 (Vero E6/NPC1-KO), and HEK293T-derived Platinum-GP (Plat-GP) cells [23] (Cell Biolabs) were grown in Dulbecco’s modified Eagle’s medium (Sigma-Aldrich) supplemented with 10% fetal calf serum. Vero E6/NPC1-KO cells were generated by previously described methods [24, 25] with a few modifications and were transduced with retroviruses expressing HEK293T-derived NPC1 and its mutant genes (Supplementary Materials and Methods).
Cloning of the NPC1 Gene into Plasmids
The coding region of the HEK293T NPC1 gene was amplified by polymerase chain reaction (PCR) analysis from complementary DNA prepared from total RNA extracted from HEK293T cells according to a previous study [26]. The PCR product was cloned into a murine leukemia virus–based retroviral vector, pMXs-puro [23]. Ten SNPs found in the 2 loops—rs772847092 (I419V and I419F), rs77815278 (Y420S), rs771644708 (Y420H), rs143797098 (P424A), rs140149624 (S425L), rs749078710 (A427T), rs748246747 (G500E), rs191537721 (D502E), and rs756587493 (D508N)—were produced by site-directed mutagenesis using a KOD-Plus-Neo polymerase (TOYOBO) with primers containing the desired nucleotide substitutions. All mutations were confirmed by DNA sequencing.
Statistical Analysis
All statistical analyses were performed using R software (version 3.2.3) [27]. Correlations between transcription and expression levels of NPC1 were estimated using the rank correlation coefficient of Spearman (rs). For comparison of viral infectivity and plaque/focus size, one-way analysis of variance, followed by the Dunnett test, and the Welch t test were used. P values of <.05 were considered to be statistically significant.
RESULTS
Structure-Guided Approach to Identifying Candidate NPC1 SNPs
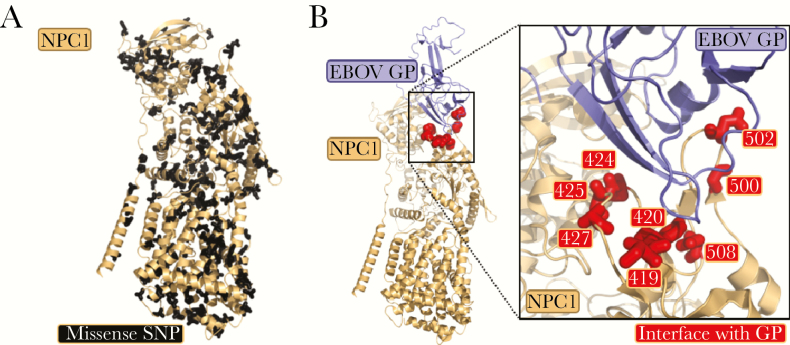
Human NPC1 has at least 254 unique SNPs listed in the NCBI SNP database. Of these SNPs, 222 are missense, resulting in amino acid changes, and they are widely distributed throughout the structure of NPC1 (Figure 1A). Using the costructure of full-length NPC1 and EBOV dGP [16], we identified 10 missense SNPs in 8 amino acid positions located in the interface (ie, 2 loop structures at amino acid positions 419–428 and 500–508) with EBOV GP (Figure 1B).
Figure 1.
Structural-guided approach to human Niemann-Pick C1 (NPC1) single-nucleotide polymorphism (SNP) selection. A, A total of 222 missense SNPs are represented in black on the structure from NPC1. B, Costructure of Ebola virus (EBOV) glycoprotein (GP; blue) and NPC1 (tan), with amino acid positions of SNPs indicated in red (Protein Data Bank identifier 5JNX) [16].
Human NPC1 Polymorphisms Affecting Filovirus Entry Into Cells
We next established an NPC1-knockout Vero E6 cell line, Vero E6/NPC1-KO cl.19 (Supplementary Figure 1A and 1B), and confirmed that its susceptibility to VSV∆G- EBOV, rVSV-EBOV, and EBOV-GFP was abolished (Supplementary Figure 1C–E). The Vero E6/NPC1-KO cl.19 cells were then transduced with a retroviral vector, resulting in 11 different cell lines stably expressing wild-type human NPC1 (293T-NPC1) or NPC1 SNP mutants (I419V, I419F, Y420S, Y420H, P424A, S425L, A427T, G500E, D502E, and D508N). Introducing the wild-type NPC1 gene into the knockout cells completely restored the susceptibility to filovirus entry and infection (Supplementary Figure 1C–E), as has been shown with NPC1-deficient Chinese hamster ovary cells and reptile-derived cells [10, 12]. Transcription and expression levels of the transduced NPC1 genes were examined by quantitative PCR and Western blot analyses, respectively (Supplementary Materials and Methods). For all NPC1 SNP mutant cell lines, expression levels of NPC1 were equivalent to or higher than those of 293T-NPC1–expressing cells (Supplementary Figure 2). We also confirmed that these NPC1s were similarly localized at endosomal vesicles (data not shown).
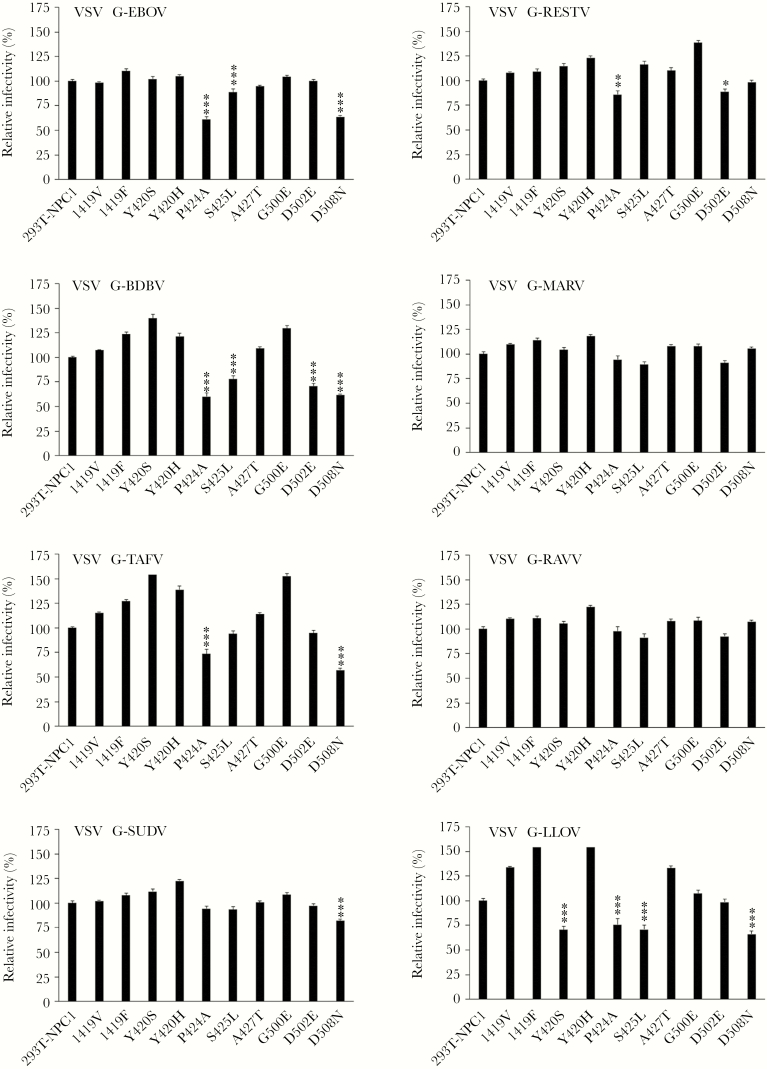
To evaluate whether these SNP substitutions affected the efficiency of viral entry, each cell line was infected with replication-incompetent VSV pseudotyped with filovirus GPs, and relative IUs were compared among the cell lines (Figure 2). We found that P424A, S425L, D502E, and D508N substitutions in NPC1 reduced the entry of VSV pseudotyped with GPs from multiple filovirus species. P424A and D508N substitutions significantly affected the entry of VSV∆G-EBOV, -BDBV, -TAFV, -SUDV, -RESTV, and -LLOV but not -MARV and/or -RAVV. On the other hand, S425L and D502E substitutions reduced the entry of VSV∆G-MARV, and some of the pseudotyped VSV with ebolavirus GPs. Y420S substitution only reduced the entry of VSV∆G-LLOV. It was noted that these substitutions resulted in different patterns of reduction corresponding to the filovirus genera (ie, Ebolavirus, Marburgvirus, and Cuevavirus). In particular, P424A/D508N and S425L/D502E substitutions seemed to be important for the reduced entry of VSVs pseudotyped with ebolavirus and marburgvirus GPs, respectively. In some cell lines, infectivity of the viruses was enhanced and it was correlated with relatively high expression levels of NPC1 (Supplementary Figure 2).
Figure 2.
Infectivity of vesicular stomatitis viruses (VSVs) pseudotyped with filovirus glycoproteins (GPs) in Vero E6 cell lines. Confluent monolayers of each cell line grown in 96-well plates were infected with VSVs containing the green fluorescent protein (GFP) gene instead of the receptor-binding VSV G protein gene (VSV∆G) and pseudotyped viruses with GPs of Ebola virus (EBOV; Mayinga), Bundibugyo virus (BDBV; Butalya), Taï Forest virus (TAFV; Pauléoula), Sudan virus (SUDV; Boniface), Reston virus (RESTV; Pennsylvania), Marburg virus (MARV; Angola), Ravn virus (RAVV; Kitum Cave), and Lloviu virus (LLOV; Asturias), designated by VSV∆G-EBOV, -BDBV, -TAFV, -SUDV, -RESTV, -MARV, -RAVV, and -LLOV, respectively. Twenty hours later, the virus infectious units (IUs) in each cell line were determined by counting the number of GFP-expressing cells with an IN Cell Analyzer 2000 (GE Healthcare). The relative infectivity in each cell line was calculated by setting the IUs given by Vero E6 cells expressing 293T-NPC1 (approximately 1000–3000 IUs/well for each assay) to 100%. Means and standard errors of 30 replicates are shown. *P < .05, **P < .01, and ***P < .001 for values significantly lower than that for 293T-NPC1.
Reduced Plaque-Forming Ability of rVSV-EBOV in Vero E6 Cells Expressing NPC1 With P424A or D508N Substitution
We then compared the plaque-forming abilities of rVSV-EBOV and rVSV-MARV using the same cell lines (Figure 3). Although statistically significant difference was not observed, the P424A and S425L substitutions moderately reduced the plaque number of rVSV-EBOV and rVSV-MARV, respectively (Figure 3A). As expected, the average plaque sizes of rVSV-EBOV in cells expressing NPC1 with the D508N substitution were significantly smaller than in 293T-NPC1–expressing cells, and the P424A substitution also slightly reduced the plaque size (Figure 3B). Consistent with the data shown in Figure 2, rVSV-MARV formed slightly but not significantly smaller plaques in the cell line expressing S425L NPC1 (Figure 3B).
Figure 3.
Plaque/focus formation of replication-competent recombinant vesicular stomatitis virus (rVSV) containing the Ebola virus (EBOV) glycoprotein (GP)–encoding gene (rVSV-EBOV), rVSV containing the Marburg virus (MARV) GP–encoding gene (rVSV-MARV), and recombinant EBOV expressing green fluorescent protein (EBOV-GFP) in Vero E6 cell lines. A, rVSV-EBOV and rVSV-MARV (multiplicity of infection = 0.0005 in Vero E6 cells) were inoculated into Vero E6 cells grown in 6-well tissue culture plates. After adsorption for 1 hour, the inoculum was removed, and the cells were overlaid with Eagle’s minimal essential medium containing 1.0% Bacto Agar (BD) and then incubated for 3 days at 37°C. Cells were stained with 0.5% crystal violet in 10% formalin, and the plaque-forming units in each cell line were determined by counting the number of all visible plaques per well (ie, 50–100 plaques for each assay). Data represent means and standard errors of at least 3 independent experiments. B, Plaque sizes were measured with ImageJ software. Means and standard errors of 50–100 plaques/well are shown. C, EBOV-GFP (multiplicity of infection = 0.002 in Vero E6 cells) were inoculated into confluent monolayers of Vero E6 cells grown in 96-well tissue culture plates. After adsorption for 1 hour, the inoculum was replaced with Eagle’s minimal essential medium containing 1.2% carboxymethyl cellulose. After incubation for 3 days at 37°C, the cells were fixed, and GFP foci in each cell line were counted under a fluorescence microscope. Data represent means and standard errors of triplicate assays. D, Focus sizes were measured with ImageJ software. Means and standard errors of 60–150 foci/well are shown. *P < .05, **P < .01, and ***P < .001 for values significantly lower than for 293T-NPC1.
Reduced Focus-Forming Ability of EBOV in Vero E6 Cells With the P424A Substitution
To examine the effects of substitutions associated with NPC1 SNPs on actual filovirus infection, we used an infectious EBOV expressing GFP and determined the viral focus numbers and average focus size in each cell line. Consistent with our pseudotyped VSV data, the P424A substitution resulted in reduced focus numbers of EBOV-GFP (Figure 3C). The average size of foci in this cell line was also smaller than in cells expressing 293T-NPC1 (Figure 3D). Although these differences were not significant in a multiple comparison analysis, the Welch t test gave significant differences as compared to 293T-NPC1–expressing cells. The D508N substitution slightly reduced the focus size of EBOV-GFP, but there was no statistically significant difference as compared to 293T-NPC1–expressing cells.
DISCUSSION
With human immunodeficiency virus type HIV-1 infection, there is a subset of people who are inherently resistant to the virus [28–31]. In particular, genetic variation in the host viral receptors has been shown to reduce the susceptibility to HIV infection in humans [28, 29]. Asymptomatic filovirus infection is less studied, but Baron et al [32] reported potential asymptomatic cases during the outbreak in Sudan in 1979, and Dean et al [33] estimated the proportion of asymptomatic transmissions during the recent epidemic in West Africa. Although host genetics and EBOV disease progression and resistance have been studied in mice [34, 35], the details of genetic polymorphisms that may affect susceptibility of humans to filoviruses have not been elucidated yet.
In the present study, we focused on 10 reported NPC1 SNP substitutions that interface with GP. Although none of the SNPs tested here completely ablated viral entry or infectivity, some SNPs were nevertheless found to be important for filovirus infection. In our experiments, P424A substitution reduced entry of VSV pseudotyped with ebolavirus but not marburgvirus GPs. Moreover, focus sizes of EBOV-GFP were also reduced in this cell line. Interestingly, Wang et al [15] demonstrated that the P424A NPC1 mutant retained binding capacity to dGP but with reduced affinity as compared to wild-type NPC1. Taken together, these findings suggest that the P424A substitution in NPC1 lowers its binding capacity to dGP, resulting in reduced viral entry and infection.
S425L substitution also reduced the infection with some pseudotyped VSVs, including VSV∆G-MARV and -RAVV. The serine residue at position 425 in NPC1 was shown to be involved in the interaction with the amino acid residue at position 142 of the EBOV GP molecule [15]. However, since amino acid residues at this position are different in EBOV and MARV GPs (serine at 142 of EBOV GP and glutamine at 126 of MARV GP, respectively), the effects of the S425L substitution might be different between EBOV and MARV. It has also been demonstrated that single amino acid mutations at positions 502 or 503 in NPC1 can reduce the efficiency of viral infection [13, 14]. Our experiments confirmed this finding, as D502E substitution reduced the entry of some of the pseudotyped viruses we tested and also reduced the efficiency of infection with EBOV-GFP (although not significantly). Notably, while the previous study introduced a significant loss of charge at residue 502 by mutating the aspartic acid to phenylalanine [13], our study shows that even minimal variation at this residue (ie, the change from D to E) can have an effect on viral entry.
Some other amino acids that are also important for binding to dGP have not been reported as SNP sites in the NPC1 loops [15]. The rapidly increasing sequence data in public databases may hereafter provide additional information on NPC1 SNP substitutions not evaluated in this study. It is also of interest to investigate multiple SNP substitutions in the loops. Although more-sensitive studies are needed to further assess the capacity for NPC1 variation to influence filovirus infection, identifying genetic variations that affect the susceptibility of hosts to filoviruses will be crucial in understanding filovirus disease progression and host cell restriction.
Supplementary Data
Supplementary materials are available at The Journal of Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Notes
Acknowledgments. We thank GE Healthcare Japan and Koshin Kagaku, for their assistance in the establishment of the IN Cell Analyzer 2000 protocol; Life Technologies Japan and Frontier Science, for their assistance in gene editing; Kim Barrymore, for editing the manuscript; and Michihito Sasaki (Division of Molecular Pathobiology, Research Center for Zoonosis Control, Hokkaido University) for anti-LAMP1 antibody.
Financial support. This work was supported by the Japan Society for the Promotion of Science, Ministry of Education, Culture, Sports, Science and Technology (Research Fellowship for Young Scientists 16J04404 and Grants-in-Aid for Scientific Research, KAKENHI, 16H02627 and 15H01249); the Intramural Research Program, National Institute of Allergy and Infectious Diseases, National Institutes of Health; and the Japanese Initiative for Progress of Research on Infectious Disease for Global Epidemics Japan Agency for Medical Research and Development (award JP17fm0208101).
Potential conflicts of interest. All authors: No reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Kuhn JH. Guide to the correct use of filoviral nomenclature. Curr Top Microbiol Immunol 2017; 411:447–60. [DOI] [PubMed] [Google Scholar]
- 2. Takada A, Robison C, Goto H, et al. A system for functional analysis of Ebola virus glycoprotein. Proc Natl Acad Sci U S A 1997; 94:14764–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hofmann-Winkler H, Kaup F, Pöhlmann S. Host cell factors in filovirus entry: novel players, new insights. Viruses 2012; 4:3336–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Takada A. Filovirus tropism: cellular molecules for viral entry. Front Microbiol 2012; 3:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Nanbo A, Imai M, Watanabe S, et al. Ebolavirus is internalized into host cells via macropinocytosis in a viral glycoprotein-dependent manner. PLoS Pathog 2010; 6:e1001121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Saeed MF, Kolokoltsov AA, Albrecht T, Davey RA. Cellular entry of ebola virus involves uptake by a macropinocytosis-like mechanism and subsequent trafficking through early and late endosomes. PLoS Pathog 2010; 6:e1001110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Aleksandrowicz P, Marzi A, Biedenkopf N, et al. Ebola virus enters host cells by macropinocytosis and clathrin-mediated endocytosis. J Infect Dis 2011; 204(Suppl 3):S957–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Chandran K, Sullivan NJ, Felbor U, Whelan SP, Cunningham JM. Endosomal proteolysis of the Ebola virus glycoprotein is necessary for infection. Science 2005; 308:1643–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Misasi J, Chandran K, Yang JY, et al. Filoviruses require endosomal cysteine proteases for entry but exhibit distinct protease preferences. J Virol 2012; 86:3284–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Carette JE, Raaben M, Wong AC, et al. Ebola virus entry requires the cholesterol transporter Niemann-Pick C1. Nature 2011; 477:340–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Côté M, Misasi J, Ren T, et al. Small molecule inhibitors reveal Niemann-Pick C1 is essential for Ebola virus infection. Nature 2011; 477:344–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Miller EH, Obernosterer G, Raaben M, et al. Ebola virus entry requires the host-programmed recognition of an intracellular receptor. EMBO J 2012; 31:1947–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ng M, Ndungo E, Kaczmarek ME, et al. Filovirus receptor NPC1 contributes to species-specific patterns of ebolavirus susceptibility in bats. eLife 2015; 4:e11785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ndungo E, Herbert AS, Raaben M, et al. A single residue in Ebola virus receptor NPC1 influences cellular host range in reptiles. mSphere 2016; 1:e00007–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wang H, Shi Y, Song J, et al. Ebola viral glycoprotein bound to its endosomal receptor Niemann-Pick C1. Cell 2016; 164:258–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gong X, Qian H, Zhou X, et al. Structural insights into the Niemann-Pick C1 (NPC1)-mediated cholesterol transfer and Ebola infection. Cell 2016; 165:1467–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Takada A, Feldmann H, Stroeher U, et al. Identification of protective epitopes on ebola virus glycoprotein at the single amino acid level by using recombinant vesicular stomatitis viruses. J Virol 2003; 77:1069–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ebihara H, Theriault S, Neumann G, et al. In vitro and in vivo characterization of recombinant Ebola viruses expressing enhanced green fluorescent protein. J Infect Dis 2007; 196(Suppl 2):S313–22. [DOI] [PubMed] [Google Scholar]
- 19. Furuyama W, Miyamoto H, Yoshida R, Takada A. Quantification of Filovirus glycoprotein-specific antibodies. Methods Mol Biol 2017; 1628:309–20. [DOI] [PubMed] [Google Scholar]
- 20. Maruyama J, Miyamoto H, Kajihara M, et al. Characterization of the envelope glycoprotein of a novel filovirus, lloviu virus. J Virol 2014; 88:99–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kajihara M, Nakayama E, Marzi A, Igarashi M, Feldmann H, Takada A. Novel mutations in Marburg virus glycoprotein associated with viral evasion from antibody mediated immune pressure. J Gen Virol 2013; 94:876–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ebihara H, Yoshimatsu K, Ogino M, et al. Pathogenicity of Hantaan virus in newborn mice: genetic reassortant study demonstrating that a single amino acid change in glycoprotein G1 is related to virulence. J Virol 2000; 74:9245–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kitamura T, Koshino Y, Shibata F, et al. Retrovirus-mediated gene transfer and expression cloning: powerful tools in functional genomics. Exp Hematol 2003; 31:1007–14. [PubMed] [Google Scholar]
- 24. Liang X, Potter J, Kumar S, et al. Rapid and highly efficient mammalian cell engineering via Cas9 protein transfection. J Biotechnol 2015; 208:44–53. [DOI] [PubMed] [Google Scholar]
- 25. Yu X, Liang X, Xie H, et al. Improved delivery of Cas9 protein/gRNA complexes using lipofectamine CRISPRMAX. Biotechnol Lett 2016; 38:919–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kuroda M, Fujikura D, Nanbo A, et al. Interaction between TIM-1 and NPC1 is important for cellular entry of Ebola virus. J Virol 2015; 89:6481–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Team RC. R: a language and environment for statistical computing Vienna, Austria:R Foundation for Statistical Computing, 2015. https://www.R-project.org/. Accessed 16 May 2017. [Google Scholar]
- 28. Liu R, Paxton WA, Choe S, et al. Homozygous defect in HIV-1 coreceptor accounts for resistance of some multiply-exposed individuals to HIV-1 infection. Cell 1996; 86:367–77. [DOI] [PubMed] [Google Scholar]
- 29. Samson M, Libert F, Doranz BJ, et al. Resistance to HIV-1 infection in caucasian individuals bearing mutant alleles of the CCR-5 chemokine receptor gene. Nature 1996; 382:722–5. [DOI] [PubMed] [Google Scholar]
- 30. O’Brien SJ, Moore JP. The effect of genetic variation in chemokines and their receptors on HIV transmission and progression to AIDS. Immunol Rev 2000; 177:99–111. [DOI] [PubMed] [Google Scholar]
- 31. Pereyra F, Addo MM, Kaufmann DE, et al. Genetic and immunologic heterogeneity among persons who control HIV infection in the absence of therapy. J Infect Dis 2008; 197:563–71. [DOI] [PubMed] [Google Scholar]
- 32. Baron RC, McCormick JB, Zubeir OA. Ebola virus disease in southern Sudan: hospital dissemination and intrafamilial spread. Bull World Health Organ 1983; 61:997–1003. [PMC free article] [PubMed] [Google Scholar]
- 33. Dean NE, Halloran ME, Yang Y, Longini IM. Transmissibility and pathogenicity of Ebola virus: a systematic review and meta-analysis of household secondary attack rate and asymptomatic infection. Clin Infect Dis 2016; 62:1277–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Rasmussen AL, Okumura A, Ferris MT, et al. Host genetic diversity enables Ebola hemorrhagic fever pathogenesis and resistance. Science 2014; 346:987–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Hill-Batorski L, Halfmann P, Marzi A, et al. Loss of interleukin 1 receptor antagonist enhances susceptibility to Ebola virus infection. J Infect Dis 2015; 212(Suppl 2):S329–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.