Abstract
Objective
To conduct a systematic review of pain anxiety, pain catastrophizing, and fear of pain measures psychometrically established in youth with chronic pain. The review addresses three specific aims: (1) to identify measures used in youth with chronic pain, summarizing their content, psychometric properties, and use; (2) to use evidence-based assessment criteria to rate each measure according to the Society of Pediatric Psychology (SPP) guidelines; (3) to pool data across studies for meta-analysis of shared variance in psychometric performance in relation to the primary outcomes of pain intensity, disability, generalized anxiety, and depression.
Methods
We searched Medline, Embase, PsycINFO, and relevant literature for possible studies to include. We identified measures studied in youth with chronic pain that assessed pain anxiety, pain catastrophizing, or fear of pain and extracted the item-level content. Study and participant characteristics, and correlation data were extracted for summary and meta-analysis, and measures were rated using the SPP evidence-based assessment criteria.
Results
Fifty-four studies (84 papers) met the inclusion criteria, including seven relevant measures: one assessed pain anxiety, three pain catastrophizing, and three fear of pain. Overall, five measures were rated as “well established.” We conducted meta-analyses on four measures with available data. We found significant positive correlations with the variables pain intensity, disability, generalized anxiety, and depression.
Conclusion
Seven measures are available to assess pain anxiety, pain catastrophizing, and fear of pain in young people with chronic pain, and most are well established. We present implications for practice and directions for future research.
Keywords: adolescents, anxiety, children, pain, meta-analysis
Introduction
Children and adolescents frequently experience and report pain (Perquin et al., 2000). Around 25% of young people experience pain that persists for >3 months (King et al., 2011), and 8% of young people report their pain to be severe and disabling (Huguet & Miró, 2008). Chronic pain in youth can significantly disrupt emotional and social functioning, and is often accompanied by generalized anxiety and depression (Forgeron, Evans, McGrath, Stevens, & Finley, 2013; Gauntlett-Gilbert & Eccleston, 2007; Kashikar-Zuck, Goldschneider, Powers, Vaught, & Hershey, 2001; Kashikar-Zuck et al., 2008). Children and adolescents with chronic pain also report significant disability, including loss of engagement with age-appropriate physical activities and impairment in everyday activities such as walking and playing sports (Palermo, Lewandowski, Long, & Burant, 2008). Pediatric fear-avoidance models (Asmundson, Noel, Petter, & Parkerson, 2012; Simons & Kaczynski, 2012) propose that pain, depression, and pain-related disability are driven and maintained by interrelated key psychological factors including pain anxiety, pain catastrophizing, and fear of pain. These constructs may be critical targets for psychological intervention, given research findings showing associations between anxiety and functioning (Fisher et al., 2014; Tran et al., 2015), and so their accurate and reliable measurement is an important objective.
Fear-avoidance models of pain behavior have been developed in both adult and adolescent chronic pain (Asmundson et al., 2012; Simons & Kaczynski, 2012; Vlaeyen, Crombez, & Linton, 2016). At their core is a group of overlapping fear-related constructs composed of fear of pain, worry, rumination, pain-related anxiety, anxiety sensitivity, and the concept of catastrophic thinking about pain and its possible consequences. Dominant are the general constructs of “pain anxiety” and “pain related fear,” and the specific idea of “pain catastrophizing.” These constructs share overlapping, as well as distinct conceptualizations. Pain anxiety refers to future-oriented apprehensions and worries about pain (Huguet, McGrath, & Pardos, 2011). Pain catastrophizing refers to exaggerated thoughts about pain and includes rumination, magnification, and helplessness (Crombez et al., 2003; Sullivan, Bishop, & Pivik, 1995). Fear is a distressing emotional reaction in response to an immediate threat (Rachman, 2013). Fear of pain often relates to beliefs that people hold regarding how detrimental pain will be (Turk & Wilson, 2010), and scales measuring this construct ask participants to respond to items that describe past, present, or future threats that are likely to increase pain (Simons, Sieberg, Carpino, Logan, & Berde, 2011). While these constructs are separated in the pediatric fear-avoidance models (Asmundson et al., 2012; Simons & Kaczynski, 2012), there are clear overlaps in their historical and current conceptualization. For example, while most agree that catastrophizing is cognitive in nature and fear is affective in nature, some consider catastrophizing as a cognitive component of the more general fear response (Huguet et al., 2011). Moreover, some conceptualizations consider fear and catastrophizing as distinct components of the broader pain anxiety response of negative anticipation of experiencing future pain (Huguet et al., 2011).
Increased attention toward these constructs has been accompanied by the development of new pediatric measures and adaptation of adult measures for use in children and adolescents. Given the expansion of this research area, it is timely to provide scientists and clinicians with a comprehensive summary of available measures to guide their research and practice. We present here a systematic review of pain anxiety, pain catastrophizing, and fear of pain measures that have been psychometrically assessed in pediatric chronic pain samples. The review focuses on three aims: (1) to describe measures of pain anxiety, pain catastrophizing, and fear of pain used in samples of youth with chronic pain, including how they were developed, the populations they are used in, and the frequency of use; (2) to assess the measures’ psychometric properties and conduct a rating of the level of evidence-based assessment according to the Society of Pediatric Psychology (SPP) guidelines (Cohen et al., 2008); (3) to meta-analyze reported correlations of pain anxiety, pain catastrophizing, and fear of pain with the primary outcome variables specified in the pediatric fear-avoidance model of pain (i.e., pain intensity, disability, general anxiety, and depression) to examine construct validity. We hypothesize that higher pain anxiety, pain catastrophizing, and fear of pain will be associated with higher pain intensity, disability, general anxiety, and depression. For simplicity, from now on, we refer to pain anxiety, pain catastrophizing, and fear of pain measures collectively as “cognitive-affective measures.”
Methods
Inclusion Criteria
We included studies of young people (<18 years of age) with chronic pain (≥3-month duration) (Merskey and Bogduk 1994) in which self-report measures of pain anxiety, pain catastrophizing, and fear of pain were reported. All pain conditions were included with the exception of pain associated with life-limiting conditions (e.g., cancer; cystic fibrosis), acute pain, and perioperative pain. These pain types/conditions were excluded from this review because they often use separate measures to assess cognitive affective or pain constructs. Studies could recruit from a variety of settings including clinical or community settings, but must meet criteria of reporting pain for ≥3 months.
We included studies using measures that have been psychometrically tested in young people with chronic pain. Studies using measures validated in adult populations only were excluded from this systematic review. We only included studies published in English because of limited resources translating abstracts in foreign languages. Measures that contained subscales of pain anxiety, pain catastrophizing, and fear of pain were included; however, studies had to explicitly state that the relevant subscale was assessed in a chronic pain (rather than a community) sample. Further, subscales that include a composite subscale (e.g., emotion-focused coping) derived from other subscales (e.g., catastrophizing, distraction) were excluded for the purposes of this review. For transparency, and in particular to avoid selective reporting bias, a protocol for this study was published online and is available at http://bit.ly/2jn1tmF.
Search Methods
To identify potential studies for inclusion, we conducted three searches of relevant databases and reviews.
First, we conducted searches of Medline, PsycINFO, and Embase for studies that assess pain anxiety, pain catastrophizing, and fear of pain in children with chronic pain. The search was conducted from inception to June 2016. For our search criteria, please see Supplementary Material S1. Two authors (EF; LC) screened abstracts, discussed papers for inclusion, and read full texts. Disagreements were discussed and a third author (TP) arbitrated.
Second, we assessed the measures used in all studies included in previously published systematic reviews of the efficacy of psychological interventions for pediatric chronic pain for inclusion of cognitive-affective measures (Eccleston et al., 2014; Fisher et al., 2014; Fisher, Law, Palermo, & Eccleston, 2015).
Third, we ran a citation search for measures identified in Steps 1 and 2 that were delivered to children with chronic pain to identify any further papers for inclusion.
Data Extraction
1. Study and measure characteristics: We extracted study characteristics including chronic pain condition, sample size, sex, author group, country of study origin, recruitment and procedures, and the cognitive-affective measure used. For each measure, we extracted the age range of the sample that the measure was tested with, noted the number of items in each measure, and identified the subscales. We did not extract demographics from community/healthy samples (youth with no pain or pain <3 months), as this was not the aim of this review. Measures were categorized as “pain anxiety,” “fear of pain,” or “pain catastrophizing” based on the label that was given to the measure/subscale in the original measure development paper.
2. Psychometrics of measures: The predominant psychometric data reported in included studies were reliability data; we were able to extract indices of internal consistencies for all of the cognitive-affective measures. We noted whether studies had reported internal consistencies from the study sample or from the original measure development paper(s) of each measure, and extracted data from only the former. For those studies that also recruited youth from community settings, we only extracted internal consistency and psychometrics for participants with chronic pain (rather than the healthy sample). We also extracted additional psychometric data on reliability or validity of each measure, including exploratory and confirmatory factor analyses. Owing to the large number of included studies, authors were not contacted for additional psychometric data.
3. Outcomes: We conducted meta-analyses of correlations between the cognitive-affective measures and pain intensity, disability, generalized anxiety, and depression. Any measures that assessed these outcome domains were eligible for inclusion in the meta-analysis, if correlations were presented in published manuscripts. If more than one measure was available for each domain, we extracted data for the most commonly used measure across included studies. For studies that recruited youth from community and chronic pain samples, we only extracted correlations for the chronic pain samples. Correlations for healthy children and adolescents, or correlations that combined healthy and chronic pain groups, were excluded from the meta-analysis. As stated, we did not contact authors for additional data for the meta-analyses.
Overlapping samples: We classified overlapping samples (i.e., including the same participants across multiple publications) in two ways: (1) identifying multiple papers from the same lab groups/author teams; (2) noting where the recruitment dates were similar or if the number of participants and means for age were matching. We clarified overlapping samples with study authors where possible. When overlapping samples were identified, we next selected the paper with the largest participant sample to include as the primary study. Data were extracted from secondary studies only where data (e.g., correlations with additional outcomes) were missing from the primary paper. On occasions when there were multiple secondary papers, we extracted data from the next largest sample.
Data Analysis
First, we summarize the pain anxiety, pain catastrophizing, and fear of pain measures used in children and adolescents with chronic pain and their relevant psychometrics (as a range of scores). We combined data from measures that have been translated to other languages, but included the same items. Second, we assess whether measures are “well-established,” “approaching well-established,” or “promising” in accordance with the Society for Pediatric Psychology (SPP) criteria on evidence-based assessment (Cohen et al., 2008). Third, we combine data and present pooled correlations for each cognitive-affective measure and the outcomes of pain, disability, general anxiety, and depression. We only performed meta-analyses if three or more individual studies reported data for each outcome. For each of the measures, we used total scores if the entire measure assessed pain anxiety, pain catastrophizing, and fear of pain. For measures that included additional but unrelated subscales, we only extracted correlations related to cognitive-affective concepts. Meta-analyses were performed with STATA using the DerSimonian–Laird random effects method, which assumes heterogeneity between studies. Heterogeneity (I2) was interpreted using the Cochrane criteria (0–40% might not be important; 30–60% moderate heterogeneity; 50–90% substantial heterogeneity; and 75–100% considerable heterogeneity) (Higgins & Green, 2011). Trim and fill analyses using Duval and Tweedie (2000) method and Rosenthal’s failsafe N (Rosenthal, 1979) were conducted to detect publication bias. As recommended, we only conducted these analyses where there were more than eight studies in a meta-analysis (Jennions & Moller, 2002).
Results
Search Results
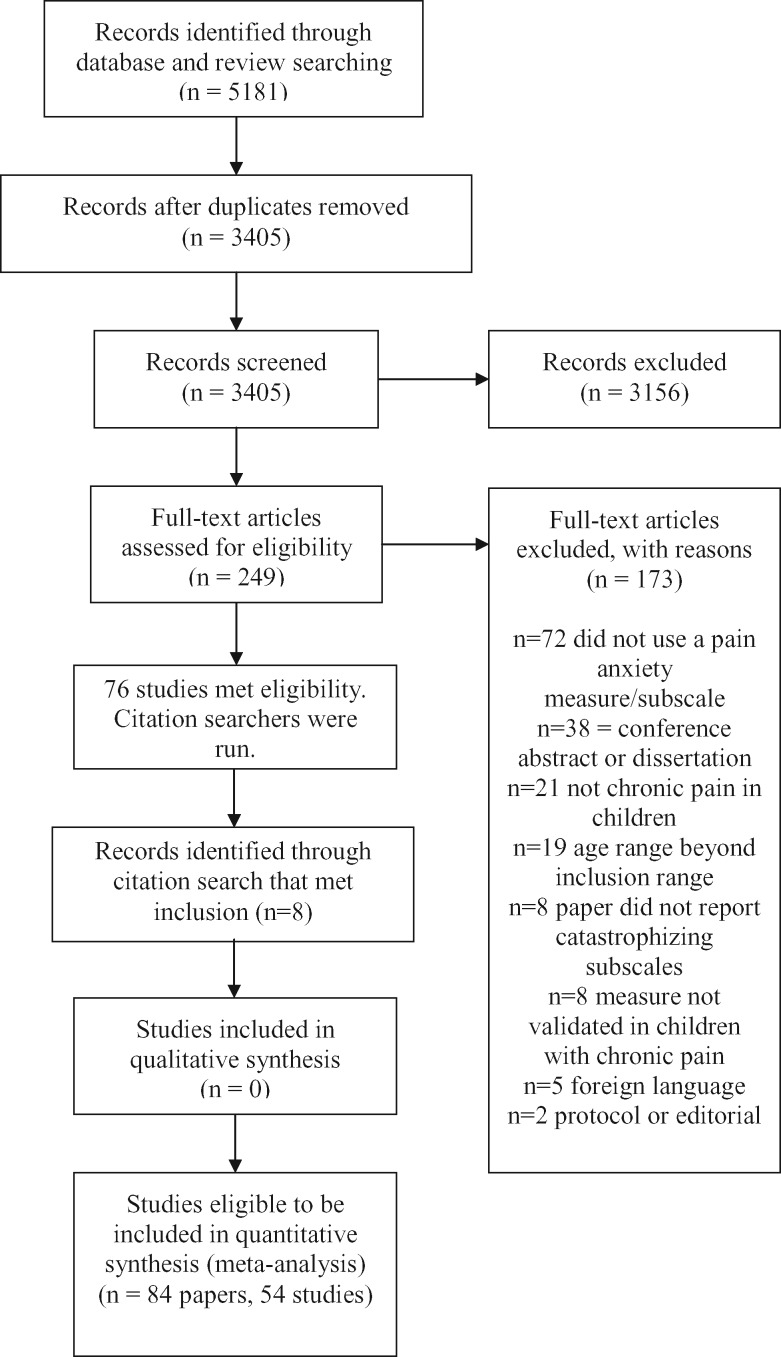
We conducted a three-stage search method. First, we searched Medline, Embase, and PsycINFO and identified 3,405 papers after duplicates were removed. The titles and abstracts were screened, 249 full papers were read, and 76 papers met the inclusion criteria. Second, we screened the studies included in three previously published systematic reviews on psychological therapies for pediatric pain, identifying any additional papers using cognitive-affective measures. No further studies were identified through this method. In total, we identified seven measures of pain anxiety, pain catastrophizing, and fear of pain in 76 papers that met inclusion. Third, a citation search of these measures was conducted and eight further papers were identified, resulting in 84 papers (for a list of included papers and references, see Supplementary Material S2). We then assessed overlapping samples within the 84 papers identified and identified 41 papers that had overlapping samples. We chose the primary papers from this group, which resulted in 11 studies. The remaining 43 papers reported individual studies. Combined, 54 studies were eligible to be included in the meta-analyses. For the remainder of the review, we will only discuss the studies included, rather than the number of papers identified. See Figure 1 for flow diagram.
Figure 1.
Flow of studies.
Included Studies
The 54 studies included 10,036 youth with chronic pain (6,008 girls; 2,639 boys; sex reported in 49 studies). The mean age of youth was 13.74 (SD = 2.12; age reported in 51 studies). The majority of studies (n = 34) recruited youth with a range of chronic pain conditions including headache, recurrent abdominal pain, musculoskeletal pain, and neuropathic pain. Eight studies included youth with only recurrent abdominal pain, seven included youth with musculoskeletal pain (e.g., juvenile idiopathic arthritis; fibromyalgia), two included youth with headache, two neuropathic pain, and one inflammatory bowel disease. Characteristics of included studies can be found in Supplementary Material S3.
Aim 1: Measures Used to Assess Pain Anxiety, Pain Catastrophizing, and Fear of Pain
Across the 54 studies, we identified seven measures that assessed cognitive-affective processes. Of these seven, one measure assessed pain anxiety, three assessed pain catastrophizing, and three assessed fear of pain. Table I describes the characteristics and development of measures, and Table II summarizes their use.
Table I.
Summary of Cognitive-Affective Measures Validated in Children and Adolescents With Chronic Pain
| Measure | Cognitive-affective domain | Number of items | Subscales | Independent expert panel | Child/adolescent input | Direct adaptation or informed by multiple measures? |
|---|---|---|---|---|---|---|
| BAPQa | Pain anxiety | 6 | Pain-specific anxiety | Y | Y (item generation; CP only) | Multiple child measures |
| FOPQ-C | Fear of pain | 24 | Fear of pain (n = 13), avoidance of activities (n = 11) | Y | Y (item generation; CP only) | Multiple adult measures |
| PCS-C | Catastrophizing | 13 | Rumination (n = 4), helplessness (n = 6), magnification (n = 3) | N | N | Direct adaptation from adult measure |
| PCQa | Catastrophizing | 5 | Internalizing/catastrophizing subscale | N | N | Multiple adult and child measures |
| PRIa | Catastrophizing | 5 | Catastrophizing subscale | N | Y (item generation; CP only) | Multiple child and adult measures |
| PPFQ | Fear of pain | 22 | Fearful thoughts scale (n = 11), fearful physical feelings and behaviors (n = 11) | Y | Y (item generation, pilot questionnaire responses; CP and healthy children) | Multiple measures (unknown whether child or adult) |
| PHODA-Youth | Fear of pain | 51 | Activities of daily life (n = 13), intensive physical activities (n = 27), social activities (n = 11) | Y | Y (item generation; CP and healthy children) | Direct adaptation from adult measure |
Other subscales not related to cognitive-affective constructs of interest in this article are available but not listed here. Yes (Y); No (N);.
Note. Bath Adolescent Pain Questionnaire = BAPQ; Children with chronic pain = CP; Fear of Pain Questionnaire for Children = FOPQ-C; Pain Catastrophizing Scale for Children = PCS-C; Pain Coping Questionnaire = PCQ; Pain Response Inventory = PRI; Pediatric Pain Fear Questionnaire = PPFQ; Photograph Series of Daily Activities = PHODA-Youth.
Table II.
Summary of Psychometric Evaluation for Cognitive-Affective Measures Validated in Youth With Chronic Pain
| Measure | Number of author groups | Age (years) | Available psychometrics |
Rating | |
|---|---|---|---|---|---|
| Reliability | Validity | ||||
| BAPQ pain-specific scale | 6 studies; 3 author groups | 11–18 | Internal consistency = 0.83 (pain management sample); 0.88 (rheumatology samples) Test–retest reliability (17 days) = 0.77 | Convergent validity | Well established |
| FOPQ-C | 5 studies; 2 author groups | 8–17 | Internal consistency = 0.92 Test–retest reliability (4 weeks) = 0.65–0.74 | Construct validity | Well established |
| Criterion-related validity | |||||
| Exploratory factor analysis | |||||
| PCS-C | 30 studies; 23 author groups | 8–16 | Internal consistency = 0.90 Test–retest reliability (5 months) = 0.71 | Construct validity | Well established |
| Exploratory factor analysis Confirmatory factor analysis | |||||
| PCQ-IC | 18 studies; 10 author groups | 8–18 | Internal consistency = 0.70 | Construct validity | Well established |
| Exploratory factor analysis Confirmatory factor analysis | |||||
| PRI—catastrophizing subscale | 7 studies; 3 author groups | 5–18 | Internal consistency = 0.84 | Construct validity | Well established |
| Confirmatory factor analysis | |||||
| PPFQ | 1 study; 1 author group | 12–21 | Internal consistency = 0.83–0.89 | Construct validity | Promising assessment (only used in one peer-reviewed article) |
| PHODA-Youth | 1 study; 1 author group | 13–21 | Internal consistency = 0.98 Test–retest reliability (4 weeks) = 0.94 | Construct validity | Well establisheda |
| Exploratory factor analysis | |||||
Since the search date of this review, one further author team (Simons et al., 2017) published on the PHODA-Youth in young people with chronic pain, meaning this measure is now well established.
Note. Bath Adolescent Pain Questionnaire = BAPQ; Fear of Pain Questionnaire for Children = FOPQ-C; Pain Catastrophizing Scale for Children = PCS-C; Pain Coping Questionnaire internalizing/catastrophizing = PCQ-IC; Pain Response Inventory = PRI; Pediatric Pain Fear Questionnaire = PPFQ; Photograph Series of Daily Activities = PHODA-Youth.
Pain anxiety: The Bath Adolescent Pain Questionnaire (BAPQ) pain-specific anxiety subscale (Eccleston et al., 2005) was the only measure of pain anxiety that we identified from our search that had been psychometrically established in youth with chronic pain. Of the 54 studies included in our systematic review, six used the BAPQ pain-specific anxiety subscale. Of these six studies, three different author groups have used the measure. The studies were primarily based in the UK (n = 4) where the original questionnaire was developed and reported. The measure has also been used in research studies in Canada and the United States. Two studies reported internal consistencies for their own sample (α = 0.83–0.87). The internal consistency for the original measure, also noted in other papers, was 0.83–0.88 in pain management and rheumatology samples, respectively. This measure is part of a multidimensional assessment of pain, covering other domains such as social and physical functioning, depression, generalized anxiety, family functioning, and social development. The items in the BAPQ pain-specific anxiety subscale mostly pertain to cognitions (I worry about my pain problem), but there is also an item regarding behavior (I avoid activities that cause pain).
Pain catastrophizing: The Pain Catastrophizing Scale for Children (PCS-C) (Crombez et al., 2003) was the most frequently used measure (in 30 studies). These studies were conducted in the United States and Canada, as well as six countries across Europe. Twenty-three separate author groups have used this measure in their studies investigating pediatric chronic pain. Eight studies reported the internal consistencies, which ranged from 0.88 to 0.95 (the measure development paper = 0.90). The first psychometric test of the PCS-C was conducted in Dutch, but has since been psychometrically tested in other languages including English, German, and Spanish. The PCS-C was the only full measure to assess pain catastrophizing in youth, combining subscales of rumination (When I have pain, I can’t keep it out of my mind), magnification (When I have pain I’m afraid that the pain will get worse), and helplessness (When I have pain I feel I can’t go on).
Two further measures of catastrophizing were subscales of coping measures, including the Pain Response Inventory (PRI) (Walker, Smith, Garber, & Van Slyke, 1997) and Pain Coping Questionnaire (PCQ) (Thastum, Zachariae, Scholer, & Herlin, 1999). Here, we only discuss the catastrophizing subscales rather than the full measures. These measures describe pain-related cognitions and do not consider pain-related behavior or physiological reactions to pain.
Reid, Gilbert, and McGrath (1998) developed and psychometrically tested the Pain Coping Questionnaire internalizing/catastrophizing scale (PCQ-IC) in healthy children and adolescents, which included items such as I worry that I will always be in pain. It was first psychometrically tested in children with chronic pain in Danish (Thastum et al., 1999), and later translated to German and tested in children with chronic pain (Hermann, Hohmeister, Zohsel, Tuttas, & Flor, 2008). Across the 16 studies, seven reported internal consistencies for this measure in chronic pain populations, which ranged from 0.73 to 0.89.
The PRI-catastrophizing scale (Walker et al., 1997) has been used in seven studies, exclusively with populations from the United States. Items such as Feel like you can’t stand it anymore are included in the subscale. The measure has been used by three different author groups (inclusive of the measure development), although the scale developer features as an author on all studies. The measure has been used most often in children with recurrent abdominal pain. Two studies reported internal consistencies for the catastrophizing subscale separately, which ranged from 0.82 to 0.83. The internal consistency of the subscale in children with chronic pain in the first psychometric study was 0.84 (Walker et al., 1997).
Fear of Pain: Three fear of pain measures have been psychometrically tested in youth with chronic pain. These include the Fear of Pain Questionnaire for Children (FOPQ-C) (Sieberg, Williams, & Simons, 2011), the Pediatric Pain Fear Questionnaire (PPFQ) (Huguet et al., 2011), and the Photograph Series of Daily Activities (PHODA-Youth) (Verbunt et al., 2015). The FOPQ-C includes 24 items relating to cognitions about pain (e.g., my pain controls my life), behaviors (e.g., I go immediately to lie down or rest when I feel really bad pain), and physiological responses to pain (e.g., I find it difficult to calm my body down when having pain). Five studies used the FOPQ-C; all conducted in the United States. Only one study (Cousins, Cohen, & Venable, 2015) was conducted separately from the original instrument developer. Four studies reported internal consistencies for their own sample, which ranged from 0.87 to 0.94 for the full measure (including both fear and avoidance subscales). The internal consistency from the first study investigating psychometric properties for the fear of pain subscale was 0.89 (Simons et al., 2011).
Similar to the FOPQ-C, the PPFQ (Huguet et al., 2011) also includes cognitive (e.g., when you are having pain, are you afraid you will have to go to the hospital?), behavioral (e.g., when you are having pain, do you stop what you are doing?), and physiological (e.g., when you are having pain, do you feel faint?) items. This measure has been used in one study, which was the first psychometric investigation study (internal consistency = 0.83–0.89). There are two subscales within this measure: fearful thoughts scale and fearful physical feelings and behaviors scale.
The PHODA-Youth (Verbunt et al., 2015) has a different response format from the other measures in this review. Youth are shown photos of daily activities on a computer and asked to imagine themselves doing each activity and then to rate how harmful they perceive the movement to be because of their pain (0–10). Photos are positioned on a scale to provide a rank order of feared activities. Three subscales emerge from this measure: activities of daily life, intensive physical activities, and social activities. We only identified one study using this measure, which was the first investigation of psychometric properties of this measure. The internal consistency was 0.98. The PHODA-Youth and PPFQ have each been used in only one study at the date of our search.
Aim 2: Assessment of Evidence-Based Measures (SPP Criteria)
We used the SPP evidence-based assessment criteria to evaluate each measure using information concerning publications in peer-reviewed articles, and psychometric properties reported (Cohen et al., 2008). Internal consistency reliabilities were adequate-to-good for all measures, although there was relatively little data presented on other psychometric properties of instruments (test–retest reliability; factor structure; discriminant validity). We found that most measures were well established (see Table II). Only two of the seven measures were classed as promising (PPFQ, PHODA-Youth) because of only being used in one peer-reviewed manuscript.
Aim 3: Meta-Analyze Correlations of Each Measure With Pain Intensity, Disability, General Anxiety, and Depression
From the 54 studies, 31 reported correlation data, and 25 of those studies reported correlation data between a cognitive-affective measure and at least one target variable (i.e., pain intensity, disability, general anxiety, or depression). It was only possible to conduct meta-analysis on correlations pertaining to four measures, the PCS-C, FOPQ-C, BAPQ, and PCQ-IC subscale, which included three or more studies reporting correlation data on at least one target variable. There were two studies that reported correlation data for the PRI, but none included correlational data between the PRI and our target outcomes. The PPFQ and PHODA-Youth have been used only once and therefore did not include enough studies to conduct a meta-analysis, although they both reported correlations between the respective measures and our target outcomes. Therefore, we extracted and analyzed correlations related to the total score of the PCS-C, the fear of pain subscale of the FOPQ-C, the pain-specific anxiety subscale of the BAPQ, and the internalizing/catastrophizing subscale of the PCQ. The purpose of these analyses was to examine the pooled correlations as an indicator of the construct validity of the measures through the pattern of associations with pain-related variables specified in the fear-avoidance model including pain intensity, functional disability, general anxiety, and depression. See Table III for statistics relating to all analyses and Supplementary Material S4 for forest plots.
Table III.
Summary of Meta-Analyses on Correlations Between Cognitive-Affective Measures and Relevant Pain and Emotional Distress Variables
| Outcome | N studies | N participants | Effect size | 95% confidence intervals | I2 (%) |
|---|---|---|---|---|---|
| PCS-C | |||||
| Pain intensitya | 11 | 3,212 | 0.32 | 0.28–0.36 | 14.99 |
| Pain-related disabilityb | 12 | 2,797 | 0.42 | 0.38–0.46 | 23.55 |
| Depression | 6 | 1,422 | 0.53 | 0.43–0.63 | 74.91 |
| General anxiety | 5 | 2,112 | 0.51 | 0.45–0.57 | 49.05 |
| FOPQ-C fear of pain subscale | |||||
| Pain intensity | 3 | 701 | 0.19 | 0.11–0.27 | 16.70 |
| Pain-related disability | 5 | 1,303 | 0.45 | 0.36–0.55 | 73.55 |
| PCQ-IC | |||||
| Pain intensity | 5 | 609 | 0.22 | 0.12–0.32 | 30.33 |
| Pain-related disability | 6 | 717 | 0.32 | 0.20–0.44 | 61.81 |
| Depression | 4 | 414 | 0.48 | 0.39–0.57 | 14.69 |
| BAPQ pain-specific anxiety | |||||
| Pain-related disability | 3 | 1,185 | 0.46 | 0.37–0.56 | 53.64 |
Note. Bath Adolescent Pain Questionnaire = BAPQ; Fear of Pain Questionnaire for Children = FOPQ-C; Pain Catastrophizing Scale for Children = PCS-C; Pain Coping Questionnaire internalizing/catastrophizing scale = PCQ-IC.
Small effect size = 0.2; moderate effect size = 0.5; large effect size = 0.8.
I2: 0–40% might not be important; 30–60% moderate heterogeneity; 50–90% substantial heterogeneity; 75–100% considerable heterogeneity.
Trim and fill meta-analysis with one filled study: 0.41 (95% CI 0.37–0.45).
Trim and fill meta-analysis with one filled study: 0.42 (95% CI 0.33–0.52).
Pain Catastrophizing Scale for Children: Four analyses were run to investigate correlations between the PCS-C and pain-related variables. As predicted, small to moderate positive effects were found between higher scores on the PCS-C and pain intensity, functional disability, general anxiety, and depression. Findings showed that higher pain catastrophizing was associated with increased pain intensity, disability, and symptoms of general anxiety and depression. The heterogeneity ranged from low to substantial across analyses. We were able to run publication bias analyses on two of the four variables (pain and disability) and found that one study may have been missing from each analysis. Despite this, the overall effects were similar to findings in the meta-analyses (Table III). The fail-safe N in the analysis investigating relationships between PCS-C and pain intensity was n = 8,238 and for the PCS-C and pain-related disability was n = 9,208.
Fear of Pain Questionnaire for Children: We ran two analyses on data relating to the FOPQ-C-fear of pain subscale. As expected, a small effect was found between higher scores on the FOPQ-C-fear of pain subscale and pain intensity, while a moderate effect was found between the FOPQ-C subscale and pain-related disability. Higher fear of pain was associated with increased pain intensity and pain-related disability. The heterogeneity for pain intensity was low, but was considerable for the analysis investigating pain-related disability. There were insufficient data to analyze associations between the fear of pain subscale and depression or general anxiety.
Pain Coping Questionnaire internalizing/catastrophizing scale: Three analyses investigating the correlations between the internalizing/catastrophizing subscale of the PCQ and pain intensity, functional disability, and depression were analyzed, revealing small to moderate effects. These findings indicate that higher scores on the subscale are associated with higher pain intensity, disability, and depression in children and adolescents with chronic pain. The heterogeneity ranged from low to substantial across analyses. There were insufficient data presented in studies to analyze associations between the PCQ-IC and general anxiety.
Bath Adolescent Pain Questionnaire pain-specific anxiety subscale: Finally, one analysis could be run investigating the association between pain anxiety measured by the BAPQ and pain-related disability. As expected, the analysis revealed a moderate positive effect, indicating that higher pain-specific anxiety was significantly associated with higher disability in this population. This analysis was moderately heterogeneous. There were insufficient data to run analyses between pain-specific anxiety and the variables pain intensity, depression, or general anxiety.
Discussion
This is the first comprehensive review of cognitive-affective measures that have been used in pediatric chronic pain populations. We aimed to summarize measures of pain anxiety, pain catastrophizing, and fear of pain that have been psychometrically tested in children and adolescents with chronic pain. These concepts were chosen following the large amount of research conducted in this area after the development and validation of the pediatric fear-avoidance model (Asmundson et al., 2012; Simons & Kaczynski, 2012). We had three specific aims. First, we set out to identify studies that had used cognitive-affective measures in young people with chronic pain and to summarize the measures. We identified seven measures that had been used across 54 studies: three that assessed fear of pain, three that assessed pain catastrophizing, and one that assessed pain anxiety. Of the seven measures, three were subscales of broader measures on coping or multidimensional functioning. Internal consistency was the most commonly reported reliability estimate, but studies differed on whether this was reported for the study sample, from the first paper investigating the psychometrics for the measure, or both. The measures have been used across differing chronic pain conditions, in youth with a mean of 13.74 years of age, which is a developmental period when chronic pain peaks in childhood (King et al., 2011). Six of the measures were traditional child self-report tools with Likert rating scales. The PHODA-Youth uses a series of photos of different activities that adolescents rank, which increases the potential personal relevance of the measure compared with traditional self-report assessments.
All measures included cognitive items, asking adolescents to report on pain-related thoughts. It is worth noting that the catastrophizing measures do not include items regarding behavior, which is consistent with catastrophizing being conceptualized as a cognitive process. Most other measures also included behavioral responses to pain; however, the primary domain assessed in pain anxiety and pain catastrophizing measures are cognitions about pain. Behavioral and physiological items are less common across these measures. Only the FOPQ-C and PPFQ include more than one item of behavioral or physiological responses to impending pain.
We identified clear similarities and differences in the measures included in this review. While no items across the measures are identical, there are common wording and phrasing across most measures. For example, when I hurt I can’t stop thinking about the pain (FOPQ-C item 8), when I am in pain, I can’t keep it out of mind (PCS-C item 9), and when you are having pain, is there nothing else other than the pain you can think of (PPFQ item 6) are similar in concept. Similarly, most measures use terms such as worry, afraid, and scared in their items. Thus, measures are more overlapping than distinct conceptually. Also, despite categorizing the measures as labeled in the original validation paper (i.e., pain anxiety, pain catastrophizing, and fear of pain), researchers and clinicians should think carefully about whether these labels are accurate and truly reflective of the items included, and how those concepts relate to the wider field of pediatric psychology. Similarly, these overlapping concepts likely account for the similar pattern of associations found with pain-related variables across all of the cognitive-affective measures.
Our second aim was to establish the evidence base of each measure according to the SPP evidence-based assessment criteria (Cohen et al., 2008). The evidence-based assessment has a relatively low threshold. For a measure to be well established, authors validating the measure must have reported psychometrics, have been used by more than one author group, and be accessible. Therefore, most of the measures included in this review were graded as “well-established.” The PPFQ did not reach this threshold, because of only being used by one author group. Further, since the date of our search, the PHODA-Youth has recently been psychometrically tested in youth with chronic pain by a separate author group (Simons et al., 2017), and therefore we rated this as well established to reflect the most up-to-date state of the field. The FOPQ-C has also been psychometrically tested in Dutch (Dekker et al., 2017) and German (Flack, Gerlach, Simons, Zernikow, & Hechler, 2017), demonstrating the quickly evolving research in this field. Despite measures being well validated and having good reliability, there were differing psychometrics supporting the validity and reliability of each measure. In general, there remain gaps in available psychometrics of these cognitive-affective measures, particularly in test–retest reliability, discriminant validity, and factor analysis, which should be the focus of future research. This reduces our confidence in being able to assess changes throughout treatment, as psychometrics such as test–retest reliability and sensitivity to change has not been conducted for most measures.
Third, we meta-analyzed the correlations between each of the cognitive-affective measures and variables (i.e., pain intensity, disability, generalized anxiety, and depression) specified in the pediatric fear-avoidance model of pain to examine construct validity. We were only able to conduct analyses with four questionnaires, and we were only able to run analyses on all four variables using the PCS-C. Correlations were not reported in all studies, and we did not contact authors to request additional data, which limited the number of meta-analyses we were able to conduct. Despite this, we found small correlations between the FOPQ-C, and PCQ-IC and pain intensity. Moderate associations were found between the PCS-C and pain intensity. Stronger correlations were found between each of the four measures and functional disability, supporting previous research that cognitive-affective measures are more strongly associated with disability than with pain intensity. As expected, moderate correlations were identified between the PCS-C and generalized anxiety and depression. Heterogeneity ranged from low to considerable, showing there were differences in the populations and specific variables included in the analyses. Despite this variability, most (6 of 10) analyses were judged to be low or moderate heterogeneity. Most analyses were not large enough to conduct publication bias analyses. Nevertheless, in the PCS-C analyses, where we were able to conduct two publication bias analyses, we found similar effects to the meta-analyses and a high fail-safe N (>8,000) demonstrating that a large number of studies are needed for the effect to be overturned. Of a potential 28 analyses, we could only conduct 10. Therefore, we are still unsure whether many of the questionnaires correlate with relevant variables in the pediatric fear-avoidance model of pain. Nevertheless, our findings provide some support for this model, that cognitive-affective measures are associated with pain intensity, functional disability, and depression. These associations are all cross-sectional, and further longitudinal work is needed in this population to validate this model.
There are some limitations that should be considered. We attempted to capture all studies that used cognitive-affective measures within pediatric chronic pain populations; however, our search criteria may have not captured additional studies, where cognitive-affective measures were used but were not a main focus or outcome. The results should be interpreted in light of other considerations. We were specific in our focus to only include measures that had been psychometrically tested in children or adolescents with chronic pain. There are other studies conducted in pediatric chronic pain samples but included cognitive-affective measures that had not previously been tested psychometrically for this population and therefore did not meet the inclusion criteria for this review. Similarly, there are child cognitive-affective measures that have been validated in healthy populations, but no psychometric testing has occurred in a chronic pain sample (e.g., Child Pain Anxiety Symptoms Scale (Pagé, Fuss, Martin, Escobar, & Katz, 2010)). Further, there were individual catastrophizing items within some measures, but no summary subscale, for example, Waldron/Varni Pediatric Pain Coping Inventory (Varni et al., 1996). With regard to the meta-analyses, we did not contact authors to request unpublished data, which restricted our publication bias analyses.
Several research and practice implications have emerged from this review. First, this review provides a summary for clinicians when choosing cognitive-affective measures for use in children and adolescents with chronic pain. To guide this choice, we highlighted the similarities and differences between the measures, and we provided an evidence-based assessment (SPP criteria) for each measure. Clinicians and researchers should be mindful when selecting measures in this area, given the potential for overlapping constructs and redundancy of using more than one cognitive-affective measure in the same population. A factor analysis on all seven cognitive-affective measures in children who have chronic pain would be ideal to determine overlap in items between measures and whether measures might be condensed into a single concise measure. Consideration should also be given to whether measures labelled as pain anxiety, catastrophizing, or fear of pain overlap with outcome measures. For example, I do not go to school because it makes my pain worse (FOPQ, Item 21) and I avoid activities that cause pain (BAPQ pain specific subscale, Item 2) could be interpreted as reflecting disability because of pain. Potential issues regarding content overlap have also been identified in other areas of pain assessment, for example, a recent content analysis of acceptance measures used in adults with chronic pain found that many items pertain to pain control rather than acceptance of pain (Lauwerier et al., 2015).
In regard to research, it is clear that there is a lack of pediatric cognitive-affective measures that have been developed using a “bottom-up” approach (i.e., developed using children’s typical thoughts and behaviors rather than adapting from adult measures). PROMIS measures designed and validated by the NIH have begun to address this issue but have not yet released a measure pertaining to pain anxiety, fear of pain, or pain catastrophizing specifically. It is not clear whether new measures are needed taking a bottom-up approach, or whether measures included in this review could or should be adapted. Nevertheless, any new or adapted measure should include cognitive, behavioral, and physiological responses to pain, as they are often inextricably experienced. Most measures included in this review (excluding the BAPQ) were adapted from one or more adult measures, with differing levels of child input. Some measures asked for feedback on items from child and adolescent pilot participants, while others perform some degree of cognitive testing to ensure that items are easily understood by children and adolescents. Developmental considerations will need to guide these decisions. For example, we have previously contested labeling child worries as “catastrophic” because of the important developmental considerations and the negative connotations associated with adult catastrophizing, indicating that a bottom-up approach to understanding child worry about pain will be useful (author blinded) cognitive-affective measures for younger children with chronic pain are scarce. Most measures in this review are psychometrically valid in children ≥8 years of age. The PRI is validated in children as young as 5 years old. Although chronic pain is less prevalent at this age, a better range of measures may be needed. A review of parent cognitive-affective measures would also be useful to conduct to assess whether parent perceptions are associated with their child’s perceptions.
Further, as alluded to earlier, comprehensive psychometrics are needed for each measure, particularly for measures used in treatment studies to determine treatment efficacy. Measures that are sensitive to change and have high test–retest reliability are essential for optimizing repeat assessment of outcomes over time. Test–retest reliability analyses were conducted with some measures considered in this review, but none assessed sensitivity to change following intervention. Determining whether these measures that are used in intervention studies can detect change is an important future direction of research. More detailed reporting of reliability and validity analyses are needed to fully understand the domains in which each measure has been tested. For example, construct validity is a broad term that encompasses different validity tests used to assess whether a measure assesses what it claims to (e.g., convergent/divergent validity; content validity; criterion validity). As such, we are unsure of the specific psychometric testing conducted on some of the measures included in this review because of lack of detailed reporting.
In conclusion, we identified seven measures assessing cognitive-affective constructs of pain anxiety, pain catastrophizing, and fear of pain in youth with chronic pain. Most measures are well established and assess cognitive and behavioral responses to pain. Most measures have strong–moderate correlations with pain intensity, disability, general anxiety, and depression, providing support for the pediatric fear-avoidance model of pain and a growing collection of measures to assess these key constructs.
Supplementary Data
Supplementary data can be found at: http://www.jpepsy.oxfordjournals.org/.
Funding
This work was supported by the National Institute of Child Health & Human Development of the National Institutes of Health under Award Number 2K24HD060068-07 (T.M.P. [principal investigator]). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflicts of interest: None declared.
Supplementary Material
References
- Asmundson G. J. G., Noel M., Petter M., Parkerson H. (2012). Pediatric fear-avoidance model of chronic pain: Foundation, application and future directions. Pain Research and Management, 17, 397–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen L. L., La Greca A. M., Blount R. L., Kazak A. E., Holmbeck G. N., Lemanek K. L. (2008). Introduction to special issue: Evidence-based assessment in pediatric psychology. Journal of Pediatric Psychology, 33, 911–915. doi:10.1093/jpepsy/jsj115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cousins L. A., Cohen L. L., Venable C. (2015). Risk and resilience in pediatric chronic pain: Exploring the protective role of optimism. Journal of Pediatric Psychology, 40, 934–942. doi:10.1093/jpepsy/jsu094 [DOI] [PubMed] [Google Scholar]
- Crombez G., Bijttebier P., Eccleston C., Mascagni T., Mertens G., Goubert L., Verstraeten K. (2003). The child version of the pain catastrophizing scale (PCS-C): A preliminary validation. Pain, 104, 639–646. [DOI] [PubMed] [Google Scholar]
- Dekker C., Bastiaenen C. H. G., de Vries J. E., Simons L. E., Goossens M. E. J. B., Verbunt J. A. M. C. F. (2017). Dutch version of the fear of pain questionnaire for adolescents with chronic pain. Disability and Rehabilitation, 3, 1–7. [DOI] [PubMed] [Google Scholar]
- Duval S., Tweedie R. (2000). A nonparametric “trim and fill” method of accounting for publication bias in meta-analysis. Journal of the American Statistical Association, 95, 89–98. doi:10.1080/01621459.2000.10473905 [Google Scholar]
- Eccleston C., Fisher E., Vervoort T., Crombez G. (2012). Worry and catastrophizing about pain in youth: a re-appraisal. Pain 1538, 1560–62. [DOI] [PubMed] [Google Scholar]
- Eccleston C., Jordan A., McCracken L. M., Sleed M., Connell H., Clinch J. (2005). The Bath Adolescent Pain Questionnaire (BAPQ): Development and preliminary psychometric evaluation of an instrument to assess the impact of chronic pain on adolescents. Pain, 118, 263–270. [DOI] [PubMed] [Google Scholar]
- Eccleston C., Palermo T. M., Williams A. C, Lewandowski Holley A., Morley S., Fisher E., Law E. (2014). Psychological therapies for the management of chronic and recurrent pain in children and adolescents. Cochrane Database of Systematic Reviews, 5, CD003968. doi:10.1002/14651858.CD003968.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher E., Heathcote L., Palermo T. M., de C Williams A. C., Lau J., Eccleston C. (2014). Systematic review and meta-analysis of psychological therapies for children with chronic pain. Journal of Pediatric Psychology, 39, 763–782. doi:10.1093/jpepsy/jsu008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher E., Law E., Palermo T. M., Eccleston C. (2015). Psychological therapies (remotely delivered) for the management of chronic and recurrent pain in children and adolescents. Cochrane Database of Systematic Reviews, 2014, CD011118. Retrieved from doi:10.1002/14651858.CD011118.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flack F., Gerlach A. L., Simons L. E., Zernikow B., Hechler T. (2017). Validation of the German Fear of Pain Questionnaire in a sample of children with mixed chronic pain conditions. European Journal of Pain. DOI: 10.1002/ejp.1022. [DOI] [PubMed] [Google Scholar]
- Forgeron P. A., Evans J., McGrath P. J., Stevens B., Finley G. A. (2013). Living with difference: Exploring the social self of adolescents with chronic pain. Pain Research and Management, 18, e115–e123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gauntlett-Gilbert J., Eccleston C. (2007). Disability in adolescents with chronic pain: Patterns and predictors across different domains of functioning. Pain, 131, 132–141. [DOI] [PubMed] [Google Scholar]
- Hermann C., Hohmeister J., Zohsel K., Tuttas M. L., Flor H. (2008). The impact of chronic pain in children and adolescents: Development and initial validation of a child and parent version of the pain experience questionnaire. Pain, 135, 251–261. [DOI] [PubMed] [Google Scholar]
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane-handbook.org. [Google Scholar]
- Higgins J. P. T., Green S. (2011). Cochrane handbook for systematic reviews of intervetnions, Version 5. 1. 0. The Cochrane Collaboration. [Google Scholar]
- Huguet A., McGrath P. J., Pardos J. (2011). Development and preliminary testing of a scale to assess pain-related fear in children and adolescents. Journal of Pain, 12, 840–848. [DOI] [PubMed] [Google Scholar]
- Huguet A., Miró J. (2008). The severity of chronic pediatric pain: An epidemiological study. The Journal of Pain, 9, 226–236. [DOI] [PubMed] [Google Scholar]
- Jennions M. D., Moller A. P. (2002). Publication bias in ecology and evolution: An empirical assessment using the ′trim and fill′ method. Biological Reviews of the Cambridge Philosophical Society, 77, 211–222. [DOI] [PubMed] [Google Scholar]
- Kashikar-Zuck S., Goldschneider K. R., Powers S. W., Vaught M. H., Hershey A. D. (2001). Depression and functional disability in chronic pediatric pain. The Clinical Journal of Pain, 17, 341–349. [DOI] [PubMed] [Google Scholar]
- Kashikar-Zuck S., Parkins I. S., Graham T. B., Lynch A. M., Passo M., Johnston M., Schikler K. N., Hashkes P. J., Banez G., Richards M. M. (2008). Anxiety, mood, and behavioral disorders among pediatric patients with juvenile fibromyalgia syndrome. The Clinical Journal of Pain, 24, 620–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King S., Chambers C. T., Huguet A., MacNevin R. C., McGrath P. J., Parker L., MacDonald A. J. (2011). The epidemiology of chronic pain in children and adolescents revisited: A systematic review. Pain, 152, 2729–2738. [DOI] [PubMed] [Google Scholar]
- Lauwerier E., Caes L., Van Damme S., Goubert L., Rosseel Y., Crombez G. (2015). Acceptance: what's in a name? A content analysis of acceptance instruments in individuals with chronic pain. The Journal of Pain, 16, 306–317. doi:10.1016/j.jpain.2015.01.001 [DOI] [PubMed] [Google Scholar]
- Merskey H., Bogduk N. (1994). Classification of chronic pain: descriptions of chronic pain syndromes and definitions of pain terms, IASP press Seattle. [Google Scholar]
- Pagé M. G., Fuss S., Martin A. L., Escobar E. M. R., Katz J. (2010). Development and preliminary validation of the child pain anxiety symptoms scale in a community sample. Journal of Pediatric Psychology, 35, 1071–1082. [DOI] [PubMed] [Google Scholar]
- Palermo T. M., Lewandowski A. S., Long A. C., Burant C. J. (2008). Validation of a self-report questionnaire version of the Child Activity Limitations Interview (CALI): The CALI-21. Pain, 139, 644–652. doi:10.1016/j.pain.2008.06.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perquin C. W., Hazebroek-Kampschreur A. A. J. M., Hunfeld J. A., Bohnen A. M., van Suijlekom-Smit L. W. A., Passchier J., van der Wouden J. C. (2000). Pain in children and adolescents: A common experience. Pain, 87, 51–58. [DOI] [PubMed] [Google Scholar]
- Rachman S. (2013). Anxiety, 3rd edn Hove: Psychology Press. [Google Scholar]
- Reid G. J., Gilbert C. A., McGrath P. J. (1998). The pain coping questionnaire: Preliminary validation. Pain, 76, 83–96. [DOI] [PubMed] [Google Scholar]
- Rosenthal R. (1979). The file drawer problem and tolerance for null results. Psychological Bulletin, 86, 638. [Google Scholar]
- Sieberg C. B., Williams S., Simons L. E. (2011). Do parent protective responses mediate the relation between parent distress and child functional disability among children with chronic pain? Journal of Pediatric Psychology, 36, 1043–1051. doi: 10.1093/jpepsy/jsr043 [DOI] [PubMed] [Google Scholar]
- Simons L. E., Kaczynski K. J. (2012). The fear avoidance model of chronic pain: examination for pediatric application. The Journal of Pain, 13, 827–835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons L. E., Pielech M., McAvoy S., Conroy C., Hogan M., Verbunt J. M. G. (2017). Photographs of Daily Activities (PHODA)-Youth English: Validating a targeted assessment of worry and anticipated. Pain, 158, 912–921. [DOI] [PubMed] [Google Scholar]
- Simons L. E., Sieberg C. B., Carpino E., Logan D. E., Berde C. (2011). The Fear of Pain Questionnaire (FOPQ): Assessment of pain-related fear among children and adolescents with chronic pain. The Journal of Pain, 12, 677–686. doi:10.1016/j.jpain.2010.12.008 [DOI] [PubMed] [Google Scholar]
- Sullivan M. J. L., Bishop S. R., Pivik J. (1995). The pain catastrophizing scale: Development and validation. Psychological Assessment, 7, 524. [Google Scholar]
- Thastum M., Zachariae R., Scholer M., Herlin T. (1999). A Danish adaptation of the pain coping questionnaire for children: Preliminary data concerning reliability and validity. Acta Paediatrica, International Journal of Paediatrics, 88, 132–138. [DOI] [PubMed] [Google Scholar]
- Tran S. T., Jastrowski Mano K. E., Hainsworth K. R., Medrano G. R., Anderson Khan K., Weisman S. J., Davies W. H. (2015). Distinct influences of anxiety and pain catastrophizing on functional outcomes in children and adolescents with chronic pain. Journal of Pediatric Psychology, 40, 744–755. doi:10.1093/jpepsy/jsv029 [DOI] [PubMed] [Google Scholar]
- Turk D. C., Wilson H. D. (2010). Fear of pain as a prognostic factor in chronic pain: Conceptual models, assessment, and treatment implications. Current Pain and Headache Reports, 14, 88–95. doi:10.1007/s11916-010-0094-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varni J. W., Waldron S. A., Gragg R. A., Rapoff M. A., Bernstein B. H., Lindsley C. B., Newcomb M. D. (1996). Development of the Waldron/Varni pediatric pain coping inventory. Pain, 67, 141–150. [DOI] [PubMed] [Google Scholar]
- Verbunt J., Nijhuis A., Vikstrom M., Stevens A., Haga N., de Jong J., Goossens M. (2015). The psychometric characteristics of an assessment instrument for perceived harmfulness in adolescents with musculoskeletal pain (PHODA-youth). European Journal of Pain, 19, 695–705. doi: 10.1002/ejp.592 [DOI] [PubMed] [Google Scholar]
- Vlaeyen J. W. S., Crombez G., Linton S. J. (2016). The fear-avoidance model of pain. Pain, 157, 1588–1589. doi:10.1097/j.pain.0000000000000574 [DOI] [PubMed] [Google Scholar]
- Walker L. S., Smith C. A., Garber J., Van Slyke D. A. (1997). Development and validation of the pain response inventory for children. Psychological Assessment, 9, 392. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.