Abstract
The purpose of this study was to examine the occurrence and covariation of four eating disorder behaviors across the elementary, middle, and high school years. In a sample of 1,906 youth measured over 5 years at nine time points, from the past year of elementary school through the second year of high school, binge eating, purging (self-induced vomiting), compensatory exercise, and fasting behavior were assessed by self-report. Over the 5-year period, rates of binge eating and purging increased but rates of compensatory exercise and fasting decreased. Girls and boys did not differ in their rates of engagement in any of the behaviors. Within time, the behaviors covaried modestly. Health-care professionals are advised to assess each behavior individually, rather than base interventions on the presence or absence of a diagnosable eating disorder. Gender should not be a basis for assessing for the presence of any of these behaviors.
Keywords: adolescents, eating disorders, developmental perspectives
Introduction
Disordered eating represents a significant public health concern. Eating disorders are the third most common chronic illness among adolescents, behind asthma and obesity (Gonzalez, Kohn, & Clarke, 2007). Importantly, the incidence of eating disorders appears to be increasing over time (Micali, Hagberg, Petersen, & Treasure, 2013). Currently, the lifetime prevalence of eating disorders in adolescents is 13% before 20 years of age (Stice, Marti, & Rohde, 2013). Notably, only 0.8–1.7% meet criteria for anorexia nervosa, and 0.8–2.6% meet criteria for bulimia nervosa (Smink, van Hoeken, Oldehinkel, & Hoek, 2014; Stice et al., 2013), the two most commonly known and frequently studied eating disorders. The remaining 9–11% of affected adolescents fall into either the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5)’s Other Specified Feeding and Eating Disorder (OSFED) or Unspecified Feeding and Eating Disorder (UFED). OSFED describes a clinically significant eating disorder that does not meet criteria for an officially recognized diagnosis (American Psychiatric Association [APA], 2013). Similarly, UFED is used to describe individuals for whom full diagnostic criteria are not met, but the reason is unspecified or there is no adequate information to make a more definitive diagnosis (APA, 2013). Further, because dimensional measures of eating disorder behavior (a) appear to more validly reflect eating disorder-related dysfunction (Luo, Donnellan, Burt, & Klump, 2016) (by dysfunction we mean repeated engagement in behaviors that disrupt the health and well-being of the individual) and (b) yield higher rates of disordered eating among adolescents (Holling et al., 2007), diagnosis rates are likely to underestimate eating disorder dysfunction.
The intent of this exploratory research is to provide descriptive information on the natural course of reported binge eating, purging (self-induced vomiting), compensatory exercise (Davis, Guller, & Smith, 2016a, 2016b; Stiles-Shields, Goldschmidt, Boepple, Glunz, Le Grange, 2011), and fasting (Davis et al, 2016a, 2016b) across the early and mid-adolescent years for both girls and boys. Doing so is important for several reasons. First, although disordered eating behaviors are manifest as young as childhood (Combs, Pearson, Zapolski, & Smith, 2013; Nicholls, Lynn, & Viner, 2011; Tanofsky-Kraff, Faden, Yanovski, Wilfley, & Yanovski, 2005), most prospective research has emphasized middle adolescence to young adulthood. Second, eating disorder behaviors in youth are associated with current and future dysfunction (Gonsalves, Hawk, & Goodenow, 2014; Hughes et al., 2013; Tanofsky-Kraff et al., 2011) and continued engagement into adulthood (Neumark-Sztainer, Wall, Larson, Eisenberg, & Loth, 2011). Third, there is little prospective information on engagement in such behaviors by boys. Fourth, little is known about the degree of stability of reports of eating disorder behaviors over time in youth, whether girls or boys. Fifth, we know little about the degree to which different eating disorder behaviors covary in youth. This investigation will be an extension of the work by Combs et al. (2013). We followed the sample first reported on by Combs et al. (2013) for an additional six waves, thus spanning the period representing the past year of elementary school through the second year of high school.
Prospective Research Among Adolescents
Elevated rates of dieting, disordered eating, compensatory exercise, and body dissatisfaction generally remain constant or increase from adolescence to young adulthood (Neumark-Sztainer et al., 2011) and often result in the onset of diagnosable eating disorders (Nagl et al, 2016; Rohde, Stice, & Marti, 2015). A large percentage of highly symptomatic 14-year-old girls remained highly symptomatic or transitioned to the OSFED class at ages 16 and 18 years (Micali et al., 2016).
The small amount of research with early adolescents paints a similar picture. First, there are meaningful symptom levels among elementary school youth (Combs et al., 2013; Tanofsky-Kraff et al., 2011). Second, there is fluctuation in symptom reports within an overall context of stability, both for reports across 6-month intervals during the transition to middle school (Combs et al., 2013) and from ages 10 to 14/15 years (Tanofsky-Kraff et al., 2011).
Youth Eating Disorder Behaviors Are Associated With Dysfunction
Even a single eating disorder behavior predicts subsequent dysfunction (Tanofsky-Kraff et al., 2011). More broadly, dysfunction in youth predicts diagnosable eating disorders in late adolescence and adulthood (Kotler, Cohen, Davies, Pine, & Walsh, 2001). In addition, eating disorder behaviors are concurrently associated with other forms of dysfunction, such as negative affect and depression (Hughes et al. 2013; Leon, Fulkerson, Perry, Keel, & Klump, 1999; Pearson, Zapolski, & Smith, 2015).
Eating Disorder Symptom Development in Boys
Among older youth, males are more likely to engage in nonpurging compensatory behaviors such as driven exercise (Allen et al., 2013; Mond et al., 2014; Stiles-Shields et al., 2011) and fasting (Allen et al., 2013; Mond et al., 2014; Pisetsky, May Chao, Dierker, May, & Striegel-Moore, 2008) compared with purging behaviors such as self-induced vomiting, for weight control. Additionally, boys’ age of onset for eating disorder behavior might be lower than that of girls (Micali et al., 2013).
Among younger youth, boys have received little scrutiny, although they were included in both Combs et al. (2013) and Tanofsky-Kraff et al. (2011). In each of these investigations, boys did not differ significantly from girls in terms of rates of disordered eating behavior (Combs et al., 2013) or negative outcomes (i.e., development of binge eating disorder; Tanofsky-Kraff et al., 2011). The tendency of eating disorder research to neglect a potentially vulnerable population such as young boys leads to the following exploratory questions: What is the rate of engagement in eating disorder behaviors among boys throughout middle school and into high school? Are eating disorder behaviors stable among boys during this time? Do the different behaviors covary? Does one eating disorder behavior predict subsequent engagement in other such behaviors?
What Is the Rate of Engagement in Eating Disorder Behaviors Among Youth?
Despite consistent reports of the prevalence of diagnosable, DSM-5 criteria-meeting eating disorders, the rate of engagement in individual eating disorder behaviors over the critical periods of childhood and adolescence is relatively unclear. Because adolescent symptoms of eating disorders are indicative of distress, dysfunction, and future psychopathology, it is important to understand patterns and trends in symptom engagement. Previous studies indicate prevalence rates for binge eating among children ranging from 9 to 30% (Tanofsky-Kraff, 2008). With regard to compensatory behaviors among adolescents, up to 23.6% report exercise for weight loss, up to 23.1% report food restriction, and up to 0.2% report purging (Micali et al., 2014).
Are Eating Disorder Behaviors Stable Over Time Among Youth?
Among childhood to early adolescent youth, there are both stability and fluctuation in reports of having engaged in a range of eating disorder behaviors (Combs et al., 2013; Tanofsky-Kraff et al., 2011). For example, half of 10-year-olds who reported loss of control eating continued to report the behavior at 4–5-year follow-up (Tanofsky-Kraff et al., 2011). Odds ratios reflecting stability over the 6-month transition from elementary to middle school were 7.58 for binge eating, 11.75 for purging, and 20.27 for use of diuretics (Combs et al., 2013). A similar process of fluctuation within the context of overall stability has been observed in older adolescent samples (Flament et al., 2015; Rohde et al., 2015).
Do Eating Disorder Symptoms Covary in Youth?
Across the transition from elementary to middle school, eating disorder symptom reports covaried significantly but only moderately (Combs et al., 2013). The same is true among older adolescents (Flament et al., 2015; Rohde et al., 2015).
Do Eating Disorder Behaviors Predict Each Other Over Time?
Clues about the riskiness of one behavior compared with another can be evaluated by examining the prediction of one behavior to the next. With the recognition that eating disorder behaviors themselves predict future diagnosable disorders, it is plausible that the progression from engagement in one behavior to full-blown diagnosis occurs steadily over time. Thus, prediction from one behavior to multiple behaviors may prove useful.
The Current Study
As mentioned above, this work is an extension of Combs et al. (2013) using the same sample of participants. This study expands on that work by exploring two of the same variables, binge eating and purging, beyond the three waves assessed by Combs et al. (2013), six waves further into middle and high school. Additionally, this examination includes an exploration of compensatory exercise and fasting behavior at all nine waves, which Combs et al. (2013) did not assess.
We organized our report to address the following four questions: (1) What are the rates of eating disorder behaviors across these years by both girls and boys? (2) Are eating disorder behaviors stable over time? (3) Within gender, do eating disorder behaviors covary with each other? (4) Do eating disorder behaviors predict each other over time?
Method
Participants
Consenting participants included 1,906 children as part of a larger study described by Combs et al. (2013). Participants were assessed at nine time points: Spring of the last year of elementary school (5th grade) and every 6 months through the Spring of 8th grade (the past year of middle school) and then in the Spring of 9th and 10th grades. Data collection began in the Spring of 2009 and concluded in the Spring of 2014. At the initiation of the study, participants were on average 10.86 years. The gender breakdown of the sample was as follows: 968 (50.9%) boys and 938 (49.1%) girls. The racial and ethnic representation included European–American (60.9%), African–American (18.7%), Hispanic (8.2%), Asian (2.9%), Middle Eastern (0.4%), and other (8.8%).
Measures
Demographic and Background Questionnaire
This measure provided the assessment of the demographic information reported above. Demographic and background information was collected at each wave of the study.
Eating Disorder Examination-Questionnaire (EDE-Q))
To assess binge eating and compensatory behaviors, we used the EDE-Q, which is a self-report version of the Eating Disorder Examination semi-structured interview (Cooper & Fairburn, 1993; Fairburn & Beglin, 1994). The EDE-Q has been shown to have good reliability and validity, particularly in clinical samples (Cooper & Fairburn, 1993; Luce & Crowther, 1999; Mond, Hay, Rodgers, Owen, & Beumont, 2004).
Following existing recommendations for use of the measure with youth (Carter, Stewart, & Fairburn, 2001), the EDE-Q was adapted for a child and adolescent sample by using age-appropriate wording, defining potentially confusing concepts, and shortening the length of time from which to recall behaviors to the past 2 weeks. For example, the word “restrict” was changed to “cut back on,” and the word “influence” was changed to “control” throughout the measure. Terms such as “purging” and “binge eating” were defined.
We defined binge eating as binge eating with loss of control (see Tanofsky-Kraff et al., 2011). For youth to be considered positive for binge eating, they had to endorse “yes” for two items: one that assessed episodes of objective binge eating, and one that assessed loss of control during these episodes. To be scored positively for purging, participants had to respond “yes” to a question asking if they had made themselves sick (throw up) in the past 2 weeks as a means of controlling their shape or weight. We measured compensatory exercise with the question, “Over the past two weeks, have you exercised a lot as a way to control your weight or because you ate a lot?” The item was dichotomous.
To measure fasting behavior, we used the item “Over the past 2 weeks, have you gone for long periods of time (8 hr or more) without eating to control your shape or weight?” Responses were dichotomous.
Procedure
Data Collection
The following procedure was approved by the university’s institutional review board and by the participating school systems and was used at all nine waves of the study. The questionnaires were administered in school cafeterias or classrooms during school hours (23 public elementary schools for Wave 1, 19 public middle schools for Waves 2–7, and seven public high schools and two private high schools for Waves 8 and 9). A passive consent procedure was used. Each family was sent a letter, through the U.S. Mail, introducing the study as a longitudinal investigation in which their children would complete a questionnaire during school hours. Families were asked to return an enclosed, stamped letter or call a phone number if they did not want their child to participate. Of 1,988 fifth grade students in the participating schools, 1,906 (95.8%) participated. Reasons for not participating included family or youth declination of consent, and other reasons such as language disabilities that precluded completing the measures. At each wave, participants were provided an assent form before participating. Students who decided to participate signed the form and then filled out the questionnaires.
It was made clear to the students that their responses on the questionnaires were to be kept confidential, and no one outside of the research team would see them. The research team introduced a federal certificate of confidentiality for the project and emphasized that the team was legally bound to keep all responses confidential. After each participant signed the assent form, the researchers then passed out packets of questionnaires. The questionnaire administration took ≤60 min. There was no compensation for participation (except for those who moved out of district). Those who did move out of the study’s school districts were contacted and asked to complete the forms by mail and were paid $30 for doing so in 6th, 7th, and 8th grades and $40 for doing so in 9th and 10th grades. Of the 1,906 participants, 109 completed the forms out of their school district and were paid for doing so.
Data Analysis
We report on results of three sets of analyses. First, we present the frequencies of engagement in each behavior at each wave by gender. Second, we present the results of latent growth curve models for each behavior over time. Using Mplus and the structural equation modeling (SEM) framework (Muthen & Muthen, 2004–2010), we modeled growth in each behavior, measured dichotomously. We modeled time since baseline because we accommodated that fact that the last two waves were 1 year from the previous wave. For growth model estimation, the standard SEM-derived baseline model is not appropriate, thus rendering standard relative fit indices such as the comparative fix index (CFI) and the nonnormed fit index (NNFI) inaccurate (Wu, West, & Taylor, 2009). Accordingly, we report two absolute fit indices, the root mean square error of approximation (RMSEA) and the standardized root mean square residual (SRMR) to judge model fit.
Third, we present the results of two SEMs followed by tests of whether those models were invariant across gender. The contribution of the SEM models is to test whether a given behavior predicts both the same behavior and other disordered eating behaviors in the future. In each of the two SEM models, we allowed cross-sectional associations between all variables or disturbance terms. We used maximum likelihood estimation robust to violations of normality. The first SEM (Model 1) specified autoregressive predictions within each eating disorder behavior (i.e., binge eating, purging, compensatory exercise, and fasting). Thus, this model involved, for example, binge eating at each wave predicting binge eating at the subsequent waves. In Model 2, we added pathways from each behavior assessed at Wave 1, the Spring of 5th grade, to the other behaviors. For example, we tested simultaneously whether binge eating at Wave 2 was predicted by Wave 1 binge eating, Wave 1 purging, Wave 1 compensatory exercise, and Wave 1 fasting. If this model fits better than Model 1, one concludes that there were significant cross-lagged predictions from one behavior to a different subsequent behavior. One can then examine the significance of individual pathways to describe the nature of the cross-lagged prediction. We then tested whether each model was invariant across gender. To do so, we tested a model specifying all prospective paths to be equal across gender. If there is no loss in model fit when adding these constraints, there is no basis for inferring that prospective prediction among the behaviors differs by gender. Because of the large number of comparisons, we used a conservative significance level of p < .001.
For the SEM prediction model, we used all four fit indices. Guidelines for what constitutes good fit vary. CFI and NNFI values above either 0.90 or 0.95 are thought to represent very good fit (Hu & Bentler, 1999; Kline, 2015). RMSEA values of ≤0.06 are thought to indicate a close fit, 0.08 a fair fit, and 0.10 a marginal fit, and SRMR values <0.09 are thought to indicate a good fit (Browne & Cudeck, 1993; Hu & Bentler, 1999). Models are judged to fit the data well when good fit is supported by most fit indices. We also report the model chi-square. To test for gender invariance, we compared the model with predictive pathways constrained to be equal to the model without those constraints, using the corrected chi-square difference test and comparison of CFI and NNFI values between the two models.
Results
Participant Retention
Of the full sample of 1,906 youth, the percentage of participants ranged from 1,843 (96.7%: the remaining 63 participants were sick for each Wave 1 data collection) at Wave 1 to 1,416 (74.3%) at Wave 9. Retention from one wave to the next ranged from 94.2 to 98.3%. At each wave, participating and nonparticipating participants did not differ on any study variables, so we inferred that data were missing at random. We therefore used the expectation maximization procedure to impute missing values, a procedure shown to more accurately approximate population data than traditional, alternative methods, such as case deletion or mean substitution (Enders, 2006; Little & Rubin, 1989). As a result, we were able to make full use of the entire sample of n = 1,906.
Possible Effects Because of School Membership
To determine whether there was significant covariance among the study variables because of participants attending the same school, intraclass coefficients were calculated for each variable (using elementary school membership, n = 23, as the nesting variable). Intraclass coefficients were all 0.00; therefore, we concluded that school membership was unrelated to study variables.
Question 1: What Are the Rates of Eating Disorder Behaviors for Girls and Boys?
The top panel of Table I provides frequencies by wave of each eating disorder behavior reported by girls in the sample: compensatory exercise, fasting, binge eating, and purging. Boys’ data are presented in the bottom panel of Table I. Girls and boys engaged in comparable levels of binge eating, purging, compensatory exercise, and fasting across 5th through 10th grades. By the end of 10th grade (Wave 9), 13.6% of girls and 12.7% of boys endorsed binge eating. Purging was indicated by 3.0% of girls and 3.4% of boys. Compensatory exercise was endorsed by 14.4% of girls and 12.9% of boys. Fasting was present in 7.7% of girls and 7.8% of boys.
Table I.
Presence of Nonpurging Compensatory Behaviors, Binge Eating, and Purging at Waves 1–9
| Girls’ | Wave 1 | Wave 2 | Wave 3 | Wave 4 | Wave 5 | Wave 6 | Wave 7 | Wave 8 | Wave 9 |
|---|---|---|---|---|---|---|---|---|---|
| Behavior | N (% of sample) | N (% of sample) | N (% of sample) | N (% of sample) | N (% of sample) | N (% of sample) | N (% of sample) | N (% of sample) | N (% of sample) |
| Binge eating | 115 (12.3) | 84 (9.0) | 81 (8.7) | 59 (6.3) | 70 (7.5) | 83 (8.9) | 102 (10.9) | 144 (15.4) | 127 (13.6) |
| Purging | 38 (4.1) | 31 (3.3) | 21 (2.2) | 20 (2.1) | 27 (2.9) | 67 (7.1) | 92 (9.8) | 63 (6.7) | 28 (3.0) |
| Compensatory Exercise | 277 (29.5) | 195 (20.8) | 213 (22.8) | 150 (16.0) | 171 (18.3) | 165 (17.6) | 190 (20.3) | 131 (14.0) | 135 (14.4) |
| Fasting | 118 (12.6) | 99 (10.6) | 95 (10.1) | 78 (8.3) | 82 (8.8) | 135 (14.4) | 145 (15.5) | 84 (9.0) | 72 (7.7) |
| Boys’ | Wave 1 | Wave 2 | Wave 3 | Wave 4 | Wave 5 | Wave 6 | Wave 7 | Wave 8 | Wave 9 |
| Behavior | N (% of sample) | N (% of sample) | N (% of sample) | N (% of sample) | N (% of sample) | N (% of sample) | N (% of sample) | N (% of sample) | N (% of sample) |
| Binge eating | 120 (12.4) | 91 (9.4) | 72 (7.4) | 62 (6.4) | 64 (6.6) | 101 (10.4) | 88 (9.1) | 150 (15.4) | 123 (12.7) |
| Purging | 53 (5.5) | 33 (3.4) | 26 (2.7) | 20 (2.1) | 20 (2.1) | 95 (9.8) | 65 (6.7) | 60 (6.2) | 33 (3.4) |
| Compensatory Exercise | 295 (30.3) | 209 (21.5) | 216 (22.2) | 171 (17.6) | 161 (16.6) | 187 (19.3) | 178 (18.3) | 153 (15.8) | 125 (12.9) |
| Fasting | 129 (13.3) | 84 (8.6) | 89 (9.2) | 76 (7.8) | 80 (8.2) | 150 (15.4) | 114 (11.7) | 83 (8.5) | 76 (7.8) |
Note. Top panel, N = 938. In each cell, N = the number of children reporting engagement in the behavior; % refers to the percentage of the overall girls’ sample represented by the number. All behaviors are dichotomized yielding a range of 0–1.
Bottom panel, N = 968. In each cell, N = the number of children reporting engagement in the behavior; % refers to the percentage of the overall boys’ sample represented by the number. All behaviors are dichotomized yielding a range of 0–1.
Differences in frequency of binge eating and compensatory behaviors between genders were tested using chi-square analyses. None of the comparisons was significantly different at the p ≥ .001 level, indicating that the genders did not differ on the frequency of binge eating or compensatory behaviors.
Question 2: Are Eating Disorder Behaviors Stable Across Time for Girls and Boys?
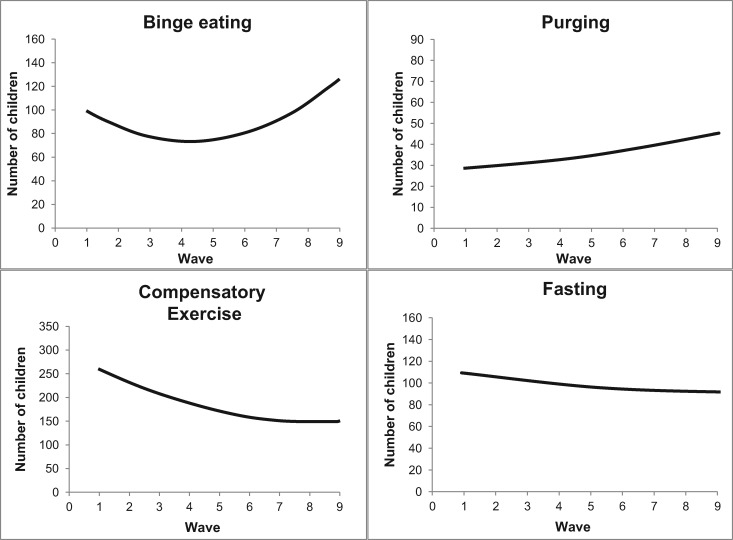
We addressed this question with two sets of analyses. First, we constructed growth models for each behavior across the nine waves from 5th grade through 10th grade to describe the pattern of change in each behavior across this developmental period. Figure 1 depicts the growth models that best fit the data for each behavior.1 For all four behaviors, a model reflecting significant linear change combined with a quadratic trend best fit the data, and fit indices showed good fit. For binge eating, the overall linear increase (b = .44, p < .001) and concave quadratic trend (b = .30, p < .001) fit the data well: RMSEA = 0.05 (confidence interval [CI] = 0.04–0.05), SRMR = 0.04. The linear slope was negatively correlated with the intercept (b = −.22, p < .001), indicating a faster rate of growth for those less likely to be binge eating at Wave 1. For purging, a similar model reflecting a linear increase with a concave quadratic trend fit the data well: RMSEA = 0.06 (CI = 0.05–0.07), SRMR = 0.04. The linear slope was again negatively correlated with the intercept (b = −.24, p < .001), indicating a faster rate of growth for those less likely to be purging at Wave 1. For compensatory exercise, an overall linear decrease (b = −.35, p < .001) and a concave quadratic trend (b = .12, p < .01) fit the data well: RMSEA = 0.04 (CI = 0.04–0.05), SRMR = 0.04. The negative linear slope was again negatively correlated with the intercept (b = −.14, p < .001), indicating those less likely to be engaging in compensatory exercise at Wave 1 declined less over time. For fasting, an overall linear decrease (b = −.38, p < .001) and a concave quadratic trend (b = .19, p < .01) fit the data well: RMSEA = 0.06 (CI = 0.05–0.06), SRMR = 0.04. The negative linear slope was again negatively correlated with the intercept (b = −.22, p < .001), indicating those less likely to be fasting at Wave 1 declined less over time. Chi-square tests revealed that rates of behavior did not differ between genders at any wave; therefore, there was no reason to model growth separately by gender.
Figure 1.
Results of growth curve modeling of each behavior: binge eating (top left), purging (top right), compensatory exercise (bottom left), and fasting (bottom right). N = 1,906.
Second, we tested an SEM autoregression predictive model, as described in the ‘data analysis’ section. This model, specifying all autoregressions and cross-sectional associations, fits well: CFI = 0.93, NNFI = 0.91, RMSEA = 0.03 (CI = 0.02–0.03), SRMR = 0.06; χ2 (432) = 986.82. Table II presents the beta weights for this model, which shows stability of each behavior across waves. We next tested whether autoregressive prediction operated in the same way for boys and girls. The first step in doing so was to test the same autoregression prediction model for both genders: CFI = 0.93; NNFI = 0.90; RMSEA = 0.03 (CI = 0.02–0.03); SRMR = 0.06; χ2 (864) = 1,512.77. We next tested a model in which each predictive path was constrained to be the same for boys and girls (144 paths). There was no drop in model fit with the addition of these constraints, either with respect to fit indices or the chi-square change statistic: CFI = 0.93; NNFI = 0.91; RMSEA = 0.03 (CI = 0.02–0.03); SRMR = 0.07; χ2 (1,008) = 1,647.47). Because specifying equal paths across gender produced no decline in model fit, one concludes that the autoregressive predictive model is invariant across gender.
Table II.
Structural Equation Modeling Results
| Autoregressions | ||
|---|---|---|
| Binge eating | Estimate | |
| Criterion | Predictors | |
| Binge eating Wave 2 | Binge eating Wave 1 | .25 |
| Binge eating Wave 3 | Binge eating Wave 2 | .29 |
| Binge eating Wave 1 | .16 | |
| Binge eating Wave 4 | Binge eating Wave 3 | .23 |
| Binge eating Wave 2 | .13 | |
| Binge eating Wave 5 | Binge eating Wave 4 | .26 |
| Binge eating Wave 6 | Binge eating Wave 5 | .24 |
| Binge eating Wave 4 | .11 | |
| Binge eating Wave 7 | Binge eating Wave 6 | .12 |
| Binge eating Wave 5 | .15 | |
| Binge eating Wave 8 | Binge eating Wave 7 | .21 |
| Binge eating Wave 6 | .14 | |
| Binge eating Wave 9 | Binge eating Wave 8 | .15 |
| Binge eating Wave 7 | .17 | |
| Purging | Estimate | |
| Criterion | Predictors | |
| Purging Wave 2 | Purging Wave 1 | .19 |
| Purging Wave 6 | Purging Wave 5 | .14 |
| Purging Wave 7 | Purging Wave 6 | .08 |
| Purging Wave 8 | Purging Wave 7 | .13 |
| Compensatory exercise |
Estimate | |
|---|---|---|
| Criterion | Predictors | |
| Compensatory exercise Wave 2 | Compensatory exercise Wave 1 | .28 |
| Compensatory exercise Wave 3 | Compensatory exercise Wave 2 | .29 |
| Compensatory exercise Wave 1 | .19 | |
| Compensatory exercise Wave 4 | Compensatory exercise Wave 3 | .24 |
| Compensatory exercise Wave 2 | .16 | |
| Compensatory exercise Wave 1 | .15 | |
| Compensatory exercise Wave 5 | Compensatory exercise Wave 4 | .19 |
| Compensatory exercise Wave 3 | .13 | |
| Compensatory exercise Wave 2 | .10 | |
| Compensatory exercise Wave 1 | .11 | |
| Compensatory exercise Wave 6 | Compensatory exercise Wave 5 | .16 |
| Compensatory exercise Wave 4 | .13 | |
| Compensatory exercise Wave 3 | .06 | |
| Compensatory exercise Wave 2 | .10 | |
| Compensatory exercise Wave 7 | Compensatory exercise Wave 6 | .15 |
| Compensatory exercise Wave 5 | .19 | |
| Compensatory exercise Wave 4 | .11 | |
| Compensatory exercise Wave 8 | Compensatory exercise Wave 7 | .16 |
| Compensatory exercise Wave 6 | .12 | |
| Compensatory exercise Wave 5 | .12 | |
| Compensatory exercise Wave 9 | Compensatory exercise Wave 8 | .24 |
| Compensatory exercise Wave 7 | .11 | |
| Compensatory exercise Wave 6 | .09 | |
| Compensatory exercise Wave 5 | .12 | |
| Fasting | Estimate | |
|---|---|---|
| Criterion | Predictors | |
| Fasting Wave 2 | Fasting Wave 1 | .23 |
| Fasting Wave 3 | Fasting Wave 2 | .25 |
| Fasting Wave 1 | .18 | |
| Fasting Wave 4 | Fasting Wave 3 | .16 |
| Fasting Wave 2 | .12 | |
| Fasting Wave 5 | Fasting Wave 4 | .23 |
| Fasting Wave 6 | Fasting Wave 5 | .27 |
| Fasting Wave 7 | Fasting Wave 6 | .15 |
| Fasting Wave 5 | .12 | |
| Fasting Wave 4 | .12 | |
| Fasting Wave 9 | Fasting Wave 8 | .24 |
Note. N = 1,906. All estimates presented represent significant results (p < .001).
Question 3: Within Gender, Do Eating Disorder Behaviors Covary With Each Other?
Table III presents cross-tabulation tables and chi-square significance tests of the covariation of each behavior with the other three behaviors at Wave 9. As the table shows, the behaviors covaried modestly. Cross-tabulation tables and chi-square significance tests of the covariation of each behavior with the other three behaviors at Waves 1–8 are presented in the online Supplementary Material.
Table III.
Covariation of Binge Eating and Compensatory Behaviors at Wave 9
| Girls (N = 938) | Binge eating |
||
|---|---|---|---|
| Yes (N =127) | No (N = 811) | ||
| Purging* | Yes (N = 28) | 14 | 14 |
| No (N = 910) | 113 | 797 | |
| Compensatory exercise* | Yes (N = 135) | 42 | 93 |
| No (N = 803) | 85 | 718 | |
| Fasting* | Yes (N = 72) | 25 | 47 |
| No (N = 866) | 102 | 764 | |
| Purging | |||
| Yes (N = 28) | No (N = 910) | ||
| Compensatory exercise* | Yes (N = 135) | 15 | 120 |
| No (N = 803) | 13 | 790 | |
| Fasting* | Yes (N = 72) | 16 | 56 |
| No (N = 866) | 12 | 854 | |
| Compensatory exercise | |||
| Yes (N = 135) | No (N = 803) | ||
| Fasting* | Yes (N = 72) | 44 | 28 |
| No (N = 866) | 91 | 775 | |
| Boys (N = 968) |
Binge eating |
||
| Yes (N = 123) | No (N = 845) | ||
| Purging* | Yes (N = 33) | 14 | 19 |
| No (N = 935) | 109 | 826 | |
| Compensatory exercise* | Yes (N = 125) | 30 | 95 |
| No (N = 843) | 93 | 750 | |
| Fasting* | Yes (N = 76) | 31 | 45 |
| No (N = 892) | 92 | 800 | |
| Purging | |||
| Yes (N = 33) | No (N = 935) | ||
| Compensatory exercise* | Yes (N = 125) | 14 | 111 |
| No (N = 847) | 19 | 824 | |
| Fasting* | Yes (N = 76) | 18 | 58 |
| No (N = 892) | 15 | 877 | |
| Compensatory exercise | |||
| Yes (N = 125) | No (N = 843) | ||
| Fasting* | Yes (N = 76) | 41 | 35 |
| No (N = 892) | 84 | 808 | |
Note. Significance level for covariation tests is from Pearson Chi Square analyses.
p < .001.
Question 4: Do Eating Disorder Behaviors Predict Each Other Over Time?
We constructed an SEM model that included all of the paths described above in the autoregression model plus cross-lagged predictions from Wave 1 scores on each variable to scores on the other three variables at each subsequent wave. That is, this model was identical to the autoregression model with the addition of estimated predictive paths from each of the four behaviors to the other three behaviors at each wave, resulting in the estimation of an additional 96 paths. This model fit the data well: CFI = 0.95; NNFI = 0.91; RMSEA = 0.03 (CI = 0.02–0.03); SRMR = 0.05; χ2 (337) = 767.70. To determine whether inclusion of the cross-lagged associations improved model fit, we compared this model with the autoregression model described above. The autoregression model is more restrictive, in that all cross-lagged associations are constrained to 0. It was unclear whether the inclusion of the cross-lagged paths provided meaningful improvement in model fit. The scaled chi-square difference test was significant [χ2(95) = 219.50, p < .001], and the CFI value was slightly higher. However, neither the NNFI nor RMSEA values changed at all between the two models. Further, only one effect emerged in the analyses: Wave 1 fasting predicted Wave 2 compensatory exercise (b = .08, p < .01), and Wave 1 compensatory exercise predicted Wave 2 fasting (b = .12, p < .001). Both compensatory exercise and fasting are symptoms of what has been described as nonpurging compensatory eating disorder (Davis, Holland, & Keel, 2014). Finally, we also tested whether the cross-lagged model was invariant across gender and it was (results not shown).
Discussion
The current study reported on the descriptive characteristics of self-reported eating disorder behavior engagement in girls and boys followed from the Spring of 5th grade into the Spring of 10th grade. We expanded on the results of Combs et al. (2013) in two ways. First, the present research extended the longitudinal period through middle school and the first 2 years of high school. Second, we reported on the occurrence of compensatory exercise and fasting, in addition to binge eating and purging, across the developmental period and at each transition. Our analyses were guided by four questions: (1) What are the rates of self-reported eating disorder behaviors across these years by both girls and boys? (2) Are eating disorder behaviors stable over time? (3) Within gender, do eating disorder behaviors covary with each other? (4) Do eating disorder behaviors predict each other over time?
We first sought to examine the rates of binge eating and compensatory behaviors in girls and boys. Whereas Combs et al. (2013) described mean declines in engagement in binge eating and purging over time from Spring of 5th grade, to Fall of 6th grade, to Spring of 6th grade, we found that trend to be followed by mean increases in both behaviors over the middle and early high school years. In contrast, rates of compensatory exercise and fasting declined over the 5 years of the study. These findings applied to both girls and boys.
Concerning the pattern and stability of eating disorder behaviors over time, we found that binge eating and purging rates both increased linearly during this developmental period. For both behaviors, this trend was modified by a concave quadratic trend, reflecting an initial decrease in the behavior followed by subsequent increases. Rates of both compensatory exercise and fasting declined linearly over time, with both trends modified by a concave quadratic trend, reflecting higher rates of decrease in the early waves compared with the later waves. Boys and girls did not differ on any behavior at any wave.
There is a clear need for model-driven research to explain these patterns of change over time. The current descriptive study provides no explanation for the finding that self-reports of each behavior declined during 5th and 6th grade. Is it the case that, normatively, as children mature in the early adolescent years, they progressively gain more control over their eating and dieting behaviors? Alternatively, is it the case that, despite efforts to clarify all concepts for youth, the youngest children overestimated their rates of engaging in these behaviors?
During the latter part of this longitudinal period, from 7th grade through the first 2 years of high school, rates of binge eating and purging increased and rates of compensatory exercise and fasting decreased. Do rates of binge eating and purging increase because of the increased experience of pressure to meet thin ideals, or increase in expectancies for reinforcement from thinness (Hohlstein, Smith, & Atlas, 1998; Stice & Whitenton, 2002)? Do some youth experiment with compensatory exercise and fasting during early adolescence and mature out of those behaviors or otherwise discard them (Davis et al., 2016a, 2016b)? Perhaps, it is the case that those who continue such behaviors into the high school years are those at greatest risk for developing diagnosable eating disorders (Kotler et al., 2001). Developmentally oriented models of change may prove useful in addressing these questions.
At Wave 9, each of the four behaviors covaried significantly. It seems clearly to be the case that engagement in one behavior increases the likelihood that one is engaging in others as well. At the same time, the covariation is, at best, modest. Because each of the behaviors is associated with dysfunction, it may not be sufficient for health-care professionals to make decisions based only on the presence of diagnosable disorders. Instead, assessment of each behavior independently may be warranted.
Interestingly, despite the covariation among the behaviors measured at the same time, engagement in any one of the behaviors did not predict subsequent increases in any of the other behaviors, beyond prediction from the same behavior measured earlier in time. For example, binge eating behavior at one wave predicted binge eating behavior the next wave, thus indicating some stability in the behaviors, but none of the other behaviors predicted next wave binge eating beyond that autoregression. The same pattern of prediction was observed for boys and girls.
It is important to note the limitations of this study. First, all eating disorder behaviors were self-reported by questionnaire. Although the measures used demonstrated good psychometric properties in this and previous studies of adolescents, face-to-face interviews provide the opportunity for clarification of terms, which may be particularly useful in a sample of youth. Second, children were asked to report engagement in the behaviors over the 2 weeks preceding the assessment. Although this procedure is the recommended one when using the EDE-Q in youth, it may lead to underestimates of engagement in the behaviors. Third, we assessed gender dichotomously and can thus provide no information on youth with fluid or changing gender identities. Fourth, the first seven assessments of this nine-wave study occurred at 6-month time intervals. The final two waves occurred at 12-month intervals and thus represent change over a longer time period.
With these limitations in mind, the current study is the first to report rates of engagement in four eating disorder behaviors during multiple assessment points spanning 5 years from elementary school into high school. Among the striking findings were patterns of increase in binge eating and purging but decrease in compensatory exercise and fasting. Because the behaviors covaried modestly, it may be important to assess the presence of each individually. It was noteworthy that rates of the behaviors did not differ between girls and boys. Gender should not be a basis for deciding to assess for the presence of these behaviors.
Supplementary Data
Supplementary data can be found at: http://www.jpepsy.oxfordjournals.org/.
Funding
This research was supported by a grant from the National Institute on Alcohol Abuse and Alcoholism (NIAAA), R0 AA 016166 awarded to Gregory T. Smith.
Conflicts of interest: None declared.
Supplementary Material
Footnotes
It is difficult to estimate complex growth models (i.e., curves reflecting multiple changes in direction over time) for the kinds of low base-rate behaviors studied here. The estimation procedure could not converge on a solution for any model specifying a cubic trend. Thus, the best-fitting models are presented with the caveat that an even larger sample might have made it possible to detect more complex behavioral trends.
References
- Allen K. L., Byrne S. M., Oddy W. H., Crosby R. D. (2013). DSM–IV–TR and DSM-5 eating disorders in adolescents: Prevalence, stability, and psychosocial correlates in a population-based sample of male and female adolescents. Journal of Abnormal Psychology, 122, 720–732. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-5 (5th ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- Browne M. W., Cudeck R. (1993). Alternative ways of assessing model fit. Sage Focus Editions, 154, 136. [Google Scholar]
- Carter J. C., Stewart D. A., Fairburn C. G. (2001). Eating disorder examination questionnaire: Norms for young adolescent girls. Behaviour Research and Therapy, 39, 625–632. [DOI] [PubMed] [Google Scholar]
- Combs J. L., Pearson C. M., Zapolski T. C. B., Smith G. T. (2013). Preadolescent disordered eating predicts subsequent eating dysfunction. Journal of Pediatric Psychology, 38, 41–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper M. J., Fairburn C. G. (1993). Demographic and clinical correlates of selective information processing in patients with bulimia nervosa. International Journal of Eating Disorders, 13, 109–116. [DOI] [PubMed] [Google Scholar]
- Davis H. A., Guller L., Smith G. T. (2016a). Developmental trajectories of compensatory exercise and fasting behavior across the middle school years. Appetite, 107, 330–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis H. A., Guller L., Smith G. T. (2016b). Developmental trajectories of boys’ driven exercise and fasting during the middle school years. Journal of Abnormal Child Psychology, 44, 1309–1319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis H. A., Holland L. A., Keel P. K. (2014). A preliminary examination of a nonpurging compensatory eating disorder. International Journal of Eating Disorders, 47, 239–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enders C. K. (2006). Analyzing structural equation models with missing data In Hancock G. R., Mueller R. O. (Eds.), A second course in structural equation modeling (pp. 313–342). Greenwich, CT: Information Age. [Google Scholar]
- Fairburn C. G., Beglin S. J. (1994). Assessment of eating disorders: Interview or self-report questionnaire? International Journal of Eating Disorders, 16, 363–370. [PubMed] [Google Scholar]
- Flament M. F., Buchholz A., Henderson K., Obeid N., Maras D., Schubert N., Paterniti S., Goldfield G. (2015). Comparative distribution and validity of DSM‐IV and DSM‐5 diagnoses of eating disorders in adolescents from the community. European Eating Disorders Review, 23, 100–110. [DOI] [PubMed] [Google Scholar]
- Gonsalves D., Hawk H., Goodenow C. (2014). Unhealthy weight control behaviors and related risk factors in Massachusetts middle and high school students. Maternal and Child Health Journal, 18, 1803–1813. [DOI] [PubMed] [Google Scholar]
- Gonzalez A., Kohn M. R., Clarke S. D. (2007). Eating disorders in adolescents. Australian Family Physician, 36, 614–619. [PubMed] [Google Scholar]
- Hohlstein L. A., Smith G. T., Atlas J. G. (1998). An application of expectancy theory to eating disorders: Development and validation of measures of eating and dieting expectancies. Psychological Assessment, 10, 49–58. [Google Scholar]
- Holling H., Kamtsiuris P., Lange M., Thierfelder W., Thamm M., Schlack R. (2007). The German health interview and examination survey for children and adolescents (KiGGS): Study management and conduct of fieldwork. Bundesgesundheitsblatt, Gesundheitsforschung, Gesundheitsschut, 50, 557–566. [DOI] [PubMed] [Google Scholar]
- Hu L. T., Bentler P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6, 1–55. [Google Scholar]
- Hughes E. K., Goldschmidt A. B., Labuschagne Z., Loeb K. L., Sawyer S. M., Le Grange D. L. (2013). Eating disorders with and without comorbid depression and anxiety: Similarities and differences in a clinical sample of children and adolescents. European Eating Disorders Review, 21, 386–394. [DOI] [PubMed] [Google Scholar]
- Kline R. B. (2015). Principles and Practice of Structural Equation Modeling. New York, NY: Guilford Publications. [Google Scholar]
- Kotler L. A., Cohen P., Davies M., Pine D. S., Walsh B. T. (2001). Longitudinal relationships between childhood, adolescent, and adult eating disorders. Journal of the American Academy of Child and Adolescent Psychiatry, 40, 1434–1440. [DOI] [PubMed] [Google Scholar]
- Leon G. R., Fulkerson J. A., Perry C. L., Keel P. K., Klump K. L. (1999). Three to four year prospective evaluation of personality and behavioral risk factors for later disordered eating in adolescent girls and boys. Journal of Youth and Adolescence, 28, 181–196. [Google Scholar]
- Little R. J., Rubin D. B. (1989). The analysis of social science data with missing values. Sociological Methods and Research, 18, 292–326. [Google Scholar]
- Luce K. H., Crowther J. H. (1999). The reliability of the eating disorder examination—Self‐report questionnaire version (EDE‐Q). International Journal of Eating Disorders, 25, 349–351. [DOI] [PubMed] [Google Scholar]
- Luo X., Donnellan M. B., Burt S. A., Klump K. L. (2016). The dimensional nature of eating pathology: Evidence from a direct comparison of categorical, dimensional, and hybrid models. Journal of Abnormal Psychology, 125, 715–726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Micali N., Hagberg K. W., Petersen I., Treasure J. L. (2013). The incidence of eating disorders in the UK in 2000–2009: Findings from the general practice research database. BMJ Open, 3, e002646.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Micali N., Horton N. J., Crosby R. D., Swanson S. A., Sonneville K. R., Solmi F., Calzo J. P., Eddy K. T., Field A. E. (2016). Eating disorder behaviours amongst adolescents: Investigating classification, persistence and prospective associations with adverse outcomes using latent class models. European Child and Adolescent Psychiatry, 26, 231–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Micali N., Ploubidis G., De Stavola B., Simonoff E., Treasure J. (2014). Frequency and patterns of eating disorder symptoms in early adolescence. Journal of Adolescent Health, 54, 574–581. [DOI] [PubMed] [Google Scholar]
- Muthen L. K., Muthen B. O. (2004-2010) Mplus: The comprehensive modeling program for applied researchers. User’s guide (3rd ed.). Los Angeles, CA: Muthen & Muthen. [Google Scholar]
- Mond J., Hall A., Bentley C., Harrison C., Gratwick‐Sarll K., Lewis V. (2014). Eating‐disordered behavior in adolescent boys: Eating disorder examination questionnaire norms. International Journal of Eating Disorders, 47, 335–341. [DOI] [PubMed] [Google Scholar]
- Mond J. M., Hay P. J., Rodgers B., Owen C., Beumont P. J. (2004). Validity of the Eating Disorder Examination Questionnaire (EDE-Q) in screening for eating disorders in community samples. Behaviour Research and Therapy, 42, 551–567. [DOI] [PubMed] [Google Scholar]
- Nagl M., Jacobi C., Paul M., Beesdo-Baum K., Höfler M., Lieb R., Wittchen H. U. (2016). Prevalence, incidence, and natural course of anorexia and bulimia nervosa among adolescents and young adults. European Child & Adolescent Psychiatry, 25, 903–918. [DOI] [PubMed] [Google Scholar]
- Neumark-Sztainer D., Wall M., Larson N. I., Eisenberg M. E., Loth K. (2011). Dieting and disordered eating behaviors from adolescence to young adulthood: Findings from a 10-year longitudinal study. Journal of the American Dietetic Association, 111, 1004–1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicholls D. E., Lynn R., Viner R. M. (2011). Childhood eating disorders: British national surveillance study. The British Journal of Psychiatry, 198, 295–301. [DOI] [PubMed] [Google Scholar]
- Pearson C. M., Zapolski T. C. B., Smith G. T. (2015). A longitudinal test of impulsivity and depression pathways to early binge eating onset. International Journal of Eating Disorders, 48, 230–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pisetsky E. M., May Chao Y., Dierker L. C., May A. M., Striegel-Moore R. H. (2008). Disordered eating and substance use in high‐school students: Results from the Youth Risk Behavior Surveillance System. International Journal of Eating Disorders, 41, 464–470. [DOI] [PubMed] [Google Scholar]
- Rohde P., Stice E., Marti C. N. (2015). Development and predictive effects of eating disorder risk factors during adolescence: Implications for prevention efforts. International Journal of Eating Disorders, 48, 187–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smink F. R., Van Hoeken D., Oldehinkel A. J., Hoek H. W. (2014). Prevalence and severity of DSM-5 eating disorders in a community cohort of adolescents. The International Journal of Eating Disorders, 47, 610–619. [DOI] [PubMed] [Google Scholar]
- Stice E., Marti C. N., Rohde P. (2013). Prevalence, incidence, impairment, and course of the proposed DSM-5 eating disorder diagnoses in an 8-year prospective community study of young women. Journal of Abnormal Psychology, 122, 445–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E., Whitenton K. (2002). Risk factors for body dissatisfaction in adolescent girls: A longitudinal investigation. Developmental Psychology, 38, 669–678. [DOI] [PubMed] [Google Scholar]
- Stiles-Shields E. C., Goldschmidt A. B., Boepple L., Glunz C., Le Grange D. (2011). Driven exercise among treatment-seeking youth with eating disorders. Eating Behaviors, 12, 328–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M. (2008). Binge eating among children and adolescents In Jelalian E., Steele R. (Eds.), Handbook of Child and Adolescent Obesity (pp. 41–57). New York, NY: Springer. [Google Scholar]
- Tanofsky-Kraff M., Faden D., Yanovski S. Z., Wilfley D. E., Yanovski J. A. (2005). The perceived onset of dieting and loss of control eating behaviors in overweight children. International Journal of Eating Disorders, 38, 112–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M., Shomaker L. B., Olsen C., Roza C. A., Wolkoff L. E., Columbo K. M., Raciti G., Zocca J. M., Wilfley D. E., Yanovski S. Z., Yanovski J. A. (2011). A prospective study of pediatric loss of control eating and psychological outcomes. Journal of Abnormal Psychology, 120, 108–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu W., West S. G., Taylor A. B. (2009). Evaluating model fit for growth curve models: Integration of fit indices from SEM and MLM frameworks. Psychological Methods, 14, 183–201. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.