Abstract
Compulsive behaviors (e.g., addiction) can be viewed as an aberrant decision process where inflexible reactions automatically evoked by stimuli (habit) take control over decision making to the detriment of a more flexible (goal-oriented) behavioral learning system. These behaviors are thought to arise from learning algorithms known as “model-based” and “model-free” reinforcement learning. Gambling disorder, a form of addiction without the confound of neurotoxic effects of drugs, showed impaired goal-directed control but the way in which problem gamblers (PG) orchestrate model-based and model-free strategies has not been evaluated. Forty-nine PG and 33 healthy participants (CP) completed a two-step sequential choice task for which model-based and model-free learning have distinct and identifiable trial-by-trial learning signatures. The influence of common psychopathological comorbidities on those two forms of learning were investigated. PG showed impaired model-based learning, particularly after unrewarded outcomes. In addition, PG exhibited faster reaction times than CP following unrewarded decisions. Troubled mood, higher impulsivity (i.e., positive and negative urgency) and current and chronic stress reported via questionnaires did not account for those results. These findings demonstrate specific reinforcement learning and decision-making deficits in behavioral addiction that advances our understanding and may be important dimensions for designing effective interventions.
Subject terms: Human behaviour, Learning algorithms
Introduction
Modern theories of addictive behaviors are built on basic neural and cognitive decision mechanisms, and posit an imbalance between past-oriented habits (e.g., drinking alcohol automatically in a given context) and present and future-oriented goals (e.g., limiting alcohol use), thus resulting in a lack of consideration for the consequences of the actions1–3. Deficits in goal-directed learning and control (e.g., prepotent response inhibition, set-shifting) have been observed across a range of disorders characterized by compulsivity such as addiction4–6 and obsessive-compulsive disorder7,8. The case of gambling disorder (GD) is of particular interest. Recently reclassified alongside substance use disorder9, mainly because those syndromes share clinical (e.g., craving, escalation in use) and neurobiological (e.g., abnormal fronto-striatal network) characteristics10,11, GD offers the opportunity to understand addiction without potentially confounding neurotoxicity associated with acute or chronic use of psychoactive substance12.
For effort and energy saving13,14, adaptive choice behavior relies on optimal orchestration between two forms of instrumental decision systems: the goal-directed system learns about the contingency between actions and outcomes and ensures that behavior is appropriate given our motivational state and/or desire for these outcomes, while the ‘habitual’ system enables actions that has been trained or ‘stamped in’ to the extent that these actions become stimulus- rather than goal-driven15. The way in which those systems interact in healthy and psychopathological conditions have received considerable attention in recent years16–19.
Whether compulsive behaviors are automatically driven by contextual elements without outcome expectations (i.e., habit)20,21 or if they remain mainly goal-oriented22–24 or both25 is still debated26. While animal model studies employing outcome-devaluation techniques find that agents presenting persistent drug use are measurably less sensitive to devaluation27, particularly in those with higher trait impulsivity28, human studies in individuals with substance use disorder (SUD) have yielded mixed results23,29,30.
As an attempt to better characterize those two forms of learning that remain difficult to dissociate experimentally26, habit and goal-directed control has recently been computationally formalized as ‘model-free’ (MF) and ‘model-based’ (MB) reinforcement learning (RL). Crucially MF and MB learning can be disentangled by using sequential decision-making paradigms. Critically, a measure of individuals’ utilization of MB RL (on a sequential decision task, the two-step task) correlates with sensitivity to outcome-devaluation paradigms classically used to probe the balance between goal-directed and habitual control31. In accordance with predictions based on animal studies32, impaired MB RL has been linked to a wide range of compulsive symptoms19,33,34.
Research investigating the relative contribution of MB and MF in clinical populations with substance use disorder (SUD) has provided a less consistent picture. While individuals with alcohol use disorder sometimes showed impaired MB after negative outcome (e.g., a non-rewarded trial)35, other studies find no difference in expression of MB choice between alcoholic and non-alcoholic participants18,33,36. Whereas binge drinkers had impaired goal-directed behavior in a computational two-step sequential decision-making task37, no association of goal-directed or habitual control and alcohol intake was found in young social drinkers38, neither between children of alcoholic father compared to their controls39. However, impaired MB was found in methamphetamine-dependent subjects33. The impact of impaired decision-making on alcohol relapse has been recently clarified in a large sample of detoxified individuals with alcohol dependence36. The risk of relapse during a follow-up period of 48 weeks was magnified in subjects holding high alcohol expectations together with low model-based control. However, reduced model-based control per se was not associated with subsequent relapse.
Critically, the discrepancy between studies in substance dependent individuals suggest that some, but not all substances of abuse have a transient or lasting deleterious impact on the balance between model-free and model-based control. If this was the case, the imbalance between both systems would not necessary be a transdiagnostic marker for compulsive disorders, as previously suggested19,40. One approach to clarify whether the balance between model-free and model-based control serves as a transdiagnostic marker or is instead a consequence of certain drugs intake is to study behavioral, non-substance addiction (e.g., gambling use disorder). Indeed, focusing on active PG therefore allows to directly evaluate addiction’s impact on decision-making, while removing the substance’s neurotoxicity as a confounding factor12. Moreover, beyond the clinical similarities between GD and SUD, shared brain vulnerability markers relevant for the study of the habitual and goal-directed modes of action have been found across gambling and substance-used disorders. For instance, hyperdopaminergic activity was found in the dorsal striatum in gamblers and substance abusers, a region implicated to habit-based responding11 associated with GD symptom severity41.
Although some deficiencies in the executive functioning have been reported in subjects with GD42, the extent to which goal-directed (versus habitual) learning might be impaired in subjects with GD remains unexplored. Thus, finding its justification from clinical and neurobiological data, the present study sought to ascertain whether problem gamblers have impaired MF/MB orchestration on a two-step task43. A previous study35 reported impaired goal-directed strategy specifically after non-rewarded trials in individuals with alcohol addiction. Moreover, reduced loss aversion in GD and alcohol dependence44 suggest that both addictive disorders show reduced sensitivity towards negative outcomes. In GD, this matches well with the clinical phenomenon of loss chasing, where GD patients continue to gamble after severe losses45. To further elucidate these mechanisms, we tested how outcome valence would differentially impact reinforcement learning in GD.
Results
Sample characteristics
Our sample consisted of 82 participants, 33 CP and 49 PG. Our final sample consisted of 78 participants: 45 PG and 33 CP. Table 1 depicts the demographic and clinical variables of PG and CP as well as between-groups comparisons.
Table 1.
Demographic and psychological measures for Problem Gamblers (PG) and Control Participants (CP): mean (SD).
| Variable | PG | CP | Between groups difference |
|---|---|---|---|
| Gender ratio (men/female) | 38/7 | 29/4 | X²(1) = 0.19, p = 0.67 |
| Age | 31.31 (9.11) | 31.27 (7.93) | t(76) = 0.02, p = 0.98 |
| Years of education | 12.73 (2.63) | 12.88 (2.87) | t(76) = 0.23, p = 0.82 |
| OSPAN | 74.42 (10.96) | 79.19 (11.40) | t(76) = 1.97, p = 0.07 |
| CPGI | 14.13 (5.02) | 0 | t(44) = 18.88, p < 0.001*** |
| DSM-V | 6 (1.38) | 0 | t(44) = 29.13, p < 0.001*** |
| Impulsivity (UPPS-P) | 49.58 (9. 5) | 48.12 (6.16) | t(75.02) = 0.82, p = 0.42 |
| Negative Urgency | 10.82 (2.97) | 8.97 (2.14) | U = 453.5, p < 0.01** |
| Positive Urgency | 12.02 (2.18) | 10.45 (2.03) | t(76) = 3.23, p < 0.01** |
| Lack of premeditation | 8.33 (3.05) | 8.61 (2.03) | U = 645.5, p = 0.32 |
| Lack of perseverance | 7.51 (3.19) | 8.33 (2.34) | U = 577, p = 0.09 |
| Sensation seeking | 10.89 (3.13) | 11.76 (2.28) | t(76) = 1.35, p = 0.18 |
| SCL-90-R | 70.13 (47.14) | 40.85 (29.37) | U = 465.5, p < 0.001*** |
| Audit | 9.22 (8.36) | 10.48 (6.1) | U = 600, p = 0.15 |
| Smoker | Non-smoker | 20/25 | 15/18 | X²(1) = 0.01, p = 0.93 |
| FTND | 4.95 (2.61) | 3.47 (2.61) | t(33) = 1.66, p = 0.11 |
| Beck Depression Inventory | 7.44 (5.79) | 4.21 (3.94) | U = 488, p = 0.01** |
| Negative affect | 22.2 (9.3) | 18.3 (5.75) | U = 580.5, p = 0.1 |
| STAI-YA | 37.51 (12.56) | 33.3 (9.11) | U = 611.5, p = 0.19 |
| STAI-YB | 44.98 (12.56) | 39.36 (10.27) | t(76) = 2.05, p < 0.05* |
| SRRS | 289 (183.28) | 222.83 (221.14) | U = 430, p < 0.05* |
| Current stress intensity | 3.46 (2.94) | 2.75 (2.19) | U = 575, p = 0.13 |
Significative differences between groups are displayed in bold. All the tests are performed with a two-tailed Student t-test, Mann-Whitney U or a Chi-square test. Welch correction was applied to Student t-tests when Levene’s test for homogeneity of variances was significant (p < 0.05).
Analyses of choice behavior
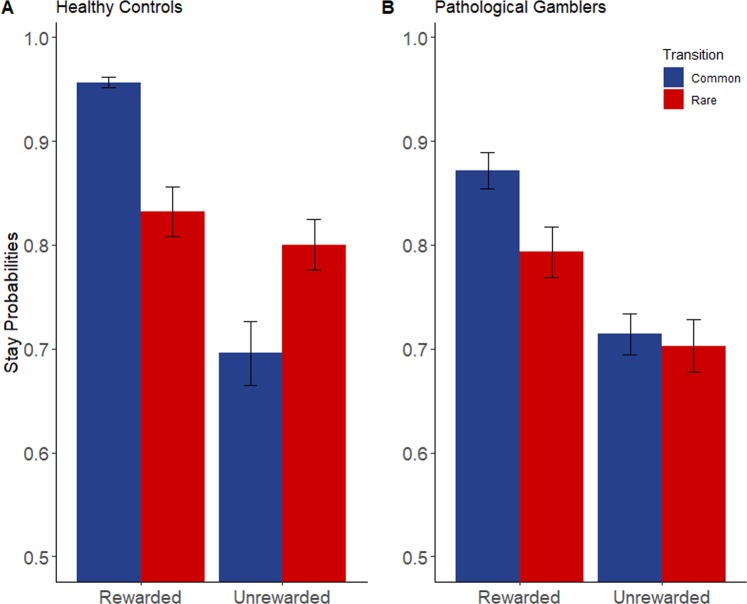
The regression analysis (see Table 2 and Fig. 1) confirmed the basic signatures of MF and MB strategies, expressed as significant effects of both previous outcome (MF learning; β (SE) = 0.55 (0.06), p < 0.001) and the interaction between previous outcome and transition type (MB learning; β (SE) = 0.32 (0.06), p < 0.001). Moreover, the regression revealed that PG and CP did not appear to differ in their MF choice contributions, as evidenced by the absence of a significant two-way group and previous outcome interaction (p = 0.67). Critically, we observed a significant three-way interaction between group (PG versus CP), previous outcome, and previous transition type (β (SE) = −0.12 (0.06), p < 0.05), indicating an attenuated MB learning signature in PG. As the MB strategy is the optimal reward-harvesting strategy in this task, we found that the proportion of rewarded trials differed significantly between the two groups, whereby the CP group was rewarded significantly more often (mean reward rate: 57.31%) than the PG group (mean reward rate: 54.83%) (F(1,78) = 7.23, p < 0.01, ƞ2p = 0.09).
Table 2.
Logistic regression coefficients indicating the influence of previous trial’s outcome, previous trial’s transition, and group on response repetition.
| Coefficient | Estimate (SE) | z value | P value |
|---|---|---|---|
| (Intercept) | 1.67 (0.1) | 16.26 | <0.001*** |
| Group | −0.16 (0.1) | −1.54 | 0.12 |
| Outcome | 0.55 (0.06) | 9.05 | <0.001*** |
| Transition | 0.2 (0.05) | 3.86 | <0.001*** |
| Group * Outcome | −0.02 (0.06) | −0.42 | 0.67 |
| Group * Transition | 0.04 (0.05) | 0.7 | 0.48 |
| Outcome * Transition | 0.32 (0.06) | 5.14 | <0.001*** |
| Group * Outcome * Transition | −0.12 (0.06) | −2 | <0.05** |
Significant results are displayed in bold. *Significance at the 0.05 level; **Significance at the 0.01 level; ***Significance at the 0.001 level.
Figure 1.
Probabilities to maintain the previous first stage choice depending on the transition and the reward during the previous trial among (A) healthy subjects and (B) pathological gamblers. Error bars represent two times the standard error.
Secondly, logistic regressions which separately examined previously rewarded and unrewarded trials (see Table 3) revealed that in both cases, the entire population expressed a basic MB effect (expressed as a main significant effect of transition; rewarded trials (β (SE) = −0.12 (0.05), p < 0.05); unrewarded trials (β (SE) = 0.51 (0.1), p < 0.001)). More importantly, this MB estimate was significantly lowered in PG only after a negative outcome, as shown by a significant negative group * previous transition interaction (β (SE) = 0.16 (0.05), p < 0.01) after a negative outcome but not after a positive outcome (β (SE) = −0.09 (0.1), p = 0.36).
Table 3.
Logistic regression coefficients indicating the influence of previous trial’s transition and group on response repetition depending on the previous trial’s outcome.
| Coefficient | Unrewarded previous trial | Rewarded previous trial | ||||
|---|---|---|---|---|---|---|
| Estimate (SE) | z value | P value | Estimate (SE) | z value | P value | |
| (Intercept) | 1.12 (0.09) | 11.93 | <0.001*** | 2.22 (0.14) | 16.07 | <0.001*** |
| Group | −0.13 (0.09) | −1.41 | 0.16 | −0.18 (0.14) | −1.34 | 0.18 |
| Transition | −0.12 (0.05) | −2.16 | <0.05* | 0.51 (0.1) | 5.32 | <0.001*** |
| Group * Transition | 0.16 (0.05) | 2.95 | <0.01** | −0.09 (0.1) | −0.92 | 0.36 |
Significant results are displayed in bold. * Significance at the 0.05 level; ** Significance at the 0.01 level; *** Significance at the 0.001 level.
Response time (RT) analyses
In the mixed ANOVA comparing the second step’s response time according to the transition between both groups (see Fig. 2), a main significant effect of the transition was found (F(1,76) = 43.72, p<0.001, η2p = 0.37). The participants are slower when the trial’s transition was rare (M = 624.74 ms, SD = 140.61 ms) than common (M = 593.33 ms, SD = 134.15 ms). The interaction between transition type and group also achieved significance (F(1,76) = 4.64, p = 0.03, η2p = 0.06). Post-hoc analyses shows that the RT difference between common and rare transition is significantly higher (t(76) = 2.15, p = 0.03, ds = 0.49) in CP (M = 43.82 ms, SD = 45 ms) than in PG (M = 22.29 ms, SD = 42.61 ms).
Figure 2.
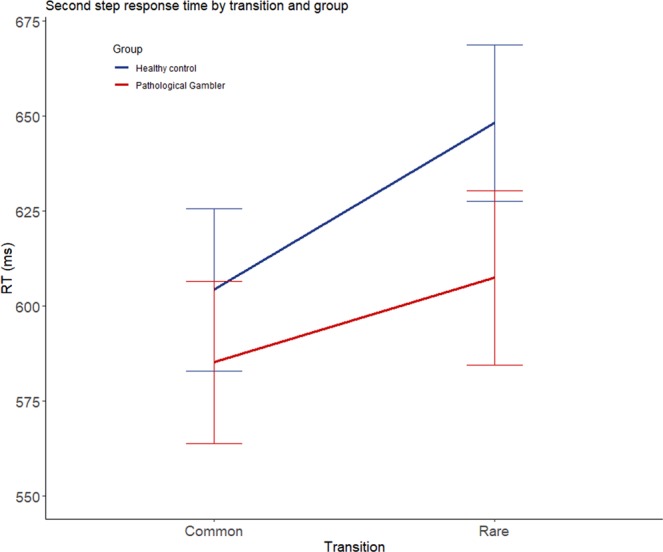
Reaction time in millisecond depending on the transition among both groups. The error bars represent the standard error.
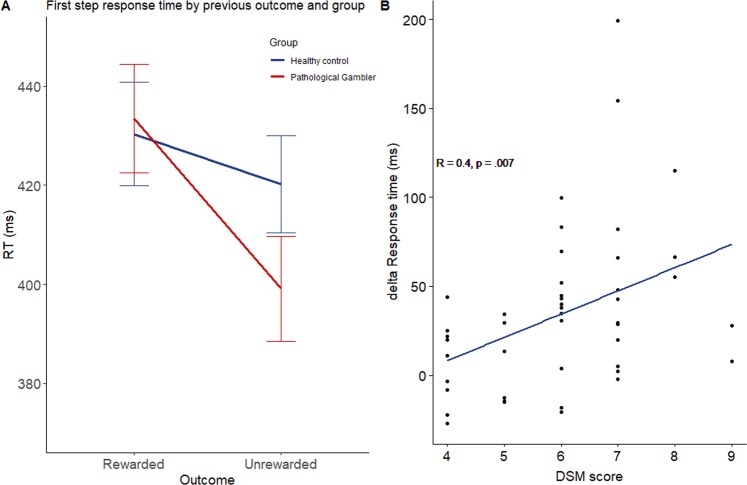
Based on past finding that MB control is associated with slower reaction times than MF46 and because we found that PG had MB deficit after an unrewarded trial, we also examined if the previous losses resulted in faster next trial RTs in PG compared to CP. We used a second mixed ANOVA to analyze the effect of the previous trial’s outcome on the first-choice response time in both groups. A significant main effect of the outcome was found (F(1,76) = 23.3, p < 0.001, η2p = 0.24), indicating that participants were faster to make first-stage choices after an absence of reward (M = 406.23 ms, SD = 84.18) than after a positive outcome (M = 432.14 ms, SD = 93.3). The interaction between outcome and group (F(1,76) = 6.92, p = 0.01, η2p = 0.08) also achieved significance (see Fig. 3A). Post-hoc analyses revealed that PG group made first-stage choices more quickly (t(44) = 5.45, p < 0.001, dz = 0.82) after a negative outcome (M = 396.53 ms, SD = 89.78) than after a positive outcome (M = 433.47 ms, SD = 102.69). This differential pattern of RTs was not observed in the CP group (t(32) = 1.57, p = 0.13). Interestingly, the difference in response time in PG between rewarded and unrewarded trials significantly correlated with the number of symptoms for GD based on the DSM-V47 (r = 0.40, p = 0.004) (see Fig. 3B).
Figure 3.
(A) Reaction time in millisecond depending on the previous trial outcome among both groups. (B) Correlation among PG between gambling severity measured by the DSM score and the response time acceleration after a negative outcome. The error bars represent the standard error.
Clinical analyses
To evaluate the impact of the clinical variables for which there was a difference between PG and CP (i.e., positive and negative urgency, depression, anxiety trait, chronic stress and psychiatric comorbidities) on learning strategies, we ran several logistic regressions with the probability of stay in the previous first step choice as dependent variable and type of outcomes and transition as well as the score at the target clinical questionnaire as independent variables. No significant interaction between any of the clinical variables and either reward type or transition x reward type was found (p > 0.05).
Discussion
The present study aimed at contributing to the understanding of impaired reinforced learning mechanism in behavioral addiction. Based on analysis of choices and reaction times, we found that PG rely less on MB RL prediction while making decision on a two-step task, especially after an unrewarded trial. This finding shed light on potentially important mechanisms involved in inflexible behaviors found in individuals with GD, which are now considered in detail.
Attenuated MB learning signature based on choices was found in PG, with less consideration for transition types, thus leading to fewer rewards. This finding echoes the main idea that impaired MB RL strategy is strongly associated with a symptom dimension comprising compulsive behavior19. Further, our results dovetail well with previous studies employing different choice paradigms (e.g., the Fabulous Fruit Task, a reinforcer devaluation test) that found that individuals with drug addiction rely too much on habits instead of goal-directed choices29.
In support to the idea of impaired MB control in the clinical sample, we found that PG showed less slowing after rare transitions than CP, which likely reflects reduced MB control48,49. Interestingly, the reduction in MB control in PG was particularly important in choices that followed a negative outcome, compared to positive ones. Thus, whereas a negative outcome, in CP signaled the need of additional cognitive control adjustment (MB control) to further avoid these negative outcomes, PG patients failed to recruit these additional control mechanisms. This could occur for a number of possible reasons.
First, the novel finding we provided is that PG is more impulsive than their controls after a non-rewarded trial, as evidenced by faster decisions (expressed as first-stage choice RTs). This phenomenon is in line with previous work reporting that losses (or non-rewarded actions) affect choice by favoring impulsive actions in healthy participants on gambling tasks50,51. Our study suggests that impulsive decisions enhances reliance on habits at the detriment of model-based control, possibly due the lack of inhibition of the habit system in the context of frustration. Second, PG could be less sensitive to extinction, a phenomenon characterizing habit formation that can be due to reduced loss aversion15, hypersensitivity to rewards, incorrect identification of statistically unlikely sequence of wins as a separate situation from more-commonly experienced losses52,53. In line with observed deficits of extinction learning in PG, recent studies suggest that GD could arise from an inflexible association between an action and its reward, even if its outcome is devaluated52–54.
Finally, although the illusion of control and uncontrolled cue-dependent relapse are common psychological explanations for behaviours observed in gambling addiction, the nature of the choice paradigm here yields that data too limited to address these possible explanations. Indeed, we failed to find a higher probability in PG than their controls to repeat the previous first step choice after an unrewarded trial, independently of the transition type. Together, those findings support a specific MB deficit in the context of reward expectancies violation, a phenomenon putatively associated with a hyperdopaminergic state41 that interferes with inhibition of basal ganglia for which D2 receptors are critical55,56. Clearly, additional work is necessary to draw more robust conclusions on neurocognitive determinants of post unrewarded actions that the present work merely suggested. In addition, we found no association between any clinical variables discriminating groups (chronic stress, state and trait anxiety, depression, negative and positive urgency) and the MB signature. This finding indicates that co-occurrence between PG and other psychopathological conditions is not the main reason why PG have goal-directed deficits.
Our findings hold some useful clinical implications. Interestingly, modest clinical outcome (e.g., low remission rate) in the treatment of gambling disorder57 could be due to the lack of consideration for the contribution of rudimentary stimulus-response associations to the addictive behavior, in favor of the idea that addiction mainly results from reinforced goal-directed actions (see the self-medication hypothesis)24. Because MB RL and cognitive control both involve overcoming habitual, stimulus-driven actions58, interventions aimed to improve executive functioning may positively impact on MB contribution. Specifically, electric stimulation (i.e., TDCS) of the dorsolateral prefrontal cortex has been shown to impact a variety of deliberative functions including risk-taking59, working memory60 and classification learning61. Stimulation on the left ventrolateral prefrontal cortex was shown to improve MB control and weight in the decisional balance62, but see for negative results63. Following this recent effort, further research is needed to test the influence of neurocognitive interventions on MB/MF RL in gambling disorder. In the same way, future studies may examine the usefulness of pharmacological intervention (e.g., amisulpride) blocking D2/D3 receptors to augment the relative contribution of MB learning strategy after a negative outcome. This should be done with careful considerations for other cognitive functions involved in dopamine modulation such as risk taking64 and incentive value65.
It is worth noting the potential limitations of this study. First, it is possible that the PG group’s behavior is in part attributable to inaccurate expectancies about future events (e.g., the gambling fallacy or hot hand fallacy)66. Put differently, inappropriate internal model of the environment’s transition structure could have been responsible for lack of consideration for transitions’ rarity, potentially contributing to both the RT and choice effects. False beliefs about probabilities (e.g., consecutive losses necessary lead to a larger monetary gain or several wins in a row increase the probability of winning later) might lead to suboptimal, yet goal-directed, strategies and, without fully probing participants’ beliefs that takes place during the realization of the task26,67, this explanation could not be entirely dismissed. It is therefore possible that decisions considered as habit-like actually result from goal-directed strategies. However, we failed to observe a “hot hand” effect (i.e., the expectation to win after a win) that would have caused faster choice RTs after rewarded trials in PG, in comparison to non-gamblers. Besides, gambling fallacy is more likely after longer runs of losses or wins68.
Another potential limitation is that the two-step task does not incentivize participants to use MB control, but instead decouples winnings from the subjects’ choice strategy so as to avoid these variables potentially confounding one another. Interestingly, a recent study reported that MB control can be reliably improved with the provision of larger incentives (e.g., higher stakes) in individuals with several psychiatric conditions69. The observed boosting model-based control with larger incentive has been thought to result from on a cost-benefit analysis, that is, higher potential payoffs justify the more effortful decision-making processes (i.e., more model-based control)58,69,70. It is worth testing whether the PG deficit in MB RL can be ameliorated in this manner, since a higher sensation seeking trait was both a prominent feature in this population71 and a factor associated with greater boosts in MB control in non-clinical participants (83). However, it should be noted that we offered to participants 30 euros plus 10 euros depending on their net performance, which can be considered as very incentive compared to other similar studies.
Finally, the influence of impaired MB learning in the pathogenesis of gambling addiction remains largely unknown. Unlike drug-taking behaviors that may cause profound disruption in learning systems11, gambling behaviors offer room to study addiction without the confounding effects of neurotoxicity associated with acute and chronic use of chemical substances10. Clearly, in the absence of longitudinal research design, this question cannot be firmly decided. However, a recent preclinical study suggested that individual differences in model-free learning prior to drug use predicted methamphetamine self-administration72.
To summarize, we found deficits in learning and decision making in problem gamblers. It is characterized by a reduced MB action control after a negative outcome. This knowledge has highlighted the importance of decision deficits not directly attributable to the neurotoxic effects of chronic drug use.
Methods
Participants
Forty-nine individuals with gambling disorder, named problem gamblers (PG), who took part in games involving little skill (i.e., slot machines, video poker, dice and pull tabs), and 33 controls (CP) matched for age and educational level were recruited. All participants were recruited through advertisement and gave written informed consent to be part of the experiment. The experiment was approved by the C.H.U. Brugmann Ethics Committee (n° OM 026) and was performed according to the Declaration of Helsinki.
All participants underwent a semi-structured interview73. All PG met the DSM-V criteria47 for gambling disorder (range: 3–9) and had a minimum of 8 on the Canadian Problem Gambling Index (CPGI)74 (range: 8–27). All PG were active gamblers, and none followed a therapy or treatment. Healthy control subjects had a score of 0 on the CPGI. The exclusion criteria for all participants were the presence of psychotic or neurologic syndromes, antecedents of substance addiction and recent utilization of psychopharmacological substances susceptible to alter cognitive functioning.
The participants’ remuneration was set on 30€ and they were told that they could win up to 10€ more depending on their net performance in the two-step decision task (RL task).
Questionnaires, experimental tasks and procedure
At the end of the experiment, each participant performed the operation span (OSPAN) task75 and filled out clinical questionnaires to estimate substance use, psychological problems and symptoms of psychopathology, current negative emotions, anxiety, depression, stress, impulsivity, craving for gambling. Alcohol use was estimated by the Alcohol Use Disorders Identification Test76,77 and nicotine dependence severity by the Fagerström Test for Nicotine Dependence78. The psychopathological symptoms were investigated using the total score of the Symptom Checklist-90-Revised (SCL-90-R)79. Negative emotions, as well as depression and anxiety, were evaluated by the negative scale of the Positive and Negative Affect Schedule80, the short version of the Beck Depression Inventory (BDI)81 and the State-Trait Anxiety Inventory (STAI-YA and STAI-YB)82, respectively. To measure chronic and current stress, the Social Readjustment Scale (SRRS)83 and visual analogue scales (range: 0–10) were administered. Several facets of impulsivity (i.e., negative urgency, positive urgency, lack of premeditation, lack of perseverance and sensation seeking) were evaluated with the short version of the UPPS Impulsive Behavior Scale84.
The entirety of the experimental procedure lasted between 1h30 and 2 h and took place individually with two experimented and well-trained neuropsychologists in a quiet room. Upon their arrival, the participants signed an informed consent and filled out a questionnaire about gambling behaviors (CPGI). Prior the RL task, two visual analogic scales (VAS) (i.e., ‘how much do you want to gamble right now?’ and ‘how much do you feel stressed right now?’) were administered. Right after the task, a second series of VAS were given, followed by the remaining clinical questionnaires.
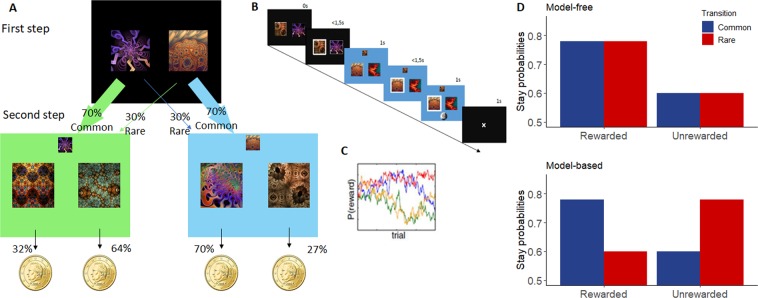
Two-step decision-making task
Participants performed 200 trials of two-step decision-making task43. This task was divided into two stages (see Fig. 4A). At the beginning of the first step, two fractal images were presented on a black screen, between which the participant had to choose. Each first-stage image led commonly (70%) to one of the two second-stages states and rarely to the other (30%). During the second stage, two images were presented on a green or a blue screen (representing the second-stage ‘state’), between which the participant had to choose. Each image led probabilistically to a reward or not, presented with a visual feedback representing a 10c coins or a 0 during the 1-second feedback interval. In order to assure continual learning and exploration during the task, each second-step image’s probability to reward money slowly varied during the task according to Gaussian random walks (SD = 0.025). They had 3 second to perform each choice and the inter-stage and inter-trial intervals both lasted 1 second.
Figure 4.
(A) Two-step decision task (adapted from Otto et al.85). (First step) Participants must choose between the two images, leading preferentially to a green or a blue screen, according to fixed probabilities. (Second step) Subject choose between the two images linked to probabilities to win money. Those probabilities slowly change with the time and vary according to the screen color. (B) Trial’s design. (C) Second step’s changes in probability of reward. (D) Theoretical decision pattern according to a pure MF strategy or to a pure MB strategy.
Prior to the task, participants were given extensive instructions about the task’s structure19. They were instructed that the first choice would preferentially lead towards a blue or a green screen, each one associated with different probabilities of winning, and that their choice at the second screen would depend on their choice on the first screen. It was stressed that transition probabilities between the first and the second stage would be constant while the probabilities of winning at the second stage could vary over time. Participants then completed a tutorial and had to provide correct responses to a quiz including three questions about the task’s structure19. In case of incorrect response to any of them, the explanation phase took place again. They sat in front of a laptop with an AZERTY keyboard. The letter ‘E’ was assigned to the left image and the letter ‘I’ to the right image.
Several measures were considered: The outcome of each second-stage choice (reward or not), transition type (common or rare), the response times to rewarded or unsuccessful trials on frequent or rare transitions, and the probabilities of making two consecutive identical first-stage choices according to the type of transition and reward (termed p(stay)). A pure model-free strategy predicts purely reinforcement-guided choices: a repetition of the previous trial’s first-stage choice only when it was previously rewarded, and a shift occurring after a previous trial being not rewarded. A pure MB strategy takes the task structure and transition type into consideration and predicts a repetition of the previous trial’s first step only if it was rewarded and following a common transition or if it was not rewarded after a rare transition (see Fig. 4D).
Data analyses
All analyses were performed using IBM SPSS Statistics v25 and RStudio Version 1.1.456. To ensure that participants’ data reflected a sufficient level of engagement to the task, in the same way as a previous study85, those who repeated previously rewarded second-step responses at a rate less than 50%, those who did not answer before the deadline more than 20 times, and those who did not try every image in each stage were removed from the data analyses. This resulted in the removement of 4 subjects. Groups were compared on each clinical variable (e.g., depression, anxiety, impulsivity, stress) by using t-tests or non-parametric tests, where appropriate.
A mixed logistic regression was carried out to analyze the influence of group (PG, CP), of previous transition type (common, rare) and of previous outcome (reward, no reward) on the probability to maintain a previous trial first step choice (stay, switch). As MB and MF learning predicting distinct patterns of first-stage repetitions to the previous trial’s events (reward and transition type), this analysis allowed for a quantitative evaluation of their contribution to the trial-by-trial learning. A pure MF strategy rends the first stage choice only impacted by the previous trial’s outcome, independently of the previous trial’s transition type, thus predicting only a main effect of the outcome. On the other hand, a pure MB strategy predicts an interaction between the outcome and the transition type85. Secondly, in order to test our hypothesis that PG had a more pronounced MB impairment after unrewarded trials, we performed two more logistic regressions, separately examining trials following a reward and trials following the absence of reward.
To assess further decision strategies based on reaction times, a mixed ANOVA with the current trial’s transition type (rare, common) as within-factor in PG and CP as between-factor was performed on the second stage response time. Indeed, the difference between second-stage RTs after common versus rare transitions reflects the level of involvement of MB control48,49.
To examine the influence of clinical status other than gambling disorder on decisional strategy on the two-step task, each clinical variable that discriminate the two groups was added separately to the mixed logistic regression.
Acknowledgements
Xavier Noël is a Research Associate at the Belgium Fund for Scientific Research. We express our gratitude to Eloïse Ligot and Charlotte Jacomet for their assistance in recruiting participants. This work was funded by the Belgium Fund for Scientific Research (PDR T.0146.18) and the Brugmann Fundation.
Author contributions
F.W. and X.N. made substantial contributions to the conception and the design of the work. F.W., R.O., M.Se. and N.D. made substantial contributions to the analysis and interpretation of the data. R.O. and N.D. helped in the creation of a new software used in the work, R.O., M.Se., N.D., A.B., M.Sa., C.K., A.C. and N.J. have substantively revised the work. M.Sa. substantively helped with the data acquisition.
Data availability
All data will be made available on the following lab website: http://psymed.ulb.be/.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bechara A. Decision making, impulse control and loss of willpower to resist drugs: a neurocognitive perspective. Nat. Neurosci. 2005;8:1458–1463. doi: 10.1038/nn1584. [DOI] [PubMed] [Google Scholar]
- 2.Everitt BJ, Robbins TW. Neural systems of reinforcement for drug addiction: from actions to habits to compulsion. Nat. Neurosci. 2005;8:1481–1489. doi: 10.1038/nn1579. [DOI] [PubMed] [Google Scholar]
- 3.Noël X, Brevers D, Bechara A. A neurocognitive approach to understanding the neurobiology of addiction. Curr. Opin. Neurobiol. 2013;23:632–638. doi: 10.1016/j.conb.2013.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Robinson TE, Berridge KC. The incentive sensitization theory of addiction: some current issues. Philos. Trans. R. Soc. B Biol. Sci. 2008;363:3137–3146. doi: 10.1098/rstb.2008.0093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zilverstand A, Huang AS, Alia-Klein N, Goldstein RZ. Neuroimaging Impaired Response Inhibition and Salience Attribution in Human Drug Addiction: A Systematic Review. Neuron. 2018;98:886–903. doi: 10.1016/j.neuron.2018.03.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee RSC, Hoppenbrouwers S, Franken I. A Systematic Meta-Review of Impulsivity and Compulsivity in Addictive Behaviors. Neuropsychol. Rev. 2019;29:14–26. doi: 10.1007/s11065-019-09402-x. [DOI] [PubMed] [Google Scholar]
- 7.Abramovitch A, Abramowitz JS, Mittelman A. The neuropsychology of adult obsessive–compulsive disorder: A meta-analysis. Clin. Psychol. Rev. 2013;33:1163–1171. doi: 10.1016/j.cpr.2013.09.004. [DOI] [PubMed] [Google Scholar]
- 8.Robbins TW, Vaghi MM, Banca P. Obsessive-Compulsive Disorder: Puzzles and Prospects. Neuron. 2019;102:27–47. doi: 10.1016/j.neuron.2019.01.046. [DOI] [PubMed] [Google Scholar]
- 9.Reilly, C. & Smith, N. The evolving definition of pathological gambling in the DSM-5. Washington, Beverly (National Center for responsible gambling (2013).
- 10.Leeman RF, Potenza MN. Similarities and differences between pathological gambling and substance use disorders: a focus on impulsivity and compulsivity. Psychopharmacology. 2012;219:469–490. doi: 10.1007/s00213-011-2550-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clark L, Boileau I, Zack M. Neuroimaging of reward mechanisms in Gambling disorder: an integrative review. Mol. Psychiatry. 2019;24:674–693. doi: 10.1038/s41380-018-0230-2. [DOI] [PubMed] [Google Scholar]
- 12.Verdejo-García A, Lawrence AJ, Clark L. Impulsivity as a vulnerability marker for substance-use disorders: review of findings from high-risk research, problem gamblers and genetic association studies. Neurosci. Biobehav. Rev. 2008;32:777–810. doi: 10.1016/j.neubiorev.2007.11.003. [DOI] [PubMed] [Google Scholar]
- 13.Balleine BW, O’Doherty JP. Human and rodent homologies in action control: corticostriatal determinants of goal-directed and habitual action. Neuropsychopharmacoly. 2010;35:48–69. doi: 10.1038/npp.2009.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Keramati M, Dezfouli A, Piray P. Speed/accuracy trade-off between the habitual and the goal-directed processes. PLoS Comput. Biol. 2011;7:e1002055. doi: 10.1371/journal.pcbi.1002055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dickinson A. Actions and Habits: The Development of Behavioural Autonomy. Philos. Trans. R. Soc. Lond. B. Biol. Sci. 1985;308:67–78. doi: 10.1098/rstb.1985.0010. [DOI] [Google Scholar]
- 16.Daw ND, Niv Y, Dayan P. Uncertainty-based competition between prefrontal and dorsolateral striatal systems for behavioral control. Nat. Neurosci. 2005;8:1704–1711. doi: 10.1038/nn1560. [DOI] [PubMed] [Google Scholar]
- 17.Dolan RJ, Dayan P. Goals and habits in the brain. Neuron. 2013;80:312–325. doi: 10.1016/j.neuron.2013.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Voon V, Reiter A, Sebold M, Groman S. Model-Based Control in Dimensional Psychiatry. Biol. Psychiatry. 2017;82:391–400. doi: 10.1016/j.biopsych.2017.04.006. [DOI] [PubMed] [Google Scholar]
- 19.Gillan, C. M., Kosinski, M., Whelan, R., Phelps, E. A. & Daw, N. D. Characterizing a psychiatric symptom dimension related to deficits in goal-directed control. eLife5 (2016). [DOI] [PMC free article] [PubMed]
- 20.Robbins TW, Everitt BJ. Drug addiction: bad habits add up. Nature. 1999;398:567–570. doi: 10.1038/19208. [DOI] [PubMed] [Google Scholar]
- 21.Everitt BJ, Robbins TW. Drug Addiction: Updating Actions to Habits to Compulsions Ten Years On. Annu. Rev. Psychol. 2016;67:23–50. doi: 10.1146/annurev-psych-122414-033457. [DOI] [PubMed] [Google Scholar]
- 22.Becker GS, Murphy KM. A Theory of Rational Addiction. J. Polit. Econ. 1988;96:675–700. doi: 10.1086/261558. [DOI] [Google Scholar]
- 23.Hogarth, L. A Critical Review of Habit Theory of Drug Dependence. In The Psychology of Habit (ed. Verplanken, B.) 325–341 (Springer International Publishing, 2018).
- 24.Khantzian EJ. The self-medication hypothesis of addictive disorders: focus on heroin and cocaine dependence. Am. J. Psychiatry. 1985;142:1259–1264. doi: 10.1176/ajp.142.11.1259. [DOI] [PubMed] [Google Scholar]
- 25.Furlong, T. M. & Corbit, L. H. Chapter 16 - Drug Addiction: Augmented Habit Learning or Failure of Goal-Directed Control? in Goal-Directed Decision Making (eds. Morris, R., Bornstein, A. & Shenhav, A.) 367–386 (Academic Press, 2018).
- 26.De Houwer J, Tanaka A, Moors A, Tibboel H. Kicking the habit: Why evidence for habits in humans might be overestimated. Motiv. Sci. 2018;4:50–59. doi: 10.1037/mot0000065. [DOI] [Google Scholar]
- 27.Dickinson A, Wood N, Smith JW. Alcohol Seeking by Rats: Action or Habit? Q. J. Exp. Psychol. Sect. B. 2002;55:331–348. doi: 10.1080/0272499024400016. [DOI] [PubMed] [Google Scholar]
- 28.Belin D, Mar AC, Dalley JW, Robbins TW, Everitt BJ. High impulsivity predicts the switch to compulsive cocaine-taking. Science. 2008;320:1352–1355. doi: 10.1126/science.1158136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sjoerds Z, et al. Behavioral and neuroimaging evidence for overreliance on habit learning in alcohol-dependent patients. Transl. Psychiatry. 2013;3:e337–e337. doi: 10.1038/tp.2013.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ersche KD, et al. Carrots and sticks fail to change behavior in cocaine addiction. Science. 2016;352:1468–1471. doi: 10.1126/science.aaf3700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gillan CM, et al. Functional Neuroimaging of Avoidance Habits in Obsessive-Compulsive Disorder. Am. J. Psychiatry. 2015;172:284–293. doi: 10.1176/appi.ajp.2014.14040525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lucantonio, F., Caprioli, D. & Schoenbaum, G. Transition from ‘model-based’ to ‘model-free’ behavioral control in addiction: involvement of the orbitofrontal cortex and dorsolateral striatum. Neuropharmacology76 (2014). [DOI] [PMC free article] [PubMed]
- 33.Voon V, et al. Disorders of compulsivity: a common bias towards learning habits. Mol. Psychiatry. 2015;20:345–352. doi: 10.1038/mp.2014.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Culbreth AJ, Westbrook A, Daw ND, Botvinick M, Barch DM. Reduced Model-Based Decision-Making in Schizophrenia. J. Abnorm. Psychol. 2016;125:777–787. doi: 10.1037/abn0000164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sebold M, et al. Model-Based and Model-Free Decisions in Alcohol Dependence. Neuropsychobiology. 2014;70:122–131. doi: 10.1159/000362840. [DOI] [PubMed] [Google Scholar]
- 36.Sebold M, et al. When Habits Are Dangerous: Alcohol Expectancies and Habitual Decision Making Predict Relapse in Alcohol Dependence. Biol. Psychiatry. 2017;82:847–856. doi: 10.1016/j.biopsych.2017.04.019. [DOI] [PubMed] [Google Scholar]
- 37.Doñamayor N, Strelchuk D, Baek K, Banca P, Voon V. The involuntary nature of binge drinking: goal directedness and awareness of intention: Automaticity of binge drinking. Addict. Biol. 2018;23:515–526. doi: 10.1111/adb.12505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nebe S, et al. No association of goal-directed and habitual control with alcohol consumption in young adults: Alcohol use and learning. Addict. Biol. 2018;23:379–393. doi: 10.1111/adb.12490. [DOI] [PubMed] [Google Scholar]
- 39.Reiter, A. M. F., Deserno, L., Wilbertz, T., Heinze, H.-J. & Schlagenhauf, F. Risk Factors for Addiction and Their Association with Model-Based Behavioral Control. Front. Behav. Neurosci. 10 (2016). [DOI] [PMC free article] [PubMed]
- 40.Gillan, C. M. et al. Comparison of the Association Between Goal-Directed Planning and Self-reported Compulsivity vs Obsessive-Compulsive Disorder Diagnosis. JAMA Psychiatry 1–10 (2019). [DOI] [PMC free article] [PubMed]
- 41.Boileau I, et al. In vivo evidence for greater amphetamine-induced dopamine release in pathological gambling: a positron emission tomography study with [11C]-(+)-PHNO. Mol. Psychiatry. 2014;19:1305–1313. doi: 10.1038/mp.2013.163. [DOI] [PubMed] [Google Scholar]
- 42.Lawrence AJ, Luty J, Bogdan NA, Sahakian BJ, Clark L. Impulsivity and response inhibition in alcohol dependence and problem gambling. Psychopharmacology. 2009;207:163–172. doi: 10.1007/s00213-009-1645-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Daw ND, Gershman SJ, Seymour B, Dayan P, Dolan RJ. Model-Based Influences on Humans’ Choices and Striatal Prediction Errors. Neuron. 2011;69:1204–1215. doi: 10.1016/j.neuron.2011.02.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Genauck A. Reduced loss aversion in pathological gambling and alcohol dependence is associated with differential alterations in amygdala and prefrontal functioning. Sci. Rep. 2017;7:11. doi: 10.1038/s41598-017-16433-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lesieur, H. R. The Chase: Career of the Compulsive Gambler (Schenkman Books Inc., 1984).
- 46.Otto AR, Gershman SJ, Markman AB, Daw ND. The curse of planning: dissecting multiple reinforcement-learning systems by taxing the central executive. Psychol. Sci. 2013;24:751–761. doi: 10.1177/0956797612463080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.American Psychiatric Association. American Psychiatric Association. & DSM-5 Task Force. Diagnostic and statistical manual of mental disorders: DSM-5 (2013).
- 48.Deserno L, et al. Ventral striatal dopamine reflects behavioral and neural signatures of model-based control during sequential decision making. Proc. Natl. Acad. Sci. USA. 2015;112:1595–1600. doi: 10.1073/pnas.1417219112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sebold M, et al. Don’t Think, Just Feel the Music: Individuals with Strong Pavlovian-to-Instrumental Transfer Effects Rely Less on Model-based Reinforcement Learning. J. Cogn. Neurosci. 2016;28:985–995. doi: 10.1162/jocn_a_00945. [DOI] [PubMed] [Google Scholar]
- 50.Delabbro PH, Winefield AH. Poker-machine gambling: An analysis of within session characteristics. Br. J. Psychol. 1999;90:425–439. doi: 10.1348/000712699161503. [DOI] [Google Scholar]
- 51.Verbruggen F, Chambers CD, Lawrence NS, McLaren IPL. Winning and losing: Effects on impulsive action. J. Exp. Psychol. Hum. Percept. Perform. 2017;43:147–168. doi: 10.1037/xhp0000284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Redish AD, Jensen S, Johnson A. A unified framework for addiction: Vulnerabilities in the decision process. Behav. Brain Sci. 2008;31:415–487. doi: 10.1017/S0140525X0800472X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Redish AD, Jensen S, Johnson A, Kurth-Nelson Z. Reconciling reinforcement learning models with behavioral extinction and renewal: Implications for addiction, relapse, and problem gambling. Psychol. Rev. 2007;114:784–805. doi: 10.1037/0033-295X.114.3.784. [DOI] [PubMed] [Google Scholar]
- 54.de Ruiter MB, et al. Response Perseveration and Ventral Prefrontal Sensitivity to Reward and Punishment in Male Problem Gamblers and Smokers. Neuropsychopharmacology. 2009;34:1027–1038. doi: 10.1038/npp.2008.175. [DOI] [PubMed] [Google Scholar]
- 55.Frank MJ, Seeberger LC, O’reilly RC. By carrot or by stick: cognitive reinforcement learning in parkinsonism. Science. 2004;306:1940–1943. doi: 10.1126/science.1102941. [DOI] [PubMed] [Google Scholar]
- 56.Maia TV, Frank MJ. From reinforcement learning models to psychiatric and neurological disorders. Nat. Neurosci. 2011;14:154–162. doi: 10.1038/nn.2723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Petry NM. Discounting of probabilistic rewards is associated with gambling abstinence in treatment-seeking pathological gamblers. J. Abnorm. Psychol. 2012;121:151–159. doi: 10.1037/a0024782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Patzelt EH, Kool W, Millner AJ, Gershman SJ. Incentives Boost Model-Based Control Across a Range of Severity on Several Psychiatric Constructs. Biol. Psychiatry. 2019;85:425–433. doi: 10.1016/j.biopsych.2018.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Fecteau S, et al. Diminishing Risk-Taking Behavior by Modulating Activity in the Prefrontal Cortex: A Direct Current Stimulation Study. J. Neurosci. 2007;27:12500–12505. doi: 10.1523/JNEUROSCI.3283-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Fregni F, et al. Anodal transcranial direct current stimulation of prefrontal cortex enhances working memory. Exp. Brain Res. 2005;166:23–30. doi: 10.1007/s00221-005-2334-6. [DOI] [PubMed] [Google Scholar]
- 61.Kincses TZ, Antal A, Nitsche MA, Bártfai O, Paulus W. Facilitation of probabilistic classification learning by transcranial direct current stimulation of the prefrontal cortex in the human. Neuropsychologia. 2004;42:113–117. doi: 10.1016/S0028-3932(03)00124-6. [DOI] [PubMed] [Google Scholar]
- 62.Weissengruber, S., Lee, S. W., O’Doherty, J. P. & Ruff, C. C. Neurostimulation Reveals Context-Dependent Arbitration Between Model-Based and Model-Free Reinforcement Learning. Cereb. Cortex, 1–13 (2019). [DOI] [PubMed]
- 63.Smittenaar P, FitzGerald THB, Romei V, Wright ND, Dolan RJ. Disruption of Dorsolateral Prefrontal Cortex Decreases Model-Based in Favor of Model-free Control in Humans. Neuron. 2013;80:914–919. doi: 10.1016/j.neuron.2013.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.St Onge JR, Floresco SB. Dopaminergic modulation of risk-based decision making. Neuropsychopharmacoly. 2009;34:681–697. doi: 10.1038/npp.2008.121. [DOI] [PubMed] [Google Scholar]
- 65.Berridge KC. The debate over dopamine’s role in reward: the case for incentive salience. Psychopharmacology. 2007;191:391–431. doi: 10.1007/s00213-006-0578-x. [DOI] [PubMed] [Google Scholar]
- 66.Joukhador J, Blaszczynski A, Maccallum F. Superstitious Beliefs in Gambling Among Problem and Non-Problem Gamblers: Preliminary Data. J. Gambl. Stud. 2004;20:171–180. doi: 10.1023/B:JOGS.0000022308.27774.2b. [DOI] [PubMed] [Google Scholar]
- 67.Clark L, et al. Pathological Choice: The Neuroscience of Gambling and Gambling Addiction. J. Neurosci. 2013;33:17617–17623. doi: 10.1523/JNEUROSCI.3231-13.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ayton P, Fischer I. The hot hand fallacy and the gambler’s fallacy: Two faces of subjective randomness? Mem. Cognit. 2004;32:1369–1378. doi: 10.3758/BF03206327. [DOI] [PubMed] [Google Scholar]
- 69.Kool, W., Cushman, F. A. & Gershman, S. J. Competition and Cooperation Between Multiple Reinforcement Learning Systems. in Goal-Directed Decision Making 153–178 (Elsevier, 2018).
- 70.Boureau Y-L, Sokol-Hessner P, Daw ND. Deciding How To Decide: Self-Control and Meta-Decision Making. Trends Cogn. Sci. 2015;19:700–710. doi: 10.1016/j.tics.2015.08.013. [DOI] [PubMed] [Google Scholar]
- 71.Coventry KR, Brown RI. Sensation seeking, gambling and gambling addictions. Addiction. 1993;88:541–554. doi: 10.1111/j.1360-0443.1993.tb02061.x. [DOI] [PubMed] [Google Scholar]
- 72.Groman SM, Massi B, Mathias SR, Lee D, Taylor JR. Model-Free and Model-Based Influences in Addiction-Related Behaviors. Biol. Psychiatry. 2019;11:936–945. doi: 10.1016/j.biopsych.2018.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Nurnberger JI, et al. Diagnostic interview for genetic studies. Rationale, unique features, and training. NIMH Genetics Initiative. Arch. Gen. Psychiatry. 1994;51:849–859. doi: 10.1001/archpsyc.1994.03950110009002. [DOI] [PubMed] [Google Scholar]
- 74.Ferris, J. & Wynne, H. The Canadian problem gambling index. Final report Ottawa: Canadian Centre on Substance Abuse (2001).
- 75.Conway ARA, et al. Working memory span tasks: A methodological review and user’s guide. Psychon. Bull. Rev. 2005;12:769–786. doi: 10.3758/BF03196772. [DOI] [PubMed] [Google Scholar]
- 76.Saunders JB, Aasland OG, Babor TF, De La Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption-II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- 77.Gache P, et al. The Alcohol Use Disorders Identification Test (AUDIT) as a Screening Tool for Excessive Drinking in Primary Care: Reliability and Validity of a French Version. Alcohol. Clin. Exp. Res. 2005;29:2001–2007. doi: 10.1097/01.alc.0000187034.58955.64. [DOI] [PubMed] [Google Scholar]
- 78.Heatherton T, Kozlowski L, Frecker R, Fagerström KO. The Fagerström test for nicotine dependence: a revision of the Fagerstrom Tolerance Questionnaire. Addiction. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- 79.Derogatis LB, Cleary PA. Confirmation of the Dimensional Structure of the Scl-90: A Study in Construct Validation. J. Clin. Psychol. 1977;33:981–989. doi: 10.1002/1097-4679(197710)33:4<981::AID-JCLP2270330412>3.0.CO;2-0. [DOI] [Google Scholar]
- 80.Watson D, Anna L, Tellegen A. Development and Validation of Brief Measures of Positive and Negative Affect: The PANAS Scales. J. Pers. Soc. Psychol. 1988;54:1063–1070. doi: 10.1037/0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- 81.Beck AT, Steer RA, Carbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clin. Psychol. Rev. 1988;8:77–100. doi: 10.1016/0272-7358(88)90050-5. [DOI] [Google Scholar]
- 82.Spielberger, C. D., Gorsuch, R. L., Lushene, R., Vagg, P. & Jacobs, G. Manual for the State-Trait Anxiety Inventory (Consulting Psychologists Press, 1983).
- 83.Holmes TH, Rahe RH. The social readjustment rating scale. J. Psychosom. Res. 1967;11:213–218. doi: 10.1016/0022-3999(67)90010-4. [DOI] [PubMed] [Google Scholar]
- 84.Whiteside SP, Lynam DR, Miller JD, Reynolds SK. Validation of the UPPS impulsive behaviour scale: a four‐factor model of impulsivity. Eur. J. Personal. 2005;19:559–574. doi: 10.1002/per.556. [DOI] [Google Scholar]
- 85.Otto AR, Raio CM, Chiang A, Phelps EA, Daw ND. Working-memory capacity protects model-based learning from stress. Proc. Natl. Acad. Sci. USA. 2013;110:20941–20946. doi: 10.1073/pnas.1312011110. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data will be made available on the following lab website: http://psymed.ulb.be/.