Abstract
The testicular seminomas are germ-cell tumors which account for approximately 50% of all testicular tumors. Most primary testicular germ cell tumors metastasize through a lymphatic system in a predictable pattern with the retroperitoneal lymph nodes being the most common initial metastatic site. Hematological metastasis to the distant organs is less common, and except for pulmonary metastasis, changes the classification from good to intermediate prognosis. Metastasis of testicular seminoma to the prostate is an extremely rare entity with only five reported cases in the literature. In this report, we present a 63-year-old male with recurrent testicular seminoma presenting in prostate.
Introduction
Testicular cancer represents 1–2% of all male malignancies with an estimated incidence of 71,105 cases and 9,507 deaths in 2018.1 It mainly affects men between the ages of 15 and 35 years. Testicular germ cell tumors are classified into seminomas and non-seminomas, with seminoma accounting for more than half of the diagnoses.
Patients typically present with a painless testicular mass. Predisposing factors include Caucasian race, personal or family history of a testicular tumor, cryptorchidism, inguinal hernia, and hypospadias.
Stage-I seminoma is localized to testis, however up to 25–30% of the stage I seminoma patients have clinically undetectable metastasis in the retroperitoneal lymph nodes and recur after orchiectomy. If metastases occur beyond the retroperitoneal lymphatics, the lung, liver, and brain are the most common sites of spread. Seminomas limited to testicle, with nodal metastasis or pulmonary metastasis are classified as good prognosis. However, non-pulmonary visceral metastasis pertains intermediate prognosis. Testicular seminoma metastasizing to the prostate is a rare occurrence; only five patients with prostate metastases from testicular seminoma were reported in the literature. We present a rare case of prostatic seminoma diagnosed three years after initial orchiectomy for stage IB testicular seminoma.
We performed a comprehensive search of electronic databases (e.g., Medline, Embase, Web of Science) using MeSH terms and keywords for testicular seminoma, prostate metastasis, and treatment.
Case report
A 63-year-old gentleman presented with 3-month history of right-sided enlarging testicular mass. His past medical history was unremarkable and had no family or previous surgical history. Physical exam revealed a right-sided slightly tender mass without overlying erythema. Ultrasonography of the right testicle confirmed a hypoechoic 5 cm mass in the right testis. Subsequently, patient underwent a right radical inguinal orchiectomy. Pathology demonstrated a pure seminoma involving the epididymis head and invading through the tunica albuginea to involve the tunica vaginalis (pT2). No vascular invasion was noted, and the spermatic cord was free of malignancy. Immunohistochemical staining was positive for CD117 and negative for CD30. CT scan of the abdomen and pelvis (A/P) with IV contrast and chest X-ray (CXR) were negative for any metastatic disease. Initial tumor markers were beta-HCG (human chorionic gonadotropin): <5, AFP (alpha-fetoprotein): 3.7, and LDH (lactate dehydrogenase): 359 (<3 times of upper limit) (Fig. 1 and Fig. 2). Patient's disease was initially classified as stage IB, T2N0M0SX. Treatment options including one dose of carboplatin vs. active surveillance discussed with the patient, and he opted for active surveillance (Table 1). Patient was compliant with active surveillance and all imaging was done on time with no evidence of recurrence. On scheduled CT scan of the abdomen and pelvis during year three of active surveillance, bilateral enlarged pelvic lymph nodes were detected. MRI of the pelvis subsequently showed an amorphous mass of 30 mm at the right basilar central zone of prostate with unequivocal extra-prostatic extension and invasion of the bilateral seminal vesicle, right greater than left. This was designated as a PI-RADS 5 lesion, high probability lesion for malignancy. There were left-sided sub centimeter perirectal lymph nodes possessing morphology and MRI characteristics suspicious for nodal metastases. The mass was seen as a large focus of uptake involving the base of the prostate and seminal vesicle and bilateral iliac chain in PET-CT scan which was suspicious for malignancy. The biopsy of the lesion from right prostate base was consistent with seminoma and positive for PLAP, CS117, OCT3/4 immunostains and negative for pancytokeratin. Patient was initiated on Bleomycin, Etoposide, Cisplatin (BEP) regimen with curative intent. During the first cycle, he developed neutropenic fever with Salmonella infection so that etoposide dose was reduced. Patient's clinical status was also complicated with bleomycin-induced pneumonitis which was alleviated with steroids. Repeat PET scan after the chemo showed interval resolution of the hypermetabolic involvement of the right prostate gland and hypermetabolic adenopathy. The patient had no clinical, laboratory or imaging findings of recurrence at the 10-month interval from last chemotherapy.
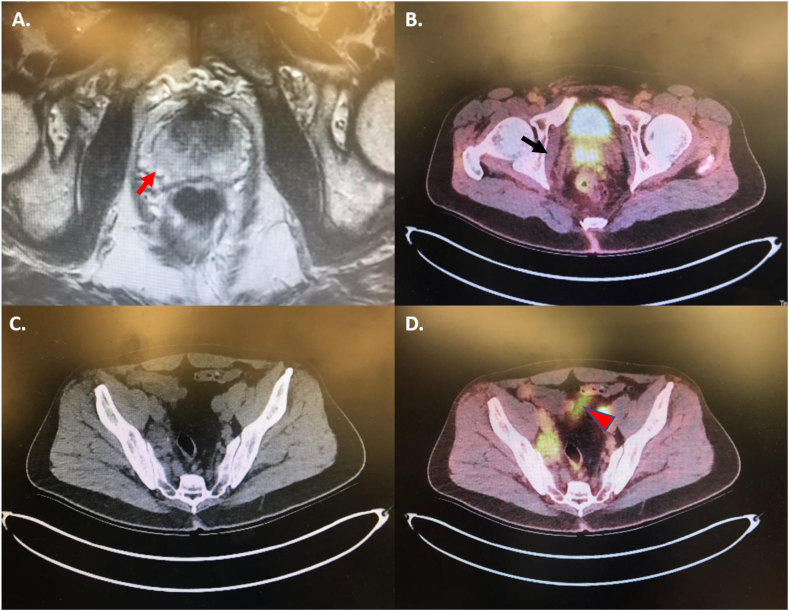
Fig. 1.
MRI of the pelvis (A) showed a 3 cm mass (red arrow) at the right basilar central zone of prostate. The mass was hyperintense in PET-CT scan involving the base of the prostate and seminal vesicle. (B, black arrow). Bilateral pelvic lymphadenopathies were noted in surveillance CT-scan (C) and they were hyperintense in PET-CT scan. (D, red arrowhead). (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
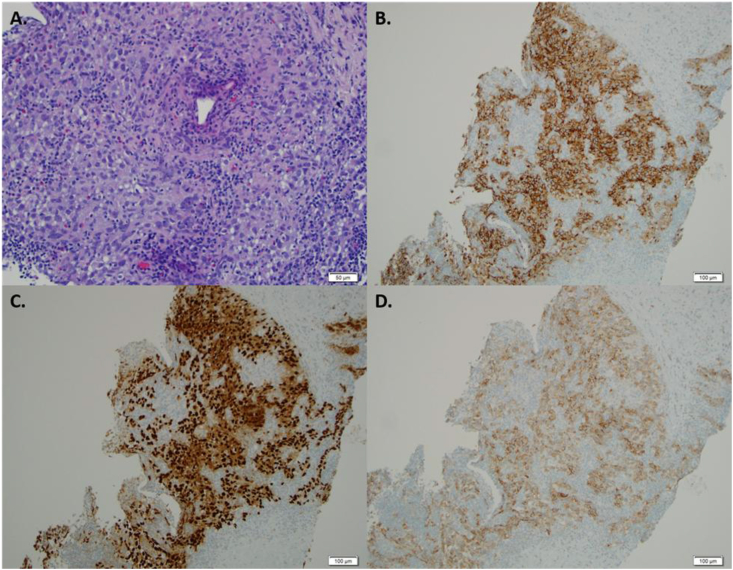
Fig. 2.
Tumor cells show pink to focally clear cytoplasm, vesicular nuclei and lymphocytic infiltration (A). Tumor cells are positive for PLAP (B), OCT3/4 (C) and CD117 (D), and negative for pancytokeratin (not shown). (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Table 1.
Active surveillance schedule planned for 5 years.
| Year (y) | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| Follow-up visits | 4 times | 4 times | 3 times | 3 times | twice |
| Tumor markers | 4 times | 4 times | 3 times | 3 times | twice |
| CT A/P, W/C | 3 times | twice | twice | once | once |
| CXR or CT chest | Annually | ||||
CT = computed tomography; A/P = abdomen and pelvis; CXR = chest x-ray.
Discussion
Metastatic spread of seminoma predominantly occurs via the lymphatic drainage pathways to the retroperitoneal lymph nodes with 84–94% developing in para-aortic lymph nodes. Our patient had only iliac lymph nodes involvement with no evidence of para-aortic lymph node involvement.
Seminomas can rarely cause prostatic metastases and the mechanism involved in prostatic infiltration is unclear. To date, five cases of prostate metastasis from testicular seminoma have been reported in the English literature. Our patient was asymptomatic when metastasis was predominantly detected, and enlarged pelvic lymph nodes were found on follow-up CT.
There are strategies to prevent relapses after post-orchiectomy for stage I seminomas. Previous studies have found comparable survival outcomes between the surveillance-only strategies and adjuvant therapies such as radiotherapy and single agent carboplatin.2 To avoid over-treatment of patients, the use of surveillance-only strategy is recommended by NCCN guidelines as a level 1 recommendation.3 A pooled analysis of four surveillance studies (638 patients) identified the size of primary tumor (>4 cm) and rete testis invasion as the main risk factors for relapse in patients with stage I seminoma managed with surveillance.4
Ruf et al. examined the biological characteristics of metastatic and stage I seminomas with clinically undetectable retroperitoneal metastasis in primary staging using small RNA next-generation sequencing. These tumors were indistinguishable from each other at the transcriptional level suggesting that metastatic seminomas are continuum of occult metastasis.5 Further studies examining the biological differences between non-metastasized seminoma and seminoma metastasized to solid organs will enhance our understanding of the biological processes of these tumors which may allow us to risk stratify patients in primary staging and minimize the unnecessary use of chemotherapy.
Conclusion
Prostate is an unusual site for metastasis from testicular cancer and metastasis can be detected years after the initial diagnosis. We, herein, highlight the possibility of prostate seminoma originating from the testis in an asymptomatic patient. More prospective studies assessing the histological and clinical risk factors for future relapse and optimal follow-up plans are warranted for stage I patients after the treatment.
References
- 1.Bray F., Ferlay J., Soerjomataram I., Siegel R.L., Torre L.A., Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA A Cancer J Clin. 2018;68(6):394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 2.Yu H.Y., Madison R.A., Setodji C.M., Saigal C.S. Quality of surveillance for stage I testis cancer in the community. J Clin Oncol. 2009;27(26):4327–4332. doi: 10.1200/JCO.2008.19.9406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Comprehensive Cancer Network Testicular cancer (version 1.2019. https://www.nccn.org/professionals/physician_gls/pdf/testicular.pdf
- 4.Warde P., Specht L., Horwich A. Prognostic factors for relapse in stage I seminoma managed by surveillance: a pooled analysis. J Clin Oncol. 2002;20(22):4448–4452. doi: 10.1200/JCO.2002.01.038. [DOI] [PubMed] [Google Scholar]
- 5.Ruf C.G., Port M., Schmelz H.U. Clinically apparent and occult metastasized seminoma: almost indistinguishable on the transcriptional level. PLoS One. 2014;9(5) doi: 10.1371/journal.pone.0095009. Published 2014 May 1. [DOI] [PMC free article] [PubMed] [Google Scholar]