Abstract
Background
We evaluate the effect of repairing the upper subscapularis tendon at an alternative location on the anterior greater tuberosity above the center of rotation using a reverse shoulder arthroplasty (RSA) muscle model.
Methods
We compared an innovative subscapularis repair on the anterior aspect of the greater tuberosity with the standard repair on the lesser tuberosity in a previously validated digital linear RSA muscle model. Standard repair vs. a new repair datasets were compared for 3 RSA designs. Each model was run through humeral abduction from 0° to 140° in 2.5° increments; the resulting moment arm measurements (model of tendon efficiency) were recorded in millimeters for 3 sections (superior, middle, inferior). An isolated upper two-thirds subscapularis repair to the anterior greater tuberosity was also evaluated (the over-the-top repair).
Results
The new over-the-top subscapularis repair significantly increased the abduction moment arm lengths in the superior, middle, and inferior subscapularis components compared with the standard repair to the lesser tuberosity at all levels of glenohumeral abduction and for all 3 RSA designs. Repair of the upper two-thirds of the subscapularis to the new location was an abductor at a much lower level of abduction compared with the native subscapularis repair.
Conclusion
By repairing the upper subscapularis tendon above the center of rotation (over-the-top repair) in an RSA muscle model, the subscapularis has an improved movement arm and functions as an abductor through a greater range of motion that may result in clinically increased muscle efficiency and improved strength.
Keywords: Shoulder abductors, shoulder abduction moment, muscle model, subscapularis repair, subscapularis tendon, reverse shoulder arthroplasty
Although reverse shoulder arthroplasty (RSA) has been proven to help patients regain function for multiple shoulder pathologies, complications remain an issue.3,4,22 Current complication rates are lower compared with early reports of RSA, but several relatively common complications exist such as dislocation and scapular spine fractures that can affect functional outcomes.7,8,24,28 Improved knowledge of techniques to prevent complications is necessary to decrease their incidence.
Subscapularis repair after RSA remains controversial but represents a potentially modifiable risk factor for dislocation. The subscapularis has been shown to be an adductor in biomechanical models of RSA counteracting the deltoid forces,1,9,12,13 especially at lower levels of abduction One cadaver study showed that only the upper subscapularis tendon was an abductor after 35° of abduction after RSA using a lateralized glenoid implant design, with the middle and lower subscapularis tendons never being abductors.1 Despite this apparent biomechanical disadvantage, some surgeons recommend subscapularis repair to reduce instability rates2,3 and improve internal rotation.7,14 Other surgeons have shown similar dislocation rates with and without subscapularis repair in RSA.4,7,20,23,25 A recent meta-analysis reported that subscapularis repair when using a medialized RSA design may be prudent to decrease the risk of dislocation,15 which is attributed to the deltoid imparting a lateral force to the humerus in the medialized RSA design. Despite these benefits, some surgeons are concerned that subscapularis repair after RSA causes a loss of external rotation due to overpowering the poor-quality remaining external rotators.23 Further confounding the debate, the effect of subscapularis repair may be implant-design specific.6,7,9,15,21,23,25
Although several authors have described their results of subscapularis repairs after RSA, none discuss the ideal location for subscapularis repair. Subscapularis repair to its original location on the lesser tuberosity in biomechanical studies renders the subscapularis as a shoulder adductor in RSA.1,9,10,12 Subscapularis repair to alternative locations on the humeral head would likely lead to different force vectors,13 which may be favorable after RSA.
Repair of the subscapularis superior to its original location on the anterior aspect of the greater tuberosity or to the anterior supraspinatus tendon has the potential to increase the abduction moment arm of the subscapularis tendon during shoulder abduction after RSA. By increasing the abduction moment, a subscapularis repair has the potential to improve motion, decrease deltoid stress, and simultaneously decrease the risk of anterior instability. The purpose of this study is to evaluate how altering the site of the subscapularis repair affects the subscapularis biomechanics, specifically the abduction moment arm, using a new repair location after RSA.
Material and methods
A previously published computer simulated biomechanical model was used to evaluate muscle moment arm lengths during glenohumeral motion.10,11 The model was used to evaluate the abduction moment arm of the subscapularis tendon in varying degrees of glenohumeral abduction, from 0° to 140° in 2.5° increments. Moment arm lengths were calculated in millimeters using a uniplanar model. In this model, the subscapularis tendon is divided into 3 parts (superior, middle, and inferior), as has been described in other models.10
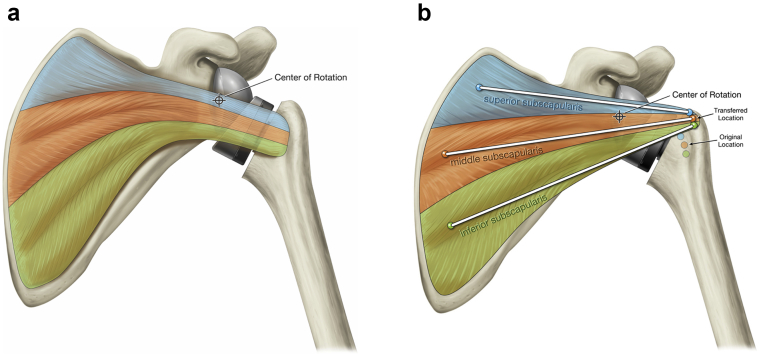
Two subscapularis tendon repair locations were evaluated: a native repair and the new tendon repair location. The native repair attached the subscapularis tendon to the native location on the lesser tuberosity (Fig. 1, a). The new repair attached the tendon superior and lateral to the bicipital groove on the anterior aspect of the greater tuberosity (Fig. 1, b). Moment arm lengths were evaluated with the 2 repair locations using 3 commonly used and available classes of RSA designs, including the medial glenoid center of rotation (COR) with a medial humerus (MGMH) design, the lateral glenoid COR with a medial humerus (LGMH) design, and the medial glenoid COR with a lateral humerus (MGLH) design.6
Figure 1.
Native vs. new repair: the native repair attaching the subscapularis tendon to the native location on the lesser tuberosity (a); the new repair attaching the tendon superior and lateral to the bicipital groove on the anterior aspect of the greater tuberosity (b).
The MGMH design used was based on the traditional Grammont RSA prosthesis (Delta Reverse Shoulder; DePuy Synthes, Warsaw, IN, USA), with a glenoid component whose COR is on the glenoid face and an inset humeral component with a 155° humeral neck shaft angle. The MGLH design was based on the Exactech Equinoxe prosthesis (Gainesville, FL, USA) whose glenoid COR is near the glenoid face (2 mm lateral to the glenoid) and has an onlay humeral component with a 145° neck angle. The LGMH design was based on the DJO Encore prosthesis (Dallas, TX, USA) whose glenoid component had a COR 10 mm lateral to the glenoid face and an inset humeral component with a 135° neck angle. A commonly used commercially available implant was modeled for each design based on published specifications (ie, the glenosphere diameter and thickness for each are 36 mm × 18 mm for MGMH, 32 mm × 26 mm for LGMH, and 38 mm × 21 mm for MGLH). Each design was implanted into the computerized bone models following the manufacturer's recommended technique. The glenoid components were placed with the goal of 2 mm of inferior overhang for the medialized glenoid designs and the inferior glenosphere aligning with the inferior edge of the glenoid in the LGMH design. The models were virtually constructed in Unigraphics NX (Siemens, Plano, TX, USA), including all bone, implant, and muscle geometries. The data were imported into custom analysis software in Matlab (Mathworks, Natick, MA, USA) to calculate the moment arm lengths during abduction.
The paired Student t-test was used to compare the new repair location with the standard repair for each part of the tendon and the entire tendon. Significance was set at an alpha level of .05.
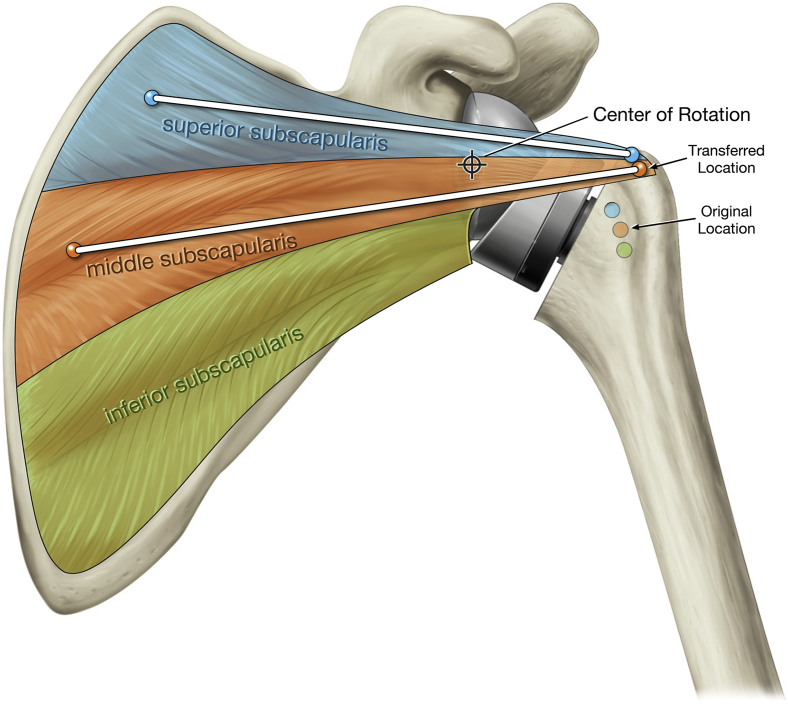
The abduction moment arm differences were then compared between the standard subscapularis repair and the new repair location for all 3 RSA designs. In addition, comparisons of the standard repair to a repair of the superior 2/3 (Fig. 2) and the superior one-third of the subscapularis tendon in the new location were calculated. These comparisons were chosen based on the new repair technique used by the first author (JJK), who has been performing this modified repair since 2015.
Figure 2.
Schematic of the upper two-thirds subscapularis repair to the new over-the-top location with force vectors in reverse shoulder arthroplasty with a medial glenoid and lateral humerus design implant.
The subscapularis repair technique in RSA described here is referred to as the over-the-top subscapularis repair. This technique was developed based on the following theoretical principles: converting the subscapularis to a shoulder abductor, decreasing the subacromial dead space, and increasing anterior shoulder stability.
Surgical technique
A subscapularis peel is used with this technique. After the reduction of the final prosthesis, a 270° release of the subscapularis is performed using blunt dissection. The superior border of the subscapularis tendon is freed from the rotator interval tissue to the coracoid base releasing the coracohumeral ligament if it is still attached. Inferior dissection is not performed to protect the axillary nerve.
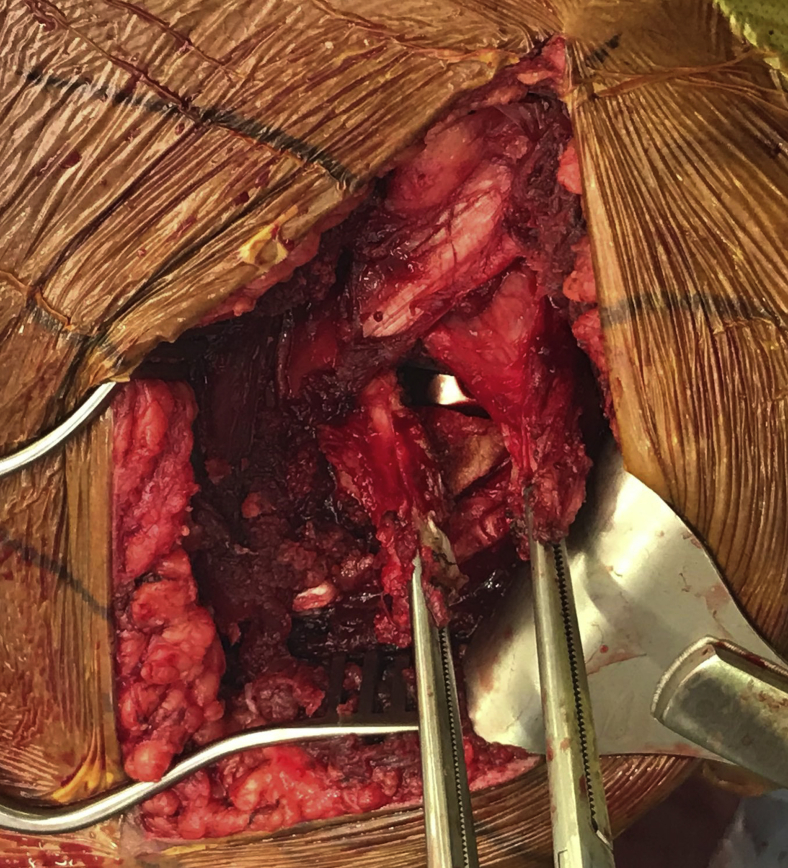
The lower subscapularis is then tenotomized longitudinally using electrocautery into the muscle under direct visualization to split the subscapularis tendon around the junction of the upper two-thirds and lower one-third as medially as possible (Fig. 3). The lateral aspect of the lower subscapularis tendon is excised.
Figure 3.
The lower subscapularis tenotomized longitudinally into the muscle with a Kocher on each part of the subscapularis tendon pulling them laterally. The medial aspect is on the top left of the image.
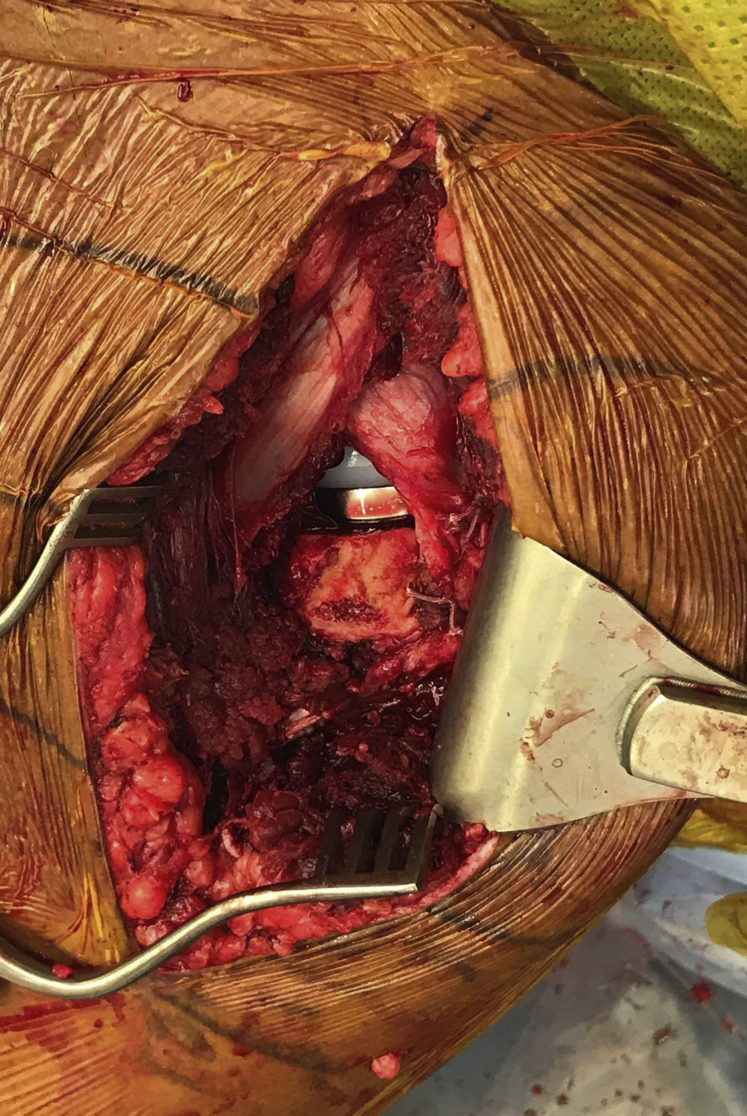
Subscapularis mobility is assessed. If the remaining tendon can be brought back to the anterior greater tuberosity with mild force at neutral abduction and 20° of external rotation, it is considered reparable. Repair of the upper subscapularis tendon is then performed to an intact anterior supraspinatus tendon or a remnant of the supraspinatus tendon on the anterior greater tuberosity with interrupted nonabsorbable suture (Fig. 4). If no soft tissue remains on the anterior greater tuberosity, then the upper subscapularis tendon is repaired through small drill holes on the anterior-most aspect of the greater tuberosity just lateral to the bicipital groove.
Figure 4.
Surgical photograph demonstrating the repair of the upper subscapularis tendon performed to an intact anterior supraspinatus tendon on the anterior greater tuberosity with interrupted nonabsorbable suture. The medial aspect is on the top left of the image.
Results
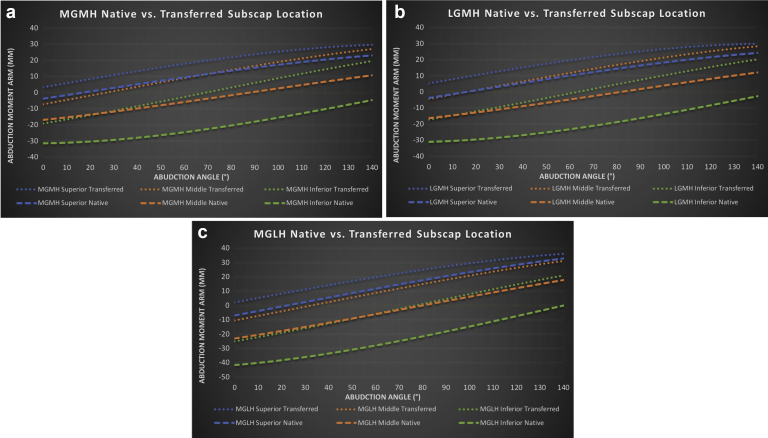
The new over-the-top repair location for the subscapularis tendon significantly increased the abduction moment arm lengths in the superior, middle, and inferior subscapularis components compared with the standard repair to the lesser tuberosity at all levels of glenohumeral abduction and for all 3 RSA designs tested (Table I, Fig. 5, a-c). In the traditional subscapularis repair position, the upper subscapularis functioned as an abductor above 17.5° of abduction at the earliest. When repaired in the over-the-top position, the upper subscapularis tendon functioned as an abductor at all angles of glenohumeral abduction. The abduction moment arm of the middle subscapularis tendon in the transferred model was similar to the superior subscapularis tendon in the native insertion model for all designs tested, transitioning from an adductor to abductor beyond 17.5° of glenohumeral abduction (Fig. 5, a-c).
Table I.
Moment arms in the different designs and scenarios tested
| Implant design | Tendon | Novel repair mean moment arm (mm) | Native repair mean moment (mm) | P value | Novel repair tipping point to be an abductor (degrees) | Native repair tipping point to be an abductor (degrees) |
|---|---|---|---|---|---|---|
| MGMH | Superior | 18.7 | 10.8 | <.0001 | 0 | 17.5 |
| Middle | 11.0 | −3.5 | <.0001 | 27.5 | 90 | |
| Inferior | 0.1 | −21.0 | <.0001 | 70 | Never | |
| Total | 9.9 | −4.6 | <.0001 | 30 | 95 | |
| LGMH | Superior | 20.3 | 11.6 | <.0001 | 0 | 17.5 |
| Middle | 13.5 | −2.4 | <.0001 | 17.5 | 82.5 | |
| Inferior | 1.8 | −19.6 | <.0001 | 65 | Never | |
| Total | 11.9 | −3.5 | <.0001 | 22.5 | 87.5 | |
| MGLH | Superior | 21.3 | 14.0 | <.0001 | 0 | 25 |
| Middle | 11.2 | −3.0 | <.0001 | 35 | 82.5 | |
| Inferior | −2.3 | −23.6 | <.0001 | 77.5 | Never | |
| Total | 10.1 | −4.2 | <.0001 | 37.5 | 85 |
MGMH, medial glenoid/medial humerus; LGMH, lateral glenoid/medial humerus; MGLH, medial glenoid/lateral humerus.
Figure 5.
The abduction moment arm of the subscapularis tendon in the native repair and the new repair location (a-c): medial glenoid/medial humerus design (MGMH, a); lateral glenoid/medial humerus (LGMH, b); medial glenoid/lateral humerus (MGLH, c).
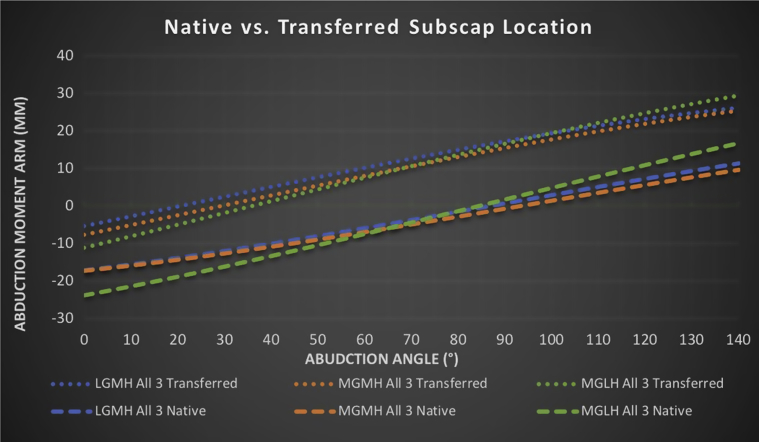
The over-the-top subscapularis repair improved the mean abduction moment arms of the entire tendon compared with the standard subscapularis repair at all angles of abduction in all 3 RSA designs evaluated (Fig. 6). The abduction moment arm increased on average 14.5 mm for the MGMH design, 14.3 mm for the MGLH design, and 15.4 mm for the LGMH design when the entire subscapularis tendon was transferred to the over-the-top position (Table I). The subscapularis became an abductor at an average of 65° earlier for the MGMH design, 47.5° earlier for the MGLH design, and 65° earlier for the LGMH design (Table I, Fig. 6). The earliest that the entire subscapularis tendon became an abductor during repair at the anatomic insertion after RSA was 85° of abduction. This was reduced to 20° of abduction with the new repair technique (Fig. 6).
Figure 6.
The mean abduction moment arm of the entire subscapularis tendon in the over-the-top subscapularis repair vs. the standard subscapularis repair in all 3 RSA designs. RSA, reverse shoulder arthroplasty; LGMH, lateral glenoid/medial humerus; MGMH, medial glenoid/medial humerus; MGLH, medial glenoid/lateral humerus.
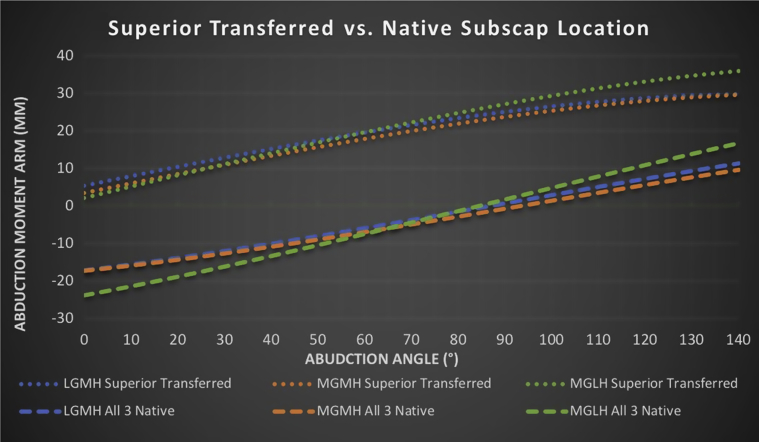
Isolated repair of the upper one-third of the subscapularis tendon to the new repair location improved the average moment arm compared with the standard repair of the entire tendon 23.7 mm in the LGMH design, 25.4 mm in the MGLH design, and 23.3 mm in the MGMH design (Fig. 7).
Figure 7.
The mean abduction moment arm of the isolated repair of the upper one-third of the subscapularis tendon to the new repair location compared with the standard repair location in all 3 RSA designs. RSA, reverse shoulder arthroplasty; LGMH, lateral glenoid/medial humerus; MGMH, medial glenoid/medial humerus; MGLH, medial glenoid/lateral humerus.
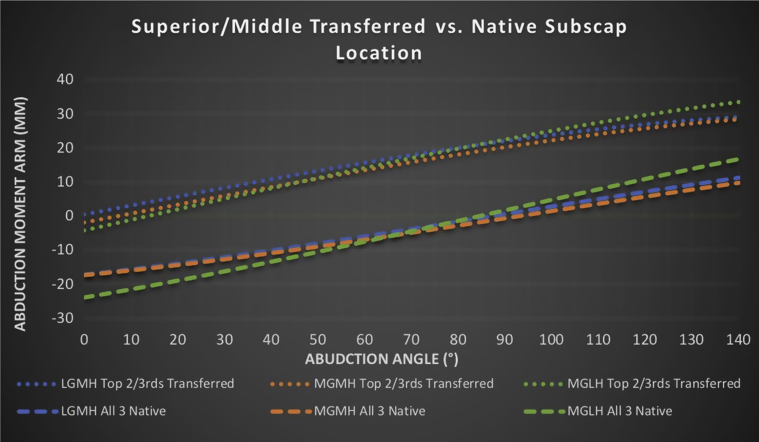
Repair of the upper two-thirds of the subscapularis tendon to the new location lateral to the bicipital groove compared with the standard repair location also improved the average abduction moment arm by 20.4 mm in the LGMG design, 20.4 mm in the MGLH design, and 19.4 mm in the MGMH design compared with the standard repair (Fig. 8). Repair of the upper two-thirds of the subscapularis to the new location was always an abductor in the LGMH design, became an abductor at 10° of abduction in the MGMH design, and became an abductor at 15° of abduction for the MGLH design (Fig. 8). By contrast, the native repair of the entire tendon does not have an abduction moment until 85° of abduction at the earliest when evaluating all 3 tested RSA designs.
Figure 8.
The mean abduction moment arm of the isolated repair of the upper one-third of the subscapularis tendon to the new repair location compared with the standard repair location in all 3 RSA designs. RSA, reverse shoulder arthroplasty; LGMH, lateral glenoid/medial humerus; MGMH, medial glenoid/medial humerus; MGLH, medial glenoid/lateral humerus.
Discussion
This study shows that there is a biomechanical abduction advantage to repairing the subscapularis using the new over-the-top location in RSA. The new repair improved the abduction moment in all degrees of glenohumeral abduction for all designs tested. This study shows that subscapularis repair in the over-the-top location, on the anterior greater tuberosity, improves abduction biomechanics compared with the standard repair location. In addition, lower subscapularis tenotomy further improves the abduction moment arm. The biomechanical abduction advantage of this repair has the possibility of improving overhead motion and may decrease complications related to deltoid muscle strain.
Several biomechanical studies have highlighted that subscapularis repair after RSA causes an adduction moment, which counteracts the deltoid forces needed for shoulder abduction,1,9,12,13 with one study demonstrating this in all 3 RSA designs.10 Hansen et al12 showed that a standard subscapularis repair to the lesser tuberosity increased the force required by the deltoid and posterior cuff for shoulder range of motion, and increased the joint reactive forces in RSA. Another MGMH RSA biomechanical study showed that subscapularis tenotomy decreased anterior shoulder stability and mean dislocation force by 18%.18 A cadaver study using an LGMH implant showed that only the upper subscapularis tendon was an abductor after 35° of abduction when evaluating the upper, middle, and lower subscapularis tendons after RSA.1 In this study, at the normal anatomic insertions, the middle and inferior subscapularis tendons were adductors throughout abduction in RSA.1 Lastly, a biomechanical RSA study using a lateralized glenosphere construct showed that the subscapularis was changed from an abductor in a native shoulder to an adductor after RSA in all degrees of flexion tested (0°-60°).9 The new over-the-top subscapularis repair increases the abduction force, which imparts a biomechanical advantage over the standard subscapularis repair technique to the lesser tuberosity in RSA.
The subscapularis has been shown to fire in-phase during native shoulder abduction in several studies.16,19,26,27 In addition, subscapularis activity patterns have correlated to supraspinatus muscle activation.19,27 Subscapularis activation in-phase with shoulder abduction further supports the biomechanical abduction advantage of the over-the-top subscapularis repair.
Kontaxis et al13 evaluated the biomechanical advantage of raising or lowering the subscapularis insertion site on the lesser tuberosity using virtual shoulder models of an MGLH RSA design. The authors found that repair to the lesser tuberosity provided an adduction moment, which was antagonistic to the deltoid during abduction. This adduction moment was lessened when the subscapularis was repaired more superiorly on the lesser tuberosity and also lessened with lower humeral neck-shaft angles. Simultaneously, lengthening of the subscapularis was minimized with a more superior repair location.13 The authors concluded that repair in a superior location has a biomechanical abduction advantage and would allow repair with less tension based on their modeling data. This study supports our results that superior subscapularis repair appears to be biomechanically advantageous in RSA. The over-the-top repair described in this study imparts a greater biomechanical advantage compared with a superior repair on the lesser tuberosity.
Studies on the range of motion effects of subscapularis repair after RSA remain conflicted. Subscapularis repair has been theorized to prevent full external rotation with RSA especially when the external rotators are deficient. Friedman et al7 found that, although internal rotation was better in the subscapularis repair group, it did not exceed the minimally clinical important difference using the MGLH design. However, active external rotation was also better in the subscapularis repair group (22° vs. 16°). Another study using the MGLH design theorized that those with a subscapularis tenotomy would have better external rotation after RSA; however, in its evaluation of 202 patients with and without subscapularis repair, the authors did not find a difference in active internal or external rotation between the groups.23
Further studies on the functional outcomes with and without subscapularis repair are also conflicted. One study found that RSA with glenosphere lateralization (+3 or +6 mm) had worse improvements in American Shoulder and Elbow Surgeons scores if the subscapularis tendon was repaired.25 In contrast, Roberson et al20 found no functional outcome, range of motion, or complication differences in 99 patients with and without subscapularis repair using lateralized glenoid prostheses. However, in the subscapularis repair subset, patients who underwent a subscapularis peel and repair had better change in forward elevation (26° more) compared with the tenotomy and repair group, but had similar American Shoulder and Elbow Surgeons and Penn Shoulder scores.20 Friedman et al7 reported on 591 primary RSA patients comparing functional outcomes with and without subscapularis repair using a lateralized humeral implant showing no difference in range of motion or outcomes scores between the groups. Similarly, another study showed a similar function in MGLH design RSA patients with and without subscapularis repair.23 There is a possible functional benefit to subscapularis repair after RSA, but studies are conflicting. This study suggests that the new repair location offers a biomechanical benefit, which may affect overall outcomes, but this study is ongoing.
Biomechanically, it makes sense that subscapularis repair has the potential to decrease the risk of anterior instability, but clinically this also appears to be affected by RSA design.5, 6, 7,9,21,23,25 Several authors have theorized that outcome and dislocation rates do not differ based on subscapularis repair in the RSA designs that lateralize either the humerus or the glenoid.6,21,23 One biomechanical cadaver study found that loading of the subscapularis tendon after RSA significantly increased the force needed for anterior dislocation in all 3 humeral neck-shaft angle designs tested.17
To our knowledge, this paper is the first to describe a lower subscapularis tenotomy with upper subscapularis repair in RSA. The biomechanical benefits of a lower subscapularis tenotomy increasing the abduction moment with the remaining subscapularis repair in RSA are evident in this study. This study shows that if only the upper one-third subscapularis tendon is repaired, it imparts only an abduction moment through all levels of abduction. If the upper two-thirds is repaired, the average abduction moment starts at very low levels of abduction. There are many clinical variables that are not assessed in this study, such as width of the tendon to be tenotomized as well as the increased surface area benefit for healing in upper two-thirds repair vs. a superior one-third repair. However, it is evident in this biomechanical analysis that tenotomy of the lower one-third of the subscapularis tendon imparts a biomechanical benefit in regard to the abduction moment in RSA when the upper subscapularis is repaired to the new over-the-top location as well as to the native location on the lesser tuberosity.
This biomechanical study has obvious limitations. The main limitation is that uniplanar biomechanical data cannot always be directly translated to multiplanar surgical anatomy; however, the study technique presented here has been used as the foundation for multiple previous studies assessing forces in an RSA model.10,11,13 In addition, this model did not evaluate all clinical scenarios of rotator cuff deficiency such as the antagonistic effects of the posterior rotator cuff. In addition, although this technique has been applied clinically, reported functional outcomes are lacking.
Conclusion
Subscapularis repair to the anterosuperior greater tuberosity after RSA imparts a biomechanical advantage in abduction compared with the standard subscapularis repair. The advantage is seen at all levels of abduction and in all 3 RSA designs evaluated. In addition, the advantage is more pronounced with a lower subscapularis tenotomy. The new over-the-top subscapularis repair appears to provide a biomechanical abduction benefit in RSA compared with a standard repair. Future studies will evaluate if this new repair imparts similar clinical benefit in RSA.
Disclaimer
Joseph J. King is a paid consultant for Exactech, Inc. Alexander T. Greene is a paid employee of Exactech, Inc. Matthew A. Hamilton is a paid employee of Exactech, Inc. Phong T. Diep is a paid employee of Exactech, Inc. This author, his immediate family, and any research foundation with which he is affiliated did not receive any financial payments or other benefits from any commercial entity related to the subject of this article. Thomas W. Wright receives royalties from Exactech, Inc., and Wolters Kluwer Health—Lippincott Williams & Wilkins. He is also a paid consultant with Exactech, Inc. Bradley S. Schoch is a paid consultant for Exactech, Inc. and receives royalties from Exactech, Inc.
Footnotes
No institutional review board approval was required as only biomechanics data are used in this study.
References
- 1.Ackland D.C., Roshan-Zamir S., Richardson M., Pandy M.G. Moment arms of the shoulder musculature after reverse total shoulder arthroplasty. J Bone Joint Surg Am. 2010;92:1221–1230. doi: 10.2106/JBJS.I.00001. [DOI] [PubMed] [Google Scholar]
- 2.Chalmers P.N., Rahman Z., Romeo A.A., Nicholson G.P. Early dislocation after reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23:737–744. doi: 10.1016/j.jse.2013.08.015. [DOI] [PubMed] [Google Scholar]
- 3.Cheung E.V., Sarkissian E.J., Sox-Harris A., Comer G.C., Saleh J.R., Diaz R. Instability after reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2018;27:1946–1952. doi: 10.1016/j.jse.2018.04.015. [DOI] [PubMed] [Google Scholar]
- 4.Clark J.C., Ritchie J., Song F.S., Kissenberth M.J., Tolan S.J., Hart N.D. Complication rates, dislocation, pain, and postoperative range of motion after reverse shoulder arthroplasty in patients with and without repair of the subscapularis. J Shoulder Elbow Surg. 2012;21:36–41. doi: 10.1016/j.jse.2011.04.009. [DOI] [PubMed] [Google Scholar]
- 5.Edwards T.B., Williams M.D., Labriola J.E., Elkousy H.A., Gartsman G.M., O'Connor D.P. Subscapularis insufficiency and the risk of shoulder dislocation after reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2009;18:892–896. doi: 10.1016/j.jse.2008.12.013. [DOI] [PubMed] [Google Scholar]
- 6.Flurin P.-H., Roche C.P. Design optimization and prosthesis classification. In: Frankle M., Marberry S., Pupello D., editors. Reverse shoulder arthroplasty. Springer; New York City: 2016. pp. 61–72. [Google Scholar]
- 7.Friedman R.J., Flurin P.-H., Wright T.W., Zuckerman J.D., Roche C.P. Comparison of reverse total shoulder arthroplasty outcomes with and without subscapularis repair. J Shoulder Elbow Surg. 2017;26:662–668. doi: 10.1016/j.jse.2016.09.027. [DOI] [PubMed] [Google Scholar]
- 8.Gallo R.A., Gamradt S.C., Mattern C.J., Cordasco F.A., Craig E.V., Dines D.M. Instability after reverse total shoulder replacement. J Shoulder Elbow Surg. 2011;20:584–590. doi: 10.1016/j.jse.2010.08.028. [DOI] [PubMed] [Google Scholar]
- 9.Greiner S., Schmidt C., Konig C., Perka C., Herrmann S. Lateralized reverse shoulder arthroplasty maintains rotational function of the remaining rotator cuff. Clin Orthop Relat Res. 2013;471:940–946. doi: 10.1007/s11999-012-2692-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hamilton M.A., Diep P., Roche C., Flurin P.H., Wright T.W., Zuckerman J.D. Effect of reverse shoulder design philosophy on muscle moment arms. J Orthop Res. 2015;33:605–613. doi: 10.1002/jor.22803. [DOI] [PubMed] [Google Scholar]
- 11.Hamilton M.A., Roche C.P., Diep P., Flurin P.H., Routman H.D. Effect of prosthesis design on muscle length and moment arms in reverse total shoulder arthroplasty. Bull Hosp Jt Dis (2013) 2013;71(Suppl 2):S31–S35. [PubMed] [Google Scholar]
- 12.Hansen M.L., Nayak A., Narayanan M.S., Worhacz K., Stowell R., Jacofsky M.C. Role of subscapularis repair on muscle force requirements with reverse shoulder arthroplasty. Bull Hosp Jt Dis (2013) 2015;73(Suppl 1):S21–S27. [PubMed] [Google Scholar]
- 13.Kontaxis A., Windsor E., Eno J., Chen X., Dines D., Gulotta L. Lateralization and attachment site affect subscapularis biomechanics after reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2019;28:e281–e283. [Google Scholar]
- 14.Lädermann A., Denard P.J., Tirefort J., Collin P., Nowak A., Schwitzguebel A.J.-P. Subscapularis-and deltoid-sparing vs traditional deltopectoral approach in reverse shoulder arthroplasty: a prospective case-control study. J Orthop Surg Res. 2017;12:112. doi: 10.1186/s13018-017-0617-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Matthewson G., Kooner S., Kwapisz A., Leiter J., Old J., MacDonald P. The effect of subscapularis repair on dislocation rates in reverse shoulder arthroplasty: a meta-analysis and systematic review. J Shoulder Elbow Surg. 2019;28:989–997. doi: 10.1016/j.jse.2018.11.069. [DOI] [PubMed] [Google Scholar]
- 16.O'Connell N.E., Cowan J., Christopher T. An investigation into EMG activity in the upper and lower portions of the subscapularis muscle during normal shoulder motion. Physiother Res Int. 2006;11:148–151. doi: 10.1002/pri.336. [DOI] [PubMed] [Google Scholar]
- 17.Oh J.H., Shin S.J., McGarry M.H., Scott J.H., Heckmann N., Lee T.Q. Biomechanical effects of humeral neck-shaft angle and subscapularis integrity in reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23:1091–1098. doi: 10.1016/j.jse.2013.11.003. [DOI] [PubMed] [Google Scholar]
- 18.Pastor M.F., Kraemer M., Wellmann M., Hurschler C., Smith T. Anterior stability of the reverse shoulder arthroplasty depending on implant configuration and rotator cuff condition. Arch Orthop Trauma Surg. 2016;136:1513–1519. doi: 10.1007/s00402-016-2560-3. [DOI] [PubMed] [Google Scholar]
- 19.Reed D., Cathers I., Halaki M., Ginn K.A. Does load influence shoulder muscle recruitment patterns during scapular plane abduction? J Sci Med Sport. 2016;19:755–760. doi: 10.1016/j.jsams.2015.10.007. [DOI] [PubMed] [Google Scholar]
- 20.Roberson T.A., Shanley E., Griscom J.T., Granade M., Hunt Q., Adams K.J. Subscapularis repair is unnecessary after lateralized reverse shoulder arthroplasty. J Bone Joint Surg Am Open Access. 2018;3:e0056. doi: 10.2106/JBJS.OA.17.00056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Routman H.D. The role of subscapularis repair in reverse total shoulder arthroplasty. Bull Hosp Jt Dis (2013) 2013;71(Suppl 2):108–112. [PubMed] [Google Scholar]
- 22.Trappey G.J., O'connor D.P., Edwards T.B. What are the instability and infection rates after reverse shoulder arthroplasty? Clin Orthop Relat Res. 2011;469:2505–2511. doi: 10.1007/s11999-010-1686-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vourazeris J.D., Wright T.W., Struk A.M., King J.J., Farmer K.W. Primary reverse total shoulder arthroplasty outcomes in patients with subscapularis repair versus tenotomy. J Shoulder Elbow Surg. 2017;26:450–457. doi: 10.1016/j.jse.2016.09.017. [DOI] [PubMed] [Google Scholar]
- 24.Wall B., Nové-Josserand L., O'Connor D.P., Edwards T.B., Walch G. Reverse total shoulder arthroplasty: a review of results according to etiology. J Bone Joint Surg Am. 2007;89:1476–1485. doi: 10.2106/JBJS.F.00666. [DOI] [PubMed] [Google Scholar]
- 25.Werner B.C., Wong A.C., Mahony G.T., Craig E.V., Dines D.M., Warren R.F. Clinical outcomes after reverse shoulder arthroplasty with and without subscapularis repair: the importance of considering glenosphere lateralization. J Am Acad Orthop Surg. 2018;26:e114–e119. doi: 10.5435/JAAOS-D-16-00781. [DOI] [PubMed] [Google Scholar]
- 26.Wickham J., Pizzari T., Balster S., Ganderton C., Watson L. The variable roles of the upper and lower subscapularis during shoulder motion. Clin Biomech (Bristol, Avon) 2014;29:885–891. doi: 10.1016/j.clinbiomech.2014.07.003. [DOI] [PubMed] [Google Scholar]
- 27.Wickham J., Pizzari T., Stansfeld K., Burnside A., Watson L. Quantifying ‘normal’ shoulder muscle activity during abduction. J Electromyogr Kinesiol. 2010;20:212–222. doi: 10.1016/j.jelekin.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 28.Wierks C., Skolasky R.L., Ji J.H., McFarland E.G. Reverse total shoulder replacement: intraoperative and early postoperative complications. Clin Orthop Relat Res. 2009;467:225–234. doi: 10.1007/s11999-008-0406-1. [DOI] [PMC free article] [PubMed] [Google Scholar]