Abstract
We present a case of Collecting duct of Bellini carcinoma (CDC) which was masquerading as Genitourinary Tuberculosis/chronic granulomatous disease in a 43 year old women, who presented with complaints of low grade fever, loss of appetite, left loin pain and dyspnoea with recent onset of haemoptysis. After extensive evaluation, she was referred to urology where she underwent a laparoscopic assisted open left radical nephrectomy which was reported to be Collecting duct carcinoma.This case is being presented for the diagnostic dilemma it elicited throughout the evaluation.
Introduction
Collecting duct carcinomas are rare, aggressive malignancies with poor prognosis, arising from collecting duct epithelium of the kidney accounting for about 1%–3% of all renal cell carcinoma (RCC).1 These tumours are found to be locally advanced and with distant metastasis at presentation with 1 to 3-years disease-specific survival. Most published literatures gives a census of 100–250 cases of CDC being reported worldwide.
Case presentation
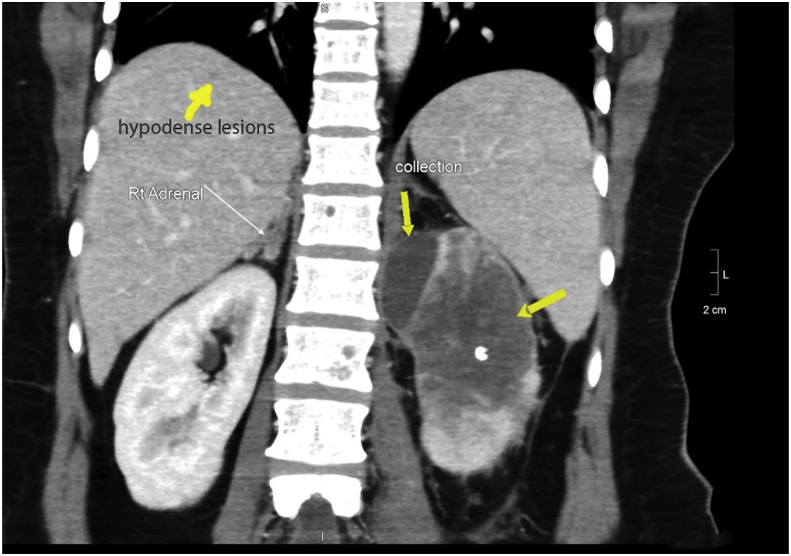
A hypertensive, diabetic, middle aged lady, was admitted with complaints of low grade fever, loss of appetite, vague left loin pain for 6 months and recent onset haemoptysis. Her lab parameters were normal with normal renal functions. CECT of whole abdomen revealed a poorly functioning upper pole and inter pole of left kidney with a 5.5 × 2.5cm subcapsular collection and renal vein thrombosis. Para aortic and mediastinal lymphadenopathy with multiple nodular lesions in liver and lungs were also seen, suggestive of malignancy or of infectious aetiology (Fig. 1).
Fig. 1.
CECT of abdomen showing sub capsular collection, non-obstructive left renal calculus, hypo-enhancing left renal upper polar and interpolar region with hypodense nodules in liver.
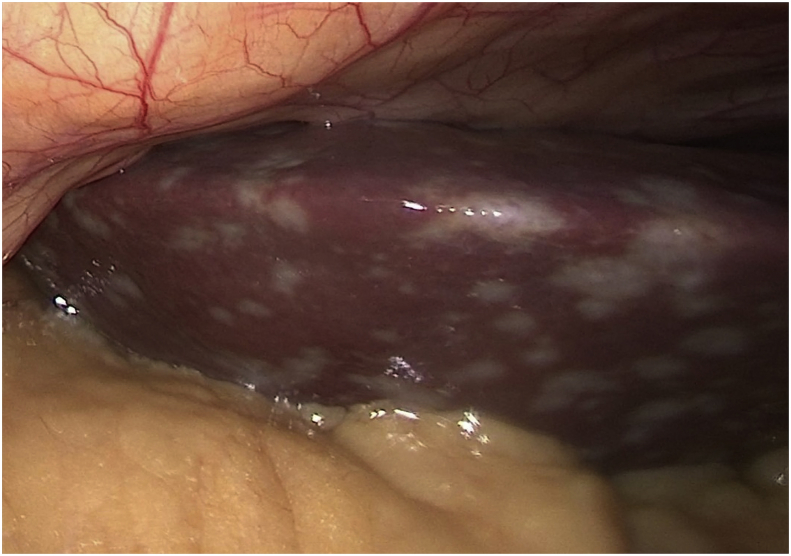
She was initially referred to a pulmonologist to evaluate for haemoptysis. Bronchoscopy, bronchial wash and Endoscopic Ultrasound guided bronchial biopsy for necrotic subcarinal nodes were negative for malignancy. GeneXpert was negative for tuberculosis. She was referred to urology department. Preoperative evaluation showed normal renal functions, coagulation profile and blood parameters. Echocardiography revealed moderate Pulmonary artery hypertension. After obtaining anaesthetist, nephrologist and pulmonologist clearance, she was taken up and successfully underwent Laparoscopic Assisted Open Left radical Nephrectomy + Para Aortic + Intra-aortocaval and Retro-aortic Lymphadenectomy. Intra-operatively laparoscopy revealed multiple whitish lesion studded all over the liver and in the retroperitoneum with extensive adhesion and nodules along the uretero-gonadal vein complex. (Fig. 2).
Fig. 2.
Intraoperative image of liver lesions.
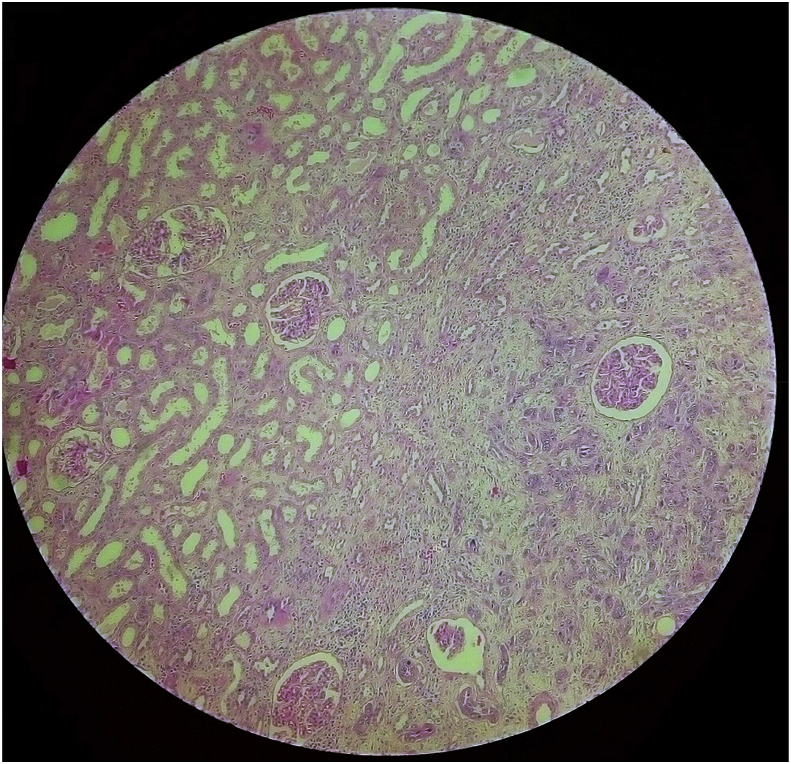
Postoperatively, the patient continued to have dyspnoea. CECT Chest revealed cavitating lesion in right lobe and partial thrombus in few of the sub-segmental branch of bilateral pulmonary arteries. She was started on Inj.Clexane. The histopathology was reported as CDC on POD-4. (Fig. 3).
Fig. 3.
This images shows infiltrative neoplasm with singly scattered, tubules and cords of neoplastic cells exhibiting dysplasia. Fibrosis is seen in the stroma.
Medical oncology opinion was obtained. Immunohistochemistry was positive for Pan cytokeratin, Vimentin, Cytokeratin 7 and 19, CD-10 and Epithelial membrane antigen, which was confirmatory of CDC of kidney. She was discharged on POD-10 and was advised to review after 3 weeks for chemotherapy. The patient was lost to follow-up. Subsequent telephonic conversation revealed that the patient had passed away one month following surgery.
Discussion
Collecting duct carcinoma (CDC) is an extremely rare malignancy of the kidney. It was first reported in 1976 by Mancilla – Jimenez, accounting for about 0.6–3% of all renal neoplasms. CDC originates from the collecting ducts of Bellini, situated in the distal part of the collecting duct in the renal medullary pyramids.2 The more common variants of RCC also mimics CDC. Hence, a precise pathologic diagnosis is of utmost importance since these malignancies have contrariness in treatment and prognosis, despite their similar clinical presentations.
CDC is predominantly common in black males (M:F = 65.3% vs. 59.9%) with mean age of 55 years, though our patient was a women in her early forties. The classical presentation is abdominal pain, flank mass and haematuria. CDC is more likely to present as high grade, high stage, lymph node positive metastatic disease. The most common metastatic sites are the lungs (57%), lymph nodes (48%) and osteoblastic bony metastasis.
The tumour is centrally located in the kidney grey-white in colour, firm in consistency often infiltrating the hilum. Histologically, there is tubulo-papillary and hobnail pattern with severe desmoplastic reactions. There is also presence of ramified vascular network and basal membrane like substance in epithelial clusters.3 The hobnail pattern is more specific for CDC.
The usual CT finding of CDC is a central medullary renal mass with minimal heterogenous contrast enhancement. There is also involvement of renal sinus and preserved renal contour akin to urotheliomas. The most common variant of clear cell and papillary variant of RCC also arises from central location, which makes the diagnosis of CDC more difficult.
CDC tumour cells express High-Molecular Weight Cytokeratins (HMWK) and Ulexeuropaeus Agglutinin-1 positivity(UEA -1)4. Conventional RCC markers such as CD10, CD15 are negative in CDC.4 Microsatellite allele typing have demonstrated monosomy of chromosome 1q, 6p, 8p and 12 q. VHL gene alteration is seen in about 8% of case of CDC.
Given the histological similarities between Urotheliomas and CDC, the later may be sensitive to chemotherapy and radiotherapy. Study with Gemcitabine with platinum based chemotherapy revealed partial to complete response in 26% of patients with metastatic CDC. Sunitinib and Nivolumab has also been shown to have potential benefit in metastatic CDC.5 Huge genomic profiling information on collecting duct carcinoma has also led to better understanding of the condition and potential targetable check points such as Programmed Death Ligand-1. Ongoing GETUG phase 2 trial and BONSAI study which explores the role of bevacizumab and Cabozantinib in metastatic CDC is expected to be over by 2021 and 2020.
Conclusion
CDC of kidney is a rare malignancy with rapidly worsening malignant course, which mostly presents as a metastatic disease in initial evaluation. The diagnosis is often by post-surgery histopathology and immunohistochemistry. Currently, surgery remains to be the first line standard of care with median survival of 13 months and with post-surgery adjuvant chemotherapy and/or targeted therapy increasing survival benefit by 4–5months.
Consent from patient
Obtained.
Funding
No funding was obtained for this case report study.
Declaration of competing interest
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.eucr.2019.101100.
Abbreviations
- RCC
Renal cell carcinoma
- CDC
Collecting duct carcinoma
- POD
post operative day
- CECT
Contrast enhanced computed tomography
Appendix A. Supplementary data
The following is the supplementary data to this article:
References
- 1.Auguet T., Molina J.C., Lorenzo A., Vila J., Sirvent J.J., Richart C. Synchronus renal cell carcinoma and Bellini duct carcinoma: a case report on a rare coincidence. World J Urol. 2000;18:449–451. doi: 10.1007/s003450000157. [DOI] [PubMed] [Google Scholar]
- 2.Chao D., Zisman A., Pantuck A.J. Collecting duct renal cell carcinoma: clinical study of a rare tumor. J Urol. 2002;167:71–74. doi: 10.1016/s0022-5347(05)65385-2. [DOI] [PubMed] [Google Scholar]
- 3.Kennedy S.M., Merino M.J., Linehan W.M., Roberts J.R., Robertson C.N., Neumann R.D. Collecting duct carcinoma of the kidney. Hum Pathol. 1990;21:449–456. doi: 10.1016/0046-8177(90)90209-n. [DOI] [PubMed] [Google Scholar]
- 4.Skinnider B.F., Folpe Al, Hennigar R.A. Distribution of cytokeratins and vimentin in adult renal neoplasm and normal renal tissue. Am J Surg Pathol. 2005;29:747–754. doi: 10.1097/01.pas.0000163362.78475.63. [DOI] [PubMed] [Google Scholar]
- 5.Miyake H., Haraguchi T., Takenaka A., Fujisawa M. Metastatic collecting duct carcinoma of the kidney responded to sunitinib. Int J Clin Oncol. 2011;16:153–155. doi: 10.1007/s10147-010-0116-z. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.