Highlights
-
•
Sacrococcygeal area is the commonest site of PNS.
-
•
However, it could be found in other regions like hand, intermammary, suprapubic, umbilicus, nose etc.
-
•
Breast pilonidal sinus is an extremely rare variant of PNS.
-
•
The aim of this report is to present a case of pilonidal sinus occurring in breast.
Keywords: Breast, Mammary, Pilonidal, Sinus, Abscess, Case report
Abstract
Introduction
Breast pilonidal sinus is an extremely rare variant of the condition, the report aims to present a case of pilonidal sinus occurring in the breast.
Case presentation
A 35-year-old female presented with a left breast discharging lesion for a 5-month duration. There was a local redness with multiple discharging sinuses on her left breast at 3–5 o’clock, 3–4 cm away from the nipple. The discharge was serosanguinous in appearance. The lesion was excised totally with primary closure under general anesthesia. Histopathological examination was consistent with pilonidal sinus.
Discussion
For atypical pilonidal sinus disease, surgery is the modality of choice but regarding sacrococcygeal pilonidal sinus, non-operative treatment begins to grow. The cardinal risk factors for recurrence and complications are male gender, family history, tobacco smoking, obesity, size of sinus, poor personal hygiene and surgical methods.
Conclusion
Breast pilonidal sinus is an extremely rare variant of the condition. It should be suspected on clinical examination. Surgical excision is the definitive treatment strategy.
1. Introduction
One of the common medical situations that accounts for almost 15% of suppurative anal conditions is pilonidal Sinus (PNS). It is an inflammatory condition resulting from skin penetration by a hair. The tract of the sinus is lined by granulation tissue which terminates in a pus-filled chamber [1,2]. The typical age range of affected individuals is 10–40 years [3]. Sacrococcygeal area is the commonest site of PNS. however, it could be found in other regions like the hands, intermammary, suprapubic, umbilicus, nose, interdigital web, groin, face, neck, prepuce, penis, postauricular, preauricular, submental, clitoris, scalp, endoanal, and axilla [[4], [5], [6], [7], [8], [9], [10]]. It may occur as an opened and discharging tract or as a manifestation of repetitive pus collection that presented like an inflammatory pattern: redness, local pain, warmth and tenderness [11,12].
Breast PNS (bPNS) is an extremely rare variant of the condition with only three reported cases in the literature [2,12,13]. The paper aims to report a rare case of bPNS in line with SCARE guidelines with a brief review of the condition [14].
1.1. Patient information
A 35-year-old housewife presented with a discharging lesion on her left breast for 5 months, not responding to medical treatment with a history of remission and relapse. She was nonsmoker, multiparous. Past-history was unremarkable.
1.2. Clinical findings
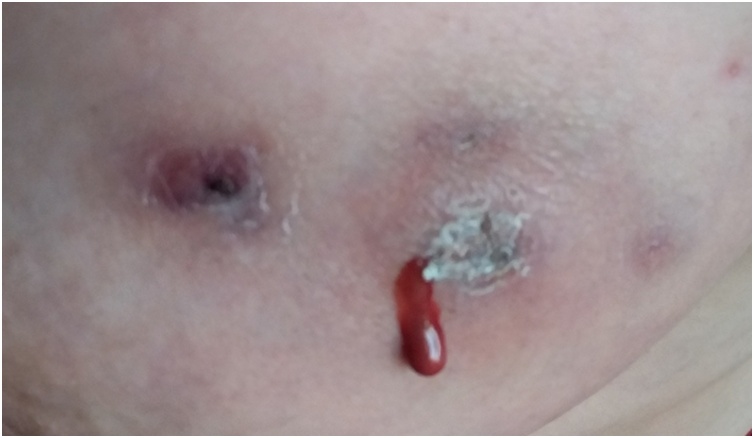
There was a local redness with multiple discharging sinuses on her left breast at 3–5 o’clock, 3–4 cm away from the nipple (Fig. 1). The discharge was mucoid in appearance.
Fig. 1.
Multiple discharging sinuses on her left breast at 3–5 o’clock.
1.3. Therapeutic intervention
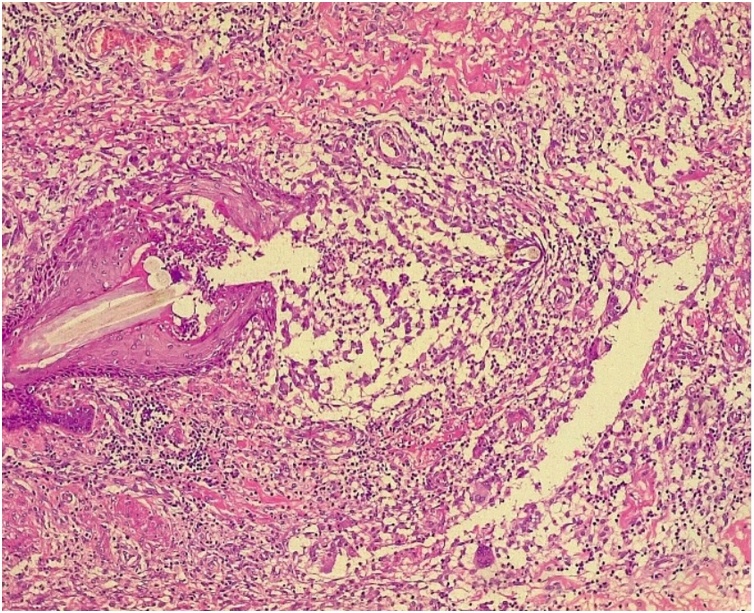
The lesion was excised totally with primary closure under general anesthesia. Histopathological examination showed invaginated epidermis forming a tract extending from the subcutaneous tissue to the skin. There was a hair shaft surrounded by granulation, consistent with a pilonidal sinus (Fig. 2).
Fig. 2.
Hair shaft surrounded by granulation tissue.
1.4. Follow-up and outcomes
Postoperatively she was followed up for six months, the wound healed completely without complications and there was no evidence for recurrence.
2. Discussion
Before puberty and after the age of forty, PNS is uncommon. The condition demonstrates male dominance with a ratio of 3:1 [15].
Young age, deep navel and cleft, hairiness, male sex, long term sitting and poor personal hygiene are among the risk factors [3]. In the management of sPNS, a variety of surgical and noninvasive techniques have been investigated. Drainage and simple incision, lying open, marsupialization, primary closure and excision, or rhomboid excision and Limberg flap were included in operative management while non-operative methods consist of different wound enhancing solutions and sclerosing agents that injected into the tract [16,17]. The ideal management should be complication-free, effective and safe, also it should minimize patient’s discomfort, recurrence rate, complications, hospital stay and long work absence. Surgical methods put the patient at risk of discomfort and long duration loss of workdays, so they do not meet the ideal treatment strategies. For atypical PNS, surgery is the modality of choice but regarding sPNS non-operative treatment begins to grow [3,17]. Recurrence and complications are not uncommon. According to the studies, cardinal risk factors for recurrence and complications are male gender, family history, tobacco, obesity, size of sinus, poor personal hygiene and surgical methods.
bPNS is a very rare variant of PNS [2,12,13]. Keighley et al. received a 52-year-old lady presenting with periareolar pain, and nipple inversion. Clinical assessment and ultrasound examination revealed periareolar abscess resistant to medication and frequent aspiration. They performed surgical excision. Histopathological examination confirmed the diagnosis of bPNS [2].
Lahiri and associates presented a case of bPNS occurred in a 28-year-old female. She presented with a 4-week history of left breast collection, the condition was provisionally diagnosed as an abscess complicating periductal mastitis, surgical excision was done and microscopic examination of the specimen revealed features consistent with bPNS [12].
Huges et al. reported their experience with a 38-year-old male patient who presented with a right breast mass for a 20-year duration with intermittent discharge from the lesion. After a thorough clinical examination and ultrasound study, they excised the lesion, histopathological examination demonstrated peri-areolar PNS disease [13].
In composite, bPNS is an extremely rare variant of the condition. It should be suspected on clinical examination. Surgical excision is the definitive treatment strategy.
Sources of funding
No source to be stated.
Ethical approval
Approval has been taken from Kscien centre.
Consent
Consent has been taken from the patient and the family of the patient.
Author’s contribution
Abdulwahid M. Salih: Surgeon performed the operation and follow up.
Shvan H. Mohammed, Fahmi H. Kakamad, and Rawezh Q. Salih: Writing the manuscript and follow up.
Zuhair D. Hammood, Hiwa O. Baba, and Imad J. Habibullah: literature review, final approval of the manuscript.
Registration of research studies
Not applicable.
Guarantor
Fahmi Hussein kakamad.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Declaration of Competing Interest
There is no conflict to be declared.
References
- 1.Salih A., Kakamad F., Essa R., Aziz M.S., Salih R.Q., Mohammed S.H. Pilonidal sinus of atypical areas: presentation and management. Pilonidal Sinus J. 2017;3(1):8–14. [Google Scholar]
- 2.Keighley J., Nadim A., Howlett D. Pilonidal abscess of the breast. BMJ Case Rep. CP. 2019;12(3) doi: 10.1136/bcr-2018-227381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shareef S.H., Hawrami T.A., Salih A.M., Kakamad F.H., Rahim H.M., Hassan H.A. Intermammary pilonidal sinus: the first case series. Int. J. Surg. Case Rep. 2017;41:265–268. doi: 10.1016/j.ijscr.2017.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Salih A.M., Kakamad F.H. A case report of endoanal pilonidal sinus. J. Case Rep. Images Surg. 2016;2(1):60–62. [Google Scholar]
- 5.Salih A.M., Kakamad F.H., Essa R.A., Mohammed S.H., Salih R.Q., Othman S. Pilonidal sinus of the umbilicus; presentation and management. Edorium J. Gastrointest. Surg. 2017;4:1–4. [Google Scholar]
- 6.Salih A.M., Kakamad F., Habibullah I.J., Abdulqadr M.H. Submental pilonidal sinus-the first reported case. Pilonidal Sinus J. 2017;3(1):4. [Google Scholar]
- 7.Salih Abdulwahid M., Kakamad Fahmi H., Essa Rawand A., Salih Rawezh Q., Rahim Hawbash M., Hassan Hunar A. Pilonidal sinus of hand; presentation and management: a systematic review of literature. Edorium J. Dermatol. 2017;2(1):1–4. [Google Scholar]
- 8.Salih A.M., Mohammed S.H., Dahat A.H. Postauricular pilonidal sinus; a case report with literature review. Pilonidal Sinus J. 2017;3(1):4. [Google Scholar]
- 9.Salih A.M., Hassan H.A., Rauf G.A., Habibullah I.J., Hammood Z.D., Hassan M.N. Pilonidal sinus of neck: a case report with literature review. Pilonidal Sinus J. 2017;3(1):5. [Google Scholar]
- 10.Shareef S.H., Salih A.M., Kakamad F.H., Habibullah I.J., Abdulqadr M.H. Intermammary pilonidal sinus: case presentation and management. Pilonidal Sinus J. 2017;3(2):2–3. [Google Scholar]
- 11.Salih A.M., Kakamad F.H., Essa R.A., Othman S., Salih R.Q., Aziz M.S. Pilonidal sinus of the face: presentation and management—a literature review. Pilonidal Sinus J. 2017;3(1):9–13. [Google Scholar]
- 12.Lahiri R., Mullen R., Ashton M.A., Abbott N.C., Pollock A.M. Pilonidal abscess in the breast: a case report. J. Surg. Case Rep. 2014;(6) doi: 10.1093/jscr/rju061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hughes R., Iqbal F.M., Salem F., Vidya R. Pilonidal cyst of the male breast: barber’s disease. Br. J. Hosp. Med. 2016;77(10):599. doi: 10.12968/hmed.2016.77.10.599a. [DOI] [PubMed] [Google Scholar]
- 14.Agha R.A., Borrelli M.R., Farwana R., Koshy K., Fowler A., Orgill D.P., For the SCARE Group The SCARE 2018 statement: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2018;60:132–136. doi: 10.1016/j.ijsu.2018.10.028. [DOI] [PubMed] [Google Scholar]
- 15.Salih A.M., Kakamad F.H., Abdulqadr M.H. Intermammary pilonidal sinus: a rare presentation. Int. J. Case Rep. Images. 2016;7(1):48–50. [Google Scholar]
- 16.Salih A.M., Kakamad F.H., Salih R.Q., Baba H.O., Mohammed S.H., Najar K.A. Pilonidal sinus of neck: a case report. Int. J. Case Rep. Images. 2018;9(1):1–4. [Google Scholar]
- 17.Salih A.M., Kakamad F.H., Salih R.Q., Mohammed S.H., Habibullah I.J., Hammood Z.D. Nonoperative management of pilonidal sinus disease: one more step toward the ideal management therapy—a randomized controlled trial. Surgery. 2018;164(1):66–70. doi: 10.1016/j.surg.2017.12.014. [DOI] [PubMed] [Google Scholar]