Abstract
Piriformis syndrome is an elusive condition that likely is overlooked and overdiagnosed in equal proportions. Image-guided injection of the muscle is an essential element in the assessment and management of this disorder. Ultrasonography allows visualization of the anatomy of the piriformis and its relation with the sciatic nerve. Ultrasound-guided injection of the muscle can be performed in an effective, reproducible fashion and, with careful attention to the details of the procedure, can be performed with minimal morbidity to the patient. This method has the advantage of being exceptionally well tolerated by the patient and can be performed in the office with minimal patient inconvenience and the opportunity for a real-time assessment of the patient's response to the injection. Our ultrasound-guided technique of piriformis muscle injection is detailed in this article.
Surgical treatment of piriformis syndrome at our center dates back to 2001 and forms the foundation of the observations made here. We initially reported an open posterior approach that, in 2009, was transitioned to an endoscopic method.1, 2, 3 Piriformis syndrome is an infrequent condition characterized by pain and tenderness localized to the piriformis and a variable number of associated sciatica symptoms, which are especially exacerbated by sitting. Approximately 5% of all sciatica cases are extraspinal in origin, with piriformis syndrome being one cause. A constellation of other disorders may present with deep buttock pain and variable sciatica, collectively referred to as “deep gluteal syndrome.”4 Distinguishing among these can present a clinical challenge, and commonly, the piriformis may be irritated either in conjunction with other structures or secondary to other disorders, such as hip or sacroiliac joint disease.
Treatment usually begins with sufficient investigation through history, examination, and imaging to implement a conservative program, including activity modification, oral anti-inflammatory medication, and supervised physical therapy, directed at modulating symptoms and improving patient quality of life. Severe cases characterized by the magnitude or duration of symptoms may require more extensive investigation and management.
The function of the piriformis changes depending on the position of the hip, and thus there are various examination maneuvers for passive stretching or resisted contraction used to elicit symptoms. The classic piriformis stretch test involves flexion, adduction, and internal rotation of the hip, assessing whether this creates pain within the region of the piriformis. This motion is also the same as the impingement test used to provoke joint symptoms associated with femoroacetabular impingement, except the symptoms from impingement would be expected to be more anteriorly based.5 With the hip extended, the piriformis is an external rotator, and buttock pain and/or sciatica symptoms are assessed with passive internal rotation (Pace sign) and resisted external rotation. With hip flexion, the muscle is an abductor, and resisted abduction in the supine position (Freiberg test)—or in the lateral decubitus position while palpating over the piriformis region—may be more sensitive.6
Historically, the 2 most reliable tests for isolating symptoms referable to the piriformis have been computed tomography–guided injection of the piriformis and palpation of the muscle along with the sciatic nerve from inside the pelvis as they exit the sciatic notch.5, 7, 8 The image-guided injection necessitates the patient being admitted to a radiology department, being disrobed for an injection requiring multiple steps for precise needle placement, and being subjected to some radiation exposure. Palpation of the piriformis from inside the pelvis is performed vaginally or rectally. Comparatively, the diagnostic qualities of an ultrasound injection are that it can be performed in the office, takes just a few moments, and requires no radiation.
The diagnostic and potentially therapeutic values of an injection in the piriformis muscle are both predicated on a technique that provides reliable placement of the medication. The purpose of this report is to describe a reliable, reproducible method for injection of the piriformis (Video 1).
Procedural Technique
The goal of the piriformis injection is to enter the piriformis musculature lateral to the sacrum and superficial to the sciatic nerve. This is performed with the ultrasound transducer in the long axis with the piriformis muscle while maintaining visualization of the piriformis musculature, lateral edge of the sacrum, and sciatic nerve to avoid needle contact with the nerve itself. This is not performed as a nerve block, so the medication is not injected into the nerve sheath but rather into the adjacent musculature.
During the procedure, the patient is in the prone position with the lower extremities in neutral rotation. The patient is positioned so that the feet are just off the edge of the examination table enough so that the rotation of the lower extremity is not affected by the foot. The ultrasound machine is placed on the symptomatic side of the patient and positioned in front of the provider. Our center uses the SonoSite M-Turbo ultrasound system. The ultrasound transducer used for the injection is based on the patient's body habitus, but typically a low-frequency curvilinear transducer is used because of the depth of the piriformis muscle. A lower-frequency linear probe could potentially be used for patients with a small body habitus. Our center uses the SonoSite C60x transducer with a 5-2 MHz bandwidth for most piriformis injections. Prior to the injection, a survey scan of the posterior gluteal muscles and piriformis is performed, visualizing the piriformis gliding beneath the gluteus maximus as the lower extremity is passively internally and externally rotated with the knee in a flexed position. It is helpful to visualize the muscle tissue from the sacrum to the attachment at the superior border of the greater trochanter. The movement of the muscle with rotation, as well as the visualization of the musculature up to the sacrum, helps to differentiate it from other muscles in the area, including the obturator internus. Identifying the sciatic nerve is also important. While the muscle is being visualized in the long axis, the nerve will be in the short axis. It is typically visualized beneath the piriformis when in the prone position but, at times, can be bifurcated, which could require a change in needle positioning. This is also helpful to know for surgical purposes. During this pre-procedure scan, Doppler imaging should be used to locate vessels that will need to be avoided. The anatomic location of smaller vessels can differ from patient to patient, so Doppler assessment is worthwhile to complete during every procedure, especially in patients taking blood thinning medication. Typically, pre-procedure images are recorded, and then the patient can be prepared for the procedure. While these images are being captured, the procedural assistant can set up the supplies and sterile tray (Fig 1).
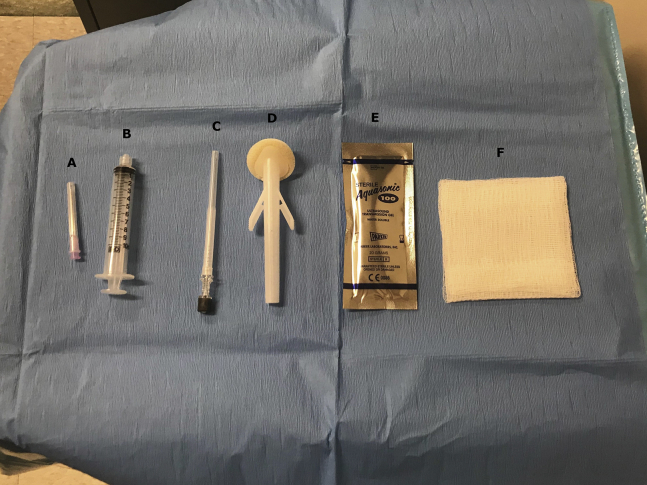
Fig 1.
Sterile tray containing procedure supplies: 1.5-inch 18-gauge needle (A), sterile 10-mL syringe (B), 3.5-inch 22-gauge beveled spinal needle (C), chlorhexidine swab (D), sterile ultrasound gel packet (E), and sterile 4 × 4–inch gauze pad (F).
(All rights are retained by Dr. Byrd.)
Prior to the injection, the patient is draped with aseptic towels or a medical pad. By use of a sterile technique, the patient's posterior gluteal area is sterilized with a chlorhexidine swab, and sterile ultrasound gel is placed over the area that has been sterilized just adjacent to the targeted injection site. Povidone-iodine should be avoided because it can stain the ultrasound transducer. After the medication has been drawn up, the procedural assistant can clean the ultrasound transducer with a germicidal cloth wipe, handing the transducer to the provider so that the ultrasound cord is also wiped down. To do this, the provider pulls the transducer cord through the wipe as the assistant holds the wipe in his or her hand. The provider should check with the manufacturer of the ultrasound system to determine the type of cloth wipes safe for the particular machine and transducer used because these are not all the same. The piriformis is then, once again, visualized in the long axis using the ultrasound transducer so that the lateral border of the sacrum, piriformis muscle, and sciatic nerve can still be visualized (Fig 2). Prior to proceeding with the injection, any excess gel is wiped away using a sterile 4 × 4–inch gauze pad. Once the correct position has been located, ethyl chloride can be sprayed on the skin for anesthetic purposes. This is performed in a manner so that the transducer is not directly in contact with the ethyl chloride because this can damage the transducer. Contact with the needle should also be avoided. Subcutaneous anesthetic is not used in our facility because we are typically using the response to the injection for diagnostic purposes. If the subcutaneous tissue or muscle tissue down to the piriformis is anesthetized, the patient could have improvement that was not related to the piriformis, therefore obscuring the diagnostic value of the procedure. This also prevents the need to stick the patient with a needle twice. Once the patient is prepared, a 3.5-inch 22-gauge sterile spinal needle is inserted bevel up approximately 0.5 to 1 cm from the ultrasound transducer (Fig 3). While maintaining visualization of the needle, the needle can then be inserted in plane with the transducer until it enters the piriformis muscle tissue at the targeted site (Fig 4). The needle trajectory can be adjusted as the needle is inserted to reach the desired location and to avoid the sciatic nerve. When the needle is in the correct position within the muscle, the medication can be injected and visualized entering the tissue (Fig 5). Once the injection is completed, the needle can be removed all while maintaining visualization. After the needle is removed, a small bandage can be applied, and the patient can be mobilized.
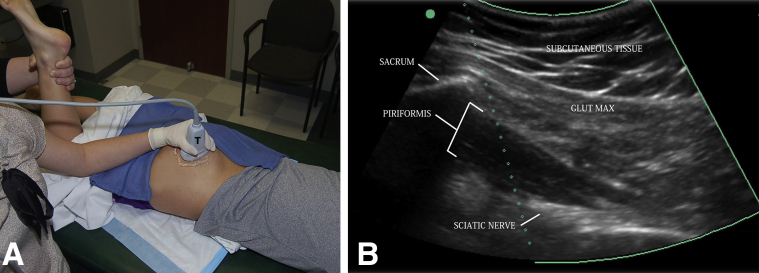
Fig 2.
(A) Inspection of the right piriformis is performed with the patient prone and the transducer (T) placed firmly over the piriformis in the long axis. With the knee flexed, an assistant can internally and externally rotate the leg, allowing visualization of the piriformis in motion throughout the subgluteal space. (B) A long-axis ultrasound image depicts the relation between the subcutaneous tissue, sacrum, gluteus maximus (Glut Max), piriformis, and sciatic nerve.
(All rights are retained by Dr. Byrd.)
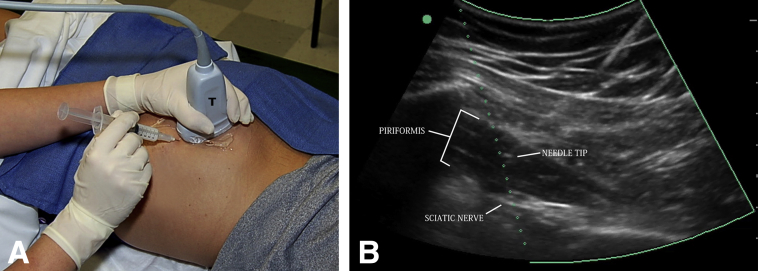
Fig 3.

The needle is placed in plane with the transducer (T), on this right hip. This allows the needle to be visualized throughout its advancement to the piriformis, avoiding the sciatic nerve.
(All rights are retained by Dr. Byrd.)
Fig 4.
(A) The needle is inserted into the musculature of the piriformis, avoiding the sciatic nerve. (T, transducer.) (B) An ultrasound image shows the needle tip entering the piriformis a safe distance from the sciatic nerve.
(All rights are retained by Dr. Byrd.)
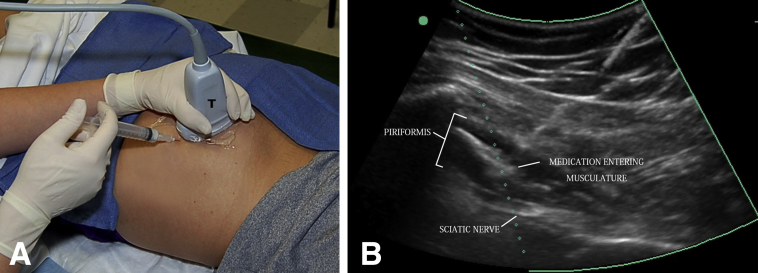
Fig 5.
(A) The medication is injected. (T, transducer.) (B) The medication is visualized entering the muscle tissue of the piriformis.
(All rights are retained by Dr. Byrd.)
Although not necessarily a medical technique, speaking to the patient casually during the procedure can help with the patient's comfort and anxiety level greatly. We find that discussing vacation plans, family, or upcoming social functions works very well. We try to make the patient as comfortable as possible, and creating a relaxed friendly environment goes a long way.
After the injection, the patient can be reassessed to determine how much of his or her overall discomfort was related to the piriformis. This may be achieved through a physical examination or having the patient functionally repeat activities that created symptoms prior to the injection. This ultrasound-guided injection technique can be used for both diagnostic injections of anesthetic and injections of corticosteroid or any other substance deemed appropriate for intra-muscular injection. Depending on what is being injected, the gauge of the needle may need to be adjusted.
After a piriformis injection is performed and tested functionally in the office for diagnostic purposes, the patient is asked to refrain from physical exercise for a specific amount of time, depending on the type of injection. If only anesthetic is injected, the patient may return to baseline activity immediately. At times, immediately after the injection, the patient may have some numbness in the posterior thigh near the buttock. Avoiding the nerve sheath prevents temporary loss of muscle function, but the patient should be monitored for a short period after the injection if driving home. If a corticosteroid is injected, the patient is asked to rest the hip area for 1 week. When physical therapy is recommended, the program can be initiated after the 1 week of rest. The patient may immediately return to activities of daily living outside of exercise with the understanding that there may be some soreness in the musculature for a couple of days.
Discussion
Ultrasound-guided injections are essential in the management of recalcitrant piriformis problems (Tables 1 and 2). The deeply situated anatomy of this small muscle creates technical challenges in both the diagnosis and treatment. Ultrasound is superior to all other available image-guided methods in terms of reliability, simplicity, accessibility, and absence of ionizing radiation.
Table 1.
Advantages and Disadvantages
| Advantages |
| Convenient and cost-effective for patient |
| Less painful than fluoroscopy-guided methods |
| Can avoid need for CT guidance or travel to imaging center |
| Allows for immediate post-injection reassessment and real-time information |
| Can visualize effusion and aspirate if needed |
| No radiation exposure |
| More accurate than landmark injections |
| Disadvantages |
| User dependent |
| Limited by body habitus |
| Upfront cost of ultrasound equipment and supplies |
| Requires time of provider in clinic to perform procedure |
CT, computed tomography.
Table 2.
Pearls and Pitfalls
| When in doubt, use more ultrasound gel. Too much gel may make a mess, but too little can limit image quality. |
| Know your limits. If you are not 100% confident in your ability to reach the piriformis due to body habitus, do not proceed. |
| The transducer should not be pressed into the soft tissues with force. It should sit securely on top of the skin. Downward force can cause compression of the soft tissues and vascular structures, obscuring visibility. |
| The transducer should be held firmly with the fingers around the probe and on the patient's skin. This will prevent the transducer from moving during the procedure, causing loss of visibility. |
| Always check for vascular structures before moving forward with an injection to prevent damage to the vessels and bleeding. |
| Locate the sciatic nerve and maintain visualization throughout the injection to prevent contact with the needle. |
| Optimize the ultrasound image prior to moving forward with an injection using appropriate depth, focal zone, and gain. |
The diagnosis of piriformis syndrome can be elusive. More commonly, the piriformis may be a contributing source of pain and dysfunction in association with other disorders, or it may occur as a compensatory problem that can obscure the principal diagnosis. Many of these problems can be well managed with simple conservative measures; however, when these lesser measures fail, ultrasound-guided injection can be an effective adjunct in both the diagnosis and treatment.
For diagnostic purposes, we use a mixture of short- and long-acting anesthetics. This allows an assessment of the response to the anesthetic within minutes but also provides several hours of anesthetic for the patient to interpret the level of improvement. For example, because sitting is often problematic, the patient can assess whether the car ride home was better than the trip to the office. For therapeutic purposes, cortisone is usually used in conjunction with supervised physical therapy. If the patient experiences a significant response, repeated injections are appropriate. If the response is brief, we have not found that serial injections have been of any added benefit. Even if the response is meaningful, we generally recommend 3 as a limit.
There are no published reports of significant complications associated with the ultrasound method of injecting the piriformis muscle, and we have observed no complications or other untoward effects in performing this procedure. However, there are significant potential concerns: Paramount among these would be injury to the sciatic nerve or inadvertent intravascular injection. It is also plausible that because the injection is not made into a well-contained space, that some anesthetic could filter around the sciatic nerve, resulting in a transient nerve block. The technique detailed here for ultrasound-guided injection of the piriformis is an effective, reliable, reproducible adjunct in the evaluation and treatment of piriformis-related disorders about the hip.
Acknowledgment
The authors acknowledge the invaluable assistance of Ashley Campbell, P.T., D.P.T., S.C.S., C.S.C.S., in the video production; Ashley Civils, L.P.N., in technical matters; and Sharon Parker, B.A. in manuscript preparation.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: J.W.T.B. is a paid speaker/presenter for and receives royalties and research support from Smith & Nephew and receives royalties from Springer. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Real-time, beginning-to-end demonstration of an ultrasound-guided injection in a left piriformis muscle highlighting the details of the methodology.
References
- 1.Byrd J.W.T. Piriformis syndrome. Oper Tech Sports Med. 2005;13:71–79. [Google Scholar]
- 2.Byrd J.W.T. Patient selection and physical examination. In: Byrd J.W.T., editor. Operative hip arthroscopy. Ed 3. Springer; New York: 2013. pp. 7–32. [Google Scholar]
- 3.Byrd J.W.T. Routine arthroscopy and access: Central and peripheral compartments, iliopsoas bursa, peritrochanteric, and subgluteal spaces. In: Byrd J.W.T., editor. Operative hip arthroscopy. Ed 3. Springer; New York: 2013. pp. 131–160. [Google Scholar]
- 4.Martin H.D., Reddy M., Gómez-Hoyos J. Deep gluteal syndrome. J Hip Preserv Surg. 2015;2:99–107. doi: 10.1093/jhps/hnv029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pace J.B., Nagle D. Piriformis syndrome. West J Med. 1976;124:435–439. [PMC free article] [PubMed] [Google Scholar]
- 6.Freiberg A.H., Vinke T.A. Sciatica and the sacroiliac joint. J Bone Joint Surg. 1934;16:126–136. [Google Scholar]
- 7.Rodrique T., Hardy R.W. Diagnosis and treatment of piriformis syndrome. Neurosurg Clin N Am. 2001;12:311–319. [PubMed] [Google Scholar]
- 8.Durrani Z., Winnie A.P. Piriformis muscle syndrome: An underdiagnosed cause of sciatica. J Pain Symptom Manage. 1991;6:374–379. doi: 10.1016/0885-3924(91)90029-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Real-time, beginning-to-end demonstration of an ultrasound-guided injection in a left piriformis muscle highlighting the details of the methodology.