Abstract
Surgical management of patellofemoral instability is technically challenging in skeletally immature patients. Special considerations in this population include activity and sports limitations, recurrence rate, risk of long-term injury to patellofemoral cartilage, and potential for physeal disruption with operative intervention. Numerous procedures have been described to address causative pathoanatomy in the patellofemoral joint, as well as its static and dynamic stabilizers. We describe our technique of combined medial patellofemoral ligament and modified Roux-Goldthwait reconstruction to address both proximal and distal malalignment in a skeletally immature patient with open physes.
Patellofemoral instability (PFI) occurs because of high-risk activities and structural variants of the patellofemoral joint. Normal joint stability relies on structures that work both passively and dynamically to allow for secure motion throughout the knee flexion-extension arc. The medial patellofemoral ligament (MPFL) and lateral retinaculum integrity, trochlear groove, vertical patella positioning, and patella tendon length are factors in the stability of the joint because these impart static structural constraints and dynamic forces that maintain anatomic patella tracking. The MPFL is the primary passive restraint in the first 20° of knee flexion. The trochlear groove accounts for stability in deeper knee flexion after the patella begins to engage the trochlea at 30° of flexion. Ideal patellar height also plays a role in stability, allowing for appropriate engagement with the trochlear groove. In addition to variations in the above described anatomy, generalized ligamentous laxity, increased Q angle, and trochlear dysplasia are recognized risk factors for PFI. Excessive lateral patella tilt caused by iliotibial band and lateral retinaculum contractures and lateral femoral condyle hypoplasia can also impact tracking and stability of the patella.1
In certain cases, PFI is caused by both proximal and distal pathoanatomic alterations. Distally, a large tibial tuberosity to trochlear groove distance (TT-TG) signifies a larger quadriceps vector (Q Angle) and greater lateral displacement force on the patella during knee motion. A TT-TG of greater than 20 mm measured on computed tomography has been shown to be a significant cutoff associated with recurrent patella dislocations and is an indication for surgical intervention. The goal of correction of the TT-TG is 10 to 5 mm. In adults, tibial tubercle osteotomy and realignment is the treatment of choice, although it may not be a viable option with open growth plates, given the location of the tibial tubercle apophysis and significant risk for physeal injury.
After initial traumatic dislocation of the patella or with chronic subluxation, the MPFL becomes incompetent, no longer acting as a restraint to lateral translation. In a skeletally immature patient with any of the aforementioned structural risk factors, surgical correction is recommended, given the high risk of recurrent instability. Options for proximal realignment include MPFL reconstruction, MPFL repair, medial imbrication, and vastus medialis oblique advancement.2 Options of distal realignment procedures are limited due to the open tibial tubercle and proximal tibial physis but include Galeazzi tenodesis, patellar tendon shortening, modified Grammont procedure, and Roux-Goldthwait procedure.1, 3 The Roux-Goldthwait corrects an increased Q angle similar to a tibial tubercle osteotomy, but without threatening the physis.
Indications and Preoperative Planning
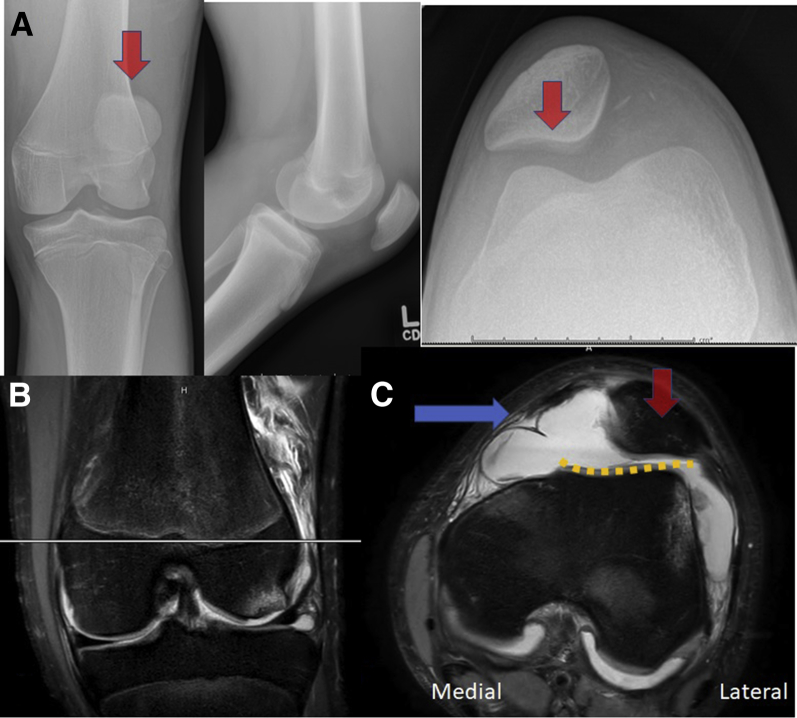
We describe a modified Roux-Goldthwait procedure with allograft MPFL reconstruction for both proximal and distal realignment to address severe PFI in the skeletally immature patient. Patients with recurrent patella instability, either subluxation or dislocation events that lead to pain and limit choice of daily activities, first are recommended a course of nonoperative management. After trials of physical therapy and bracing fail, patients with continued instability are offered surgical correction. Respecting open physes, we chose a combination of a Roux-Goldthwait procedure for distal realignment and an allograft MPFL reconstruction, secured with a suture anchors distal to the physes without threatening growth. Preoperative magnetic resonance imaging is performed (Fig 1) to evaluate concomitant knee pathology such as an MPFL tear, osteochondral defects, loose bodies, and to assess the TT-TG distance, which ideally is less than 15 mm, and if greater than 20 mm is associated with recurrent instability and is an indication for distal corrective realignment.
Fig 1.
Patient’s left side. Preoperative (A) anteroposterior, lateral, merchant radiographs show the lateral sitting patella (red arrow) are magnetic resonance (MR) images (B) coronal cut for cross reference and (C) axial T2-weighted MR images of a skeletally immature male with recurrent patellofemoral dislocation after failure of conservative management. MR demonstrates severe trochlear dysplasia with a shallow trochlear groove (orange dotted line), MPFL tear (blue arrow), lateral patella (red arrow), and significant joint effusion. His tibial tuberosity to trochlear groove distance measured 26 mm, warranting distal realignment.
Surgical Technique
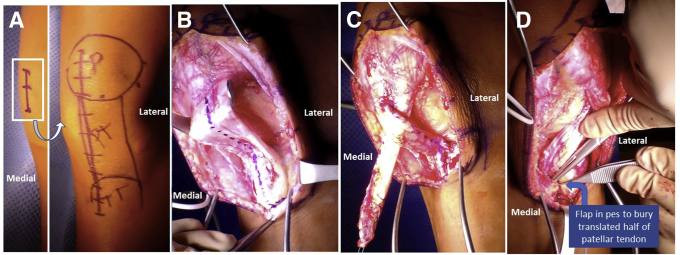
The patient is placed supine on a standard radiolucent operating room table and then induced under general anesthesia. Preoperative landmarks, including the medial epicondyle, patellar poles, patellar tendon borders, and the tibial tubercle, and pre-planned incisions are then marked (Fig 2A, Video 1). A 12-cm midline incision from the tibial tubercle to the inferior pole of the patella is made. The medial and lateral borders of the patellar tendon are identified. With standard anterior medial and anterior lateral arthroscopy portals, diagnostic arthroscopy is performed, and any relevant intra-articular pathology is addressed. Next, a lateral release within the midportion of the lateral retinaculum starting at the superior patella and ending at the lateral portal is performed using cautery. Hemostasis is carefully achieved using electrocautery because hemarthrosis is a known side effect of a lateral release and can lead to painful swelling. Care is taken through each layer to prevent penetration of the subcutaneous layer of the skin and to avoid entering the vastus lateralis tendon.
Fig 2.
Patient's left side. (A) Palpation and marking of anatomic landmarks including the patella, patellar tendon, and tibial tubercle anteriorly with a planned 12 cm midline incision. After exposure, (B) the patellar tendon is marked along the center and split longitudinally with a no. 10 scalpel, and (C) the lateral half is whip-stitched and passed inferomedially to form a “Roux” pattern. (D) A flap is then created in the pes anserinus to bury the free end of the translated lateral half of the patellar tendon to create a new insertion that is distal and medial to the insertion of the middle half.
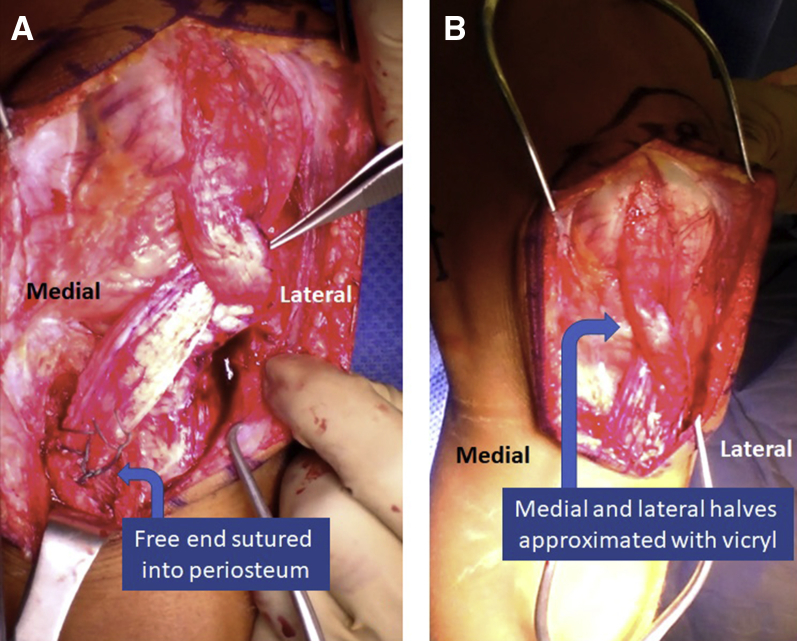
Returning to the open procedure, the central paratenon is split longitudinally and dissected free of the tendon medially and laterally (Fig 2B). Posteriorly the tendon is freed from the fat pad, ensuring complete dissection of the patellar tendon from the inferior pole of the patella to the tibial tubercle. A scalpel is used to divide the patellar tendon into medial and lateral halves. The lateral half of the patellar tendon is subperiosteally dissected off the tibial tubercle. A no. 2 Ethibond suture is placed in locking Krackow fashion into the distal half of the lateral patellar tendon (Fig 2C). The lateral patellar tendon is passed deep to the medial half of the tendon. An “L”-shaped incision is made over the pes anserinus with the transverse arm distal to the tibial physis and the longitudinal arm medial to the tibial tubercle apophysis. Dissection deep to the periosteum (Fig 2D) is performed until distal to the pes anserine tendons. A free needle is placed on the no. 2 Ethibond sutures and passed deep into periosteum and coming out distal to the pes anserine tendons. Use preoperative planning to determine patella height because care should be taken not to overdistalize the tendon. The second arm of the no. 2 Ethibond suture is passed in a similar location in horizontal mattress fashion with an abundant soft tissue bridge. The patellar tendon is now tied deep to the periosteum with a no. 2 Ethibond suture (Fig 3A). Additional Figure-of-8 sutures are placed, securing the transferred patellar tendon to the pes tendons, as well as closure of the “L” split of the pes anserine tendons. A 0-Vicryl suture is used to approximate the medial and lateral halves of the patellar tendon more proximally (Fig 3B).
Fig 3.
Patient's left side. (A) The free end of the tendon is sutured to the periosteum of its attachment site with no. 2 Ethibond, and (B) Vicryl sutures are used to approximate the medial and lateral halves of the patellar tendon proximally.
The following step is the MPFL reconstruction, which can be done using the surgeon's preferred technique and method of fixation, taking care to avoid damage to the medial distal femoral physis by using fluoroscopic guidance to place the femoral fixation distal to the distal femoral physis anterior to Blumensaat's line at Schottle's point. These authors' preferred technique is all suture anchor fixation in the patella using a Smith and Nephew Q-Fix Mini (Andover, MA) and a double-loaded 2.9 Osteoraptor for femoral fixation. Semi-tendonosis or Tibials Anterior allograft is routinely used for MPFL reconstruction. After the MPFL reconstruction, patella positioning is confirmed to be centralized, with range of motion no longer allowing for lateral translation of the patella. There should be a negative J sign. Range of motion from 0° to 60° of flexion should not tension the Roux-Goldthwait reconstruction. Irrigation, closure, and local anesthetic injection is performed before final dressings, and a hinged knee brace is fitted. After surgery, we keep the patient partial weightbearing with crutches for 6 weeks with restricted range of motion from 0° to 50° for the first 3 weeks, then advance to 0° to 90° per protocol.
Discussion
Risk factors for PFI include variations in patient anatomy that can be corrected surgically when rehabilitation, supportive bracing, and periods of immobilization that fail to diminish the patella instability. Careful assessment of anatomic and patient-related risk factors for recurrence should be completed. A combined proximal and distal realignment, such as MPFL reconstruction with modified Roux-Goldthwait, may provide superior results in high-risk, skeletally immature athletes.
Because of concern for physeal damage, surgical techniques to treat PFI in skeletally immature patients rely primarily on soft tissue procedures. The authors prefer a combination of a modified Roux-Goldthwait and an MPFL reconstruction to treat severe PFI with recurrent dislocation and elevated TT-TG distance (Tables 1 and 2). With the Roux-Goldthwait technique, the surgeon can medialize and distalize the patella to improve tracking similar to what would be achieved with Trillat, Maquet, and Fulkerson osteotomies without risk for physeal disruption. Critics of the Roux-Goldthwait express concern over the increased rotation and tilt of the patella that remains uncorrected with this procedure. The addition of the MPFL reconstruction corrects this lateral rotation and tilt while providing a second restraint to lateral translation.4 In our clinical experience, our patients have not experienced problems related to malrotation of the patella. Likewise, the need for revision surgery after combined MPFL and Roux-Goldthwait procedures has yet to be seen in our clinic.
Table 1.
Pearls and Pitfalls of the Modified Roux-Goldthwait Procedure
| Pearls |
| Lateral tendon subperiosteal release; to ensure periosteal to bone healing when transferred |
| Attachment of tendon distal to proximal tibia physis and medial to tibial tubercle apophysis |
| Ensure complete mobilization of patella tendon, inferior pole of patella to superior aspect of tibial tubercle |
| MPFL femoral attachment is at Schottle's Point just distal to femoral physis |
| Pitfalls |
| Improper hemostasis during lateral release, can lead to knee hemarthrosis and painful swelling |
| Ensure tendon is released from insertion subperiosteally and not through the tendon, which would potentially limit healing potential |
| Breach of anterior cortex during patella fixation could cause potential stress riser or fracture |
| MPFL femoral attachment placed at or proximal to femoral physis could potentially cause growth arrest |
| Ensure early but limited ROM to protect patella tendon transfer |
| Ensure early PT for quad activation to prevent quad atrophy |
MPFL, medial patellofemoral ligament; PT, physical therapy; ROM, range of motion.
Table 2.
Advantages and Disadvantages of the Modified Roux-Goldthwait Procedure
| Advantages |
| Physeal sparing option for Q angle realignment, instead of a tibial tubercle osteotomy |
| Greater correction |
| Adjustable correction |
| Strong fixation while only detaching half of PT |
| Does not require additional tendon sacrifice (hamstrings spared) |
| No implanted hardware, and therefore no secondary surgeries for hardware removal |
| Disadvantages |
| Distalizing patellar tendon attachment increases patellofemoral joint contact pressures; if too high could lead to early OA |
| Concern of malrotation of patella after tendon transfer |
| Potential for incomplete correction due to young age of patient, leading to possibility of future revision surgery |
| Large anterior scar |
OA, Osteoarthritis; PT, physical therapy.
Given the variation in proposed techniques, outcomes-based literature has been limited primarily to case series. The original Roux-Goldthwait procedure was described in the late 1800s with multiple surgeon-specific modifications and additions reported since, including lateral release, medial reefing/combination, vastus medialis advancement, and adjuvant patellar tendon transfers.5 Chrisman et al.6 reported 93% satisfactory results with a Roux-Goldthwait procedure in their series of skeletally immature patients. More recently, Marsh et al.7 also reported excellent results in 26 of 30 cases and a high rate of return to normal physical activity. However, studies have not consistently shown superior outcomes with one technique over another likely attributable to heterogenous techniques and reporting. No high-level evidence studies are available on this topic. In their recent systematic review of more than 1000 cases, Longo et al.8 found most distal realignment procedures were successful in correcting PFI. They reported an overall recurrence rate of 7% after analyzing various distal realignment procedures, including tibial tubercle transfer with and without proximal realignment, Elmslie-Trillat, Roux-Goldthwait, Goldthwait with and without lateral release, Fulkerson, modified Grammont, and various combinations of above procedures, suggesting that the various techniques as reported in the 38 articles that met their inclusion criteria for follow-up appear to be similarly efficacious.8
The assorted procedures, although successful in managing PFI, have several complications specific to the nature of each surgery. Patellofemoral osteoarthritis has been reported with procedures that increase the joint contact pressures, symptomatic hardware requiring subsequent removal with procedures involving prominent screws, wound complications, patella or proximal tibia fractures, arthrofibrosis and limited range of motion, neuroma, deep vein thrombosis, and peroneal nerve palsies have all been reported.1, 8 In the procedures reviewed, complications have been reported to range from 0% to 7% for distal realignment procedures, depending on the specific surgery performed, and up to 26% for proximal, mainly MPFL reconstructive procedures.1, 8
In conclusion, in skeletally immature patients, where an MPFL reconstruction alone would not suffice because of the anatomic risk factors predisposing the patient to recurrent PFI, a physeal-sparing distal realignment procedure should be performed. We recommend using a Roux-Goldthwait correction in combination with a double bundle allograft MPFL reconstruction and lateral release to properly balance the knee and maintain patella tracking through the range-of-motion arc.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Surgical video demonstrates the technique for a modified Roux-Goldthwait procedure in a skeletally immature patient with open physes. Patient's left side. The video focuses on the Roux-Goldthwait portion of the procedure; however, this is performed in conjunction first with a diagnostic arthroscopy and lateral retinacular release, and ultimately with a medial patellofemoral ligament reconstruction using a semitendinosus allograft for both proximal and distal realignment.
References
- 1.Gausden E.B., Fabricant P.D., Taylor S.A. Medial patellofemoral reconstruction in children and adolescents. JBJS Rev. 2015;3(10) doi: 10.2106/JBJS.RVW.N.00091. [DOI] [PubMed] [Google Scholar]
- 2.Panni A.S., Cerciello S., Vasso M. Patellofemoral instability: Surgical treatment of soft tissues. Joints. 2013;1:34–39. [PMC free article] [PubMed] [Google Scholar]
- 3.Kraus T., Lidder S., Švehlík M. Patella re-alignment in children with a modified Grammont technique. Acta Orthop. 2012;83:504–510. doi: 10.3109/17453674.2012.736168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arshi A., Cohen J.R., Wang J.C., Hame S.L., McAllister D.R., Jones K.J. Operative management of patellar instability in the United States: An evaluation of national practice patterns, surgical trends, and complications. Orthop J Sport Med. 2016;4 doi: 10.1177/2325967116662873. 2325967116662873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marcacci M., Zaffagnini S., Iacono F., Visani A., Petitto A., Neri N.P. Results in the treatment of recurrent dislocation of the patella after 30 years’ follow-up. Knee Surg Sports Traumatol Arthrosc. 1995;3:163–166. doi: 10.1007/BF01565476. [DOI] [PubMed] [Google Scholar]
- 6.Chrisman O.D., Snook G.A., Wilson T.C. A long-term prospective study of the Hauser and Roux-Goldthwait procedures for recurrent patellar dislocation. Clin Orthop Relat Res. 1979;144:27–30. [PubMed] [Google Scholar]
- 7.Marsh J.S., Daigneault J.P., Sethi P., Polzhofer G.K. Treatment of Recurrent Patellar Instability with a Modification of the Roux-Goldthwait Technique. J Pediatr Orthop. 2006;26:461–465. doi: 10.1097/01.bpo.0000217711.34492.48. [DOI] [PubMed] [Google Scholar]
- 8.Longo U.G., Rizzello G., Ciuffreda M. Elmslie-Trillat, Maquet, Fulkerson, Roux Goldthwait, and other distal realignment procedures for the management of patellar dislocation: Systematic review and quantitative synthesis of the literature. Arthroscopy. 2016;32:929–943. doi: 10.1016/j.arthro.2015.10.019. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Surgical video demonstrates the technique for a modified Roux-Goldthwait procedure in a skeletally immature patient with open physes. Patient's left side. The video focuses on the Roux-Goldthwait portion of the procedure; however, this is performed in conjunction first with a diagnostic arthroscopy and lateral retinacular release, and ultimately with a medial patellofemoral ligament reconstruction using a semitendinosus allograft for both proximal and distal realignment.