Abstract
The posterolateral corner of the knee is composed of the fibular collateral ligament, popliteus tendon, and popliteofibular ligament, which provide varus and rotational stability to the knee. An anatomic technique reconstructs these structures through 2 femoral sockets and 1 tibial and 1 fibular tunnel. This reconstruction can be performed using a peroneus longus autograft that is prepared as a Y construct. The peroneus longus autograft is preferred because it provides adequate length and diameter for the entire reconstruction. Initially, the doubled loop of the Y is passed into the tibial tunnel and fixed with an adjustable cortical button. The shorter limb of the Y is used for reconstruction of the popliteus tendon. The longer limb of the Y is passed from posterior to anterior through the fibular tunnel and is fixed in the tunnel with an interference screw to re-create the popliteofibular ligament. The remaining graft is then shuttled deep to the iliotibial band and superficial to the popliteus tendon, into the femoral socket, to re-create the fibular collateral ligament.
The posterolateral corner (PLC) of the knee was once an area that was poorly understood and much feared by surgeons. However, the seminal work by LaPrade et al.1 has helped resolve much of the confusion on the anatomy and biomechanical function of this area. The 3 main structures of the PLC are the fibular collateral ligament (FCL), popliteus tendon (PT), and popliteofibular ligament (PFL). Although the FCL is the primary restraint to varus at lower flexion angles, the PT is the principal external rotation stabilizer at higher flexion angles and the PFL stabilizes the knee in internal rotation.2, 3, 4 The overwhelming majority of PLC injuries occur in a multiligament instability scenario, in association with anterior cruciate ligament or posterior cruciate ligament (PCL) tears. Recognition of this injury by clinical examination or on imaging is critical not just for restoration of normal knee biomechanics but also for the impact it has on other ligament reconstructions.5, 6
The original technique for anatomic reconstruction of the FCL, PT, and PFL described by LaPrade et al.7 used a split Achilles tendon allograft. The ability of this reconstruction to restore knee stability and improve functional outcomes has also been reported.8 The availability, cost, and quality of tendon allograft are an issue. A similar technique has been described with successful results when performed using hamstring autograft as well.9 This, however, requires the harvest of 2 separate hamstring tendon autografts.
We present our technique of anatomic PLC reconstruction using a single peroneus longus (PL) tendon autograft. A graft length of 25 to 28 cm is adequate for the entire reconstruction, thus sparing the hamstrings to be used for another intra- or extra-articular reconstruction.
Diagnosis and Indication for Surgery
It is essential to confirm the diagnosis of a grade 3 PLC injury to devise a surgical plan for managing the grafts, sequence of surgery, and execution. Clinical examination relies on tests such as the varus stress test, dial test, extension recurvatum test, and reverse pivot-shift test.3 Bilateral varus stress radiographs in 20° of knee flexion can confirm a grade 3 tear when the side-to-side difference in the lateral opening is more than 4 mm.10 In chronic cases, obtaining a long-leg anteroposterior scanogram is helpful to identify varus malalignment, which must be corrected prior to a ligament reconstruction.11 Magnetic resonance imaging is an important tool to identify the exact structures that might be injured (Fig 1). The most reliable arthroscopic sign to injured PLC structures in the presence of the lateral drive-through sign (Fig 2).
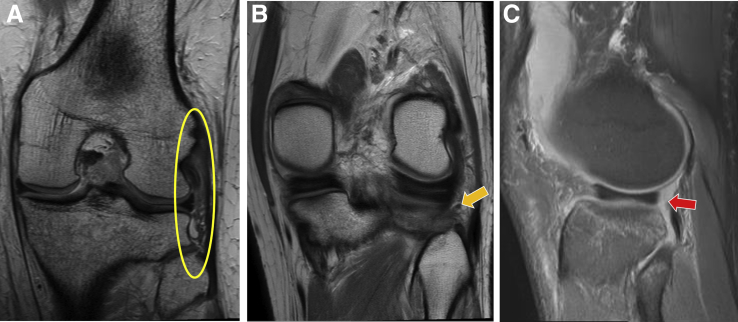
Fig 1.
Magnetic resonance imaging scan of left knee. (A) The fibular collateral ligament and popliteus tendon injury is seen as hyperintensity and waviness of fibers (oval) on the T2-weighted coronal image. (B) A more posterior T2 coronal section shows disruption of the popliteofibular ligament (arrow). (C) The meniscopopliteal fibers are injured, as seen as an area of hyperintensity on the proton density fat-saturated sagittal image (arrow).
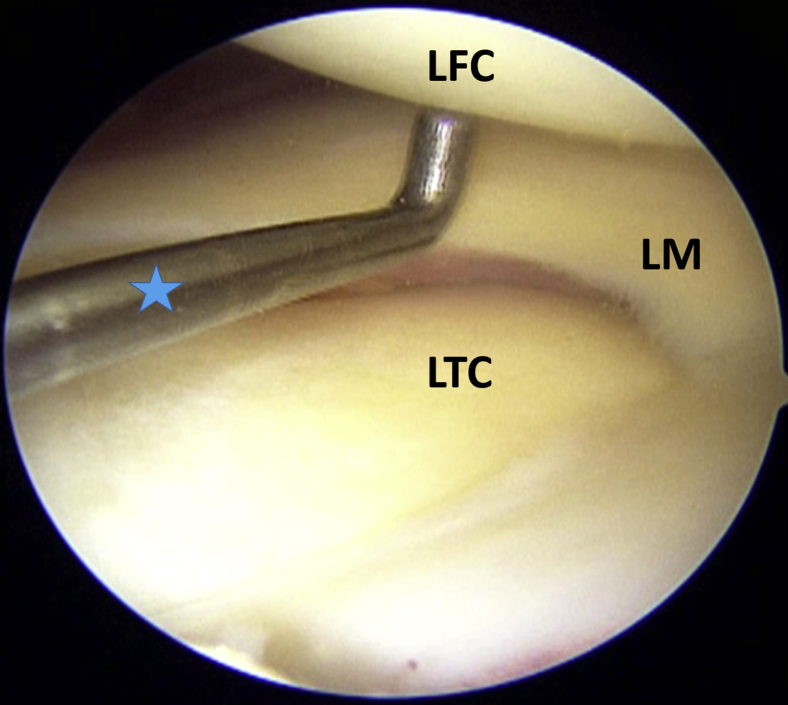
Fig 2.
Arthroscopic drive-through sign. A left knee, placed in a figure-of-4 position, is viewed from the anterolateral portal with a 30° arthroscope and instrumentation from the standard anteromedial portal. The portion beyond the elbow of the hook probe (star) is 4 mm in length and can be seen to be easily driven into the lateral compartment as it opens up owing to the injured structures of the posterolateral corner. (LFC, lateral femoral condyle; LM, lateral meniscus; LTC, lateral tibial condyle.)
Surgical Technique
The entire surgical technique is described in Video 1. The case presented here underwent an anatomic PLC reconstruction of the left knee.
Position
The patient is positioned supine on the operating table, and a high thigh tourniquet is applied with adequate padding. Foot support is placed with 90° of knee flexion, and a lateral thigh support is applied. A detailed examination under anesthesia is performed. The limb is prepared and draped in standard fashion.
Graft Harvest and Preparation
The PL tendon is harvested from the same side using a small, 2- to 3-cm longitudinal incision made just posterior to the lateral malleolus, and the peroneal fascia is dissected off. The PL tendon is the one that lies more posterior and is easily delivered out. The distal end of the tendon is cut 1 cm from the proximal margin of the peroneal retinaculum, and the end is sutured to aid is harvesting with a tendon stripper (Fig 3). The graft obtained must be 25 to 26 cm long (as is usually the case). The PL tendon is usually thick enough to provide a sturdy reconstruction. The muscle is cleaned off the tendon, and the graft is prepared in the manner described in Figure 4 to obtain a Y configuration. The minimal length required for this technique is 250 mm. The graft is marked at 25 mm from the distal tip (mark 1), then at 45 mm from the previous mark (mark 2), and finally at 25 mm from the second mark (mark 3). The segment between the distal end of the graft and mark 1 is whipstitched with No. 2 FiberWire (Arthrex, Naples, FL), and the loop of the TightRope RT (Arthrex) is placed at mark 3. A length of 25 mm of looped graft around the TightRope RT loop is then sutured to prevent slippage from the loop. The final prepared Y graft construct has a distal 25 mm for insertion into the femur popliteus socket, a 45-mm-long segment for the PT, a looped 25-mm segment for the tibial tunnel insertion of the popliteus and PFL, and a longer graft segment to be used for the PFL and FCL reconstruction. The shorter limb will be used for popliteus reconstruction based on the fact that the PT is about 43 mm in length.12
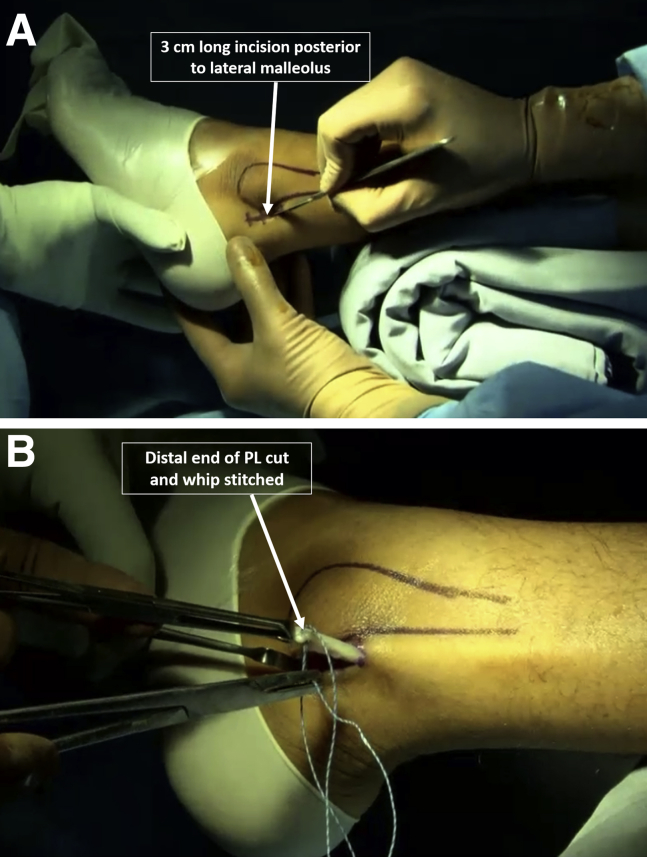
Fig 3.
Peroneus longus (PL) tendon harvest. A left ankle is viewed from the left side. (A) A 3-cm longitudinal incision is made just posterior to the lateral malleolus, and the peroneal fascia is dissected off. The PL tendon is the one that lies more posterior and is easily delivered out. (B) The distal end of the tendon is cut 1 cm from the proximal margin of the peroneal retinaculum, and the end is sutured to aid is harvesting with a tendon stripper.
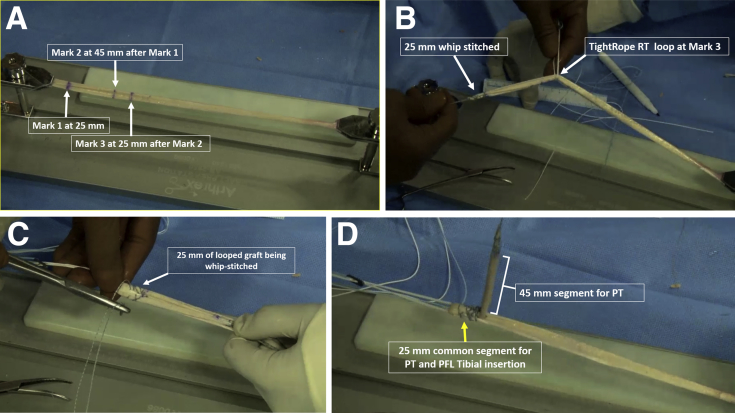
Fig 4.
Y configuration graft preparation. (A) The harvested peroneus longus tendon is cleaned and laid out on a graft preparation board. The minimal length required for this technique is 250 mm. The graft is marked at 25 mm from the distal tip (mark 1), then at 45 mm from the previous mark (mark 2), and finally at 25 mm from the second mark (mark 3). (B) The segment between the distal end of the graft and mark 1 is whipstitched with No. 2 FiberWire, and the loop of the TightRope RT is placed at mark 3. (C) A length of 25 mm of looped graft around the TightRope RT loop is sutured to prevent slippage from the loop. (D) The final prepared Y graft construct has a distal 25 mm for insertion into the femur popliteus socket, a 45-mm-long segment for the popliteus tendon (PT), a looped 25-mm segment for the tibial tunnel insertion of the popliteus and popliteofibular ligament (PFL), and a longer graft segment to be used for the popliteofibular and fibular collateral ligament reconstruction.
Surgical Dissection
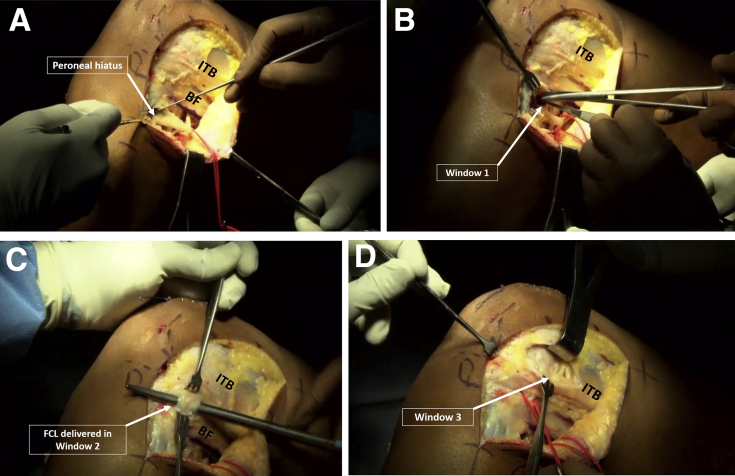
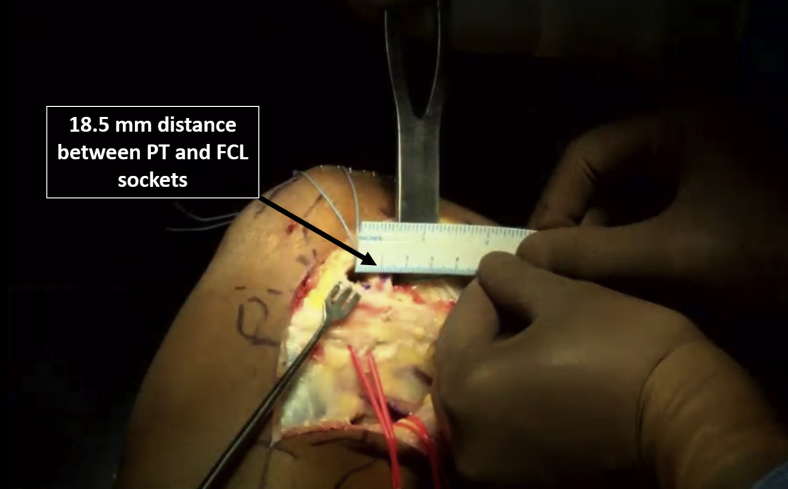
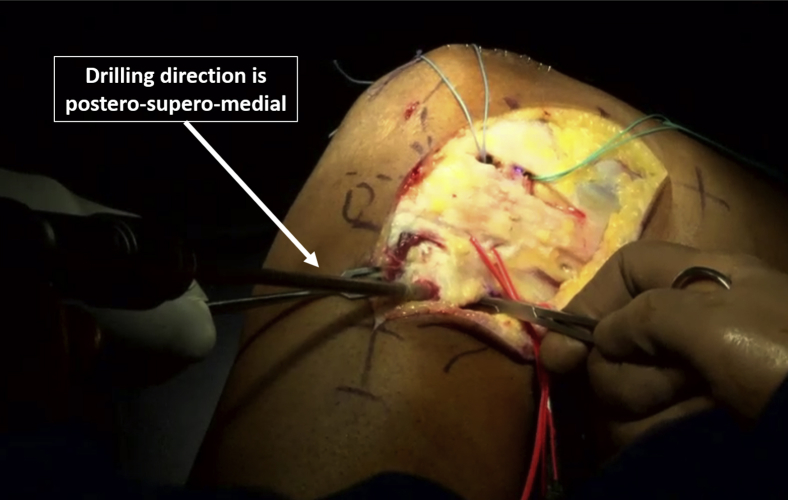
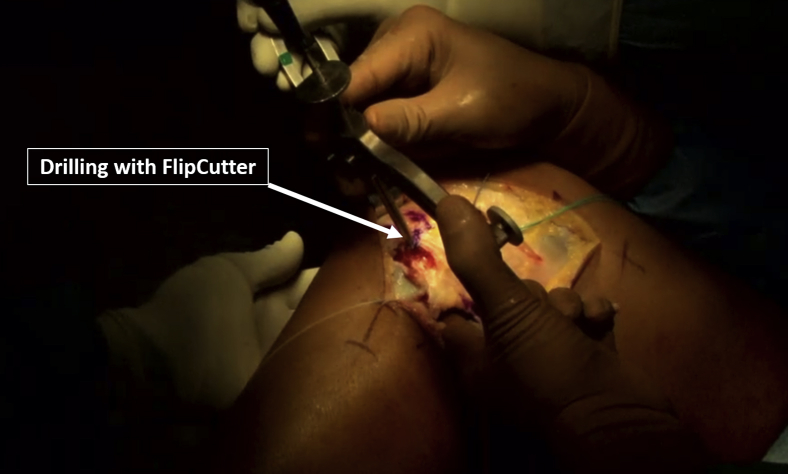
Surgical dissection must be performed prior to arthroscopy to avoid fluid extravasation, unless the diagnosis is in doubt. A 15-cm-long longitudinal incision, extending from 3 cm proximal to the lateral epicondyle of the femur to 5 cm distal to the fibular styloid, is made, with the knee in extension. As the knee is flexed, the incision becomes curvilinear. Full-thickness fasciocutaneous flaps are developed. The first step is to perform a common peroneal nerve neurolysis as described in Figure 5. The neurolysis must be performed extending from the peroneal hiatus in the PL muscle distally, up to a distance of 6 cm proximally. Three soft-tissue windows are created to access sites for bone socket drilling. Window 1 is created through the peroneal fascia posterior to the fibula styloid and extending medially to access the posterior tibial popliteus sulcus, about 1 cm distal to the joint line. Window 2 is created between the biceps femoris tendon and iliotibial band, and the FCL is visualized here. Window 3 is created by longitudinally incising the iliotibial band to access the lateral aspect of the femoral condyle. The lateral epicondyle and popliteus sulcus need to be identified here. The femoral insertions of the FCL and PT are identified in window 3. The FCL socket is created using a 7-mm reamer, up to a depth of 25 mm, at a point 1.4 mm proximal and 3.1 mm distal to the lateral epicondyle. Similarly, a 7 × 25–mm socket is created for the PT insertion at the proximal fifth of the popliteus sulcus. There must be an adequate bone bridge between the 2 sockets, and the distance between their centers is about 18.5 mm (Fig 6). The fibula is drilled next; this can be performed using a jig, but freehand drilling is our preferred technique. The starting point for the drill pin is at the FCL insertion on the anterolateral aspect of the fibular styloid, about 28 mm distal to the tip. The direction is posterior-superior-medial to reach the fibular insertion of the popliteofibular ligament. When the drill is directed 50° externally rotated from the midline and 60° cephalad with respect to the joint line, the tunnel created is anatomic and is in the best available bone, as described by Wechter et al.13 Tunnel drilling is performed with a 6-mm reamer because of the limited space available and for fracture prevention (Fig 7). Finally, the tibia is drilled to accommodate the doubled limb of the Y graft, which is usually 8 mm in diameter. The tibial socket is thus created using an 8-mm FlipCutter (Arthrex). A PCL Femur Jig (Arthrex) is placed at the posterior tibial popliteus sulcus, 1 cm distal to the joint line, accessed from window 1. The entry is from a point just distal and medial to the Gerdy tubercle, which is a flat area. Retro-drilling is performed for a distance of 28 to 30 mm after ensuring that the stepped drill sleeve is tapped in anteriorly and the flipped drill tip is sitting against the posterior cortex to prevent inadvertent blowout anteriorly (Fig 8).
Fig 5.
Common peroneal nerve neurolysis and creation of soft-tissue windows. A left knee is viewed from the left side. (A) The first step in dissection of the lateral side of the knee is to perform a careful common peroneal nerve neurolysis extending from the peroneal hiatus in the peroneus longus muscle distally, up to a distance of 6 cm proximally. (B) Window 1 is created through the peroneal fascia posterior to the fibula styloid and extending medially to access the posterior tibial popliteus sulcus, about 1 cm distal to the joint line. (C) Window 2 is created between the biceps femoris tendon (BF) and iliotibial band, and the fibular collateral ligament (FCL) is visualized here. (D) Window 3 is created by longitudinally incising the iliotibial band (ITB) to access the lateral aspect of the femoral condyle. The lateral epicondyle and popliteus sulcus need to be identified here.
Fig 6.
Femoral socket creation. A left knee is viewed from the left side. The fibular collateral ligament (FCL) socket is created using a 7-mm reamer, up to a depth of 25 mm, at a point 1.4 mm proximal and 3.1 mm distal to the lateral epicondyle. Similarly, a 7 × 25–mm socket is created for the popliteus tendon (PT) insertion at the proximal fifth of the popliteus sulcus. There must be an adequate bone bridge between the 2 sockets, and the distance between their centers is about 18.5 mm.
Fig 7.
Fibular tunnel drilling. A left knee is viewed from the left side. The starting point for the drill pin is at the fibular collateral ligament insertion on the anterolateral aspect of the fibular styloid, about 28 mm distal to the tip. The direction is posterior-superior-medial to reach the fibular insertion of the popliteofibular ligament. When the drill is directed 50° externally rotated from the midline and 60° cephalad with respect to the joint line, the tunnel created is anatomic and is in the best available bone. Tunnel drilling is performed with a 6-mm reamer because of the limited space available and for fracture prevention.
Fig 8.
Tibial socket creation. A left knee is viewed from the left side. The tibial socket is created using an 8-mm FlipCutter, which is the same as the diameter of the looped portion of the graft. A PCL Femur Jig is placed at the posterior tibial popliteus sulcus, 1 cm distal to the joint line. The entry is from a point just distal and medial to the Gerdy tubercle, which is a flat area. Retro-drilling is performed for a distance of 28 to 30 mm after ensuring that the stepped drill sleeve is tapped in anteriorly and the flipped tip is against the posterior cortex to prevent inadvertent blowout anteriorly.
Graft Passage and Fixation
The graft is fixed in the tibia first. The sutures of the TightRope RT, which contains 25 mm of the looped portion of the graft, is shuttled from posterior to anterior in the tibial socket over a suture loop. The graft is pulled so that the TightRope RT button sits flat on the tibia; then, 25 mm of the looped graft, which has previously been sutured, is inserted into the tibial socket by cinching the TightRope RT loop sutures (Fig 9). The shorter limb of the Y graft meant for popliteus reconstruction is passed deep to the IT band, dunked into the popliteus femoral socket, and fixed with a 7 × 23–mm BioComposite screw (Arthrex), keeping the knee in 90° of flexion and 5° of internal rotation with a valgus force applied (Fig 10). The popliteofibular ligament is reconstructed next. The longer limb of the Y graft is shuttled through the fibular tunnel from posterior to anterior over a suture loop. The knee is kept in 90° of flexion, traction is applied to the graft, and fixation is performed with a 6 × 23–mm BioComposite screw in the anterior-posterior direction while a valgus force is applied to the knee (Fig 11). The remaining length of the graft is used to reconstruct the FCL. The graft is shuttled deep to the iliotibial band but superficial to the PT graft to reach the femoral FCL socket. The graft is marked at 25 mm and sutured with No. 2 FiberWire, and excess graft length can be discarded. This end of the graft is inserted into the FCL femoral socket, and fixation is achieved with a 7 × 23–mm BioComposite interference screw while traction is applied to the graft and the knee is kept in 30° of flexion with application of a valgus force (Fig 12). The TightRope RT can finally be re-tensioned to remove any creep in the PT or PFL segments. The final reconstruction is as shown in Figure 13.
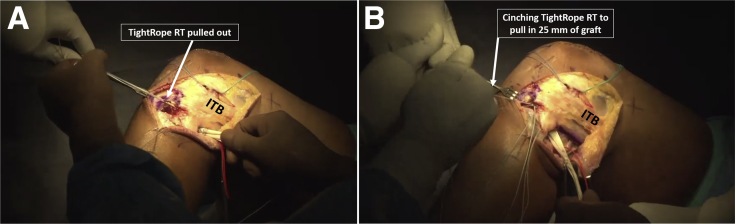
Fig 9.
Tibial fixation with TightRope RT. A left knee is viewed from the left side. (A) The sutures of the TightRope RT are shuttled from posterior to anterior in the tibial socket over a suture loop. (B) The graft is pulled so that the TightRope RT button sits flat on the tibia; then, 25 mm of the looped graft, which has previously been sutured, is inserted into the tibial socket by cinching the TightRope RT loop sutures. (ITB, iliotibial band.)
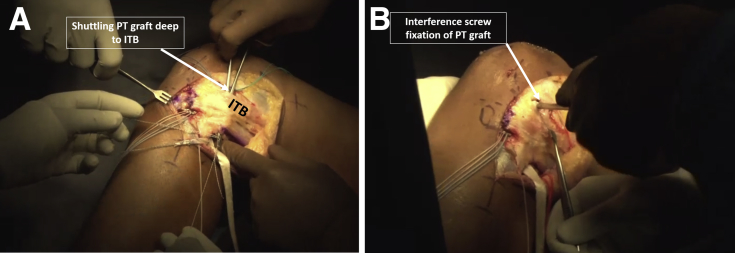
Fig 10.
Popliteus tendon (PT) graft passage and fixation. A left knee is viewed from the left side. (A) The shorter limb of the Y graft is passed deep to the iliotibial band (ITB), and the end is inserted into the femoral socket for the popliteus socket using a suture loop. (B) Fixation is performed with a 7 × 23–mm BioComposite interference screw while traction is applied to the graft and the knee is kept in 90° of flexion and 5° of internal rotation with application of a valgus force.
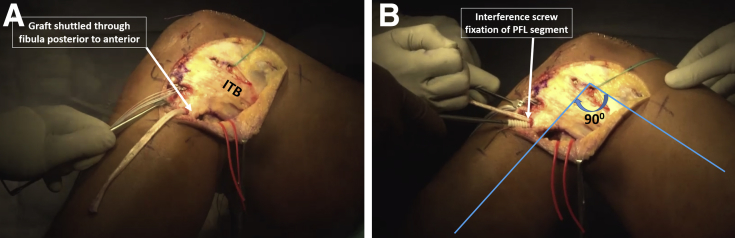
Fig 11.
Popliteofibular ligament (PFL) reconstruction. A left knee is viewed from the left side. (A) The longer limb of the graft is passed through the fibular tunnel from posterior to anterior using a suture loop. (B) Fixation is performed with a 6 × 23–mm BioComposite interference screw passed from anterior to posterior while traction is applied to the graft and the knee is kept in 90° of flexion with application of a valgus force. (ITB, iliotibial band.)
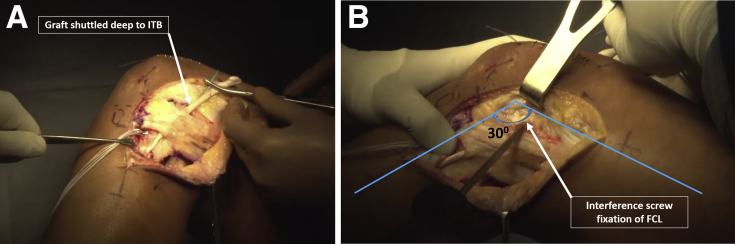
Fig 12.
Fibular collateral ligament (FCL) reconstruction. A left knee is viewed from the left side. (A) The remaining graft is shuttled deep to the iliotibial band (ITB) but superficial to the popliteus tendon graft to reach the femoral FCL socket. The graft is marked at 25 mm and sutured with No. 2 FiberWire, and excess graft length can be discarded. (B) This end of the graft is inserted into the femoral socket, and fixation is achieved with a 7 × 23–mm BioComposite interference screw while traction is applied to the graft and the knee is kept in 30° of flexion with application of a valgus force.
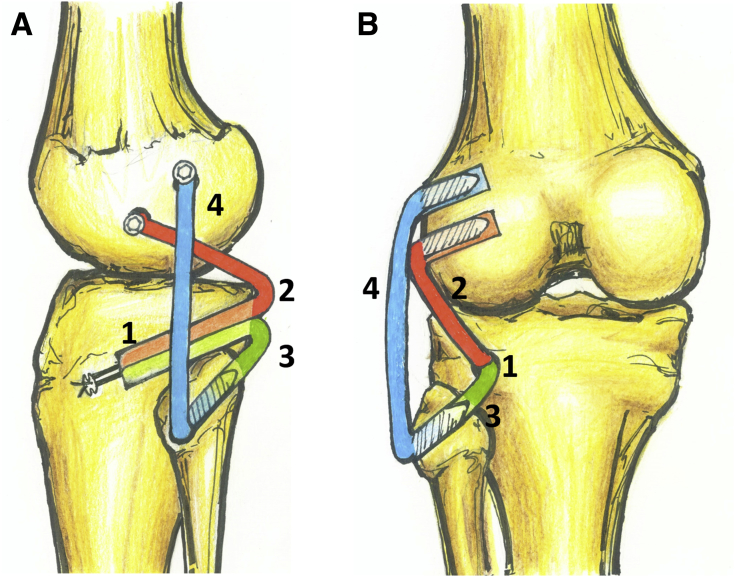
Fig 13.
Sequence of completed reconstruction. (A) Lateral view of left knee. The common looped graft segment is fixed in the tibia first, followed by the popliteus tendon graft (red) in the femur, the popliteofibular ligament graft (green) in the fibula, and finally, the fibular collateral ligament graft (blue) in the femur. (B) Posterior view of left knee showing completed reconstruction with the sequence of graft passage and fixation (1, 2, 3, and 4).
Rehabilitation
The early stage of rehabilitation focuses on reduction of swelling and pain, as well as restoration of muscle activity. Cryotherapy and static exercises are commenced immediately. Weight-bearing and range-of-motion restrictions are guided by concomitant ligament and meniscus surgery. In general, partial weight bearing with a brace and knee bending up to 90° is allowed, unless a simultaneous PCL reconstruction or meniscus root repair is performed, when non–weight bearing becomes imperative. Gradual progression to strength and proprioception training and open kinetic chain exercises at 6 to 8 weeks is begun. Resumption of sports activities is usually delayed until 8 to 9 months.
Discussion
The described technique of anatomic reconstruction is based on the anatomic landmarks and technique described by LaPrade et al.7 but with significant modifications. Our preference is to use the autologous PL tendon, which has proved to be an excellent graft in knee anterior cruciate ligament surgery.14 It is easy to harvest and provides a good working length and sufficient diameter for a strong reconstruction with minimal donor-site morbidity.
PLC reconstruction is usually performed as part of a multiligament reconstruction, and a limitation of autograft presents a dilemma to the surgeon, especially when there is a concern of not using the contralateral limb for graft harvest. However, if the length of the PL is less than 25 cm, an additional graft such as gracilis or semitendinosus tendon graft must be used as well.
The sequence of graft passage and fixation is basically the reverse of the description of LaPrade et al.7 but does ensure plenty of graft in the bone sockets for healing. Suspensory fixation of the graft in the tibia is probably better because it allows superior healing, withoutcompromising the fixation strength.15 The biomechanical principles of reconstruction of each limb, that is, the FCL, PT, and PFL, can be adhered to because each segment can be tensioned and fixed independently. More important, an adjustable loop allows re-tensioning of the PT and PFL segments that can elongate owing to creep while cycling the knee.
The technical pearls and pitfalls are described in Table 1. The described technique does have some limitations; these are described in Table 2. In conclusion, our technique of anatomic PLC reconstruction can be performed with a Y construct of a single tendon autograft and still allow independent tensioning and fixation of each of the segments.
Table 1.
Pearls and Pitfalls
| Description | |
|---|---|
| Pearls | |
| Graft harvesting | The PL tendon lies posterior to the peroneus brevis at this location as described. Although the PL can be easily delivered out after incising the fascia, the peroneus brevis has muscle attached and this helps identify the correct tendon. |
| Graft preparation | The tendon graft must be sutured with a high-strength suture material only (e.g., No. 2 FiberWire). The interference screw fixation in the femur can cause graft laceration, and the presence of such suture material will provide protection from this complication. |
| Surgical approach | Making a liberal incision and raising a full-thickness fasciocutaneous flap prevent wound complications. |
| Performing a common peroneal nerve neurolysis prior to drilling the tunnels is a sine qua non. | |
| Drilling the fibula can be tricky, but freehand passage of a 2.4-mm drill pin keeping the 50°/60° trajectory ensures the best bone. | |
| Intra-articular work such as femoral drilling for ACL reconstruction should be performed after the lateral dissection to avoid distortion of tissue planes due to fluid extravasation. | |
| The femoral drilling for an ACL reconstruction can be performed in an outside-in manner to prevent graft coalition. | |
| Graft passage | The common PT/PFL segment must be marked at 25 mm, and only so much of the graft must be pulled into the tibial tunnel. |
| The tunnel edges in the femur, tibia, and fibula must be chamfered with a rasp to prevent graft abrasion. | |
| Graft fixation | The distal end of the PL tendon is tubular like the PT, and this must be used for PT reconstruction in the femur. |
| The fixation of the PT and PFL must be achieved in 90° of knee flexion and 5° of internal rotation with a valgus force. | |
| Re-tensioning of the TightRope RT button at 80° to 90° of knee flexion will ensure that the PT and PFL segments in the tibia do not have any residual slack. | |
| Pitfalls | |
| Graft harvesting | The harvested PL tendon must be at least 25 cm in length. If this is not the case, as can be possible in very small individuals, the PL must not be used for this technique and a supplemental graft such as gracilis tendon graft must be used as well. |
| Graft preparation | Care should be taken to suture the 2 limbs in an unequal fashion with the short limb being 95 mm from 1 end. |
| The ends of the tendon entering the sockets should be sutured for a length of at least 25 mm with high-strength suture. Lack of an appropriate length of suture or strength of suture may result in graft laceration. | |
| Surgical approach | In the subacute scenario, care must be taken to isolate the common peroneal nerve carefully. In such situations, the nerve may look like scar tissue or tendon and tendon or scar tissue may look like the nerve. |
| If careful attention is not paid to anatomic landmarks, the resulting reconstruction may not restore the stability. | |
| Graft passage | The tibial tunnel graft passage is the most challenging because the graft has to be pulled in from posterior to anterior. If it becomes hung up on soft tissue, then the fixation point of the tibia will be insecure, leading to compromised stability of the reconstruction. |
| Graft fixation | The cortical button must be sitting flush on the bone. Failure to ensure this would lead to slackness in the PT and PFL reconstruction. |
ACL, anterior cruciate ligament; PFL, popliteofibular ligament; PL, peroneus longus; PT, popliteus tendon.
Table 2.
Limitations
| The biomechanical strength of the described construct has not been studied in the laboratory or clinical setting. |
| A graft length of 25 mm is essential for this technique. |
| If the anterior tibial cortex blows out while drilling with the FlipCutter, this technique must be aborted. Tibial fixation of the graft can be performed with an interference screw as a salvage procedure. |
Footnotes
The authors report the following potential conflicts of interest or sources of funding: S.R.T. receives support from Arthrex, Zimmer Biomet, Smith and Nephew, and ConMed and receives royalties from Jaypee Publishers. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Anatomic posterolateral corner reconstruction in left knee with autogenous peroneus longus Y graft construct. The peroneus longus tendon is harvested from the left side and is measured to be at least 25 cm in length. The Y graft construct is prepared by looping the graft around a TightRope RT at 95 mm from the distal end. The prepared graft has a common 25-mm-long portion, a short segment for popliteus reconstruction, and a longer segment for popliteofibular and fibular collateral ligament reconstruction. Lateral dissection is begun with common peroneal nerve neurolysis. A tibial socket is created using a FlipCutter with a PCL Femur Jig as guide. The femoral and fibular tunnels are drilled. The graft is passed into the tibia first, followed by popliteus tendon, popliteofibular ligament, and fibular collateral ligament graft passage and fixation with an interference screw.
References
- 1.LaPrade R.F., Ly T.V., Wentorf F.A., Engebretsen L. The posterolateral attachments of the knee. Am J Sports Med. 2003;31:854–860. doi: 10.1177/03635465030310062101. [DOI] [PubMed] [Google Scholar]
- 2.LaPrade R.F., Wozniczka J.K., Stellmaker M.P., Wijdicks C.A. Analysis of the static function of the popliteus tendon and evaluation of an anatomic reconstruction. Am J Sports Med. 2010;38:543–549. doi: 10.1177/0363546509349493. [DOI] [PubMed] [Google Scholar]
- 3.Chahla J., Moatshe G., Dean C.S., LaPrade R.F. Posterolateral corner of the knee: Current concepts. Arch Bone Joint Surg. 2016;4:97–103. [PMC free article] [PubMed] [Google Scholar]
- 4.Ranawat A., Baker C.L., Henry S., Harner C.D. Posterolateral corner injury of the knee: Evaluation and management. J Am Acad Orthop Surg. 2008;16:506–518. [PubMed] [Google Scholar]
- 5.Harner C.D., Vogrin T.M., Höher J., Ma C.B., Woo S.L.Y. Biomechanical analysis of a posterior cruciate ligament reconstruction. Am J Sports Med. 2000;28:32–39. doi: 10.1177/03635465000280011801. [DOI] [PubMed] [Google Scholar]
- 6.LaPrade R.F., Resig S., Wentorf F., Lewis J.L. The effects of grade III posterolateral knee complex injuries on anterior cruciate ligament graft force. Am J Sports Med. 1999;27:469–475. doi: 10.1177/03635465990270041101. [DOI] [PubMed] [Google Scholar]
- 7.LaPrade R.F., Johansen S., Wentorf F.A., Engebretsen L., Esterberg J.L., Tso A. An analysis of an anatomical posterolateral knee reconstruction. Am J Sports Med. 2004;32:1405–1414. doi: 10.1177/0363546503262687. [DOI] [PubMed] [Google Scholar]
- 8.LaPrade R.F., Johansen S., Agel J., Risberg M.A., Moksnes H., Engebretsen L. Outcomes of an anatomic posterolateral knee reconstruction. J Bone Joint Surg Am. 2010;92:16–22. doi: 10.2106/JBJS.I.00474. [DOI] [PubMed] [Google Scholar]
- 9.Franciozi C.E., Albertoni L.J.B., Kubota M.S. A hamstring-based anatomic posterolateral knee reconstruction with autografts improves both radiographic instability and functional outcomes. Arthroscopy. 2019;35:1676–1685.e3. doi: 10.1016/j.arthro.2019.01.016. [DOI] [PubMed] [Google Scholar]
- 10.LaPrade R.F., Heikes C., Bakker A.J., Jakobsen R.B. The reproducibility and repeatability of varus stress radiographs in the assessment of isolated fibular collateral ligament and grade-III posterolateral knee injuries. J Bone Joint Surg Am. 2008;90:2069–2076. doi: 10.2106/JBJS.G.00979. [DOI] [PubMed] [Google Scholar]
- 11.Arthur A., LaPrade R.F., Agel J. Proximal tibial opening wedge osteotomy as the initial treatment for chronic posterolateral corner deficiency in the varus knee. Am J Sports Med. 2007;35:1844–1850. doi: 10.1177/0363546507304717. [DOI] [PubMed] [Google Scholar]
- 12.Fineberg M.S., Duquin T.R., Axelrod J.R. Arthroscopic visualization of the popliteus tendon. Arthroscopy. 2008;24:174–177. doi: 10.1016/j.arthro.2007.08.018. [DOI] [PubMed] [Google Scholar]
- 13.Wechter J.F., Bohm K.C., Macalena J.A., Sikka R.S., Tompkins M. Part II: The 50°/60° fibular tunnel trajectory for posterolateral corner reconstruction in a cadaver model. Knee Surg Sports Traumatol Arthrosc. 2014;23:1895–1899. doi: 10.1007/s00167-014-3087-1. [DOI] [PubMed] [Google Scholar]
- 14.Rhatomy S., Asikin A.I.Z., Wardani A.E., Rukmoyo T., Lumban-Gaol I., Budhiparama N.C. Peroneus longus autograft can be recommended as a superior graft to hamstring tendon in single-bundle ACL reconstruction. https://doi.org/10.1007/s00167-019-05455-w [published online March 15, 2019]. Knee Surg Sports Traumatol Arthrosc. [DOI] [PubMed]
- 15.Smith P.A., Stannard J.P., Pfeiffer F.M., Kuroki K., Bozynski C.C., Cook J.L. Suspensory versus interference screw fixation for arthroscopic anterior cruciate ligament reconstruction in a translational large-animal model. Arthroscopy. 2016;32:1086–1097. doi: 10.1016/j.arthro.2015.11.026. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Anatomic posterolateral corner reconstruction in left knee with autogenous peroneus longus Y graft construct. The peroneus longus tendon is harvested from the left side and is measured to be at least 25 cm in length. The Y graft construct is prepared by looping the graft around a TightRope RT at 95 mm from the distal end. The prepared graft has a common 25-mm-long portion, a short segment for popliteus reconstruction, and a longer segment for popliteofibular and fibular collateral ligament reconstruction. Lateral dissection is begun with common peroneal nerve neurolysis. A tibial socket is created using a FlipCutter with a PCL Femur Jig as guide. The femoral and fibular tunnels are drilled. The graft is passed into the tibia first, followed by popliteus tendon, popliteofibular ligament, and fibular collateral ligament graft passage and fixation with an interference screw.